Abstract
Purpose of Review
The present work summarizes the clinical relevance of coronary flow capacity (CFC) with an eye on future perspectives.
Recent findings
CFC concept has been recently introduced providing a comprehensive framework for coronary physiology evaluation.
Summary
It has been widely demonstrated that coronary artery disease (CAD) is a complex disease with a multifactorial etiology resulting from different pathogenic mechanisms. Cardiac positron emission tomography (PET) currently represents the gold standard for CAD assessment, providing absolute myocardial perfusion data including coronary flow reserve (CFR), calculated as the ratio of hyperemic to rest absolute myocardial blood flows. CFC can be obtained from dynamic PET images by plotting the primary stress perfusion data and CFR values for each pixel on a graph of predefined exact ranges. The routine evaluation of this parameter may add diagnostic and prognostic value to clinical and conventional imaging data.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It has been widely demonstrated that coronary artery disease (CAD) is a complex disease with a multifactorial etiology resulting from different pathogenic mechanisms [1, 2•].
Despite great technological improvements in diagnosis and dramatic advances in therapeutic approaches, CAD is the primary single cause of mortality and global loss of disability adjusted life years [3]. Moreover, the CAD-related mortality is estimated to increase due to worsening of metabolic risk factors especially in developing countries.
The available invasive and non-invasive imaging tools have been proved being able to provide a large amount of data to identify the presence, extension, and severity of CAD with diagnostic and prognostic upshots [4 5, 6, 7, 8, 9, 10].
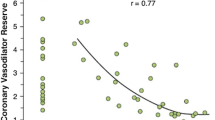
Cardiac positron emission tomography (PET) currently represents the gold standard for CAD assessment, providing absolute myocardial perfusion data including coronary flow reserve (CFR), calculated as the ratio of hyperemic to rest absolute myocardial blood flows (MBF). Such parameter reflects coronary vasodilator capacity. It should be taken into account that CFR depends on both coronary hemodynamics at rest and under stress conditions, and that any physiological change may accidentally affect the CFR estimation [11]. To overcome such limitations, Johnson and Gould have recently introduced the coronary flow capacity (CFC) concept, proposing a comprehensive framework for coronary physiology evaluation [12, 13•, 14].
CFC Measurement
CFC combines hyperemic MBF and CFR with thresholds for definite or possible ischemia to comprehensively assess all relevant coronary flow characteristics [15] on pixel bases. In detail, this parameter can be obtained from dynamic PET images by plotting the primary stress perfusion data and CFR values for each pixel on a graph of predefined exact ranges consistent with minimal, mild, moderate, or severely reduced CFC [12, 13•].
On a color scale basis a map of left ventricle CFC can be interpreted as follows: red, normal, referring to healthy individuals with no risk factors (CFR > 2.9 and stress perfusion > 2.17 cc/min/g); orange, minimally reduced, defined by risk factors only without clinically manifest CAD (CFR > 2.38 to 2.9 and stress perfusion > 1.82 to 2.17 cc/min/g); yellow, mildly reduced, denoting documented stable CAD without angina or ST depression on ECG during dipyridamole stress (CFR > 1.6 to 2.38 and stress perfusion > 1.09 to 1.82 cc/min/g); green, moderately reduced, with possible ischemia (CFR > 1.27 to 1.6 and stress perfusion > 0.83 to 1.09 cc/min/g); blue, severely reduced with definite ischemia (CFR 1.0 to 1.27 and stress perfusion ≤ 0.83 cc/min/g); dark blue, defined by myocardial steal with stress perfusion falling below rest perfusion (CFR < 1.0) [13•, 14].
CFC from Diagnosis to Prognosis
The clinical meaning of this parameter takes into account that rest images may result heterogeneous and become more uniform or normalize under stress conditions due to endothelial dysfunction associated with CAD [16, 17]. Thus, resting myocardial perfusion may cause corresponding heterogeneous CFR either with or without segmental or diffuse flow limiting stenosis caused by coronary atherosclerosis. However, this heterogeneity typically does not follow specific coronary artery distributions, but it can be identified by CFP map that differentiates among endothelial mediated heterogeneity, flow limiting stenosis, and diffuse global disease [18].
