Abstract
A number of studies have reported that zinc plays a substantial role in the development of metabolic syndrome, taking part in the regulation of cytokine expression, suppressing inflammation, and is also required to activate antioxidant enzymes that scavenge reactive oxygen species, reducing oxidative stress. Zinc also plays a role in the correct functioning of lipid and glucose metabolism, regulating and forming the expression of insulin. In numerous studies, zinc supplementation has been found to improve blood pressure, glucose, and LDL cholesterol serum level. Deeper knowledge of zinc’s properties may help in treating metabolic syndrome, thus protecting against stroke and angina pectoris, and ultimately against death.
Similar content being viewed by others
Introduction
Zinc (Zn) is one of the most common trace elements in the human body and plays a substantial role in growth and development, acting as a signaling factor [1]. This metal takes part in the regulation of chronic inflammatory status through the reduction of inflammatory cytokines. Zinc also reduces oxidative stress by participating in the synthesis of antioxidant enzymes and acts as a catalyzer of enzymes, taking part in lipid, carbohydrate, and protein metabolism. It is involved in the synthesis, storage, and release of insulin, which suggests the critical role of this microelement in the progression of type-2 diabetes mellitus, atherosclerosis, and metabolic syndrome (MS) [2,3,4,5].
Studies of zinc concentration in the human body are scarce, and have shown inconsistent results. Zinc deficiency has been observed in patients in some counties with increased oxidative stress and generation of inflammatory status and the decrease concentrations of this element occur in patients with MS [3], in patients with type 2 diabetes mellitus [6] and with hypertension [7] than in healthy people.
Some studies showed that high concentration of zinc is associated with impaired lipid profile and risk of MS [8,9,10]. In the last study, increase in erythrocyte zinc concentration and high zincuria was observed in patients with MS [11]. Obtained results indicate that zinc is strongly associated with oxidation stress, inflammation, and lipid and glucose status and it can be assumed that zinc status may be a predictor of metabolic disorders.
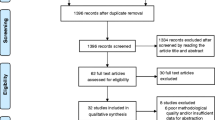
Taking together, current knowledge reflects the need for a critical overview of the zinc role in metabolic disorders. The proposed review summarizes the advances of the last years (2010–2017), providing new insights into the association between zinc status and inflammation, oxidative stress, lipid, and glucose metabolism.
Zinc status in metabolic disorders
Multiple studies have demonstrated the interaction between obesity and Zn homeostasis. In particular, blood Zn levels were found to be significantly decreased in obese patients [12, 13]. Erythrocyte Zn levels were also shown to be negatively associated with anthropometric markers of obesity like BMI and waist circumference [14]. At the same time, the decrease in serum Zn levels was accompanied by increased urinary concentrations, being indicative of increased Zn excretion in obesity [15]. Low nutritional Zn status in obesity is also associated with aggravation of obesity-related metabolic disturbances like insulin resistance, inflammation, and altered lipid profile [16].
Similarly, short-term (8-week) weight loss in obese women was associated with a significant improvement of serum Zn levels, being negatively associated with body fat percentage [17].
The role of Zn dyshomeostasis in obesity is also confirmed by the results of supplementation trials. In particular, administration of 30 mg/day Zn gluconate for 1 month resulted in a significant decrease in body weight and BMI values as well as serum TG concentrations [18]. Eight-week treatment with 20 mg/day zinc also resulted in a significant decrease in BMI and BMI z score in obese children, although remaining abnormally high. At the same time, Zn supplementation was also associated with improvement of lipoprotein profile (decreased ApoB/ApoA1, oxLDL, total cholesterol and LDL-cholesterol values) and reduced leptin levels [19].
It is also suggested that zinc deficiency may be an important risk factor of diabetes mellitus II. In several studies, decreased concentration of zinc status was observed in diabetic patients compared to healthy people [20,21,22,23,24,25,26]. Sinha et al. [20] have demonstrated that zinc plasma levels are inversely correlated with glycemic status (HbA1C) in diabetes mellitus, while in patients with MS an association between high zinc concentration in urine (zincuria) and fasting glucose level, glycated hemoglobin level, insulin resistance, and also CRP were found. In one study, inadequate zinc intake was observed and zinc deficiency was suggested in patients with MS [27]. The relation between inadequate zinc intake and raised insulin concentration in blood was also noticed in adolescents [28]. Some recent studies showed that zinc supplementation improved glucose metabolism and insulin sensitivity in diabetic patients [29,30,31]. It was also found that zinc supplementation reduced fasting plasma glucose, serum insulin and insulin resistance in gestational diabetes in women [32]. However, in other studies, the association between zinc supply and glucose metabolism and insulin resistance was not confirmed [18, 33].
In our opinion, the association between metabolic disorders and zinc status is mainly mediated by inflammation, oxidative stress, modulation of zinc transporters, and altered lipid and glucose metabolism.
Inflammation
A significant decrease in zinc levels in obese population with inflammatory state was observed. According to research, it increases risk of the development of obesity-related complications. It has been mentioned that zinc takes part in the regulation of proinflammatory cytokines expression through many mechanisms (Fig. 1) [34].
The influence of zinc on oxidative stress and inflammation. Zinc prevents the generation of reactive oxygen species through a number of mechanisms. Zn is a cofactor of Cu,Zn-SOD, which catalyzes the dismutation of superoxide. It up-regulates Nrf2, being the principal regulator of antioxidant system functioning, thus increasing GSH synthesis, GPx activity, and other mechanisms of detoxification. Zinc also affects the generation of reactive oxygen species through modulation of prooxidant pathways. Zn-induced decrease in NADPH oxidase activity results in decreased superoxide production. Through induction of metallothionein synthesis, Zn may decrease the availability of redox metals and their participation in Fenton reaction. Susceptibility of proteins to free radical oxidation is also inhibited by zinc through protection of thiol groups. Zn-induced inhibition of redox-sensitive proinflammatory transcription factors is accompanied by decreased production of proinflammatory cytokines, enzymes, and adhesion molecules, thus resulting in the prevention of inflammatory response
During inflammatory state, white adipose tissue produces cytokines such as (interleukin-6) IL-6, which stimulates the secretion of C-reactive protein (CRP) in the liver, which is a sensitive marker of inflammation, tissue damage, and impairs vascular endothelial function. On the other hand, TNF-α contributes to the acute-phase response by enabling IL-6, which increases proinflammatory cytokines such as adiponectin [35]. In a double-blinded, placebo trial in elderly subjects, Bao et al. [27] have shown a significant increase in plasma zinc levels, a decrease in CRP, TNF-α, and Il-6 plasma concentrations in a response of the zinc supplementation. While different studies have shown the inverse association between IL-6, TNF-α, CRP, and serum zinc levels in adults aged 40 [36]. According to the authors, zinc supplementation positively impacts inflammatory state reduction in obese patients with metabolic syndrome. Also, in type 2 diabetes mellitus patients, impaired zinc homeostasis leads to uncontrolled expression of immune mediators, such as IL-1β, IL-6, and NF-κB, which at the same time simultaneously exacerbate the immune response and lead to pathogenesis, negatively affecting β-cells. The long-term exposure of β-cells to IL-1β and IL-6 may lead to apoptosis, resulting in insulin resistance and increased glucose levels in the blood [37].
NF-κB is one of the major immune response transcription factors in the development of atherosclerosis [35]. This inflammatory pathway takes part in the expression of pro-inflammatory cytokines, CRP, MMPs, and controls genes, which regulate proliferation, apoptosis, cell adhesion, tissue remodeling, inflammatory processes, immune responses, and cellular-stress responses [38]. Some authors have shown that zinc ions lead to signal transduction, thus making zinc involved in NF-κB inhibition [34]. Another negative impact of zinc regarding NF-κB activity appears through inhibition of lipopolysaccharide-induced activation of NF-κB, which in the same time suppresses TNF-α secretion in monocytes [39]. Also, zinc ions imported to macrophages or monocytes by ZIP8 (zinc transporter) during inflammatory state provokes NF-κB inhibition [40]. It seems that ZIP8 plays a crucial role in inflammation.
The main negative regulator of NF-κB activity is zinc finger protein (A20), which is known as a cell protector against TNF-α-induced NF-κB toxicity, decreasing its level, along with IL-1β. Prasad et al. [41] have demonstrated that this zinc–protein complex suppress TNF-α and IL-1β production, inhibiting the activity of NF-κB in endothelial cells. It has been reported that zinc supplementation reduces the level of these cytokines, reactive oxygen species (ROS), and polysaccharides by increasing the concentration of A20 and PPAR-α. Zinc influences the expression of peroxisome proliferator-activated receptors α (PPARs-α), which plays a significant role in lipoprotein and glucose metabolism. These receptors also suppress NF-κB activity. The inhibition of NF-κB by zinc via A20 and PPARs signaling pathways are the most important mechanism because zinc decreases pro-inflammatory cytokines in atherosclerosis [35].
