Abstract
Lactic acid bacteria (LAB) in the microbiota play an important role in human and animal health and, when used as probiotics, can contribute to an increased growth performance in livestock management. Animals living in their native habitat can serve as natural sources of microorganisms, so isolation of LAB strains from wild boars could provide the opportunity to develop effective probiotics to improve production in swine industry. In this study, the probiotic potential of 56 LAB isolates, originated from the ileum, colon, caecum and faeces of 5 wild boars, were assessed in vitro in details. Their taxonomic identity at species level and their antibacterial activity against four representative strains of potentially pathogenic bacteria were determined. The ability to tolerate low pH and bile salt, antibiotic susceptibility, bile salt hydrolase activity and lack of hemolysis were tested. Draft genome sequences of ten Limosilactobacillus mucosae and three Leuconostoc suionicum strains were determined. Bioinformatic analysis excluded the presence of any known acquired antibiotic resistance genes. Three genes, encoding mesentericin B105 and two different bacteriocin-IIc class proteins, as well as two genes with possible involvement in mesentericin secretion (mesE) and transport (mesD) were identified in two L. suionicum strains. Lam29 protein, a component of an ABC transporter with proved function as mucin- and epithelial cell-adhesion factor, and a bile salt hydrolase gene were found in all ten L. mucosae genomes. Comprehensive reconsideration of all data helps to select candidate strains to assess their probiotic potential further in animal experiments.
Similar content being viewed by others
Introduction
A balanced and highly diverse microbiota is essential for healthy life of living organisms in the animal kingdom. Perturbed balance of the microbiota may lead to disease development. Conditions in industrial scale livestock production frequently result in increased stress and health problems. Farming conditions, environmental and nutritional effects and weaning difficulties are the main stress factors in the pig production sector affecting significantly animal health and production. The usage of antibiotics, to overcome stress related negative health effects as well as for growth promotion particularly, was banned in the European Union and in many other countries [1]. Probiotics, used as feed supplements, can serve as alternatives to antibiotics in various cases to avoid economic losses in swine production [2]. Probiotics have beneficial impacts on the balance of gastrointestinal microbiota, the ability to fight enteric pathogens, and capacity to support the immune system [3].
Lactic acid bacteria (LAB) are the most commonly used microorganisms as probiotics. LAB display a strong antimicrobial activity against a range of pathogenic microorganisms and can provide nutritional and health benefits to the hosts [4]. Among LAB, the most commonly used probiotic strains belong to lactobacilli [5], at a large extent due to the “Generally Regarded as Safe” (GRAS) status of these organisms [6]. Probiotic strains for pigs can improve growth performance, feed conversion efficiency, nutrient utilization, community structure of intestinal microbiota, gut health and regulate the immune system. There are several requirements for probiotic bacteria, the most important being that they must be harmless to the host, i.e. they must not have hemolytic activity or carry acquired antibiotic resistance determinants. It must also possess beneficial properties, such as antibacterial activity, pH and bile acid tolerance, vitamin production, immune-stimulatory activity. However, a given strain does need to possess all the beneficial properties. The roles of Lactobacillus sp. as probiotics for swine were reviewed widely [2, 7].
The source of probiotic strains is important, and they should be isolated from the intestinal microflora of the host animal species in order to achieve easier intestinal colonization and more specific applications. Host specificity was observed among lactobacilli isolated from human and animal sources [8]. Lactobacilli and streptococci isolated from swine have shown better adherence to swine squamous epithelial cells than strains isolated from other animals [9], indicating that survival of probiotic bacteria is dependent on a host-specific environment.
Although there is an extensive literature on the intestinal flora of domestic pig, the knowledge on the intestinal flora of wild boar, which are taxonomically the same species, is scarce. One of the main differences between domestic pigs and wild boars, apart from genetic differences, is that wild boars have to survive under natural conditions without the use of any feed additives, antibiotics or probiotics used in livestock production. Their microbiota may contain beneficial microorganisms that help to prevent various diseases and provide resistance to pathogens. As a result of domestication and prolonged selection in large-scale farming, the composition of the gut microbiota of domestic pigs has changed significantly, and bacterial strains with physiologically beneficial effects that are still found in natural populations may have been lost. Wild boars have a very diverse fecal bacterial community, probably due to their complex food structure [10], therefore it is possible to isolate microorganisms with different properties. Furthermore, wild boars have generally shown high tolerance and/or resistance to many diseases, suggesting that their gut bacteria may be a good source for isolation of potential probiotic strains. Therefore, we have chosen the intestinal contents of the different segments of the intestinal tract of wild boars as a source for the isolation of useful microorganisms. Recognition of the value of wild boar as a potential source of probiotic strains has been reported recently [11, 12].
The aim of the present study was to identify LAB isolated from wild boars and to screen them for probiotic attributes and safety properties in vitro, in order to select strains that can be used as direct fed microbials in the swine industry. The sampled wild boars were living in their native habitat, in one of the less human-affected regions in Hungary. Guidelines for the evaluation of probiotic activity of candidate strains, recommended by the Food and Agriculture Organization of the United Nations (FAO) [13] and reviewed in several articles [14,15,16], were followed to characterize the isolates. Determination of draft genome sequences and their bioinformatic analyses also facilitated the selection of candidate strains for further evaluation in animal experiments as direct-fed microbials for pigs.
Materials and Methods
Sources and Collection of Samples
Samples were taken from 5 (#1 - #5) wild boars (Sus scrofa) living in a native habitat of the Zemplén Mountain in Hungary near to the Slovakian border [17]. Wild boars were shot during regular hunts organized by the local hunting party in Füzérkomlós, the rightful owner of this hunting area for hunting with reference to the LV of 1996 Hungarian State Law on wildlife protection, wildlife management, and hunting, where the boars were professionally eviscerated. All the animals were healthy except for boar #1, which showed signs of enteritis with diarrhea [17]. Four of the wild boars were sows (#1 - #3 and #5) and one boar was male (#4). Three of the sampled animals were adults (#1 - #3), while two (#4 and #5) were young animals. During sampling, the parts of the intestinal tract designated for sampling were sealed with forceps, excised and transported to the laboratory under refrigerated and anaerobic conditions using anaerobic jars and processed within 24 h. The intestinal contents from ileum, colon, caecum and rectum were removed under sterile conditions.
Isolation and Identification of Lactic Acid Bacteria
Handling and Storage of Bacterial Samples
One gram from each sample was aseptically added to 5 mL of sterile phosphate buffered saline (PBS) solution (pH 7.2) and mixed thoroughly. Serial dilutions were performed and 0.1 mL aliquots from the dilutions were plated out onto different kinds of media such as BHI – Brain Heart Infusion Agar (Biolab Ltd., Hungary), TSA – Tryptic Soy Agar (Biolab Ltd., Hungary), M17 Agar (Biolab Ltd., Hungary), MRS – De Man, Rogosa and Sharpe Agar (BIOKAR Diagnostics, France), MRSCC – MRS agar supplemented with 5-5 g L−1 maltose, fructose, sucrose and 0.05 g L−1 cysteine-HCL (Sigma-Aldrich, Japan) and EA – Elliker Agar (Biolab Ltd., Hungary) in triplicate by spreading method. One set of the plates was incubated in an aerobic thermostat, the second set was placed into a CO2 (5 %) incubator (Sheldon Manufacturing, Inc., OR, US) (semi-anaerobic condition) and the third set of plates was placed into anaerobic jars supplemented with AnaeroGen 2.5 L sachets (Oxoid, Basingstoke, UK). Incubation was carried out at 35 °C for 48-72 hrs.
Single colonies (without selection) were suspended in 105 μL PBS buffer, then 45 μL of 50 % glycerol was added and the tubes were placed into a -70 °C freezer for storage.
Screening and Species-level Determination of Isolates By 16S Sanger Sequencing
Polymerase chain reaction (PCR) was used for determination of the 16S sequence of the isolates. A single colony was suspended in 100 μL peptone saline water (0.85 % NaCl and 0.1 % peptone) buffer. PCR was carried out using DreamTaq 2X PCR master mix (Thermo Scientific Ltd, UK) according to manufacturer’s instructions. As template, 1 μL of cell suspension from each strain in the collection was used in 20 μL reaction. Primer Lac1F (5’-AGCAGTAGGGAATCTTCCA-3’) and Lac2GCR (5’-ATTYCACCGCTACACATG-3’) [18] were used for screening LAB strains, Leucgrp fw (5’-GCGGCTGCGGCGTCACCTAG-3’) and Leucgrp rev (5’-GGNTACCTTGTTACGACTTC-3’) primers [19] were used to identify isolates belonging to the Leuconostoc genus. Universal primer pair, 27f (5’-AGAGTTTGATCCTGGCTCAG-3’) and 1492r (5’-GGTTACCTTGTTACGACTT-3’) [20] was used for amplification of the 16S rDNA. PCR conditions were the same as given in the papers reporting the primer pairs. The PCR products were purified using MinElute PCR Purification Kit (QIAGEN, Germany) according to the manufacturer’s instructions, and then sequenced with both primers (27f and 1492r). Sequencing of the amplicons was performed using Big-Dye Sequencer ABI 3130xl by BIOMI Ltd. (Gödöllő, Hungary). Sequence homologies were examined by comparing the sequences obtained with those of the NCBI databases (Reference RNA Sequences (refseq_ma) and RefSeq Genome Database (refseq_genomes)) using Basic Local Alignment Search Tool (BLAST) software [21] and identified according to the closest relative.
Screening of Isolates for Probiotic Attributes
Demonstration of Antimicrobial Activities
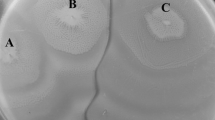
To assess the antimicrobial activity of the isolates the agar well diffusion assay [22] was applied. The isolates were inoculated to MRSCC broth at 35 °C for 24 h and the cell-free supernatants were collected by centrifugation (15,600×g, 10 min) to use in the test. Out of the 4 tester strains, Escherichia coli W3110 [23], Staphylococcus aureus SP17 [24] and Salmonella enterica serov. Typhimurium LT2 (ATCC 700720) were cultured in Luria-Bertani (LB) broth [25] and plated on LB agar, while M17 media (broth and agar) (Biolab Ltd., Hungary) were used to work with Streptococcus thermophilus T9 (Hungarian Dairy Research Institute Ltd, Hungary). After spreading 0.1 mL of overnight grown cultures from the tester strains on the agar plates by soft agar overlay, wells of 5 mm diameters were punched. Aliquots (80 μL) from the supernatants of the LAB cultures were dispensed into the wells, and the plates were incubated for 24 h at 35 °C and the appearance of a clearing zone was examined. The diameter of clear inhibition zone around the wells was measured with a ruler and isolates were rated as –, +, ++ and +++ (–: 6 mm; +: >6-9 mm; ++: 9-15 mm and +++: >15 mm).