Indeed, as compared with regional or global CFR or stress perfusion data, available literature demonstrates that CFC recognizes individual regional and global heterogeneities refining cardiac events risk prediction [13•, 18].
Yet, the caffeine effect on the stressor kinetic may affect the clinical meaning of CFC metrics estimation. It has been shown that even low serum caffeine levels may cause heterogeneously reduced maximal regional and global values of stress flow and CFR, with CFC distribution changing over the entire LV [19, 20].
Moreover, besides patient preparation, the pharmacological stress type may also affect the robustness of provided flow data. Kitkungvan and co-workers previously showed that standard stress PET imaging protocol using 6-min adenosine infusion with 82Rb administration at 3 min is the most appropriate adenosine protocol for quantifying both CFC and CFR, with comparable results to a 4-min dipyridamole infusion with Rb-82 injection at 8 min [21]. The reported finding also highlighted how inadequate stress protocol may mislead results interpretation.
In a recent investigation, involving 3774 patients, the Authors demonstrated that CFC integrating regional CFR and regional absolute stress perfusion in cc/min/g by 82Rb PET provides automated, objective, artery-specific, regional size–severity, physiologic quantification of CAD severity associated with high risk of death and myocardial infarction independently of standard risk factors and other quantitative PET parameters [13•].
More recently, in a 10-year follow-up investigation performed on a population of 5274 patients, Gould and co-workers demonstrated that severely reduced CFC predicted higher death, myocardial infarction, stroke, and revascularization than any other severity 82Rb PET metric including CFR and stress MBF [22••].
In addition, the clinical benefit of revascularization guided by the evaluation of CFC has been reported by Bober and collaborators [23], who nicely proved that regions with severely reduced CFC on baseline 82Rb PET showed a significant improvement in quantitative perfusion after revascularization while regions without reduced CFC demonstrated no perfusion improvement after analogue procedure.
Miura et al., using a different tracer, by mean 13 N-ammonia PET/CT, carried out an investigation on 137 patients without known CAD [24•]. The Authors proposed the modified CFC (mCFC) to assess microvascular dysfunction. Such parameter, integrating regional CFR and regional absolute stress perfusion, allows to define as “normal” or “minimally reduced” the flow in each left ventricle coronary territory with a color-based interpretation of the flow capacity. Interestingly, mCFC showed an incremental power for predicting cardiovascular mortality with a 25% prevalence of coronary microvascular dysfunction defined by mCFC.
The Future of the CFC Concept
The emerging role of CFC in the identification of patients with impaired coronary function opens the way to future investigations focused on challenging populations, such as women, diabetic and obese patients, not only with diagnostic implications but also aiming to achieve a deeper understanding of the pathophysiological patterns of coronary flow impairment.
As observed in the WISE study, women with reduced CFR were significantly more likely to have reduced exercise capacity and worst overall prognosis [25]. However, the relationship between functional capacity and coronary function still remains unclear and could be further explored with the CFC concept.
With regard to obese population, Upadhyaya et al. [26] nicely demonstrated, with 13 N-ammonia PET dynamic imaging, a U-turn pattern of the hyperaemic MBF across the range from normal weight, overweight, obesity, and morbid obesity. In detail, the Authors showed that hyperaemic MBF gradually declined from normal weight, overweight, and obesity, while it increased again in morbid obesity with comparable data to those obtained in subjects with normal weight. The interplay between fat and coronary function is still under investigation, and a potential estimation of CFC may help to obtain a big picture of such a complex mechanism. The topic may become even more appealing if we consider the added value of hybrid imaging in evaluating not only functional data from PET modality but also CT results obtained from the integrated approach [27].
Furthermore, despite the robust knowledge accomplished [28], an unquantifiable amount of data is still missing to achieve a complete understanding of the cross talk between coronary blood flow and physiological factors involved in the metabolic asset of diabetic patients.