Zinc also plays a key role in regulating the function of MMP2 and MMP9 named gelatinases whose expression increases during inflammation with artery damage. They belong to the group of zinc-dependent matrix metalloproteinases (MMPs), which bind zinc ions to the catalytic site for their activation, forming coenzymes. MMPs cause the degradation of various components of ECM and they mediate its remodeling, which enables cell migration, and facilitates the pathogenesis processes. Thus, they play an important role in immunity and angiogenesis, whereby their dysregulation may contribute to inflammation or atherosclerosis [42, 43]. Jagadeesha et al. [44] have reported that the activation of zinc-dependent endopeptidase MMP9 enables cell migration, while other authors have shown significant increasing of the MMP9 serum levels and lower zinc concentration in patients with unstable atherosclerotic plaque [45]. According to research, high MMP9 serum concentrations may increase the risk of atherosclerosis. Instead, some studies have revealed that zinc supplementation with a high-fat diet inhibits MMP2 and MMP9, decreases the inflammatory state, and lowers TG, LDL, IL-6, and CRP and increases HDL, as well as protecting the liver in rabbits [46]. Obtained results highlight the protective role of zinc against artery damage and atherosclerosis.
Oxidative stress
Oxidative stress plays a significant role in MS development, being tightly associated with inflammation, and providing a link between certain MS components like obesity, diabetes, dyslipidemia, and hypertension. Moreover, recent studies proposed that oxidative stress may be considered as one of the components of MS [47].
Physiological concentration of zinc inhibits the production of reactive oxygen species, such as superoxide anion (·O−), hydrogen peroxide (H2O2), and radical hydroxyl (OH·) [48] as well as reactive nitrogen species including peroxynitrite (Fig. 1) [49]. The antioxidant effect of zinc may be mediated through direct action of zinc ion, its structural role in antioxidant proteins, and modulation metallothionein induction. Direct antioxidant activity of Zn ions is associated with its binding to thiol groups, thus protecting them from oxidation [50, 51].
Zinc is a cofactor of antioxidant enzyme Cu,Zn-superoxide dismutase (SOD1), which is suppressed under Zn-deficient conditions [52]. It has also been demonstrated that Zn may indirectly affect the activity of other antioxidant enzymes. In particular, Zn supplementation significantly increased GPx activity through modulation of Se status [53]. It has also been demonstrated that nanoformulated Cu,Zn-SOD is capable of decreasing adipose tissue [54] and vascular [55] inflammation in obese mice.
According to Manea et al. [56], the inhibition of NF-κB, in whose regulation zinc plays a critical role, holds up the expression of NOX1 and NOX4, which play an important role in redox status determination in blood vessels. They cause damage to vessels through by increasing the number of thrombins, causing NOX activation and elevated production of ROS, which leads to DNA and lipid oxidation, concurring to atherosclerosis [57], which has also been confirmed in Jagadeesha et al.’s [44] research. It is also notable that free zinc deficiency contributes to the inhibition of the N-methyl-d-aspartate receptor (NMDAR), which leads to an increased level of ROS [35, 58,59,60].
As stated earlier, Zn-dependent modulation of the antioxidant system is at least partially mediated by its influence on transcription factors. Nuclear factor erythroid 2-related factor 2 (Nrf2) is one of the key transcription factors regulating antioxidant system activity. It protects against oxidative stress at an early stage, scavenging reactive oxygen and nitrogen species, while zinc regulates its expression and transcription [58]. Li et al. [58] have demonstrated that zinc deficiency suppresses Nrf2 activity in diabetes-induced renal oxidative damage in mice. The intracellular concentration of zinc is partly regulated through MTs and closely linking the redox status of the cell to cellular availability of zinc ions [61].
It has been demonstrated that obesity-associated induction of MT expression in adipose tissue is a protective response, being at least partially mediated through modulation of oxidative and endoplasmic reticulum stress [62]. However, another group of authors has linked increased adipose tissue MT expression with the rate of insulin resistance [61]. Corresponding to the earlier-discussed role of Zn in MT synthesis, Zn intake and Zn status in obese patients were significantly associated with peripheral blood mononuclear cell MT levels [16]. Experimental studies have also demonstrated the impact of Zn status on antioxidant systems in obesity. In particular, Chen et al. [63] have assessed the effect of zinc deficiency and zinc supplementation on antioxidant expression in high-fat diet mice, inducing vascular inflammation and oxidative stress, demonstrating that zinc insufficiency exacerbates antioxidant expression, whereas zinc supplementation improves that expression.
It is worth mentioning that zinc does not always act as an antioxidant. In terms of high intracellular zinc levels, it can possess prooxidant properties. In particular, it has been demonstrated that zinc oxide nanoparticles significantly increased oxidative stress in 3T3-L1 adipocytes in a dose-dependent manner [64], although increasing the expression of antioxidant enzymes [65].
Some studies have demonstrated a tight interaction between metabolic syndrome and its components and the activity of Zn-dependent antioxidant systems. In particular, low serum SOD activity and zinc intake were shown to be associated with an incidence of MS in Shanghai, China [66].
Taheri et al. [67] reported decreasing activities of SOD and increases in GSH-Px (glutathione peroxide) and GR activities in diabetic patients. Correspondingly, serum Zn and SOD levels are significantly inversely correlated with HbA1c levels [68]. Hayens et al. [61] and Ogawa et al. [48] have demonstrated an elevated concentration of metallothionein 2a gene expression in diabetes individuals [61] and rats [48]. In contrast, Bellomo et al. [60] reported decreases in MT mRNA levels in response to high glucose concentration in β-cells in a mice model. Numerous experimental studies have demonstrated that Zn supplementation causes increased MT expression [69, 70]. However, it has been noted that in type 2 diabetics with normal Zn status, supplementation did not improve oxidative status and glucose metabolism [71].
Cu,Zn-SOD was also shown to play a significant role in altered lipid profile in diabetic patients [72]. Decreased activity of Cu,Zn-SOD in relation to Zn-deficiency was observed in hypertensive patients. Certain studies have demonstrated increased SOD activities in metabolic syndrome and its components. In particular, Vávrova et al. [73] have shown altered antioxidant enzymes levels in patients with metabolic syndrome, including significantly increased Cu,Zn-SOD and glutathione reductase (GR) activities, and lower activities of CAT and PON1 (paraoxonase) in association with low GSH levels. Similarly, erythrocyte SOD activity was increased in type 2 diabetics, being significantly associated with Zn levels and glycemic control. The authors state that the increased enzyme activity is a response to counteract oxidative stress in terms of adequate zinc supply [74].
Therefore, zinc has a protective potential against metabolic syndrome-associated oxidative stress through induction of transcription factors (including (ARE)-Nrf2 signaling) and a subsequent up-regulation of enzymatic and non-enzymatic antioxidants, induction of metallothionein synthesis, its structural role in Cu,Zn-SOD (SOD1), and, finally, its direct antioxidant activity. It seems that metabolic stress during obesity and metabolic syndrome induces a compensatory response, being characterized by increased Zn-mediated mechanisms of antioxidant protection. However, in terms of poor Zn status due to increased Zn excretion or insufficient intake, their mechanisms may not be activated, resulting in aggravation of metabolic disturbances.
Lipid metabolism
Adipose tissue is the main depot of the lipids in the human organism and expanded adipose tissue mass due to overaccumulation of lipids is the morphological substrate of obesity. Therefore, a tight interaction between Zn and adipose tissue dysfunction is of particular interest. Numerous studies have indicated an association between serum zinc levels and lipid metabolism [75]. In clinical and experimental studies, it has been reported that zinc supplementation results in the total cholesterol, LDL cholesterol, and triglycerides decreasing, and the HDL cholesterol increasing in patients [29, 52]. Instead, Weigand and Egenolf [76] have shown that moderate zinc deficiency did not alter lipid concentration and fatty acid composition in the liver of rats fed a high-fat diet. In other studies, zinc deficiency exacerbates hepatic lipid metabolism, while Zn supplementation increases hepatocyte activity and improves lipid metabolism in the liver [77, 78]. Moreover, short-term zinc supplementation in obese patients decreases weight and TG levels without significant change in lipid and glucose profile [18, 79, 80].
Numerous studies have demonstrated that the state of adipose tissue in obesity and other pathologies is tightly associated with Zn status. Experimental studies have demonstrated a significant decrease in adipose tissue Zn content and its negative correlation with insulin, HOMA-IR, and TNF-α values in obese animals [81]. A significant decrease in adipose tissue Zn levels was detected in animals fed both Zn-adequate and Zn-deficient high-fat diets. At the same time, dietary Zn deficiency in overfed animals resulted in a significant increase in serum leptin levels, being accompanied by a more intensive macrophage infiltration as compared to the HFD-Zn-adequate group [82]. In opposite, other studies showed that a high-fat diet significantly elevated the zinc level in plasma in rats [83].