Determination of Acid Tolerance of Selected Isolates
The acid tolerance of the isolates was tested at pH 2.0 and 3.0 in pilot experiments and finally measured accurately at pH 2.5. The isolates were sub-cultured in MRSCC broth at 35 °C for 24 h. From the cultures, 60 μL were added to 3 mL of MRSCC broth which was adjusted to pH 2.5. Viable count was conducted by counting colony forming units (CFU) on MRSCC agar plates from 20 μL aliquots taken immediately after inoculation and after 1 and 2 hours of incubation. Liquid cultures were incubated in CO2 incubator while plates were incubated in anaerobic jars (Oxoid, UK) containing AnaeroGen™ 2.5 L sachet (Thermo Scientific, UK).
Bile Tolerance Assay to Determine the Sensitivity of Isolates
To evaluate the ability of isolates growing in the presence of bile salt, isolates were cultured in MRSCC broth supplemented with 0.3 and 1.0 % (w/v) bile salt (bovine, Sigma-Aldrich, USA). Viable count was conducted by counting colony forming units on MRSCC agar plates from 20 μL aliquots taken after 4 and 7 hours of incubation. Liquid cultures were incubated in CO2 incubator while plates were incubated in anaerobic jars (Oxoid, UK) containing AnaeroGen™ 2.5 L sachet (Thermo Scientific, UK).
Tests for Addressing Safety Concerns
Antibiotic Susceptibility Testing to Detect Certain Acquired Antibiotic Resistances
The selection of antibiotics was based on previous publications [26,27,28]. These publications were designed to detect antibiotics specific to Gram-positive bacteria and representing multiple antibiotic types. Susceptibility of strains to selected antibiotics was evaluated by soft agar overlay disc diffusion method on MRSCC agar [26], with slight modifications (Petri plates, containing 20 mL agar, were overlaid with 3 ml of 0.8 % soft agar seeded with 50 μL of an active culture at 45 ℃). The following antibiotic discs (BIO-RAD, France) were used: erythromycin (15 μg), kanamycin (30 μg), tetracycline (30 μg), trimethoprim (5 μg), vancomycin (30 μg), oxacillin (5 μg) and azithromycin (15 μg). The diameters of inhibition zones were determined after anaerobic incubation at 35 ℃ for 24 h by using a Scan 500 inhibition zone reader (Interscience, France). Strains were categorized as resistant (R), intermediate (I) or susceptible (S) according to interpretative standards described previously [27]. The interpretation for oxacillin and azithromycin were based on data reported by the National Committee for Clinical Laboratory Standards [29] for staphylococci, as no other data of inhibition zone diameters for Limosilactobacillus were found in the literature. However, LAB strains showed various patterns when disks of 1 μg oxacillin were used [30, 31]. Quality was controlled by using Staphylococcus aureus ATCC 25923 for oxacillin and azithromycin and Enterococcus faecalis ATCC 19433 for the rest.
Monitoring the Presence of Bile Salt Hydrolase (BSH) Activity
BSH activity of candidate probiotics can be evaluated by the well-established agar plate assay [32]. In the setup of the semi-qualitative assay, we followed the report of [33] with some modifications. Sterile filter paper discs of 8 mm diameter were impregnated with 20 μL of cultured isolates on MRSCC agar (supplemented with 0.5 % sodium salt of taurodeoxycholic acid (Sigma-Aldrich, MO, USA) and 0.37 % CaCl2) plates. Plates were incubated at 35 °C for 72 h in anaerobic condition and the diameters of the precipitation zones around the disks were measured and rated as –, +, ++ and +++ (–: ≤ 14 mm, no precipitation zone; +: 14-24 mm; ++: 24-29 mm and +++: > 29 mm). Results were obtained and averaged from three independently repeated experiments.
Blood Hemolysis Test to Confirm the Safe Use of Isolates
Isolates were cultured in MRSCC broth for 24 h at 35 °C and the streak plate methods were performed on Columbia agar (Biolab Ltd., Hungary) plates supplemented with sterile sheep blood (5 % v/v) and kept for anaerobic incubation at 35 °C for 48 h. Hemolytic activity was judged by visual observation using Salmonella enterica serov. Typhimurium LT2 and Staphylococcus aureus SP17 strains as positive controls, showing complete hemolysis.
Genome Sequencing and Bioinformatics Analyses
Sequence Determination of Selected LAB Strains
The complete genome sequence of ten Limosilactobacillus mucosae (formerly Lactobacillus mucosae) [34] and three Leuconostoc suionicum (formerly Leuconostoc mesenteroides subs. suionicum) [35] strains were determined. Strains were grown using MRSCC broth medium at 35 °C for 24 h, then the cells were harvested and kept frozen in a –70 °C freezer until delivered to the sequencing facility. DNA preparation and sequence determination of the strains were performed by Xenovea Ltd. (Szeged, Hungary), except strain F1 which was performed by BIOMI Ltd. (Gödöllő, Hungary). De novo assembly of the raw reads was performed with SPAdes v3.0.0 software [36, 37] (https://cab.spbu.ru/software/spades/). After the de novo assembly, contigs below 500 bp were filtered out by using in-house Linux scripts. Contamination was removed using a BLAST search against the eukaryotic RefSeq sequences. RefSeq sequences were downloaded from NCBI. If the alignment length of the match was bigger than the half of the contig’s length we marked the scaffold as contamination and removed it from further analysis. The sequences of the cleaned draft genomes were deposited in the NCBI database, under accession number PRJNA926800.
Bioinformatics Analyses of Sequenced Potential LAB Strains
K-Mer Analyses
Draft genome sequences of the strains were analyzed by KmerFinder 3.2 program (Software version 3.0.2) [38,39,40]. The service was available at the homepage of Center for Genomic Epidemiology (https://cge.food.dtu.dk/services/KmerFinder/). Sequences in FASTA format were uploaded and compared to sequences in the “Bacteria organism” database (version 2022-07-11). “Query Coverage (%), the percentage of input query Kmers that match the template” in the output of the results, was used to evaluate taxonomical relationships at strain level.
Phylogenetic Analyses
Whole genome alignment was performed using progressiveMauve [41] (build date: Feb 13 2015). The command lines were the following for Limosilactobacillus:
progressiveMauve --output-guide-tree=Limosilactobacillus.tree --output Limosilactobacillus *.fasta
and for Leuconostoc:
progressiveMauve --output-guide-tree=Leuconostoc.tree --output Leuconostoc *.fasta
The guided tree was used to create trees which were drawn by using the ape package from R [42]. The used commands were the following for Limosilactobacillus:tree1 <- read.tree(“Limosilactobacillus.tree”); plot(tree1)and for Leuconostoc:
tree2 <- read.tree(“Leuconostoc.tree”); plot(tree2)
Similarity matrixes were created by using FastANI (version 1.33) [43]. The program calculates the average nucleotide identity for every sequence pair. The query and reference dataset were the same, they contained sequences of selected publicly available strains and of our sequenced strains. The command line options were the following for Limosilactobacillus:
fastANI --ql Limosilactobacillus.txt --rl Limosilactobacillus.txt -o Limosilactobacillus.out --matrix -t 10
and for Leuconostoc:
fastANI --ql Leuconostoc.txt --rl Leuconostoc.txt -o Leuconostoc.out --matrix -t 10
Screening for the Presence of Antibiotic Resistance Genes
Draft genome sequences of the strains were analyzed by ResFinder 4.1 software [44,45,46] to uncover the presence of any acquired antibiotic resistance gene. The service, available at the homepage of “Center for Genomic Epidemiology” (https://cge.food.dtu.dk/services/ResFinder/), was used with the following settings: selected %ID threshold 90 %, selected minimum length 60 %. ResFinder database: (2022-05-24). Sequences in FASTA format were uploaded according to instructions of the service provider.
Screening for Known Bacteriocin Genes
BAGEL4 web server (http://bagel4.molgenrug.nl/) has the ability for searching bacteriocins and RiPPs (ribosomally synthesized and posttranslationally modified peptides) [47]. Genome sequences were uploaded in FASTA format. Analyses were focused on genes with possible involvement in biosynthesis and functioning of bacteriocins.
Genes with Potential Relevance for Probiotics
A 29-kDa protein (Lam29) from L. mucosae ME-340 is an ABC transporter component, but it has also been shown to function as mucin- and epithelial cell-adhesion factor [48, 49]. Sequence of the lam29 gene was identified in each L. mucosae draft genome sequence by BLAST search. Genes were cut using seqret program [50]. Multiple alignment was constructed using Mafft (version 7.429) [51] with the following parameters:
-
--treeout --thread 10 --localpair --maxiterate 2000 --clustalout –reorder
The final tree was drawn using the ape package of R [42].
BSH genes were identified using Tblastn [52] search, because the query sequence was protein. Seqret from Emboss [50] was used to cut the region of the genes. Multiple alignment was constructed using Mafft with the same parameters as mentioned above. The final tree was drawn using the ape package of R [42].
Data Availability of Draft Genome Sequences
Tha draft genome sequences are available at NCBI under the BioProject: PRJNA926800.
Results
Isolation and Identification of Lactic Acid Bacteria
Bacterial Isolates and Their Screening By PCR Amplification
A primary strain collection of 4334 isolates has been established from colonies of different kinds of bacteria, originated from four locations of the gastrointestinal tracts (ileum, colon, caecum and rectum) of five wild boars living in natural habitat. Altogether, 1650 ileum, 1049 colon, 727 caecum and 908 rectum isolates were collected; 1128, 1624, 655, 409 and 518 derived from wild boar #1 to wild boar #5, respectively. Aerobic condition provided 2738 isolates, while semi-anaerobic and anaerobic gave 436 and 1160 ones, respectively.
For the screening of isolates from the strain collection, isolates belonging to four genera such as Lactobacillus, Pediococcus, Leuconostoc and Weissella could be identified by LAB specific PCR. PCR positive isolates were purified by sub-culturing and plating until pure colonies were obtained, and a secondary strain collection (894 isolates) has been created from pure cultures. For further screening and characterization, 166 strains were selected (Supplementary Table 1). PCR specific for Leuconostoc genus was suitable to identify 20 strains which belong to this genus (Supplementary Table 1), while classification of the rest of the isolates required other sequence-based method, such as 16S sequencing.