The diagnostic and prognostic relevance of the CFC becomes even more interesting when looking at recent introduction of novel perfusion tracers such as the 18F-Flurpiridaz [29, 30, 31]. The available data have already demonstrated 18F-Flurpiridaz advantageous properties for CFR and MBF quantification. In addition, when compared with myocardial perfusion imaging by single photon emission tomography (SPECT), 18F-Flurpiridaz PET imaging shows better image quality and higher diagnostic value [31]. The potential implications of CFC estimation by this radiopharmaceutical may open the way to innovative applications for a deeper understanding of clinical meaning of flow heterogeneity.
Likewise, in the era of dynamic SPECT [32, 33], the opportunity to implement available quantification software with CFC estimation tool, thanks to the wide spread of cadmium-zinc-telluride technologies, may encourage innovative research on large scale and finally refine clinical practice routine in the personalized medicine direction.
It is widely accepted that the concept of CFC can be potentially applied to different imaging modalities that provide absolute quantification of myocardial perfusion including dynamic myocardial computed tomography perfusion (CTP) [34]. A CT-based approach boasts the advantage to deliver both functional and anatomical information at the same time. However, the still high radiation dose accounting for a mean effective radiation dose of 9 mSv makes these nuclear medicine techniques less appealing than the conventional ones [34, 35]. Nevertheless, it should be taken into account that dose optimization is among the main goals of hardware research, and a great reduction of administered dose is expected by the next generation imaging design.
Conclusions
The CFC parameter integrates CFR and stress MBF to improve the potential of dynamic imaging to identify coronary flow impairment. The routine evaluation of this metric may add diagnostic and prognostic value to clinical and conventional imaging data; however, its potential has not been fully investigated. The incoming PET tracers and the technological improvement of available non-invasive imaging modalities [36, 37] will be the bricks on which to build the future of CFC into clinical practice.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cheema AN, Yanagawa B, Verma S, Bagai A, Liu S. Myocardial infarction with nonobstructive coronary artery disease (MINOCA): a review of pathophysiology and management. Curr Opin Cardiol. 2021;36(5):589–96. https://doi.org/10.1097/HCO.0000000000000886.
•Malakar AK, Choudhury D, Halder B, Paul P, Uddin A, Chakraborty S. A review on coronary artery disease, its risk factors, and therapeutics. J Cell Physiol. 2019;234(10):16812–16823. https://doi.org/10.1002/jcp.28350. (This review reveals the absolute global and regional trends of the CAD and the importance and contribution of CAD for global health.)
Ralapanawa U, Sivakanesan R. Epidemiology and the magnitude of coronary artery disease and acute coronary syndrome: a narrative review. J Epidemiol Glob Health. 2021;11(2):169–77. https://doi.org/10.2991/jegh.k.201217.001.
Nappi C, Ponsiglione A, Acampa W, Gaudieri V, Zampella E, Assante R, Cuocolo R, Mannarino T, Dell’Aversana S, Petretta M, Imbriaco M, Cuocolo A. Relationship between epicardial adipose tissue and coronary vascular function in patients with suspected coronary artery disease and normal myocardial perfusion imaging. Eur Heart J Cardiovasc Imaging. 2019;20(12):1379–87. https://doi.org/10.1093/ehjci/jez182.
Nappi C, Gaudieri V, Acampa W, Arumugam P, Assante R, Zampella E, Mannarino T, Mainolfi CG, Imbriaco M, Petretta M, Cuocolo A. Coronary vascular age: AN alternate means for predicting stress-induced myocardial ischemia in patients with suspected coronary artery disease. J Nucl Cardiol. 2019;26(4):1348–55. https://doi.org/10.1007/s12350-018-1191-1.
Zampella E, Acampa W, Assante R, Nappi C, Gaudieri V, Mainolfi CG, Green R, Cantoni V, Panico M, Klain M, Petretta M, Slomka PJ, Cuocolo A. Combined evaluation of regional coronary artery calcium and myocardial perfusion by 82Rb PET/CT in the identification of obstructive coronary artery disease. Eur J Nucl Med Mol Imaging. 2018;45(4):521–9. https://doi.org/10.1007/s00259-018-3935-1.