It seems that Zn does not passively react to the changes in adipose tissue mass. Although being rather contradictory, the existing data demonstrate that the metabolic effects of Zn in obesity may be associated with its interference with leptin production.
Experimental studies demonstrate that adequate adipose tissue Zn status is required for normal adipocyte functioning and leptin synthesis to provide a leptin-mediated negative feedback. Taking into account the fact that Zn supplementation was associated with a further increase of serum leptin levels in obese leptin-resistant subjects, being accompanied by improvement of weight and metabolic parameters, one can propose that Zn may also decrease the rate of leptin resistance. At the same time, Baltaci and Mogulkoc have proposed that leptin may act as a possible link between zinc and immunity [84].
Zinc has a significant impact on other adipokines. In particular, it has been demonstrated that Zn stimulates oligomerization of higher molecular weight forms of adiponectin through modulation of disulfide bond formation [85]. These findings are in agreement with the clinical observation of a positive correlation between serum Zn and adiponectin levels in obese patients with polycystic ovary syndrome [86]. Moreover, 50 mg/day of Zn supplementation for 12 weeks in obese examinees was associated with a significant more than twofold increase in serum adiponectin concentration [87].
Zinc-α 2-glycoprotein (ZAG), a novel adipokine, was shown to be inhibited by a high-fat diet and obesity, inflammatory stimuli (TNF α), glucocorticoid receptor antagonists, eicosapentaenoic acid, and β3-adrenoceptor antagonists, whereas glucocorticoids, cancer cachexia, and β3-agonists increase ZAG production [88]. The physiological effect of ZAG in adipose tissue is related to regulation of lipid metabolism. In particular, ZAG decreases fatty acid synthase (FAS), acetyl-coenzyme A carboxylase 1 (ACC1), acyl-coenzyme A: diacylglycerol transferase 1 (DGAT1), and increases hormone-sensitive lipase (HSL) activity, resulting in increased lipolysis and decreased lipogenesis in murine adipose tissue [89]. Antiobesity effect was confirmed by Russell et al. [90], who reported that decreasing the concentration of ZAG induces lipolysis, which manifests as increasing glycerol levels in rat plasma. They have also demonstrated elevated lipid utilization as a result of decreasing TG levels [90, 91]. According to Yang et al. [92], ZAG is also correlated with insulin resistance. These authors have found lower levels of this adipokine in obese patients with type 2 diabetes mellitus. Inverse associations between insulin resistance, obesity, leptin mRNA, and ZAG mRNA levels have also been found by Mracek et al. [93], who assumed that ZAG has a protective affect against obesity, and as a consequence, against metabolic syndrome, too. Mracek et al. [94] have also revealed that TNFα exhibits a repressive effect on ZAG expression in differentiated adipocytes, which suggests that inflammation exacerbates ZAG operation. Zhu et al. [95] have confirmed that, in hypertensive patients, the ZAG level decreases and the TNFα level increases at the same time. Russell et al. [90] have documented lipolytic activity of ZAG and reductions in body fat mass during treatment of mice for 15 days with ZAG. The effects of ZAG on adipose tissue metabolism may also be mediated through a positive influence on adiponectin expression [96]. Taking into account the presence of zinc-binding sites on zinc-α 2-glycoprotein molecule and its role in adipose tissue physiology [97], one can propose that ZAG may mediate at least a part of the effects of Zn in obesity. Figure 2 shows the schematic diagram of ZAG function in adipose tissues.
Functions of ZAG in adipose tissue. Expression of ZAG is down- or up-regulated by the negative or positive stimuli. In adipose tissue, ZAG inhibits FAS and ACC1 activity, thus resulting in decreased fatty acid synthesis. Lower level of free fatty acids together with ZAG-induced increase in adiponectin expression may significantly reduce insulin resistance. Depression of DGAT1 activity suppresses triglyceride synthesis. Together with up-regulation of HSL the latter results in lower lipid deposition in adipose tissue
The targets for Zn-mediated impact on energy metabolism may include PPARs (proliferator-activated receptors), which are responsible for the expression of mRNA genes that play a critical role in energy metabolism [98, 99]. Three types of PPAR can be singled out: PPARα, PPARβ/δ, and PPARγ. PPARα and PPARβ/δ are mainly responsible for regulation of fatty acid degradation, whereas PPARγ takes part in lipid storage, regulates adipocyte differentiation, and enhances adipogenesis and insulin sensitivity [100,101,102,103,104]. The significant role of zinc in the zinc-finger protein as part of the proper functioning of PPARs has been confirmed by the research of Zhou et al. [101].
The observed interactions between Zn status and adipokine production are dependent on the functional state of the cell. In particular, certain studies have indicated that modulation of Zn levels has a significant impact on adipose tissue differentiation. A recent study demonstrated that zinc oxide (ZnO)-treatment (1–4 mg/l) upregulated PPARγ, FABP4, C/EBPα, and SREBP1 mRNA expression and stimulated lipid accumulation in adipocytes during adipogenesis [105]. Similar findings were obtained for zinc-chelated vitamin C [106]. In contrast, Justus et al. [107] have shown that zinc deficiency does not exacerbate PPARγ gene expression in rats. At the same time, certain studies demonstrated that ZnO nanoparticles (> 10 µg/ml) may be toxic to adipose tissue-derived mesenchymal stem cells, decreasing cell viability through induction of apoptosis [108].
The impact of Zn on adipocyte differentiation may be related to the functioning of various Zn-containing proteins that have been recognized as early regulators of adipogenesis [109]. In particular, it has been demonstrated that Zn-finger protein ZNF638 is induced at early stages of adipocyte differentiation and stimulates adipogenesis through C/EBPs and subsequent up-regulation of PPARy. In turn, ZNF638 knockdown inhibits adipogenesis [110]. Another Zn-finger protein, Zfp423, was also shown to be the factor stimulating adipocyte differentiation acting via stimulation of PPARy expression. It is also notable that Zfp423 deficiency is associated with impairment of both white and brown adipose tissue development [111]. Zfp467 stimulates progenitor cell differentiation from osteoblastic to adipocyte lineage, increasing PPARy, C/EBPa, adiponectin and resistin expression [112]. At the same time, Zfp467 suppression stimulated osteoblast commitment and alleviated osteoporosis, being characterized by specific changes of adipogenic and osteogenic marker proteins [113]. In turn, Zfp521 acts as a negative regulator of adipogenesis at least partially through inhibition of Zfp423 expression [114]. Other Zn-finger proteins involved in regulation of adipocyte determination and differentiation include Znf395, Shn-2, GATA proteins, SLUG, Egr2/Egr1, ZBTB16, YY1, and Krüppel-like factors [115].
Zinc and insulin secretion
Zinc is an essential trace element required for the normal synthesis, storage and secretion of insulin in pancreatic β-cells. It has been reported in a recent study that the depletion of zinc negatively impacts insulin sensitivity and glucose tolerance [116]. Instead, Jayawardena et al. [117] have shown that zinc supplementation improves glucose homeostasis in patients with diabetes. Ahn et al. [118] have reported that zinc concentrations are inversely associated with insulin resistance but not correlated with metabolic syndrome. This metal also stimulates glycolysis, inhibits gluconeogenesis, and plays a role in glucose transport in adipocytes [119].
Insulin is co-stored and co-crystallized in granules in pancreatic β-cells with free cytosolic zinc. Six insulin monomers congregate in β-cells into a hexamer with two zinc ions in the center, and this form is stored and transported across the cell membrane as an insulin-zinc crystal in the normal functioning of β-cells. Slepchenko et al. [120] have shown inhibition of the zinc feature upon further glucose-stimulated secretion of insulin. After the zinc–insulin complexes have been secreted, they start to dissociate; only the insulin monomer is an active form of the hormone. The elevated extracellular concentration of free zinc is related to the increase in insulin secretion [60, 120,121,122].
Along with insulin, zinc also takes part in the inhibition of glucagon secretion in response to high glucose concentrations. Glucagon is a hormone secreted by α-cells of the pancreas, which increase the glucose blood level during hypoglycemia. When the glucose concentration decreases, zinc is released from the β-cells with insulin, triggering glucagon secretion [121]. These findings were confirmed in the research conducted by Slucca et al. [123] and Myers [124]. These authors have confirmed the inhibitive properties of zinc released with insulin on glucagon function in mice. Glucagon also regulates glycogen breakdown and gluconeogenesis and decreases at the same time triglyceride synthesis by the liver [11].