Demonstration of Antimicrobial Activities of the Selected Isolates
Ability of the 166 LAB strains to produce any antimicrobial compound was tested against 4 tester strains, Escherichia coli W3110, Staphylococcus aureus SP17, Salmonella enterica serov. Typhimurium LT2 (ATCC 700720) and Streptococcus thermophilus T9. The antimicrobial activity was quantified by measuring the diameter of the inhibition zone and rated as -, +, ++ and +++.
Of the 166 strains, 164 exerted antimicrobial activity against Escherichia coli and 158 against Salmonella enterica and Staphylococcus aureus. It was found that 64 strains had inhibitory effect on the growth of Streptococcus thermophilus as well (Supplementary Table 1).
The 166 isolates were grouped according to their antibiotic activity patterns. The 20 Leuconostoc isolates were classified into 3 groups while the other LAB isolates were classified into 46 groups (results are presented in Table 1 and Supplementary Table 1).
There were 56 isolates (9 Leuconostoc and 47 other LAB strains) selected for further characterization which represented the majority of the groups (Table 1). In addition to the obtained rating patterns of antimicrobial activity, origin of the samples was also taken into consideration to cover as many gut regions as possible from each wild boar.
Taxonomic Identification of Selected Isolates
Sequencing of the 16S rRNA gene region (~1380±40 bp sequence between nucleotides 27 and 1492) from each selected strain was used for taxonomic identification at species level. Comparison of the obtained sequences to sequences in NCBI databases resulted in the identification of 47 Limosilactobacillus mucosae (L. mucosae) and 9 Leuconostoc suionicum (L. suionicum) strains (Table 1 and Supplementary Table 1). BLAST search in both refseq_ma and refseq_genomes databases gave concordant results for L. mucosae strains.
In the case of Leuconostoc strains, searches in the refseq_ma database identified the strains as a member of Leuconostoc mesenteroides species with 99.93 % identity, while searches in the refseq_genomes database identified the strains as a member of L. suionicum species with 100 % identity. We have accepted L. suionicum species as the closest relatives.
Screening of Isolates for Probiotic Attributes
Determination of Acid Tolerance of the Isolates
The effect of acidity on the viability of the selected isolates was assessed by measuring their growth at pH 2.5 in MRSCC broth. Viable colony forming units were detected in aliquots collected immediately after inoculation and after 1 and 2 hours of incubation, reflecting the time spent by food in the stomach [53]. The experiment was also performed at pH 2.0 and pH 3.0, but the results were inconclusive. Essentially, at pH 3.0 there were no significant difference between viability of the isolates, whereas at pH 2.0 all strains were seriously affected after 1 h (data not shown).
The majority of L. mucosae strains tolerated pH 2.5 for 2 hours very well, as viable counts were close to or even higher than the starting state (over 0.7 log unit increase in the case of F4, F23, F49, F68, F116 and F132), while in some cases (F10, F105, F120 and F122) a significant reduction (1-3 log units) was observed (Supplementary Table 2).
L. suionicum strains were rather sensitive to low pH exposure, as differences were visible after 1 h incubation. The viability of four strains was reduced with 1.5-2.1 log units (F150, F151, F156 and F163) while the other five strains lost their viability entirely. Further incubation eliminated viability of all strains (Supplementary Table 2).
Identification of Isolates Tolerant to Bile Stress
When the experimental parameters were determined, the bile salt concentration of 0.3 % was considered as physiological condition in mammalian guts [54], whereas 1.0 % bile salt concentration represented a high stress condition. The 7 h incubation time resemble to the time that bacteria spend in the gut region where high bile salt stress condition occurs.
At 0.3 % bile salt concentration, 28 out of the 56 strains showed increased viable counts after 7 h incubation compared to initial counts, two of them over 0.8 log units (F139 and F151) (Table 3). Decrease in viable counts were less than 0.2 log unit in the case of another 12 strains. Only 3 strains (F13, F45 and F69) suffered over 1.0 log unit decrease in viable counts at this condition (Supplementary Table 3).
At 1.0 % bile salt concentration, only three L. mucosae (F20, F84 and F88) and two L. suionicum (F151 and F158) strains were able to maintain or exceed initial counts after 7 h incubation. Six L. mucosae (F2, F4, F7, F35, F45 and F133) and two L. suionicum (F150 and F156) strains showed less than 0.4 log unit decrease. These 13 strains were considered to be highly tolerant against bile stress. Four L. mucosae strains (F15, F16, F71 and F132) were rather sensitive against bile stress (over 2.5 log units decrease in viable counts) (Supplementary Table 3).
Tests for Addressing Safety Concerns of LAB Strains
Antibiotic Susceptibility Testing to Determine Resistance Pattern of Isolates
We have tested the 56 strains for 7 antibiotics (erythromycin, kanamycin, tetracycline, trimethoprim, vancomycin, oxacillin and azithromycin) by disc diffusion method and the results are shown in Fig.1. All strains were resistant to vancomycin and kanamycin, however, we have found 5 L. mucosae strains (F10, F20, F23, F24 and F113) sensitive to trimethoprim, while the rest of the strains were resistant. All strains were sensitive to erythromycin. There were no strains resistant to tetracycline, oxacillin and azithromycin but the phenotype distribution of L. mucosae strains was 29 sensitive and 18 intermediate to tetracycline, 35 sensitive and 12 intermediate to oxacillin and 37 sensitive and 10 intermediate to azithromycin, according to criteria published in [27]. L. suionicum strains were mainly sensitive to these three antibiotics except for 1 intermediate to tetracycline (F158) and 2-2 intermediate to oxacillin (F147 and F150) and azithromycin (F150 and F158).
Heat map of antibiotic susceptibility classification of selected isolates. F1-F146 are L. mucosae, while F147-F166 are L. suionicum strains. Horizontal lines maintain and separate groups established according to antimicrobial patterns of the strains. Strains in a group have identical antimicrobial pattern for the four tester strains used. (Table 1 and Supplementary Table 1). Color coding: red = resistant; orange = intermediate and green = susceptible
Monitoring the Presence of Bile Salt Hydrolase (BSH) and Blood Hemolysis Activity
Out of the 56 isolates tested for BSH activity, none of the 9 L. suionicum strains were positive, while all the 47 L. mucosae strains expressed reasonable activity. Strains F14, F16, F18, F69, F79 and F105 showed below average, while F10, F35, F49, F133, F139 and F146 showed above average BSH activity (Table 2).
It is important that probiotic bacteria do not cause lyses of red blood cells in the host organism. Although there are no published reports on the hemolytic activity in lactobacilli so far, for safety reasons, the analyses cannot be avoided. None of the strains, except positive controls (Salmonella enterica serov. Typhimurium LT2 and Staphylococcus aureus SP17), showed hemolytic activity under the assay conditions.
Genome Sequencing and Bioinformatics Analyses
Whole Genome Sequencing of Selected Isolates
Ten L. mucosae and three L. suionicum strains were selected for whole genome sequencing. Features of sequence assembly are shown in Table 3, and the sequences were deposited in NCBI database (accession number PRJNA926800). The relatively low contig numbers and the size of longest contigs indicate that sequencing quality meets the general standards. The genome size range of L. mucosae strains is 1.86-2.45 Mb [55], and the observed genome size of our strains fell in the range of 2.08-2.32 Mb (Table 3), while the genome size of L. suionicum falls between 2.02 and 2.13 Mb according to ten known strains available in NCBI database, our genomes have a size range of 2.13-2.16 Mb (Table 3).
Taxonomic Analyses of Isolates Based On Whole Genome Sequencing
K-mer analysis can identify the closest relatives of a query sequence within a targeted database, in our case the “Bacteria database”. All ten L. mucosae strains showed the best match to L. mucosae LM1 strain (Accession No: NZ_CP011013.1), however, F7, F88 and F108 comprise a cluster with values within the 65-71 % range, while the other 7 strains formed a different cluster with values in the 16-21 % range (Table 3). All three L. suionicum strains showed the best match to L. mesenteroides subsp. suionicum DSM 20241 (Accession No: NZ_CP015247.1). Due to a recent update in the NCBI database, accession number NZ_CP015247.1 now represents the genome sequence of L. suionicum DSM 20241. The K-mer analyses confirmed the results of our previous, 16S sequence-based species identification as well as identified the closest known relatives in the database at strain level.
Phylogenetic Relationships of the Sequenced Strains
Sequence comparison of the draft genome of the strains by FastANI (version 1.33) program revealed their relationships. Similarity matrixes, based on the average nucleotide identity for each sequence pair, were obtained (Supplementary Table 4) and relationship between the strains was demonstrated by phylogenetic trees (Fig. 2A and B).
Phylogenetic relationship of Limosilactobacillus (A) and Leuconostoc (B) strains based on comparison of whole genome sequences. CP011013.1 indicates the position of L. mucosae LM1 (Accession No: NZ_CP011013.1) in part A and CP015247.1 indicates the position of L. suionicum DSM 20241 (Accession No: NZ_CP015247.1) in part B, which were the best matching strains according to the K-mer analyses. Strain sequences used for comparison with genome sequences of our strains were obtained from the NCBI database and marked with their accession numbers. L. reuteri SD2112 (CP002844.1) was used as outgroup control, and CP062966.1, CP058954.1, CP049766.1 and JSWI00000000.1 refer to L. mucosae strains, such as LM011, A1, L1 and DPC6426, respectively in part A. CP058345.1 refers to Leuconostoc sp. MTCC 10508, reclassified as L. suionicum [56], and AP017935.1 refers to L. suionicum LT-38, while CP028255.1, CP021966.1, CP035271.1, CP035746.1, CP021491.1 and CP035139.1 refer to L. mesenteroides strains, such as SRCM102735, CBA7131, SRCM103453, SRCM103460, WiKim33 and SRCM103456, respectively in part B
The L. mucosae strains F7, F88 and F108 form a subclade, which is clustered together with certain known L. mucosae strains available in the database such as LM1 (NZ_CP011013.1), LM011 (CP062966.1), L1 (CP049766.1), A1 (CP058954.1) and DPC6426 (JSWI00000000.1). The other 7 sequenced strains form another subclade but with higher diversity in their genome sequences (Fig. 2A). However, the subclade of 7 strains could be divided further into two clusters, one containing the genomes of the F1, F2, F20 and F146 strains while the other one the genomes of the F4, F17 and F45 strains. It is worth noting that clustering of the strains was completely independent from their origin within the gastrointestinal tract.