Danad I, Raijmakers PG, Driessen RS, Leipsic J, Raju R, Naoum C, Knuuti J, Mäki M, Underwood RS, Min JK, Elmore K, Stuijfzand WJ, van Royen N, Tulevski II, Somsen AG, Huisman MC, van Lingen AA, Heymans MW, van de Ven PM, van Kuijk C, Lammertsma AA, van Rossum AC, Knaapen P. Comparison of coronary CT angiography, SPECT, PET, and hybrid imaging for diagnosis of ischemic heart disease determined by fractional flow reserve. JAMA Cardiol. 2017;2(10):1100–7. https://doi.org/10.1001/jamacardio.2017.2471.
Al Badarin FJ, Malhotra S. Diagnosis and prognosis of coronary artery disease with SPECT and PET. Curr Cardiol Rep. 2019;21(7):57. https://doi.org/10.1007/s11886-019-1146-4.
Aljizeeri A, Ahmed AI, Alfaris MA, Ahmed D, Farea J, Elneama A, Suliman I, Alharthi M, Ahmed A, Alsaileek A, Al-Mallah MH. Myocardial flow reserve and coronary calcification in prognosis of patients with suspected coronary artery disease. JACC Cardiovasc Imaging. 2021;14(12):2443–52. https://doi.org/10.1016/j.jcmg.2021.01.024.
Hoffman JIE. Problems of coronary flow reserve. Ann Biomed Eng. 2000;28:884–96. https://doi.org/10.1114/1.1308503.
Johnson NP, Gould KL. Integrating noninvasive absolute flow, coronary flow reserve, and ischemic thresholds into a comprehensive map of physiological severity. JACC Cardiovasc Imaging. 2012;5(4):430–40. https://doi.org/10.1016/j.jcmg.2011.12.014.
Hoffman JIE. Problems of Coronary Flow Reserve. Ann Biomed Eng. 2000;28:884–96. https://doi.org/10.1114/1.1308503.
•Gould KL, Johnson NP, Roby AE, Nguyen T, Kirkeeide R, Haynie M, Lai D, Zhu H, Patel MB, Smalling R, Arain S, Balan P, Nguyen T, Estrera A, Sdringola S, Madjid M, Nascimbene A, Loyalka P, Kar B, Gregoric I, Safi H, McPherson D. Regional, artery-specific thresholds of quantitative myocardial perfusion by PET associated with reduced myocardial infarction and death after revascularization in stable coronary artery disease. J Nucl Med. 2019;60(3):410–417. https://doi.org/10.2967/jnumed.118.211953(This paper showed that CFC by 82Rb PET, integrating regional CFR and regional absolute stress perfusion, provides automated, objective and artery-specific quantification of CAD severity.)
Gould KL, Bui L, Kitkungvan D, Patel MB. Reliability and reproducibility of absolute myocardial blood flow: does it depend on the PET/CT technology, the vasodilator, and/or the software? Curr Cardiol Rep. 2021;23(3):12. https://doi.org/10.1007/s11886-021-01449-8.
de Winter RW, Jukema RA, van Diemen PA, Schumacher SP, Driessen RS, Stuijfzand WJ, Everaars H, Bom MJ, van Rossum AC, van de Ven PM, Verouden NJ, Nap A, Raijmakers PG, Danad I, Knaapen P. The impact of coronary revascularization on vessel-specific coronary flow capacity and long-term outcomes: a serial [15O]H2O positron emission tomography perfusion imaging study. Eur Heart J Cardiovasc Imaging. 2022;23(6):743–752.
Loghin C, Sdringola S, Gould KL. Does coronary vasodilation after adenosine override endothelin-1-induced coronary vasoconstriction? Am J Physiol Heart Circ Physiol. 2007;292(1):H496-502. https://doi.org/10.1152/ajpheart.00818.2006.
Johnson NP, Gould KL. Physiology of endothelin in producing myocardial perfusion heterogeneity: a mechanistic study using darusentan and positron emission tomography. J Nucl Cardiol. 2013;20(5):835–44. https://doi.org/10.1007/s12350-013-9756-5.