Zn transporters
The interaction between zinc status and obesity may be at least partially mediated by obesity-induced modulation of zinc transporters that regulate cellular and intracellular Zn fluxes [1]. In particular, in obese women, the highest expression was observed for ZnT1 followed by Zip1, whereas no significant expression of Zip3 was found [125]. It has been revealed that obese patients were characterized by a significantly lower expression of Zip14 in subcutaneous adipose tissue, whereas a 10-week weight loss period significantly increased gene expression. Zip14 expression directly correlated with PPARy expression and HDL-C concentration, although being negatively associated with anthropometric markers of obesity, body fat percentage, HOMA-IR, blood glucose, insulin, and TG levels [126].
It was also observed that the deficiency of zinc-transporter protein 7 (ZnT7) plays a substantial role in lipid metabolism [127]. It was found that the ZnT7 expression was induced by lipogenic differentiation in ZnT7 knockout mice and the decreased expression of this transporter exacerbates the signal transduction pathway activity, which regulates basal and insulin-stimulated glucose uptake in adipocytes [128].
It has also been demonstrated that SLC39A14, a member of the ZIP protein subfamily, is induced during the early stages of adipogenesis, being associated with increased Zn uptake [126]. It is also notable that Zip14 regulates inflammatory signaling in adipocyte hypertrophy [129]. These findings are in agreement with the earlier data indicating a transient increase of intracellular Zn levels in 3T3L1 cells at the transition from G0/G1- to S-phase of the cell cycle, followed by a decline to the initial levels. Moreover, significantly lower ZnT4, ZnT5, ZnT9, Zip1, Zip4, and Zip6 mRNA levels in lymphocytes were revealed in obese Korean women. Moreover, ZnT4, Zip1, and Zip6 mRNA levels were inversely associated with CRP concentration, whereas ZnT4 and ZnT5 mRNA levels were characterized by an inverse correlation with TNF-α [130]. It has recently been shown that ZIP13 is a crucial regulator of beige adipocyte biogenesis and thermogenesis. Inhibition of ZIP13 function enhanced beige adipocyte biogenesis and energy expenditure by regulating C/EBP-β expression in mouse [131]. It seems that the association between zinc homeostasis and brown adipose tissue, thermogenesis, and inflammation may contribute to the development of new therapies for obesity and metabolic syndrome. Figure 3 summarizes the role of zinc-finger proteins and zinc transporters in regulation of adipogenesis.
It is suggested that also in glycemic control and glucose homeostasis transport zinc proteins play a crucial role. ZnT8 seems to be one of the most important zinc transporters in diabetes. Zinc-protein (ZnT8) is mainly expressed in pancreatic INS-1 β-cells, which contain the largest amount of zinc; this complex induces glucose-stimulated insulin secretion. ZnT8 plays an important role in zinc transport from the cytoplasm into insulin secretory granules within islets, and is thus an essential transporter in the synthesis, storage, and function of insulin [124, 132, 133]. Wijesekara et al. [134] and Pound et al. [133] have shown that zinc deficiency in mice may lead to ZnT8 depletion and may contribute to perturbed function of the islets of Langerhans and increased of insulin, leading to a greater risk of type 2 diabetes mellitus. These authors also reported that ZnT8 depletion may trigger the formation of atypical insulin-zinc secretory granules [133, 134]. Furthermore, Merriman et al. [135] have found that even mutations in ZnT8 may cause greater risk of type 2 diabetes.
Zinc also plays a crucial role in insulin degradation in the liver. It has been found that mutation in ZnT8 may contribute to dysregulation in insulin in the first passage through the liver and increase risk of type 2 diabetes mellitus development [136]. Huang et al. [137, 138] demonstrated that ZnT7 transporter is also implicated in glucose–insulin homeostasis.
Βeta-cells contain larger amounts of zinc ions than are required for the formation of the zinc–insulin granules. After the co-crystallization and secretion of the insulin–zinc granules, the remaining quantities of zinc are redistributed to the cytosol by Zip transporters [139, 140]. Hardy et al. [139] have demonstrated increased levels of free cytosolic zinc in response to a higher level of Zip-4 in mice, whereas Liu et al. [140] reported an elevated concentration of zinc ions in response to increased activity of Zip-6 and Zip-7 transporters. Myers et al. [141] attempted to find a connection between Zip-7 activity and carbohydrate homeostasis; they demonstrated the contribution of Zip-7 to glucose uptake and the storage of glycogen in skeletal muscles. They also conclude that this transporter may be used in insulin resistance treatment. Feitosa et al. [142] have shown that Zip-14 also takes part in zinc homeostasis during inflammation caused by obesity. They also reported elevated plasma concentrations of IL-6, leading to the increased expression of Zip-14 in obese women.
Recent studies have brought attention to the fact that zinc acts as a signaling factor. The mechanism of zinc’s insulin-mimetic activity has been observed in several studies on glucose and lipid metabolism [124]. The signal–transduction mechanism of ZIP10 reflects the role of Zn signaling in B cell function. Zip10-KO mice study showed evidence that ZIP10 signaling regulates caspase activity, promotes the survival of pro-B cells, and regulates the function of mature B-cells [1].
Conclusions and perspectives
Zinc is an essential trace element that plays a substantial role in the prevention of metabolic syndrome, including atherogenic dyslipidemia, hyperglycemia, insulinemia, and elevated blood pressure through the inhibition of proinflammatory cytokine expression, which suppresses ROS production, protecting against oxidative stress damage. Zinc takes part in ROS neutralization as well as in glucose and lipid metabolism. Zinc is thus highly significant in the pathogenesis of metabolic syndrome, which suggests that zinc supplementation would have a positive effect in regressing metabolic syndrome.
Further investigations of the relationship between Zn and cytokines, adipokines, antioxidants, and receptors are needed to explain the role of zinc in health and diseases. Modulation of zinc status may become a new target in the prevention and treatment of metabolic disorders. It has been shown that Zn transporters play the crucial role in zinc homeostasis in the body [1]. It seems that deeper knowledge about physiological functions of Zn transporters and the ability to control their activity may be an important factor in developing new therapies for Zn-related diseases.