L. suionicum strains F150, F151 and F156 clustered together with L. suionicum DSM 20241 (NZ_CP015247.1) and other L. suionicum strains such as MTCC 10508 (CP058345.1) and LT-38 (AP017935.1) but they were completely distinct from the group of L. mesenteroides strains (Fig. 2B).
Testing for the Presence of Transmissible Antibiotic Resistance Genes
Draft genome sequences were analyzed to identify strains carrying potentially transmissible antibiotic resistance determinants. ResFinder 4.1 was applied and the results did not provide evidence for the presence of any known acquired antibiotic resistance gene in the strains investigated (data not shown). Consequently, our strains can be considered safe regarding possible transmissible antibiotic resistances.
Screening for Known Bacteriocin Genes
The BAGEL4 web tool was used to identify genes with possible bacteriocin function in the sequences of the strains. There were no hits with significant similarity (protein BLAST results were below 50 % match) to any known bacteriocin protein or peptide in the sequences of the L. mucosae strains. The annotation of the LM1 sequence, their closest relative L. mucosae, was also checked in the database and the result was also negative.
In the case of L. suionicum strains, no bacteriocin gene was detected in F151 according to BAGEL4 search, while F150 and F156 showed identical, positive results. Both strains have the same identical bacteriocin genes, encoding a 53 amino acid (AA) long peptide with 96.23 % identity to mesentericin B105 according to BAGEL4 and lactococcin family bacteriocin (Accession number: WP_032489578) according to protein BLAST. In the close proximity of this gene (1310 bp downstream), two tandem open reading frames were identified. The mesD gene, encoding a 722 AA long protein, showed 84.10 % identity to mesentericin Y105 transport/processing ATP-binding protein, MesD (Accession number: Q10418.1). Next to this gene, the mesE gene, coding a 458 AA long protein, showed 66.81 % identity to mesentericin Y105 secretion protein, MesE (Accession number: Q10419.1).
Upstream to the mesentericin B105 gene, there were two more genes, encoding bacteriocin class IIc type proteins. The 48 AA protein showed 97.96 % identity to lactococcin G-beta/enterocin 1071B family bacteriocin (Accession number: WP_010015613.1), while the 47 AA protein showed 95.74 % identity to lactococcin G-alpha/enterocin 1071A family bacteriocin (Accession number: WP_224172900.1).
Identification of Genes With Potential Relevance for Probiotics
Gastrointestinal retention of probiotic bacteria is highly dependent on the interaction between bacterial cell surface proteins and the mucus layer of the host gut. In the case of L. mucosae, a 29-kDa protein (Lam29), a cysteine-binding protein of an ABC transporter, has been identified previously and its mucin- and epithelial cell-adhesion capability was proved. We have intended to see whether the Lam29 protein gene exist in our strains. The corresponding coding region has been identified in each L. mucosae draft genome sequence, and they were compared to sequences of other L. mucosae strains found in the NCBI database. Relationships of the alleles are shown in a phylogenetic tree (Fig. 3A). Clustering of F1, F2 and F20 as well as F7, F88 and F108 strains based on relatedness of the lam29 genes resemble their clustering based on the entire genomes, while clustering of F146 together with F4 and F45 and the position of F17 shows a significant alteration in this context.
Phylogenetic relationship of lam29 genes (A) and bsh genes (B) found in Limosilactobacillus mucosae strains. Sequences used for comparison with sequences of our strains were obtained from NCBI database and marked with their accession numbers. AB458523.1 refers to ABC2745 gene in L. mucosae OLL2745, CP062966.1 refers to L. mucosae LM011 in part A, and CP011013.1, CP058954.1, CP049766.1 and JSWI00000000.1 refer in both part A and B to L. mucosae strains, such as LM1, A1, L1 and DPC6426, respectively
It has been shown experimentally that all 47 L. mucosae strains expressed reasonable BSH activity, while none out of the 9 L. suionicum strains did. We have intended to trace this phenomenon in the obtained sequences as well. No bsh gene was found in the L. suionicum sequences, while one bsh gene was identified in each L. mucosae genome, and their relationship is presented in a phylogenetic tree (Fig.3B). Clustering of F1, F2, F20 and F146 as well as F4, F17 and F45 strains based on relatedness of the bsh genes is similar to their clustering based on the entire genome sequences. F88 and F108 also clustered together as it could be expected but F7 did not join to this group, it rather showed closer relationship with L. mucosae LM1.
Discussion
Probiotics development has become a promising field of biological investments in the last decade. Despite the fact that large number of probiotic strains have been isolated, characterized and published so far and many of them are commercially available worldwide, discovery of new strains with promising probiotic properties is always desirable, as probiotic features are strain-specific and possess different beneficial properties and effects [3, 57]. In our study we report our efforts to isolate lactic acid bacteria from free-living wild boars to select strains with probiotic values for swine industry.
To establish a primary strain collection, colonies were isolated from gut content at four locations of the gastrointestinal tracts (ileum, colon, caecum and rectum) of five wild boars. The use of six different media in three incubation conditions (aerobic, semi-anaerobic and anaerobic) ensured that a broad spectrum of bacteria was isolated.
For screening the isolates, a PCR-based approach was an efficient way to narrow down the strain collection by using a primer pair, specific for four genera (Lactobacillus, Pediococcus, Leuconostoc, and Weissella) [18]. The narrowed collection including the genus Lactobacillus, the one that has been found to be safe for consumption (having “Generally Regarded as Safe” (GRAS) status) [6]. PCR positive isolates were further classified by culture-based methods. This step led to further selection of the isolates, since only well-culturable strains are suitable for probiotics development, so strains not meeting this criterium were omitted from further study.
Based on the above criteria, 166 strains were selected for further screening. Since having antimicrobial activity is one of the main requirements for probiotics, the isolates were evaluated for their antibacterial activity against four tester strains and according to their antimicrobial activity pattern, 56 strains were selected for further analysis.
Taxonomic identification at species level, based on 16S rDNA sequence determination and comparison to sequences in reference databases, was essential for further characterization of potential probiotic isolates. It is worth mentioning that a major reclassification of lactobacilli species was performed recently [34], renaming the former species Lactobacillus mucosae to Limosilactobacillus mucosae. Leuconostoc suionicum is a young species, it was first established as a subspecies within the L. mesenteroides species [58] and later became a self-standing species [35]. Out of our 166 strains we have identified so far, 61 L. mucosae and 11 L. suionicum strains (Supplementary Table 1). There is currently no explanation why only these two species were identified from our samples instead of isolating more species, particularly from lactobacilli. However, it remains possible that other species are present among the remaining 94 isolates.
L. mucosae was discovered by Roos et al. [59] as a new Lactobacillus species with in vitro mucus-binding ability, isolated from pig small intestine. Since then, L. mucosae strains were isolated from human source, such as feces [60], ileal epithelium [61], vaginal tract [62] and from bovine intestine and stool [63], as well as from milk of goat [64], sheep [65] and donkey [66]. Recently, the isolation and comparative genome analyses of 93 of L. mucosae strains from different niches have been reported [55]. Taxonomic position of the species within the genus Limosilactobacillus has been confirmed recently [67]. In parallel to isolation of new L. mucosae strains of different origins, the evaluation of the probiotic potential of the species was also performed, confirming that L. mucosae strains can be selected as probiotics since they possess a broad spectrum of biological functional attributes [66]. L. mucosae strain LM1 has been studied extensively in vitro [59, 68,69,70,71,72,73] and its probiotic potential was also investigated in vivo [74].
L. mucosae strains have been shown to inhibit a number of Gram (+) and Gram (-) pathogens [71], such as Escherichia coli, Salmonella enterica [69] and Staphylococcus aureus [75]. Our results are consistent with these findings, 56 out of the 61 identified L. mucosae strains exerted antimicrobial activity against Escherichia coli, Salmonella enterica and Staphylococcus aureus, while 38 of them had inhibited the growth of Streptococcus thermophilus (Supplementary Table 1 and Table 1).
Regarding Leuconostoc suionicum, the first complete genome sequence was published in 2017 (L. suionicum DSM 20241 [76]). Currently, 2 complete and 8 draft genome sequences are available in the NCBI database, and recent reclassification within the Leuconostoc genus confirmed the taxonomic status of the species [77]. A high degree of similarity between the genome sequences of L. suionicum and Leuconostoc mesenteroides was detected, which is not surprising since the previous L. suionicum strains belonged to a subspecies of Leuconostoc mesenteroides [35]. Studies addressing probiotic assessment of microorganisms in the genus Leuconostoc, in particular L. mesenteroides species, are very diverse in the literature but no detailed probiotic study has been performed on strains of L. suionicum species. It was shown that all 20 Leuconostoc strains, including the 11 L. suionicum ones exerted antimicrobial activity against Escherichia coli, Salmonella enterica and Staphylococcus aureus but not against Streptococcus thermophilus (Supplementary Table 1 and Table 1).
It is very important that probiotic strains do not cause any harm to the host organism, so their safety of use should be monitored in this respect as well. According to safety regulations and standards [1], – “Strains of micro-organisms carrying an acquired resistance to antimicrobial(s) shall not be used as feed additives, unless it can be demonstrated that resistance is a result of chromosomal mutation(s) and it is not transferable.” –, determination of the antibiotic susceptibility profile of potential strains should be performed. The aim is to exclude the presence of any transmissible, acquired antibiotic resistance gene, but the presence of non-transmissible, intrinsic antibiotic resistance genes is acceptable or can be even beneficial. Seven antibiotics (erythromycin, kanamycin, tetracycline, trimethoprim, vancomycin, oxacillin and azithromycin) were used to determine the antibiotic resistance/susceptibility patterns of the selected strains by disc diffusion method.