Gould KL, Johnson NP. Quantitative coronary physiology for clinical management: the imaging standard. Curr Cardiol Rep. 2016;18(1):9. https://doi.org/10.1007/s11886-015-0684-7.
Kitkungvan D, Bui L, Johnson NP, Patel MB, Roby AE, Vejpongsa P, Babar AK, Madjid M, Nacimbene A, Kumar S, DeGolovine A, Gould KL. Quantitative myocardial perfusion positron emission tomography and caffeine revisited with new insights on major adverse cardiovascular events and coronary flow capacity. Eur Heart J Cardiovasc Imaging. 2019;20(7):751–62. https://doi.org/10.1093/ehjci/jez080.
Danad I, Szymonifka J, Schulman-Marcus J, Min JK. Static and dynamic assessment of myocardial perfusion by computed tomography. Eur Heart J Cardiovasc Imaging. 2016;17(8):836–44. https://doi.org/10.1093/ehjci/jew044.
Kitkungvan D, Lai D, Zhu H, Roby AE, Johnson NP, Steptoe DD, Patel MB, Kirkeeide R, Gould KL. Optimal adenosine stress for maximum stress perfusion, coronary flow reserve, and pixel distribution of coronary flow capacity by Kolmogorov-Smirnov analysis. Circ Cardiovasc Imaging. 2017;10(2):e005650. https://doi.org/10.1161/CIRCIMAGING.116.005650.
••Gould KL, Kitkungvan D, Johnson NP, Nguyen T, Kirkeeide R, Bui L, Patel MB, Roby AE, Madjid M, Zhu H, Lai D. Mortality prediction by quantitative PET perfusion expressed as coronary flow capacity with and without revascularization. JACC Cardiovasc Imaging. 2021;14(5):1020–1034. https://doi.org/10.1016/j.jcmg.2020.08.040. (This 10-years follow-up investigation showed that severely reduced CFC predicted higher death, myocardial infarction, stroke, and revascularization than any other severity 82Rb PET parameters.)
Bober RM, Milani RV, Oktay AA, Javed F, Polin NM, Morin DP. The impact of revascularization on myocardial blood flow as assessed by positron emission tomography. Eur J Nucl Med Mol Imaging. 2019;46(6):1226–39. https://doi.org/10.1007/s00259-019-04278-8.
•Miura S, Naya M, Kumamaru H, Ando A, Miyazaki C, Yamashita T. Prognostic value of modified coronary flow capacity by 13N-ammonia myocardial perfusion positron emission tomography in patients without obstructive coronary arteries. J Cardiol. 2022;79(2):247–256. https://doi.org/10.1016/j.jjcc.2021.09.001. (In this paper, the Authors using 13N-ammonia PET/CT showed that the modified CFC showed an incremental power for predicting cardiovascular mortality with a 25% prevalence of coronary microvascular dysfunction in 137 patients without known CAD.)
Handberg E, Johnson BD, Arant CB, Wessel TR, Kerensky RA, von Mering G, Olson MB, Reis SE, Shaw L, Bairey Merz CN, Sharaf BL, Sopko G, Pepine CJ. Impaired coronary vascular reactivity and functional capacity in women: results from the NHLBI Women’s Ischemia Syndrome Evaluation (WISE) Study. J Am Coll Cardiol. 2006;47(3 Suppl):S44–9. https://doi.org/10.1016/j.jacc.2005.10.023.
Upadhyaya A, Bhandiwad A, Lang J, Sadhu JS, Barrs C, Jain S, Brown DL, Peterson LR, Dehdashti F, Gropler RJ, Schindler TH. Coronary circulatory function with increasing obesity: a complex U-turn. Eur J Clin Invest. 2022;52(6):e13755. https://doi.org/10.1111/eci.13755.
Nappi C, Ponsiglione A, Acampa W, Gaudieri V, Zampella E, Assante R, Cuocolo R, Mannarino T, Dell’Aversana S, Petretta M, Imbriaco M, Cuocolo A. Relationship between epicardial adipose tissue and coronary vascular function in patients with suspected coronary artery disease and normal myocardial perfusion imaging. Eur Heart J Cardiovasc Imaging. 2019;20(12):1379–87. https://doi.org/10.1093/ehjci/jez182.