References
Hara T, Takeda TA, Takagishi T, Fukue K, Kambe T, Fukada TJ (2017) Physiological roles of zinc transporters: molecular and genetic importance in zinc homeostasis. J Physiol Sci 67(2):283–301
Ahn BI, Kim MJ, Koo HS, Seo N, Joo NS, Kim YS (2014) Serum zinc concentration is inversely associated with insulin resistance but not related with metabolic syndrome in nondiabetic Korean adults. Biol Trace Elem Res 160(2):169–175
Seo JA, Song SW, Han K, Lee KJ, Kim HN (2014) The associations between serum zinc levels and metabolic syndrome in the Korean population: findings from the 2010 Korean National Health and Nutrition Examination Survey. PLoS One 9(8):e105990
Otto MCCD, Alonso A, Lee DH, Delclos GL, Jenny NS, Jiang R, Lima JA, Symanski E, Jacobs DR, Nettleton JA (2011) Dietary micronutrient intakes are associated with markers of inflammation but not with markers of subclinical atherosclerosis. J Nutr 141(8):1508S–1515S
Motamed S, Ebrahimi M, Safarian M, Ghayour-Mobarhan M, Mouhebati M, Azarpazhouh M, Esmailie H, Norouzi A, Ferns GAA (2013) Micronutrient intake and the presence of the metabolic syndrome. N Am J Med Sci 5(6):377–385
Daradkeh G, Zerie M, Othman M, Chandra P, Jaiosi A, Mahmood L, Alowainati B, Mohammad I, Daghash M (2014) Zinc status among type (2) diabetes mellitus in the State of Qatar. Public Health Front 3(1):4–10
Marcinek K, Suliburska J, Krejpcio Z, Bogdanski P (2015) Evaluation of mineral status in hypertensive patients undergoing pharmacotherapy. Rocz Panstw Zakl Hig 66(1):61–67
Ghasemi A, Zahediasl S, Hosseini-Esfahani F, Azizi F (2014) Gender differences in the relationship between serum zinc concentration and metabolic syndrome. Ann Hum Biol 41(5):436–442
Yu Y, Cai Z, Zheng J, Chen J, Zhang X, Huang XF, Li D (2012) Serum levels of polyunsaturated fatty acids are low in Chinese men with metabolic syndrome, whereas serum levels of saturated fatty acids, zinc, and magnesium are high. Nutr Res 32(2):71–77
Rotter I, Kosik-Bogacka D, Dolegowska B, Safranow K, Lubkowska A, Laszczynska M (2015) Relationship between the concentrations of heavy metals and bioelements in aging men with metabolic syndrome. Int J Environ Res Public Health 12:3944–3961
Freitas EP, Cunha AT, Aquino SL, Pedrosa LF, Lima SC, Lima JG, Almeida MG, Sena-Evangelista K (2017) Zinc status biomarkers and cardiometabolic risk factors in metabolic syndrome: a case control study. Nutrients. doi:10.3390/nu9020175
de Luis DA, Pacheco D, Izaola O, Terroba MC, Cuellar L, Cabezas G (2013) Micronutrient status in morbidly obese women before bariatric surgery. Surg Obes Relat Dis 9(2):323–327
Suliburska J, Cofta S, Gajewska E, Kalmus G, Sobieska M, Samborski W, Bogdanski P (2013) The evaluation of selected serum mineral concentrations and their association with insulin resistance in obese adolescents. Eur Rev Med Pharmacol Sci 17(17):2396–2400
Ferro FED, de Sousa Lima VB, Mello Soares NR, Franciscato Cozzolino SM, Nascimento Marreiro DD (2011) Biomarkers of metabolic syndrome and its relationship with the zinc nutritional status in obese women. Nutr Hosp 26(3):650–654
Błażewicz A, Klatka M, Astel A, Partyka M, Kocjan R (2013) Differences in trace metal concentrations (Co, Cu, Fe, Mn, Zn, Cd, and Ni) in whole blood, plasma, and urine of obese and nonobese children. Biol Trace Elem Res 155(2):190–200
Costarelli L, Muti E, Malavolta M, Cipriano C, Giacconi R, Tesei S, Tirabassi G (2010) Distinctive modulation of inflammatory and metabolic parameters in relation to zinc nutritional status in adult overweight/obese subjects. J Nutr Biochem 21(5):432–437
Voruganti VS, Cai G, Klohe DM, Jordan KC, Lane MA, Freeland-Graves JH (2010) Short-term weight loss in overweight/obese low-income women improves plasma zinc and metabolic syndrome risk factors. J Trace Elem Med Biol 24(4):271–276
Payahoo L, Ostadrahimi A, Mobasseri M, Bishak YK, Farrin N, Jafarabadi MA, Ostadrahimi A (2013) Effects of zinc supplementation on the anthropometric measurements, lipid profiles and fasting blood glucose in the healthy obese adults. Advan Pharm Bull 3(1):161–165
Kelishadi R, Hashemipour M, Adeli K, Tavakoli N, Movahedian-Attar A, Shapouri J, Rouzbahani A (2010) Effect of zinc supplementation on markers of insulin resistance, oxidative stress, and inflammation among prepubescent children with metabolic syndrome. Metab Syndr Relat Disord 8(6):505–510
Sinha S, Sen S (2014) Status of zinc and magnesium levels in type 2 diabetes mellitus and its relationship with glycemic status. Int J Diabetes Dev Ctries 34(4):220–223
Olaniyan OO, Awonuga MAM, Ajetunmobi AF, Adeleke IA, Fagbolade OJ, Olabiyi KO, Oyekanmi BA, Osadolor HB (2012) Serum copper and zinc levels in Nigerian type 2 diabetic patients. Afr J Diabetes Med 20(2):36–38
Devi TR, Hijam D, Dubey A, Debnath S, Oinam P, Devi NGT, Singh WG (2016) Study of serum zinc and copper levels in type 2 diabetes mellitus. Int J Contem Med Res 3(4):2454–7379
Kaur J, Singh T (2015) Estimation of serum magnesium and zinc levels in type-2 diabetes mellitus. Int J Bioassays 4(1):3654–3656
Yahya H, Yahya KM, Saqib A (2011) Minerals and type 2 diabetes mellitus—levels of zinc, magnesium and chromium in diabetic and nondiabetic population. J UMDC 2:1
Jyothirmayi B, Vasantha M (2015) Study of zinc and glycated Hb levels in diabetic complications. Int J Pharm Clin Res 7(5):360–363
Kumar DA, Priya VS, Jaiprabhu J, Ramalingam K (2014) Serum copper and zinc levels significance in type 2 diabetic patients. J Med Sci Tech 3(2):79–81
Bao B, Prasad AS, Beck FWJ, Fitzgerald JT, Snell D, Bao GW, Singh T, Cardozo LJ (2010) Zinc decreases C-reactive protein, lipid peroxidation, and inflammatory cytokines in elderly subjects: a potential implication of zinc as an atheroprotective agent. Am J Clim Nutr 91(6):1634–1641
Ho M, Baur LA, Cowell CT, Samman S, Garnett SP (2016) Zinc status, dietary zinc intake and metabolic risk in Australian children and adolescents; Nepean Longitudinal Study. Eur J Nutr 30:1–8
El-Ashmony SMA, Morsi HK, Abdelhafez AM (2012) Effect of zinc supplementation on glycemic control, lipid profile, and renal functions in patients with type II diabetes: a single blinded, randomized, placebo-controlled, trial. J Biol Agric Health 2(6):33
Kanoni S, Nettleton JA, Hivert M-F, Ye Z, van Rooij FJA, Shungin D, Sonestedt E, Ngwal JS, Wojczynski MK, Lemaitre RN, Gustafsson S, Anderson JS et al (2011) Total zinc intake may modify the glucose-raising effect of a zinc transporter (SLC30A8) variant a 14-cohort meta-analysis. Diabetes 60(9):2407–2416
Islam MR, Attia J, Ali L, McEvoy M, Selim S, Sibbritt D, Akhter A, Akter S, Peel R, Faruque O, Mona T, Lona H, Milton AH (2016) Zinc supplementation for improving glucose handling in pre-diabetes: a double-blind randomized placebo controlled pilot study. Diabetes Res Clin Pract 115:39–46
Karamali M, Heidarzadeh Z, Seifati SM, Samimi M, Tabassi Z, Hajijafari M, Asemi Z, Esmaillzadeh A (2015) Zinc supplementation and the effects on metabolic status in gestational diabetes: a randomized, double-blind, placebo-controlled trial. J Diabetes Complic 29(8):1314–1319
El Dib R, Gameiro OL, Ogata MS, Módolo NS, Braz LG, Jorge EC, do Nascimento P Jr, Beletate V (2015) Zinc supplementation for the prevention of type 2 diabetes mellitus in adults with insulin resistance. Cochrane Database Syst Rev 28(5). doi:10.1002/14651858.CD005525.pub3
Haase H, Rink L (2014) Zinc signals and immune function. BioFactors 40(1):27–40
Fernández-Sánchez A, Madrigal-Santillán E, Bautista M, Jaime Esquivel-Soto J, Morales-González A, Esquivel-Chirino C, Durante-Montiel I, Sánchez-Rivera G, Valadez-Vega C, Morales-González JA (2011) Inflammation, oxidative stress, and obesity. Int J Mol Sci 12(5):3117–3132