In general, most Lactobacillus species are intrinsically resistant to kanamycin, vancomycin and trimethoprim, while sensitive to tetracycline, erythromycin and oxacillin [78, 79]. However, acquired determinants encoding resistance for tetracycline and erythromycin were detected in some Lactobacillus species [79]. It is difficult to say how reliably the vast amount of data and analyses accumulated for the genus Lactobacillus can be applied to the genus Limosilactobacillus. Data on the susceptibility of L. mucosae strains are sparse, but two strains reported were resistant to vancomycin and sensitive to tetracycline and erythromycin [66]. As expected, all 47 L. mucosae strains tested were resistant to vancomycin and kanamycin but surprisingly 5 strains were sensitive to trimethoprim. All 47 strains were sensitive to erythromycin. Although none of the strains were resistant to tetracycline, oxacillin and azithromycin, 18, 12 and 10 strains had intermediate phenotype, respectively (Fig. 1). If all strains with intermediate antibiotic resistance are excluded, 21 of the 47 L. mucosae strains need to be excluded from further probiotic development.
Leuconostoc species have intrinsic resistance to vancomycin and trimethoprim, while atypical resistance to kanamycin, tetracycline and erythromycin has been observed [80]. All 9 L. suionicum strains tested were resistant to vancomycin, trimethoprim and kanamycin (Fig. 1), and all strains were sensitive to erythromycin. While vancomycin and trimethoprim resistance are acceptable, the presence of kanamycin resistance raises concerns. It will be necessary to prove their non-transmissible nature if the strains are selected for probiotics development. Intermediate phenotypes were also detected: 1 strain to tetracycline and 2-2 strains showed intermediate resistance to oxacillin and azithromycin respectively (Fig. 1). These results suggest that a total of 3 out of 9 L. suionicum strains should be considered for exclusion.
As a molecular approach we have used specific primer pairs to reveal the presence of blaZ gene for ampicillin, tet(K) for tetracycline, sat4 for streptothricin, mph(C) and msrA for macrolides, mecA for meticillin and oxacillin, dfr(A) for trimethoprim, aph(3)-III for kanamycin resistance by PCR methods [28]. None of these genes were present in our strains investigated. Since both the disk diffusion antibiotic susceptibility and PCR tests have serious limitation, whole genome sequence could be a good way to assess the safety of the strains. Draft whole genome sequences of ten L. mucosae and three L. suionicum strains were determined. Bioinformatic analysis ruled out the presence of any known acquired antibiotic resistance gene within these genomes. Based on this result, there is no reason to exclude any of these candidate strains due to presence of prohibited transmissible antibiotic resistance.
Taxonomical identity of the strains was confirmed in three independent ways. Primarily, 16S rDNA sequencing gave convincing results for species-level identification. Using draft genome sequences, K-mer analyses identified the best matching sequences in the database and thus, in addition to species determination, the closest relatives were identified at strain level (Table 3). Finally, analysis of the average nucleotide identity (ANI) of the genomes of our own and some related strains in the NCBI database confirmed the previous results, and phylogenetic trees showed the relationship between the strains investigated (Fig. 2A and B).
Phylogenetic relationship of the strains, as shown by both, the pairwise values of the similarity matrix of the ANI analyses (Supplementary Table 4) and phylogenetic trees (Fig. 2A and B), indicate that our isolation and screening protocol worked well and allowed the identification of distinct strains for both species. L. mucosae strain F7, F88 and F108 are closely related to the type strain L. mucosae LM1 and some other known strains in the database, while the other 7 strains form a separate subclade (Table 3 and Fig. 2A). The similarity between L. suionicum strains F150 and F156 is 99.9999 % based on FastANI analysis, indicating that they could be identical. Although it would not be a surprising result, since they derived from the same sample, but their behavior was different in both, the antimicrobial activity test (Table 1) and antibiotic susceptibility profile (Fig. 1), so they are still considered to be different strains.
Bacteriocin production of some LAB strains may ensure their stable persistence in the microbial population as they may have competitive advantage over other microorganisms. The presence of enterolysin A genes was reported in several L. mucosae strains by sequence analyses [55]. However, there was no known bacteriocin gene detected either in our L. mucosae strains, or in the closest relative L. mucosae LM1, although some of the strains, such as F1, F2, F4 and F7, exhibited strong antimicrobial activity against several different microorganisms.
The sequences of the two very closely related L. suionicum strains (F150 and F156) contained such genetic elements that are likely to be involved in antibacterial function, whereas we could not identify bacteriocin related genes in the closely related F151. From the antibacterial factors identified in Leuconostoc strains F150 and F156, mesentericin B105 could theoretically be functional, as it has been reported that the MesDE secretion machinery is capable of transporting and maturing different pre-bacteriocins, mesentericin Y105 and B105 [81]. Since the mesDE genes in strains F150 and F156 showed significant similarity to the mesDE genes of the mesentericin Y105 system, and it has been previously shown that the mesentericin Y105 system is cross-compatible with B105 system [81, 82], and as a consequence, functional mesentericin B105 may be present in F150 and F156 strains. In addition to mesDE genes, the mesentericin operon in different Leuconostoc strains also contained some additional genes [83], however, we have not identified similar genes in the region.
It is well known that there are multifunctional proteins, sometimes called moonlighting proteins, which perform two or more functions in addition to their primary (originally identified) function [84]. In lactobacilli, the following proteins have been reported to act as mucin adhesion factors: elongation factor Tu (EF-Tu), glyceraldehyde 3-phosphate dehydrogenase (GAPDH), chaperonin GroEL, and ATP-binding cassette (ABC) transporter [85]. The presence of the mucus-binding protein (MUB) leaded to the discovery of the new species, Lactobacillus mucosae [59] and mucin-adhesion ability of L. mucosae LM1 was tested in vitro [69]. The elongation factor Tu, glyceraldehyde 3-phosphate dehydrogenase, and the phosphocarrier protein HPr were upregulated in L. mucosae LM1 when co-cultured with intestinal porcine epithelial cells [72]. In L. mucosae a 29-kDa protein (Lam29), an ABC transporter component protein has been identified and its mucin- and epithelial cell-adhesion capability was proved [48, 49]. The presence of an orthologue gene of the ABC transporter protein has also been demonstrated in the L. mucosae LM1 genome [68].
It is evident that mucin binding ability of the strains investigated needs to be addressed experimentally, since even more than one adhesion factor may be involved, and their combined effect should be determined. However, the Lam29 protein appears to be a L. mucosae-specific mucin adhesion factor, and the presence of the lam29 gene in the sequenced strains raises the possibility that the strains possess one of the desirable properties of probiotics, the ability to bind mucins. The likelihood of the presence of a functional lam29 gene in our strains investigated is further supported by the fact that the proven mucin-binding L. mucosae LM1 was their closest relative in the entire database (Table 3), the relationship of this gene family is presented in Fig. 3A.
Gut microbial enzymes contribute significantly to bile acid metabolism through deconjugation and dehydroxylation reactions to generate unconjugated and secondary bile acids. These microbial enzymes (which include bile salt hydrolase (BSH)) are essential for bile acid homeostasis in the host and represent a vital contribution of the gut microbiome to host health [86].
Conjugated bile acids are toxic to bacteria, particularly at low pH, and can affect the bacteria growth in different regions of the GI tract [87]. BSH can confer a protective effect to certain bacteria through bile acid deconjugation and can be an advantage during bacterial colonization, thus BSH activity can be associated with a higher survival of intestinal transit by rendering them more tolerant to bile salts. Therefore, it has become a selection criterium for probiotics [88,89,90,91]. However, it is yet not completely clear whether BSH activity is a desirable property [92], as high levels of certain secondary bile acids have proinflammatory effect [93] and can promote the development of infectious, inflammatory or malignant diseases [94, 95]. On the other hand, abundance of the bsh gene was significantly reduced in patients with inflammatory bowel disease (IBD) and type-2 diabetes [96].
BSH enzymes are present in various microbial species in most phyla [89]. It was shown that BSH-positive LAB commonly exists in the GIT and the BSH activity of LAB was correlated with their natural habitat [97]. BSH-encoding lactobacilli have primarily a vertebrate-adapted lifestyle as opposed to environment- or plant-associated lactobacilli [95].
The number of bsh alleles can vary, with up to 4 different alleles occurring in certain isolates of different Lactobacillus species [98,99,100,101,102,103], but misclassification of bsh genes in databases has also occurred [98, 103]. It was shown by in silico analysis of 8 Lactobacillus mucosae genomes that all of them contained only one bsh gene [98]. More than 300 LAB strains belonging to several genera have been investigated and BSH activity was found in the majority of Lactobacillus strains but was absent in L. mesenteroides strains [97]. Our results coincide with these findings, since BSH activity was found in all the 47 L. mucosae strains investigated (Table 2) and identified one bsh gene in each of the 10 sequenced genomes (Fig. 3B). Surprisingly, no bsh gene was found in the genome sequence of L. mucosae LM011 (Accession number: CP062966.1). On the other hand, our 9 L. suionicum strains did not show any BSH activity (Table 2), and three sequenced genomes did not contain any bsh gene.
For probiotics development, isolation of candidate bacteria, assessment of their probiotic potential and safety attributes in vitro are only the beginning steps. In this context, a wide range of in vitro attributes should be investigated, preferably using a combination of classical microbiological, molecular biological and genomic methods. In this way, the range of potential probiotic strains can be narrowed down considerably, as we have done in our current work. However, even the most careful in vitro experiments cannot provide a conclusive answer as to which strains are suitable for use as probiotics. As a consequence, potential probiotic strains can and should be tested in targeted animal experiments.
In our study, from the rich primary collection of isolates from different gut contents of wild boars, 56 strains were selected for detailed analyses. The majority of the strains possessed antibacterial activity against four different common bacteria, including pathogenic ones, and were highly tolerant to stress factors, characteristic for gut environment, such as low pH and high bile concentration. None of the strains had hemolytic activity, and there was no sign of having any transmissible antibiotic resistance genes as well. It is still not clear whether high BSH activity will be a desirable attribute for the final probiotic development, but by having the full spectrum (strong, medium and weak activity in L. mucosae strains and no activity in L. suionicum strains) available, it gives us the opportunity to select strains with the desired characteristics. Further assessment in the course of in vivo feeding experiments is necessary to prove the usefulness of probiotic strains in pig farming.