Severino P, D’Amato A, Netti L, Pucci M, Infusino F, Maestrini V, Mancone M, Fedele F. Myocardial ischemia and diabetes mellitus: role of oxidative stress in the connection between cardiac metabolism and coronary blood flow. J Diabetes Res. 2019;4(2019):9489826. https://doi.org/10.1155/2019/9489826.
Moody JB, Poitrasson-Rivière A, Hagio T, Buckley C, Weinberg RL, Corbett JR, Murthy VL, Ficaro EP. Added value of myocardial blood flow using 18F-flurpiridaz PET to diagnose coronary artery disease: the flurpiridaz 301 trial. J Nucl Cardiol. 2021;28(5):2313–29. https://doi.org/10.1007/s12350-020-02034-2.
Guehl NJ, Normandin MD, Wooten DW, Rozen G, Sitek A, Ruskin J, Shoup TM, Ptaszek LM, El Fakhri G, Alpert NM. Single-scan rest/stress imaging: validation in a porcine model with 18F-Flurpiridaz. Eur J Nucl Med Mol Imaging. 2017;44(9):1538–46. https://doi.org/10.1007/s00259-017-3684-6.
Berman DS, Maddahi J, Tamarappoo BK, et al. Phase II safety and clinical comparison with single-photon emission computed tomography myocardial perfusion imaging for detection of coronary artery disease: Flurpiridaz F 18 positron emission tomography. J Am Coll Cardiol. 2013;61(4):469–77.
Acampa W, Zampella E, Assante R, Genova A, De Simini G, Mannarino T, D’Antonio A, Gaudieri V, Nappi C, Buongiorno P, Mainolfi CG, Petretta M, Cuocolo A. Quantification of myocardial perfusion reserve by CZT-SPECT: a head-to-head comparison with 82Rubidium PET imaging. J Nucl Cardiol. 2021;28(6):2827–39. https://doi.org/10.1007/s12350-020-02129-w.
Otaki Y, Manabe O, Miller RJH, Manrique A, Nganoa C, Roth N, Berman DS, Germano G, Slomka PJ, Agostini D. Quantification of myocardial blood flow by CZT-SPECT with motion correction and comparison with 15O-water PET. J Nucl Cardiol. 2021;28(4):1477–86. https://doi.org/10.1007/s12350-019-01854-1.
Rossi A, Ferrante G. Imaging of coronary flow capacity: is there a role for dynamic CT perfusion imaging? Eur J Nucl Med Mol Imaging. 2019;46(9):1765–7. https://doi.org/10.1007/s00259-019-04362-z.
Hubbard L, Lipinski J, Ziemer B, Malkasian S, Sadeghi B, Javan H, et al. Comprehensive assessment of coronary artery disease by using first-pass analysis dynamic CT perfusion: validation in a swine model. Radiology. 2018;286:93–102.
Ponsiglione A, Ascione R, Nappi C, Imbriaco M, Klain M, Cuocolo R, Cuocolo A, Petretta M. Cardiac hybrid imaging: novel tracers for novel targets. J Geriatr Cardiol. 2021;18(9):748–58. https://doi.org/10.11909/j.issn.1671-5411.2021.09.006.
Green R, Cantoni V, Acampa W, Assante R, Zampella E, Nappi C, Gaudieri V, Mannarino T, Cuocolo R, Petretta M, Cuocolo A. Prognostic value of coronary flow reserve in patients with suspected or known coronary artery disease referred to PET myocardial perfusion imaging: a meta-analysis. J Nucl Cardiol. 2021;28(3):904–18. https://doi.org/10.1007/s12350-019-02000-7.
Funding
Open access funding provided by Università degli Studi di Napoli Federico II within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiac Nuclear Imaging
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nappi, C., Ponsiglione, A., Falzarano, M. et al. Insights into Myocardial Perfusion PET Imaging: the Coronary Flow Capacity. Curr Cardiovasc Imaging Rep 15, 37–41 (2022). https://doi.org/10.1007/s12410-022-09568-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12410-022-09568-8