Jung S, Kyung Kim MK, Choi BY (2015) The relationship between zinc status and inflammatory marker levels in rural Korean adults aged 40 and older. PLoS One 10(6):e0130016
Donath MY, Böni-Schnetzler M, Ellingsgaard H, Halban PA, Ehses JA (2010) Cytokine production by islets in health and diabetes: cellular origin, regulation and function. Trends Endocrinol Metab 21(5):261–267
Olbert M, Wyszogrodzka G, Młyniec K, Librowski T (2017) Antioxidant and anti-inflammatory effects of zinc. Zinc-dependent NF-κB signaling. Inflammopharmacology 25(1):11–24
von Bülow V, Dubben S, Engelhardt G, Hebel S, Plümäkers B, Heine H, Rink L, Haase H (2017) Zinc-dependent suppression of TNF-alpha production is mediated by protein kinase A-induced inhibition of Raf-1, I kappa B kinase beta, and NF-kappa B. J Immunol 179(6):4180–4186
Liu MJ, Bao S, Gálvez-Peralta M, Pyle CJ, Rudawsky AC, Pavlovicz RE, Killilea DW, Li C, Nebert DW, Wewers MD, Knoell DL (2013) ZIP8 regulates host defense through zinc-mediated inhibition of NF-κB. Cell Rep 3(2):386–400
Prasad AS (2014) Zinc is an antioxidant and anti-inflammatory agent: its role in human health. Front Nutr 1:14. doi:10.3389/fnut.2014.00014
Löffek S, Schilling O, Franzke CW (2011) Biological role of matrix metalloproteinases: a critical balance. Eur Respir J 38:191–208
Chen Q, Jin M, Yang F, Zhu J, Xiao Q, Zhang L (2013) Matrix metalloproteinases: inflammatory regulators of cell behaviors in vascular formation and remodeling. Mediat Inflamm. doi:10.1155/2013/928315
Jagadeesha DK, Takapoo M, Banfi B, Bhalla RC, Miller FJ (2012) Nox1 transactivation of epidermal growth factor receptor promotes N-cadherin shedding and smooth muscle cell migration. Cardiovasc Res 93(3):406–413
Usmanova ZA (2015) Relationship between the levels of MMP-9, TIMP-1, and zinc in biological samples of patients with carotid atherosclerosis. IJBM 5(2):60–64
Xu C, Huang Z, Liu L, Luo C, Lu G, Li Q, Gao X (2015) Zinc regulates lipid metabolism and MMPs expression in lipid disturbance rabbits. Biol Trace Elem Res 168(2):411–420
Hopps E, Noto D, Caimi G, Averna MR (2010) A novel component of the metabolic syndrome: the oxidative stress. Nutr Metab Cardiovasc Dis 20(1):72–77
Ogawa D, Asanuma M, Miyazaki I, Tachibana H, Wada J, Sogawa N, Sugaya T, Kitamura S, Maeshima Y, Shikata K (2011) High glucose increases metallothionein expression in renal proximal tubular epithelial cells. Exp Diabetes Res. doi:10.1155/2011/534872
Hadwan MH, Almashhedy LA, Alsalman ARS (2014) Study of the effects of oral zinc supplementation on peroxynitrite levels, arginase activity and NO synthase activity in seminal plasma of Iraqi asthenospermic patients. Reprod Biol Endocrinol 12:1. doi:10.1186/1477-7827-12-1
Oteiza PI (2012) Zinc and the modulation of redox homeostasis. Free Radic Biol Med 53(9):1748–1759
Korkmaz-Icöz S, Atmanli A, Radovits T, Li S, Hegedüs P, Ruppert M, Brlecic P, Yoshikawa Y, Yasui H, Karck M, Szabó GJ (2016) Administration of zinc complex of acetylsalicylic acid after the onset of myocardial injuryprotects the heart by upregulation of antioxidant enzymes. J Physiol Sci 66(2):113–125
Li HT, Jiao M, Chen J, Liang Y (2010) Roles of zinc and copper in modulating the oxidative refolding of bovine copper, zinc superoxide dismutase. Acta Biochim Biophys Sin (Shanghai) 42(3):183–194
Skalny AA, Tinkov AA, Medvedeva YS, Alchinova IB, Karganov MY, Skalny AV, Nikonorov AA (2015) Effect of short-term zinc supplementation on zinc and selenium tissue distribution and serum antioxidant enzymes. Acta Sci Pol Technol Aliment 14(3):269–276
Perriotte-Olson C, Adi N, Manickam DS, Westwood RA, Desouza CV, Natarajan G, Saraswathi V (2014) Nanoformulated copper/zinc superoxide dismutase reduces adipose inflammation in obesity. Obesity 24(1):148–156
Saraswathi V, Ganesan M, Perriotte-Olson C, Manickam DS, Westwood RA, Zimmerman MC, Kabanov AV (2016) Nanoformulated copper/zinc superoxide dismutase attenuates vascular cell activation and aortic inflammation in obesity. Biochem Biophys Res Commun 469(3):495–500
Manea A, Tanase LI, Raicu M, Simionescu M (2010) Transcriptional regulation of NADPH oxidase isoforms, Nox1 and Nox4, by nuclear factor-kappaB in human aortic smooth muscle cells. Biochem Biophys Res Commun 396(4):901–907
Marseglia L, Manti S, D’Angelo G, Nicotera A, Parisi E, Rosa Di, Gitto E, Arrigo T (2015) Oxidative stress in obesity: a critical component in human diseases. Int J Mol Sci 16(1):378–400
Li B, Cui W, Tan Y, Luo P, Chen Q, Zhang C, Qu W, Miao L, Cai L (2014) Zinc is essential for the transcription function of Nrf2 in human renal tubule cells in vitro and mouse kidney in vivo under the diabetic condition. J Cell Mol Med 18(5):895–906
Ruttkay-Nedecky B, Nejdl L, Gumulec J, Zitka O, Masarik M, Eckschlager T, Stiborova M, Adam V, Kizek R (2013) The role of metallothionein in oxidative stress. Int J Mol Sci 14:6044–6066
Bellomo EA, Meur G, Rutter GA (2011) Glucose regulates free cytosolic Zn2+ concentration, Slc39 (ZiP), and metallothionein gene expression in primary pancreatic islet β-cells. J Biol Chem 286(29):25778–25789
Haynes V, Connor T, Tchernof A, Vidal H, Dubois S (2013) Metallothionein 2a gene expression is increased in subcutaneous adipose tissue of type 2 diabetic patients. Mol Genet Metab 108(1):90–94
Sato M, Kawakami T, Kadota Y, Mori M, Suzuki S (2013) Obesity and metallothionein. Curr Pharm Biotechnol 14(4):432–440
Chen J, Wang S, Luo M, Zhang Z, Dai X, Kong M, Cai L, Wang Y, Shi B, Tan Y (2016) From the cover: zinc deficiency worsens and supplementation prevents high-fat diet induced vascular inflammation, oxidative stress, and pathological remodeling. Toxicol Sci 153(1):124–136
Muthuraman P, Ramkumar K, Kim DH (2014) Analysis of dose-dependent effect of zinc oxide nanoparticles on the oxidative stress and antioxidant enzyme activity in adipocytes. Appl Biochem Biotechnol 174(8):2851–2863
Pandurangan M, Veerappan M, Kim DH (2015) Cytotoxicity of zinc oxide nanoparticles on antioxidant enzyme activities and mRNA expression in the cocultured C2C12 and 3T3-L1 cells. Appl Biochem Biotechnol 175(3):1270–1280
Li YR, Guo HW, Wu M, Liu M (2013) Serum and dietary antioxidant status is associated with lower prevalence of the metabolic syndrome in a study in Shanghai, China. Asia Pac J Clin Nutr 22(1):60–68
Taheri E, Djalali M, Saedisomeolia A, Moghadam AM, Djazayeri A, Qorbani M (2012) The relationship between the activates of antioxidant enzymes in red blood cells and body mass index in Iranian type 2 diabetes and healthy subjects. J Diabetes Metab Disord 11(1):3. doi:10.1186/2251-6581-11-3
Doddigarla Z, Parwez I, Ahmad J (2016) Correlation of serum chromium, zinc, magnesium and SOD levels with HbA1c in type 2 diabetes: a cross sectional analysis. Diabetes Metab Syndr 10(1 Suppl 1):S126–S129
Wang X, Li H, Fan Z, Liu Y (2012) Effect of zinc supplementation on type 2 diabetes parameters and liver metallothionein expressions in Wistar rats. J Physiol Biochem 68(4):563–572
Sun W, Wang Y, Miao X, Wang Y, Zhang L, Xin Y, Cai L (2014) Renal improvement by zinc in diabetic mice is associated with glucose metabolism signaling mediated by metallothionein and Akt, but not Akt2. Free Radic Biol Med 68:22–34
Seet RC, Lee CYJ, Lim EC, Quek AM, Huang H, Huang SH, Halliwell B (2011) Oral zinc supplementation does not improve oxidative stress or vascular function in patients with type 2 diabetes with normal zinc levels. Atherosclerosis 219(1):231–239
Marjani A, Moradi A, Saeedi M (2017) Plasma lipid peroxidation zinc and erythrocyte Cu-Zn superoxide dismutase enzyme activity in patients with type 2 diabetes mellitus in Gorgan City (South East of the Caspian Sea). J Med Sci 7(4):585–590
Vávrová L, Kodydková J, Zeman M, Dušejovská M, Macášek J, Staňková B, Tvrzická E, Zák A (2013) Altered activities of antioxidant enzymes in patients with metabolic syndrome. Obes Facts 6(1):39–47