References
European Parliament and the Council of the European Union (2008) Commission Regulation (EC) No 429/2008 of 25 April 2008 on detailed rules for the implementation of Regulation (EC) No 1831/2003 of the European Parliament and of the Council as regards the preparation and the presentation of applications and the assessment and the authorisation of feed additives Off J Eur Union L133:1-653. http://data.europa.eu/eli/reg/2008/429/oj
Dowarah R, Verma AK, Agarwal N (2017) The use of Lactobacillus as an alternative of antibiotic growth promoters in pigs: A review. Anim Nutr 3:1–6. https://doi.org/10.1016/j.aninu.2016.11.002
Sirichokchatchawan W, Pupa P, Praechansri P, Am-in N, Tanasupawat S, Sonthayanon P, Prapasarakula N (2018) Autochthonous lactic acid bacteria isolated from pig faeces in Thailand show probiotic properties and antibacterial activity against enteric pathogenic bacteria. Microbial Pathogenesis 119:208–215. https://doi.org/10.1016/j.micpath.2018.04.031
Devi SM, Archer AC, Halami PM (2015) Screening, characterization and in vitro evaluation of probiotic properties among lactic acid bacteria through comparative analysis. Probiotics Antimicro Prot 7:181–192. https://doi.org/10.1007/s12602-015-9195-5
Zhang Z, Lv J, Pan L, Zhang Y (2018) Roles and applications of probiotic Lactobacillus strains. Appl Microbiol Biotechnol 102:8135–8143. https://doi.org/10.1007/s00253-018-9217-9
United States Food and Drug Administration (2018) Generally Recognized as Safe (GRAS). Microorganisms and Microbial-Derived Ingredients Used in Food (Partial List). Available at https://www.fda.gov/food/generally-recognized-safe-gras/microorganisms-microbial-derived-ingredients-used-food-partial-list
Valeriano VD, Balolong MP, Kang DK (2017) Probiotic roles of Lactobacillus sp. in swine: insights from gut microbiota. J Appl Microbiol 122:554–567. https://doi.org/10.1111/jam.13364
Morelli L (2000) In vitro selection of probiotic lactobacilli: a critical appraisal. Curr Issues Intest Microbiol 1:59-67. https://www.researchgate.net/publication/11644989
Barrow PA, Brooker BE, Fuller R, Newport MJ (1980) The attachment of bacteria to the gastric epithelium of the pig and its importance in the microecology of the intestine. J Appl Bacteriol 48:147–154. https://doi.org/10.1111/j.1365-2672.1980.tb05216.x
Huang J, Zhang W, Fan R, Liu Z, Huang T, Li J, Du T, Xiong T (2020) Composition and Functional Diversity of Fecal Bacterial Community of Wild Boar, Commercial Pig and Domestic Native Pig as Revealed by 16S rRNA Gene Sequencing. Arch Microbiol 202(4):843–57. https://doi.org/10.1007/s00203-019-01787-w
Li M, Wang Y, Cui H, Li Y, Sun Y, Qiu HJ (2020) Characterization of lactic acid bacteria isolated from the gastrointestinal tract of a wild boar as potential probiotics. Front Vet Sci 7:49. https://doi.org/10.3389/fvets.2020.00049
Zhong Y, Fu D, Deng Z, Tang W, Mao J, Zhu T, Zhang Y, Liu J, Wang H (2022) Lactic acid bacteria mixture isolated from wild pig alleviated the gut inflammation of mice challenged by Escherichia coli. Front Immunol 13:822754. https://doi.org/10.3389/fimmu.2022.822754
FAO/WHO, Guidelines for the Evaluation of Probiotics in Food (2002) Report of a Joint FAO/WHO Working Group on Drafting Guidelines for the Evaluation of Probiotics in Food. London, Ontario, Canada, April 30 and May 1, 2002. Available at https://www.fao.org/3/a0512e/a0512e.pdf
Shokryazdan P, Jahromi MF, Liang JB, Ho YW (2017) Probiotics: From isolation to application. J Am Col Nutr 36:666–676. https://doi.org/10.1080/07315724.2017.1337529
De Melo Pereira GV, de Oliveira Coelho B, Júnior AIM, Thomaz-Soccol V, Soccol CR (2018) How to select a probiotic? A review and update of methods and criteria. Biotechnol Adv 36:2060–2076. https://doi.org/10.1016/j.biotechadv.2018.09.003
Byakika S, Mukisa IM, Byaruhanga YB, Muyanja C (2019) A review of criteria and methods for evaluating the probiotic potential of microorganisms. Food Rev Int 35:427–466. https://doi.org/10.1080/87559129.2019.1584815
Libisch B, Keresztény T, Kerényi Z, Kocsis R, Sipos R, Papp PP, Olasz F (2020) Metagenomic analysis of acquired antibiotic resistance determinants in the gut microbiota of wild boars (Sus scrofa) – preliminary results. J Vet Res 64:111–118. https://doi.org/10.2478/jvetres-2020-0015
Walter J, Hertel C, Tannock GW, Lis CM, Munro K, Hammes WP (2001) Detection of Lactobacillus, Pediococcus, Leuconostoc, and Weissella species in human faeces by using group-specific PCR primers and denaturing gradient gel electrophoresis. Appl Environ Microbiol 67:2578–2585. https://doi.org/10.1128/AEM.67.6.2578-2585.2001
Schillinger U, Boehringer B, Wallbaum S, Caroline L, Gonfa A, Huch Neé Kostinek M, Holzapfel WH, Franz CM (2008) A genus-specific PCR method for differentiation between Leuconostoc and Weissella and its application in identification of heterofermentative lactic acid bacteria from coffee fermentation. FEMS Microbiol Lett 286:222–226. https://doi.org/10.1111/j.1574-6968.2008.01286.x
Lane DJ (1991) 16S/23S rRNA sequencing. In: Stackebrandt E, Goodfellow M (eds) Nucleic acid techniques in bacterial systematics. Wiley, New York, USA, pp 117–175
Altschul S, Gish W, Miller W, Myers E, Lipman D (1990) Basic local alignment search tool. J Mol Biol 215:403–410. https://doi.org/10.1016/S0022-2836(05)80360-2
Schillinger U, Lücke FK (1989) Antibacterial activity of Lactobacillus sake isolated from meat. Appl Environ Microbiol 55:1901–1906. https://doi.org/10.1128/aem.55.8.1901-1906.1989
Bachmann BJ (1972) Pedigrees of some mutant strains of Escherichia coli K-12. Bacteriol Rev 36:525–557. https://doi.org/10.1128/br.36.4.525-557.1972
Német Z, Albert E, Nagy T, Olasz F, Barta E, Kiss J, Dán Á, Bányai K, Hermans K, Biksi I (2015) Draft genome sequence of a highly virulent rabbit Staphylococcus aureus strain. Genome Announc 3:e00461-15. https://doi.org/10.1128/genomeA.00461-15
Lennox ES (1955) Transduction of linked genetic characters of the host by bacteriophage P1. Virology 1:190–206. https://doi.org/10.1016/0042-6822(55)90016-7
Charteris WP, Kelly PM, Morelli L, Collins JK (2001) Gradient diffusion antibiotic susceptibility testing of potentially probiotic Lactobacilli. J Food Prot 64:2007–2014. https://doi.org/10.4315/0362-028X-64.12.2007
Charteris WP, Kelly PM, Morelli L, Collins JK (1998) Antibiotic susceptibility of potentially probiotic Lactobacillus species. J Food Prot 61:1636–1643. https://doi.org/10.4315/0362-028X-61.12.1636
Perreten V, Vorlet-Fawer L, Slickers P, Ehricht R, Kuhnert P, Frey J (2005) Microarray-based detection of 90 antibiotic resistance genes of gram-positive bacteria. J Clin Microbiol 43:2291–302. https://doi.org/10.1128/JCM.43.5.2291-2302.2005
CLSI (2020) Performance standards for antimicrobial disk and dilution susceptibility tests for bacteria isolated from animals. 5th ed. CLSI supplement VET01S. Clinical and Laboratory Standards Institute. http://clsivet.org/dashboard.aspx
Bilková A, Dubničková M, Sepová HK (2013) Antimicrobial susceptibility and immunomodulatory properties of lamb isolate of Lactobacillus mucosae, new probiotic candidate. European Pharmaceutical Journal 60(2):1–6. https://doi.org/10.2478/afpuc-2013-0017
Chen T, Wang L, Li Q, Long Y, Lin Y, Yin Y (2020) Functional probiotics of lactic acid bacteria from Hu sheep milk. BMC Microbiol 20(1):1–12. https://doi.org/10.1186/s12866-020-01920-6
Dashkevicz MP, Feighner SD (1989) Development of a differential medium for bile salt hydrolase-active Lactobacillus spp. Appl Environ Microbiol 55:11–16. https://doi.org/10.1128/aem.55.1.11-16.1989
Guo XH, Kim JM, Nam HM, Park SY, Kim JM (2010) Screening lactic acid bacteria from swine origins for multistrain probiotics based on in vitro functional properties. Anaerobe 16:321–326. https://doi.org/10.1016/j.anaerobe.2010.03.006
Zheng J, Wittouck S, Salvetti E, Franz CMAP, Harris HMB, Mattarelli P, O’Toole PW, Pot B, Vandamme P, Walter J, Watanabe K, Wuyts S, Felis GE, Gänzle MG, Lebeer S (2020) A taxonomic note on the genus Lactobacillus: Description of 23 novel genera, emended description of the genus Lactobacillus Beijerinck 1901, and union of Lactobacillaceae and Leuconostocaceae. Int J Syst Evol Microbiol 70:2782–2858. https://doi.org/10.1099/ijsem.0.004107
Jeon HH, Kim KH, Chun BH, Ryu BH, Han NS, Jeon CO (2017) A proposal of Leuconostoc mesenteroides subsp. jonggajibkimchii subsp. nov. and reclassification of Leuconostoc mesenteroides subsp. suionicum (Gu et al., 2012) as Leuconostoc suionicum sp. nov. based on complete genome sequences. Int J Syst Evol Microbiol 67:2225–2230. https://doi.org/10.1099/ijsem.0.001930
Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M et al (2012) SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol 19:455–477. https://doi.org/10.1089/cmb.2012.0021
Prjibelski A, Antipov D, Meleshko D, Lapidus A, Korobeynikov A (2020) Using SPAdes De Novo Assembler. Current Protocols in Bioinformatics 70:e102. https://doi.org/10.1002/cpbi.102
Hasman H, Saputra D, Sicheritz-Ponten T, Lund O, Svendsen CA, Frimodt-Møller N, Aarestrup FM (2014) Rapid whole-genome sequencing for detection and characterization of microorganisms directly from clinical samples. J Clinical Microbiol 52:139–146. https://doi.org/10.1128/JCM.02452-13
Larsen MV, Cosentino S, Lukjancenko O, Saputra D, Rasmussen S, Hasman H, Sicheritz-Ponten T, Aarestrup FM, Ussery DW, Lund O (2014) Benchmarking of methods for genomic taxonomy. J Clinical Microbiol 52:1529–1539. https://doi.org/10.1128/JCM.02981-13
Clausen PTLC, Aarestrup FM, Lund O (2018) Rapid and precise alignment of raw reads against redundant databases with KMA. BMC Bioinformatics 19:307. https://doi.org/10.1186/s12859-018-2336-6
Darling AE, Mau B, Perna NT (2010) progressiveMauve: multiple genome alignment with gene gain, loss and rearrangement. PLoS One 5:e11147. https://doi.org/10.1371/journal.pone.0011147
Paradis E, Schliep K (2019) ape 5.0: an environment for modern phylogenetics and evolutionary analyses in R. Bioinformatics 35:526–528. https://doi.org/10.1093/bioinformatics/bty633
Jain C, Rodriguez-R LM, Phillippy AM, Konstantinidis KT, Aluru S (2018) High throughput ANI analysis of 90K prokaryotic genomes reveals clear species boundaries. Nat Commun 9:5114. https://doi.org/10.1038/s41467-018-07641-9
Bortolaia V, Kaas RS, Ruppe E, Roberts MC, Schwarz S et al (2020) ResFinder 4.0 for predictions of phenotypes from genotypes. J Antimicrob Chemother 75:3491–3500. https://doi.org/10.1093/jac/dkaa345
Zankari E, Allesøe R, Joensen KG, Cavaco LM, Lund O, Aarestrup FM (2020) PointFinder: a novel web tool for WGS-based detection of antimicrobial resistance associated with chromosomal point mutations in bacterial pathogens. J Antimicrob Chemother 72:2764–2768. https://doi.org/10.1093/jac/dkx217
Camacho C, Coulouris G, Avagyan V, Ma N, Papadopoulos J, Bealer K, Madden TL (2009) BLAST+: architecture and applications. BMC Bioinformatics 10:421. https://doi.org/10.1186/1471-2105-10-421
van Heel AJ, de Jong A, Song C, Viel JH, Kok J, Kuipers OP (2018) BAGEL4: a user-friendly web server to thoroughly mine RiPPs and bacteriocins. Nucl Acids Res 46:W278–W281. https://doi.org/10.1093/nar/gky383
Watanabe M, Kinoshita H, Nitta M, Yukishita R, Kawai Y et al (2010) Identification of a new adhesin-like protein from Lactobacillus mucosae ME-340 with specific affinity to the human blood group A and B antigens. J Appl Microbiol 109:927–935. https://doi.org/10.1111/j.1365-2672.2010.04719.x
Watanabe M, Kinoshita H, Huang IN, Eguchi K, Tsurumi T et al (2012) An adhesin-like protein, Lam29, from Lactobacillus mucosae ME-340 binds to histone H3 and blood group antigens in human colonic mucus. Biosc. Biotechnol Biochem 76:1655–1660. https://doi.org/10.1271/bbb.120150
Rice P, Longden I, Bleasby A (2000) EMBOSS: The European Molecular Biology Open Software Suite. Trends Genet 16:276–277. https://doi.org/10.1016/S0168-9525(00)02024-2
Katoh K, Standley DM (2013) MAFFT multiple sequence alignment software version 7: improvements in performance and usability. Mol Biol Evol 30:772–780. https://doi.org/10.1093/molbev/mst010
Boratyn GM, Camacho C, Cooper PS, Coulouris G, Fong A et al (2013) BLAST: a more efficient report with usability improvements. Nucleic Acids Res. 41:W29–W33. https://doi.org/10.1093/nar/gkt282
Maragkoudakis PA, Zoumpopoulou G, Miaris C, Kalantzopoulos G, Pot B, Tsakalidou E (2006) Probiotic potential of Lactobacillus strains isolated from dairy products. Int Dairy J 16:189–199. https://doi.org/10.1016/j.idairyj.2005.02.009
Jose NM, Bunt CR, Hussain MA (2015) Comparison of microbiological and probiotic characteristics of Lactobacilli isolates from dairy food products and animal rumen contents. Microorg 3:198–212. https://doi.org/10.3390/microorganisms3020198
Jia Y, Yang B, Ross P, Stanton C, Zhang H, Zhao J, Chen W (2020) Comparative genomics analysis of Lactobacillus mucosae from different niches. Genes 11:95. https://doi.org/10.3390/genes11010095
Kaushal G, Singh SP (2020) Comparative genome analysis provides shreds of molecular evidence for reclassification of Leuconostoc mesenteroides MTCC 10508 as a strain of Leu. suionicum. Genomics 112:4023–4031. https://doi.org/10.1016/j.ygeno.2020.06.040
Casarotti SN, Carneiro BM, Todorov SD, Nero LA, Rahal P, Penna ALB (2017) In vitro assessment of safety and probiotic potential characteristics of Lactobacillusstrains isolated from water buffalo mozzarella cheese. Ann Microbiol 67:289–301. https://doi.org/10.1007/s13213-017-1258-2
Gu CT, Wang F, Li CY, Liu F, Huo GC (2012) Leuconostoc mesenteroides subsp. suionicum subsp. nov. Int J Syst Evol Microbiol 62:1548–1551. https://doi.org/10.1099/ijs.0.031203-0
Roos S, Karner F, Axelsson L, Jonsson H (2000) Lactobacillus mucosae sp. nov., a new species with in vitro mucus-binding activity isolated from pig intestine. Int J Syst Evol Microbiol 50:251–258. https://doi.org/10.1099/00207713-50-1-251
Bleckwedel J, Teran LC, Bonacina J, Saavedra L, Mozzi F, Raya RR (2014) Draft genome sequence of the mannitol-producing strain Lactobacillus mucosae CRL573. Genome Announc. 2:e01292-14. https://doi.org/10.1128/genomeA.01292-14
Fakhry S, Manzo N, D’Apuzzo E, Pietrini L, Sorrentini I, Ricca E, De Felice M, Baccigalupi L (2009) Characterization of intestinal bacteria tightly bound to the human ileal epithelium. Res Microbiol 160:817–823. https://doi.org/10.1016/j.resmic.2009.09.009
Pavlova SI, Kilic AO, Kilic SS, So JS, Nader-Macias ME, Simoes JA, Tao L (2002) Genetic diversity of vaginal lactobacilli from women in different countries based on 16S rRNA gene sequences. J Appl Microbiol 92:451–459. https://doi.org/10.1046/j.1365-2672.2002.01547.x
London LE, Price NP, Ryan P, Wang L, Auty MA, Fitzgerald GF, Stanton C, Ross RP (2014) Characterization of a bovine isolate Lactobacillus mucosae DPC 6426 which produces an exopolysaccharide composed predominantly of mannose residues. J Appl Microbiol 117:509–517. https://doi.org/10.1111/jam.12542
de Moraes GMD, de Abreu LR, do Egito AS, Salles HO, da Silva LMF, Nero LA, Todorov SD, dos Santos KMO (2017) Functional properties of Lactobacillus mucosae strains isolated from Brazilian goat milk. Probiotics Antimicrobiol Prot 9:235–245. https://doi.org/10.1007/s12602-016-9244-8
Repally A, Perumal V, Dasari A, Palanichamy E, Venkatesan A (2018) Isolation, identification of Lactobacillus mucosae AN1 and its antilisterial peptide purification and characterization. Probiotics Antimicrobiol Prot 10:775–786. https://doi.org/10.1007/s12602-017-9341-3
Rastogi S, Mittal V, Singh A (2020) In vitro evaluation of probiotic potential and safety assessment of Lactobacillus mucosae strains isolated from donkey’s lactation. Probiotics Antimicro Prot 12:1045–1056. https://doi.org/10.1007/s12602-019-09610-0
Ksiezarek M, Grosso F, Ribeiro TG, Peixe L (2022) Genomic diversity of genus Limosilactobacillus. Microb Genom 8:000847. https://doi.org/10.1099/mgen.0.000847
Lee JH, Valeriano VD, Shin YR, Chae JP, Kim GB, Ham JS, Chun J, Kang DK (2012) Genome sequence of Lactobacillus mucosae LM1, isolated from piglet feces. J Bacteriol 194:4766. https://doi.org/10.1128/JB.01011-12
Valeriano VD, Parungao-Balolong MM, Kang DK (2014) In vitro evaluation of the mucin-adhesion ability and probiotic potential of Lactobacillus mucosae LM1. J Appl Microbiol 117:485–497. https://doi.org/10.1111/jam.12539
Valeriano VD, Bagon BB, Balolong MP, Kang DK (2016) Carbohydrate-binding specificities of potential probiotic Lactobacillus strains in porcine jejunal (IPEC-J2) cells and porcine mucin. J Microbiol 54:510–519. https://doi.org/10.1007/s12275-016-6168-7
Valeriano VDV, Oh JK, Bagon BB, Kim H, Kang DK (2019) Comparative genomic analysis of Lactobacillus mucosae LM1 identifies potential niche-specific genes and pathways for gastrointestinal adaptation. Genomics 111:24–33. https://doi.org/10.1016/j.ygeno.2017.12.009
Pajarillo EAB, Kim SH, Valeriano VD, Lee JY, Kang DK (2017) Proteomic view of the crosstalk between Lactobacillus mucosae and intestinal epithelial cells in co-culture revealed by Q exactive-based quantitative proteomics. Front Microbiol 12:2459. https://doi.org/10.3389/fmicb.2017.02459
Bagon BB, Oh JK, Valeriano VDV, Pajarillo EAB, Kang DK (2021) Exploring the bile stress response of Lactobacillus mucosae LM1 through exoproteome analysis. Molecules 26:5695. https://doi.org/10.3390/molecules26185695
Zhang Q, Vasquez R, Yoo JM, Kim SH, Kang DK, Kim IH (2022) Dietary supplementation of Limosilactobacillus mucosae LM1 enhances immune functions and modulates gut microbiota without affecting the growth performance of growing pigs. Front Vet Sci 9:918114. https://doi.org/10.3389/fvets.2022.918114
Bilkova A, Kinova Sepova H, Bukovsky M, Bezakova L (2011) Antibacterial potential of lactobacilli isolated from a lamb. Veterinarni Medicina 56:319-324. https://doi.org/10.17221/1583-VETMED