Lima VBDS, Sampaio FDA, Bezerra DLC, Moita Neto JM, Marreiro DDN (2011) Parameters of glycemic control and their relationship with zinc concentrations in blood and with superoxide dismutase enzyme activity in type 2 diabetes patients. Arq Bras Endocrinol Metabol 55(9):701–707
Ranasinghe P, Wathurapatha WS, Ishara MH, Jayawardana R, Galappatthy P, Katulanda P, Constantine GR (2015) Effects of Zinc supplementation on serum lipids: a systematic review and meta-analysis. Nutr Metab 12:26. doi:10.1186/s12986-015-0023-4
Weigand E, Egenolf J (2017) Moderate zinc deficiency does not alter lipid and fatty acid composition in the liver of weanling rats fed diets rich in cocoa butter or safflower oil. J Nutr Metab. doi:10.1155/2017/4798963
Tayeb W, Nakbi A, Cheraief I, Miled A, Hammami M (2013) Alteration of lipid status and lipid metabolism, induction of oxidative stress and lipid peroxidation by 2,4-dichlorophenoxyacetic herbicide in rat liver. Toxicol Mech Methods 23(6):449–458
Li X, Guan Y, Shi X, Ding H, Song Y, Li C, Liu R, Liu G (2013) Effects of high zinc levels on the lipid synthesis in rat hepatocytes. Biol Trace Elem Res 154(1):97–102
Khan MI, Siddique KU, Ashfaq F, Ali W, Reddy HD, Mishra A (2013) Effect of high-dose zinc supplementation with oral hypoglycemic agents on glycemic control and inflammation in type-2 diabetic nephropathy patients. J Nat Sci Biol Med 4(2):336–340
Gunasekara P, Hettiarachchi M, Liyanage C, Lekamwasam S (2011) Effects of zinc and multimineral vitamin supplementation on glycemic and lipid control in adult diabetes. Diabetes Metab Syndr Obes 4:53–60
Tinkov AA, Popova EV, Gatiatulina ER, Skalnaya AA, Yakovenko EN, Alchinova IB, Nikonorov AA (2016) Decreased adipose tissue zinc content is associated with metabolic parameters in high fat fed Wistar rats. Acta Sci Pol Technol Aliment 15(1):99–105
Liu MJ, Bao S, Bolin ER, Burris DL, Xu X, Sun Q, Failla ML (2013) Zinc deficiency augments leptin production and exacerbates macrophage infiltration into adipose tissue in mice fed a high-fat diet. J Nutr 143(7):1036–1045
Charradi K, Elkahoui S, Limam F, Aouani EJ (2013)High-fat diet induced an oxidative stress in white adipose tissue and disturbed plasma transition metals in rat: prevention by grape seed and skin extract. J Physiol Sci 63(6):445–455
Baltaci AK, Mogulkoc R (2012) Leptin and zinc relation: in regulation of food intake and immunity. Indian J Endocrinol Metab 16(Suppl 3):S611–S616
Briggs DB, Giron RM, Schnittker K, Hart MV, Park CK, Hausrath AC, Tsao TS (2012) Zinc enhances adiponectin oligomerization to octadecamers but decreases the rate of disulfide bond formation. Biometals 25(2):469–486
Mazloomi S, Alizadeh N, Aminzare M, Niroomand S, Mousavi SN (2017) Serum zinc and adiponectin levels in patients with polycystic ovary syndrome, adjusted for anthropometric, biochemical, dietary intake, and physical activity measures. Biol Trace Elem Res. doi:10.1007/s12011-017-0951-0
Soheylikhah SEDIGHEH, Dehestani MR, Mohammadi SM, Afkhami AM, Eghbali SA, Dehghan F (2012) The effect of zinc supplementation on serum adiponectin concentration and insulin resistance in first degree relatives of diabetic patients. Iran J Diabetes Obes 4(2):57–62
Bing C, Mracek T, Gao D, Trayhurn P (2012) Zinc-α2-glycoprotein: an adipokine modulator of body fat mass? Int J Obes 34(11):1559–1565
Garrido-Sánchez L, García-Fuentes E, Fernández-García D, Escote X, Alcaide J, Perez-Martinez P, Vendrell J, Tinahones FJ (2012) Zinc-alpha 2-glycoprotein gene expression in adipose tissue is related with insulin resistance and lipolytic genes in morbidly obese patients. PLoS One 7(3):e33264
Russell ST, Tisdale MJ (2011) Studies on the antiobesity effect of zinc-α2-glycoprotein in the ob/ob mouse. Int J Obes 35:345–354
Cabassi A, Tedeschi S (2013) Zinc-α2-glycoprotein as a marker of fat catabolism in humans. Curr Opin Clin Nutr Metab Care 16(3):267–271
Yang M, Liu R, Li S, Luo Y, Zhang Y, Zhang L, Liu D, Wang Y, Xiong Z, Boden G et al (2013) Zinc-α2-glycoprotein is associated with insulin resistance in humans and is regulated by hyperglycemia, hyperinsulinemia, or liraglutide administration: cross-sectional and interventional studies in normal subjects, insulin-resistant subjects, and subjects with newly diagnosed diabetes. Diabetes Care 36(5):1074–1082
Mracek T, Ding Q, Tzanavari T, Kos K, Pinkney J, Wilding J, Trayhurn P, Bing C (2010) The adipokine zinc-a2-glycoprotein (ZAG) is downregulated with fat mass expansion in obesity. Clin Endocrinol 72:334–341
Mracek T, Gao D, Tzanavari T, Bao Y, Xiao X, Stocker C, Trayhurn P, Bing C (2010) Downregulation of zinc-a2-glycoprotein in adipose tissue and liver of obese ob/ob mice and by tumour necrosis factor-a in adipocytes. J Endocrinol 204:165–172
Zhu HJ, Wang X, Pan H, Gong F, Zhang D, Li N, Wang L, Yang H (2014) Serum levels of the adipokine zinc-α2-glycoprotein are decreased in patients with hypertension. ISRN Endocrinol. doi:10.1155/2014/374090
Balaz M, Vician M, Janakova Z, Kurdiova T, Surova M, Imrich R, Belan V (2014) Subcutaneous adipose tissue zinc-α2-glycoprotein is associated with adipose tissue and whole-body insulin sensitivity. Obesity 22(8):1821–1829
Zahid H, Miah L, Lau AM, Brochard L, Hati D, Bui TT, McDermott LC (2016) Zinc-induced oligomerization of zinc α2 glycoprotein reveals multiple fatty acid-binding sites. Biochem J 473(1):43–54
Goto T, Lee JY, Teraminami A, Kim YI, Hirai S, Uemura T, Inoue H, Takahashi N, Kawada T (2011) Activation of peroxisome proliferator-activated receptor-alpha stimulates both differentiation and fatty acid oxidation in adipocytes. J Lipid Res 52(5):873–884
Fruchart JC (2013) Selective peroxisome proliferator-activated receptor α modulators (SPPARMα): the next generation of peroxisome proliferator-activated receptor α-agonists. Cardiovasc Diabetol 31(12):82. doi:10.1186/1475-2840-12-82
Grygiel-Górniak B (2014) Peroxisome proliferator-activated receptors and their ligands: nutritional and clinical implications—a review. Nutr J 14(13):17. doi:10.1186/1475-2891-13-17
Zhou T, Yan X, Wang G, Liu H, Gan X, Zhang T, Wang J, Liang Li L (2015) Evolutionary pattern and regulation analysis to support why diversity functions existed within PPAR gene family members. Biomed Res Int. doi:10.1155/2015/613910
Bergen WG, Burnett DD (2013) Topics in transcriptional control of lipid metabolism: from transcription factors to gene-promoter polymorphisms. J Genoms 20(1):13–21
Lee J-E, Ge K (2014) Transcriptional and epigenetic regulation of PPARγ expression during adipogenesis. Cell Biosci 4:29. doi:10.1186/2045-3701-4-29
Seale P (2015) Transcriptional regulatory circuits controlling brown fat development and activation. Diabetes 64(7):2369–2375
Pandurangan M, Jin BY, Kim DH (2016) ZnO Nanoparticles upregulates adipocyte differentiation in 3T3-L1 cells. Biol Trace Elem Res 170(1):201–207
Ghosh C, Yang SH, Kim JG, Jeon TI, Yoon BH, Lee JY, Hwang SG (2013) Zinc-chelated vitamin C stimulates adipogenesis of 3T3-L1 cells. Asian–Australas J Anim Sci 26(8):1189–1196
Justus J, Weigand EA (2014) Moderate zinc deficiency does not impair gene expression of PPARα, PPARγ, and mitochondrial enoyl-CoA delta isomerase in the liver of growing rats. Nutr Metab Insights 7:29–37
Orazizadeh M, Khodadadi A, Bayati V, Saremy S, Farasat M, Khorsandi L (2015) In vitro toxic effects of zinc oxide nanoparticles on rat adipose tissue-derived mesenchymal stem cells. Cell J 17(3):412–421
Mueller E (2014) Understanding the variegation of fat: novel regulators of adipocyte differentiation and fat tissue biology. Biochim Biophys Acta 1842(3):352–357