Chun BH, Lee SH, Jeon HH, Kim DW, Jeon CO (2017) Complete genome sequence of Leuconostoc suionicum DSM 20241T provides insights into its functional and metabolic features. Stand Genomic Sci 12:38. https://doi.org/10.1186/s40793-017-0256-0
Raimondi S, Candeliere F, Amaretti A, Costa S, Vertuani S, Spampinato G, Rossi M (2022) Phylogenomic analysis of the genus Leuconostoc. Front Microbiol 13: 897656. https://doi.org/10.3389/fmicb.2022.897656
Abriouel H, Casado Muñoz MDC, Lavilla Lerma L, Pérez Montoro B, Bockelmann W, Pichner R, Kabisch J, Cho GS, Franz CMAP, Gálvez A, Benomar N (2015) New insights in antibiotic resistance of Lactobacillus species from fermented foods. Food Res Int 78:465–481. https://doi.org/10.1016/j.foodres.2015.09.016
Campedelli I, Mathur H, Salvetti E, Clarke S, Rea MC, Torriani S, Ross RP, Hill C, O’Toole PW (2018) Genus-wide assessment of antibiotic resistance in Lactobacillus spp. Appl Environ Microbiol 85:e01738-18. https://doi.org/10.1128/AEM.01738-18
Flórez AB, Campedelli I, Delgado S, Alegría Á, Salvetti E, Felis GE, Mayo B, Torriani S (2016) Antibiotic susceptibility profiles of dairy Leuconostoc, analysis of the genetic basis of atypical resistances and transfer of genes in vitro and in a food matrix. PLoS One 11:e0145203. https://doi.org/10.1371/journal.pone.0145203
Aucher W, Simonet V, Fremaux C, Dalet K, Simon L, Cenatiempo Y, Frère J, Berjeaud JM (2004) Differences in mesentericin secretion systems from two Leuconostoc strains. FEMS Microbiol Lett 232:15–22. https://doi.org/10.1016/S0378-1097(04)00011-4
Morisset D, Frere J (2002) Heterologous expression of bacteriocins using the mesentericin Y105 dedicated transport system by Leuconostoc mesenteroides. Biochimie 84:569–576. https://doi.org/10.1016/S0300-9084(02)01413-X
Fremaux C, Héchard Y, Cenatiempo Y (1995) Mesentericin Y105 gene clusters in Leuconostoc mesenteroides Y105. Microbiology 141:1637–45. https://doi.org/10.1099/13500872-141-7-1637
Jeffery CJ (2009) Moonlighting proteins—An update. Mol Biosyst 5:345–350. https://doi.org/10.1039/B900658N
Nishiyama K, Sugiyama M, Mukai T (2016) Adhesion properties of lactic acid bacteria on intestinal mucin. Microorganisms 4:34. https://doi.org/10.3390/microorganisms4030034
Long SL, Gahan CGM, Joyce SA (2017) Interactions between gut bacteria and bile in health and disease. Mol Aspects Med 56:54–65. https://doi.org/10.1016/j.mam.2017.06.002
Islam KB, Fukiya S, Hagio M, Fujii N, Ishizuka S, Ooka T, Ogura Y, Hayashi T, Yokota A (2011) Bile acid is a host factor that regulates the composition of the cecal microbiota in rats. Gastroenterology 141:1773–1781. https://doi.org/10.1053/j.gastro.2011.07.046
Bateup JM, McConnell MA, Jenkinson HF, Tannock GW (1995) Comparison of Lactobacillus strains with respect to bile salt hydrolase activity, colonization of the gastrointestinal tract, and growth rate of the murine host. Appl Environ Microbiol 61:1147–1149. https://doi.org/10.1128/aem.61.3.1147-1149.1995
Grill JP, Cayuela C, Antoine JM, Schneider F (2000) Isolation and characterization of a Lactobacillus amylovorus mutant depleted in conjugated bile salt hydrolase activity: relation between activity and bile salt resistance. J Appl Microbiol 89:553–563. https://doi.org/10.1046/j.1365-2672.2000.01147.x
de Smet I, Van Hoorde L, Vande Woestyne M, Christiaens H, Verstraete W (1995) Significance of bile salt hydrolytic activities of lactobacilli. J Appl Bacteriol 79:292–301. https://doi.org/10.1111/j.1365-2672.1995.tb03140.x
Jones BV, Begley M, Hill C, Gahan CGM, Marchesi JR (2008) Functional and comparative metagenomic analysis of bile salt hydrolase activity in the human gut microbiome. Proc Natl Acad Sci 105:13580–13585. https://doi.org/10.1073/pnas.0804437105
Begley M, Hill C, Gahan CG (2006) Bile salt hydrolase activity in probiotics. Appl Environ Microbiol 72:1729–1738. https://doi.org/10.1128/AEM.72.3.1729-1738.2006
Bernstein C, Holubec H, Bhattacharyya AK, Nguyen H, Payne CM, Zaitlin B, Bernstein H (2011) Carcinogenicity of deoxycholate, a secondary bile acid. Arch Toxicol 85:863–871. https://doi.org/10.1007/s00204-011-0648-7
O’Keefe SJ, Li JV, Lahti L, Ou J, Carbonero F, Mohammed K et al (2015) Fat, fibre and cancer risk in African Americans and rural Africans. Nat Commun 6:6342. https://doi.org/10.1038/ncomms7342
Yoshimoto S, Loo TM, Atarashi K, Kanda H, Sato S, Oyadomari S, Iwakura Y, Oshima K, Morita H, Hattori M, Honda K, Ishikawa Y, Hara E, Ohtani N (2013) Obesity-induced gut microbial metabolite promotes liver cancer through senescence secretome. Nature 499:97–101. https://doi.org/10.1038/nature12347
Labbé A, Ganopolsky JG, Martoni CJ, Prakash S, Jones ML (2014) Bacterial bile metabolising gene abundance in Crohn’s, ulcerative colitis and type 2 diabetes metagenomes. PLoS One 9:e115175. https://doi.org/10.1371/journal.pone.0115175
Tanaka H, Doesburg K, Iwasaki T, Mierau I (1999) Screening of lactic acid bacteria for bile salt hydrolase activity. J Dairy Sci 82:2530–2535. https://doi.org/10.3168/jds.S0022-0302(99)75506-2
O’Flaherty S, Briner Crawley A, Theriot CM, Barrangou R (2018) The Lactobacillus bile salt hydrolase repertoire reveals niche-specific adaptation. mSphere 3: e00140-18. https://doi.org/10.1128/mSphere.00140-18
McAuliffe O, Cano RJ, Klaenhammer TR (2005) Genetic analysis of two bile salt hydrolase activities in Lactobacillus acidophilus NCFM. Appl Environ Microbiol 71:4925–4929. https://doi.org/10.1128/AEM.71.8.4925-4929.2005
Lambert JM, Bongers RS, de Vos WM, Kleerebezem M (2008) Functional analysis of four bile salt hydrolase and penicillin acylase family members in Lactobacillus plantarum WCFS1. Appl Environ Microbiol 74:4719–4726. https://doi.org/10.1128/AEM.00137-08
Fang F, Li Y, Bumann M, Raftis EJ, Casey PG, Cooney JC, Walsh MA, O’Toole PW (2009) Allelic variation of bile salt hydrolase genes in Lactobacillus salivarius does not determine bile resistance levels. J Bacteriol 191:5743–5757. https://doi.org/10.1128/JB.00506-09
Chae JP, Valeriano VD, Kim GB, Kang DK (2013) Molecular cloning, characterization and comparison of bile salt hydrolases from Lactobacillus johnsonii PF01. J Appl Microbiol 114:121–133. https://doi.org/10.1111/jam.12027
Lambert JM, Siezen RJ, de Vos WM, Kleerebezem M (2008) Improved annotation of conjugated bile acid hydrolase superfamily members in Gram-positive bacteria. Microbiology 154:2492–2500. https://doi.org/10.1099/mic.0.2008/016808-0
Acknowledgements
The Gróf István Károlyi Hunting Party (Füzérkomlós, Hungary) is acknowledged for providing permission to sample the hunted wild boars in the Zemplén Mountains, Hungary. We are thankful to Ilona Könczölné-Keresztúri and Andrea Bogár for the excellent technical assistance. We are also thankful to Vincent Perreten for providing Staphylococcus haemolyticus VPS617 and to Zoltán Német for providing Staphylococcus aureus SP17 used as reference strains.
Funding
Open access funding provided by Hungarian University of Agriculture and Life Sciences. This research was funded by the Hungarian National Research, Development and Innovation Office, grant number TKP2020-NKA-24 (F.O.); the European Commission through the NeoGiant Horizon 2020 project with Grant Agreement ID 101036768 (K.P.); the Hungarian National Laboratory Project, grant number RRF-2.3.1-21-2022-00007 (K.P.); the Hungarian National Research, Development and Innovation Office, grant numbers NKFI K 132687 (F.O.) and 2019-2.1.11-TÉT-2020-00141 (B.L.) T.K. was supported by the PhD fellowship of Hungarian University of Agriculture and Life Sciences, Doctoral School of Biology, Gödöllő, Hungary. S.C was supported by the PhD fellowship of the Stipendium Hungaricum scholarship of the Hungarian Government at the Hungarian University of Agriculture and Life Sciences, Doctoral School of Biology, Gödöllő, Hungary.
Author information
Authors and Affiliations
Contributions
Conceptualization, Péter P. Papp, Ferenc Olasz and Tibor Keresztény; Methodology: Péter P. Papp, Ferenc Olasz, Tibor Nagy and Tibor Keresztény; Formal analysis and investigation: Tibor Keresztény, Balázs Libisch, Péter P. Papp, Tibor Nagy, Ferenc Olasz, Stephanya Corral Orbe, Zoltán Kerényi, Róbert Kocsis, and Katalin Posta; Writing-original draft preparation: Péter P. Papp, Ferenc Olasz and Tibor Nagy; Writing- review and editing: Tibor Keresztény, Péter P. Papp, Ferenc Olasz, and Katalin Posta; Funding acquisition: Ferenc Olasz, Balázs Libisch and Katalin Posta; Supervision: Katalin Posta, Péter P. Papp and Ferenc Olasz.
Corresponding author
Ethics declarations
Consent for Publication
All authors have read and approved the final manuscript.
Conflicts of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Keresztény, T., Libisch, B., Orbe, S.C. et al. Isolation and Characterization of Lactic Acid Bacteria With Probiotic Attributes From Different Parts of the Gastrointestinal Tract of Free-living Wild Boars in Hungary. Probiotics & Antimicro. Prot. (2023). https://doi.org/10.1007/s12602-023-10113-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s12602-023-10113-2