Meruvu S, Hugendubler L, Mueller E (2011) Regulation of adipocyte differentiation by the zinc finger protein ZNF638. J Biol Chem 286(30):26516–26523
Gupta RK, Arany Z, Seale P, Mepani RJ, Ye L, Conroe HM, Spiegelman BM (2010) Transcriptional control of preadipocyte determination by Zfp423. Nature 464(7288):619–623
Quach JM, Walker EC, Allan E, Solano M, Yokoyama A, Kato S, Martin TJ (2011) Zinc finger protein 467 is a novel regulator of osteoblast and adipocyte commitment. J Biol Chem 286(6):4186–4198
You L, Pan L, Chen L, Chen JY, Zhang X, Lv Z, Fu D (2012) Suppression of zinc finger protein 467 alleviates osteoporosis through promoting differentiation of adipose derived stem cells to osteoblasts. J Transl Med 10(1):11. doi:10.1186/1479-5876-10-11
Kang S, Akerblad P, Kiviranta R, Gupta RK, Kajimura S, Griffin MJ, Min J, Baron R, Rosen ED (2012) Regulation of early adipose commitment by Zfp521. PLoS Biol 10(11):e1001433
Wei S, Zhang L, Zhou X, Du M, Jiang Z, Hausman GJ, Dodson MV (2013) Emerging roles of zinc finger proteins in regulating adipogenesis. Cell Mol Life Sci 70(23):4569–4584
Yanga HK, Leea SH, Hanc K, Kanga B, Leed SY, Yoona KH, Kwona HS, Parkf YM (2015) Lower serum zinc levels are associated with unhealthy metabolic status in normal-weight adults: the 2010 Korea National Health and Nutrition Examination Survey. Diabetes Metabol 41:282–290
Jayawardena R, Ranasinghe P, Galappatthy P, Malkanthi R, Constantine G, Katulanda P (2012) Effects of zinc supplementation on diabetes mellitus: a systematic review and meta-analysis. Diabetol Metab Syndr 4(1):13
Ahn B-I, Kim MJ, Koo HS, Seo N, Joo N-S, Kim Y-S (2014) Serum zinc concentration is inversely associated with insulin resistance but not related with metabolic syndrome in nondiabetic Korean adults. Biol Trace Elem Res 160:169–175
Ranasinghe P, Pigera S, Galappatthy P, Katulanda P, Constantine GR (2015) Zinc and diabetes mellitus: understanding molecular mechanisms and clinical implications. Daru 23(1):44. doi:10.1186/s40199-015-0127-4
Slepchenko KG, Daniels NA, Guo A, Li YV (2015) Autocrine effect of Zn2+ on the glucose-stimulated insulin secretion. Endocrine 50(1):110–122
Slepchenko KG, James CB, Li YV (2013) Inhibitory effect of zinc on glucose-stimulated zinc/insulin secretion in an insulin-secreting β-cell line. Exp Physiol 98(8):1301–1311
Kira G, Slepchenko K, Yang V (2012) Rising intracellular zinc by membrane depolarization and glucose in insulin-secreting clonal HIT-T15 beta cells. Exp Diabetes Res. doi:10.1155/2012/190309
Slucca M, Harmon JS, Oseid EA, Bryan J, Robertson RP (2010) ATP-sensitive K + channel mediates the zinc switch-off signal for glucagon response during glucose deprivation. Diabetes 59(1):128–134
Myers SA (2015) Zinc transporters and zinc signaling: new insights into their role in type 2 diabetes. Int J Endocrinol. doi:10.1155/2015/167503
dos Santos Rocha PBK, de Castro Amorim A, de Sousa AF, do Monte SJH, da Mata Sousa LCD, do Nascimento Nogueira N, do Nascimento Marreiro D (2011) Expression of the zinc transporters genes and metallothionein in obese women. Biol Trace Elem Res 143(2):603–611
Maxel T, Smidt K, Larsen A, Bennetzen M, Cullberg K, Fjeldborg K, Lund S, Pedersen SB, Rungby J (2015) Gene expression of the zinc transporter ZIP14 (SLC39a14) is affected by weight loss and metabolic status and associates with PPARγ in human adipose tissue and 3T3-L1 pre-adipocytes. BMC Obes 2:46
Tepaamorndech S, Kirschke CP, Huang L (2014) Linking cellular zinc status to body weight and fat mass: mapping quantitative trait loci in Znt7 knockout mice. Mamm Genome 25(7–8):335–353
Tepaamorndech S, Kirschke CP, Pedersen TL, Keyes WR, Newman JW, Huang L (2016) Zinc transporter 7 deficiency affects lipid synthesis in adipocytes by inhibiting insulin-dependent Akt activation and glucose uptake. FEBS J 283(2):378–394
Troche C, Aydemir TB, Cousins RJ (2016) Zinc transporter Slc39a14 regulates inflammatory signaling associated with hypertrophic adiposity. Am J Physiol Endocrinol Metab 310(4):258–268
Noh H, Paik HY, Kim J, Chung J (2014) The alteration of zinc transporter gene expression is associated with inflammatory markers in obese women. Biol Trace Elem Res 158(1):1–8
Fukunaka A, Fukada T, Bhin J, Suzuki L, Tsuzuki T, Takamine Y, Bin BH, Yoshihara T, Ichinoseki-Sekine N, Naito H, Miyatsuka T, Takamiya S, Sasaki T, Inagaki T, Kitamura T, Kajimura S, Watada H, Fujitani Y (2017) Zinc transporter ZIP13 suppresses beige adipocyte biogenesis and energy expenditure by regulating C/EBP-β expression. PLoS Genet 13(8):e1006950. doi:10.1371/journal.pgen.1006950
Solomou A, Meur G, Bellomo E, Hodson DJ, Tomas A, Li SM, Philippe E, Herrera PL, Magnan C, Rutter GA (2015) The zinc transporter Slc30a8/ZnT8 is required in a subpopulation of pancreatic α-cells for hypoglycemia-induced glucagon secretion. J Biol Chem 290(35):21432–21442
Pound LD, Sarkar SA, Ustione A, Dadi PK, Shadoan MK, Lee CE, Walters JA, Shiota M, McGuinness OP, Jacobson DA et al (2012) The physiological effects of deleting the mouse SLC30A8 gene encoding zinc transporter-8 are influenced by gender and genetic background. PLoS One 7(7):40972
Wijesekara N, Dai FF, Hardy AB, Giglou PR, Bhattacharjee A, Koshkin V, Chimienti F, Gaisano HY, Rutter GA, Wheeler MB (2010) Beta cell-specific Znt8 deletion in mice causes marked defects in insulin processing, crystallisation and secretion. Diabetologia 53(8):1656–1668
Merriman M, Huang Q, Rutter GA, Fu D (2016) Lipid-tuned zinc transport activity of human ZnT8 protein correlates with risk for type-2 diabetes. J Biol Chem 291(53):26950–26957
Tamaki M, Fujitani Y, Hara A, Uchida T, Tamura Y, Takeno K, Kawaguchi M, Watanabe T, Ogihara T, Fukunaka A et al (2013) The diabetes-susceptible gene SLC30A8/ZnT8 regulates hepatic insulin clearance. J Clin Invest 123(10):4513–4524
Huang L, Yan M, Kirschke CP (2010) Over-expression of ZnT7 increases insulin synthesis and secretion in pancreatic beta-cells by promoting insulin gene transcription. Exp Cell Res 316(16):2630–2643
Huang L, Kirschke CP, Lay YA, Levy LB, Lamirande DE, Zhang PH (2012) Znt7-null mice are more susceptible to diet-induced glucose intolerance and insulin resistance. J Biol Chem 287(40):33883–33896
Hardy AB, Prentice KJ, Froese S, Liu Y, Andrews GK, Wheeler MB (2015) Zip4 mediated zinc influx stimulates insulin secretion in pancreatic beta cells. PLoS One 10(3):0119136
Liu Y, Batchuluun B, Ho L, Zhu D, Prentice KJ, Bhattacharjee A, Zhang M, Pourasgari F, Hardy AB, Taylor KM, Gaisano H, Dai FF, Wheeler MB (2015) Characterization of zinc influx transporters (ZIPs) in pancreatic β cells: roles in regulating cytosolic zinc homeostasis and insulin secretion. J Biol Chem 290(30):18757–18769
Myers SA, Nield A, Chew GS, Myers MA (2013) The zinc transporter, Slc39a7 (Zip7) is implicated in glycaemic control in skeletal muscle cells. PLoS One 8(11):e79316
Feitosa MC, Lima VB, Moita Neto JM, Marreiro DN (2013) Plasma concentration of IL-6 and TNF-α and its relationship with zincemia in obese women. Rev Assoc Med Bras 59(5):429–434
Acknowledgements
All authors have read and approved the final manuscript.
Author information
Authors and Affiliations
Contributions
JO collected literature and drafted the manuscript; AT and AS drafted the manuscript and prepared the figures; JS developed the concept and drafted the manuscript; JO, AT, AS, and JS edited and revised the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Funding
This article was not funded by any grants.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Olechnowicz, J., Tinkov, A., Skalny, A. et al. Zinc status is associated with inflammation, oxidative stress, lipid, and glucose metabolism. J Physiol Sci 68, 19–31 (2018). https://doi.org/10.1007/s12576-017-0571-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-017-0571-7