Abstract
Introduction
Spinal muscular atrophy (SMA) is a neurogenic disorder associated with progressive loss of muscle function, respiratory failure, and premature mortality. This study aimed to describe and compare real-world health care resource utilization (HCRU) and costs for US patients with SMA treated with disease-modifying treatments, including onasemnogene abeparvovec, nusinersen, and/or risdiplam.
Methods
This study used claims and structured electronic medical record data from the HealthVerity claims database (January 1, 2017–March 31, 2021). Eligible patients were aged ≤ 2 years at index (treatment initiation or switch), diagnosed with SMA, had ≥ 1 pharmacy/medical claim for onasemnogene abeparvovec, nusinersen, and/or risdiplam, and continuous enrollment ≥ 1 month pre- and ≥ 2 months post-index. SMA-related HCRU and costs during the study period (> 12 months post-index) were compared between treatment groups before and after propensity score weighting. Costs were adjusted to 2021 USD.
Results
Of 74 included patients, 62 (83.8%) received nusinersen and 12 (16.2%) received onasemnogene abeparvovec (monotherapy, n = 9; onasemnogene abeparvovec after nusinersen [switching], n = 3). After weighting, nusinersen-treated patients had greater annual numbers of inpatient (mean 5.3 nusinersen vs. 1.8 onasemnogene abeparvovec) and emergency department (mean 3.0 nusinersen vs. 1.5 onasemnogene abeparvovec; p < 0.05) visits, and greater annual SMA-related medical costs (mean $78,446 nusinersen vs. $29,438 onasemnogene abeparvovec; mean difference $49,007, p < 0.05) than onasemnogene abeparvovec-treated patients. Onasemnogene abeparvovec-treated patients incurred greater SMA-treatment pharmacy costs than nusinersen-treated patients (mean $2,241,875 onasemnogene abeparvovec vs. $693,191 nusinersen; mean difference $1,548,684, p < 0.05).
Conclusions
SMA is associated with substantial economic burden. Patients treated with onasemnogene abeparvovec had greater SMA treatment-related pharmacy costs but lower SMA-related HCRU and medical costs compared with patients receiving nusinersen monotherapy.
Plain Language Summary
Spinal muscular atrophy (SMA) is a crippling neurodegenerative disease with symptoms of respiratory failure, muscle weakness and loss of function, and premature death. This study describes and compares real-world health care resource utilization (HCRU) and costs for US patients with SMA receiving current treatments (e.g., onasemnogene abeparvovec, nusinersen, risdiplam) using claims and electronic medical record data from a US claims database. Patients included (n = 74) in the study were ≤ 2 years old at treatment initiation/switching of treatments (index), had been diagnosed with SMA and had one or more pharmacy or medical claim for onasemnogene abeparvovec, nusinersen, or risdiplam, and were continuously enrolled for ≥ 1 month before and ≥ 2 months after index. SMA-related HCRU and costs during the study period (up to 12 months post-index) were compared between treatment groups before and after propensity score weighting, with costs adjusted to 2021 USD. Propensity score weighting allows better comparison between patients in treatment and comparison groups by assigning patients different “weights.” This weighting allows investigators to be certain that differences in outcomes between patient groups are a result of a particular treatment. After weighting, nusinersen-treated patients had a greater number of inpatient and emergency department visits and greater SMA-related medical costs annually, whereas patients who received onasemnogene abeparvovec had greater pharmacy costs. Our study indicates the greater medical costs among patients receiving nusinersen were largely driven by invasive procedures, such as tracheostomy and gastrostomy, that required hospitalization, but the exact mechanism of greater HCRU/costs associated with nusinersen needs to be further assessed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Survival motor neuron (SMN)-targeting disease-modifying treatments (DMTs) such as onasemnogene abeparvovec and nusinersen are established standard of care for patients with spinal muscular atrophy (SMA), but real-world data comparing the economic impact associated with different DMTs are limited. |
What was learned from this study? |
We found that SMA-related health care resource utilization (HCRU) and medical costs were lower for children treated with onasemnogene abeparvovec than for children receiving nusinersen monotherapy. The greater medical costs among children treated with nusinersen may be explained by greater use of invasive procedures (e.g., tracheostomy, gastrostomy) in inpatient settings as well as unobserved or unbalanced patient characteristics between the two treatment groups. |
SMA is associated with substantial economic burden and the literature demonstrates that HCRU and health care costs associated with SMA reflect a common theme of the costliness of this disease as reported in previous US-based studies on its economic burden. |
Introduction
Spinal muscular atrophy (SMA) is a neurogenetic disorder characterized by the degeneration of anterior horn cells in the spinal cord and brainstem motor nuclei, leading to progressive muscular atrophy and impairment of motor neuron function [1]. It is an autosomal recessive disorder most commonly caused by the loss or mutation of the survival motor neuron 1 (SMN1) gene on chromosome 5q13, resulting in a deficiency of the SMN1 protein [2, 3]. SMA has an estimated incidence of 1:6000 to 1:10,000 live births [4,5,6,7,8]. The clinical severity of SMA varies widely and it is classified into subtypes according to age at disease onset and motor function achieved, ranging from the most severe (SMA type 0, prenatal onset) to the mildest (SMA type 4, adult onset) [4, 5]. As SMA is associated with progressive respiratory insufficiency and respiratory failure, premature mortality is a common consequence, particularly with SMA types 0 and 1 [9]. Indeed, SMA was the most common monogenic cause of infant mortality before the advent of disease-modifying treatments (DMTs) [8].
The management and prognosis for patients with SMA have evolved following recent advances in medical treatment focusing on motor neuron protection, muscle preservation, and gene enhancement or replacement [10]. There are currently three DMTs approved by the US Food and Drug Administration (FDA) for the treatment of SMA: nusinersen (approved in 2016) [11], onasemnogene abeparvovec (2019) [12], and risdiplam (2020) [13]. Nusinersen, an antisense oligonucleotide, alters the messenger ribonucleic acid (mRNA) splicing pattern of the SMN2 gene to increase production of full-length SMN protein [14]. Nusinersen is designed for lifelong intrathecal administration and, after four loading doses, requires a maintenance dose once every 4 months. Risdiplam is a small molecule SMN2-directed RNA splicing modifier that increases exon 7 inclusion in SMN2 mRNA [15, 16]. Risdiplam is designed for daily oral administration and is a lifelong treatment. Onasemnogene abeparvovec is a gene therapy that replaces the mutated SMN1 gene with normal SMN1 to increase SMN protein expression in motor neurons to prevent cell death, improve neuronal and muscular function, and increase overall patient survival [17,18,19,20]. It is delivered as a one-time, single-dose, intravenous infusion and indicated for the treatment of pediatric patients aged < 2 years with SMA and biallelic mutations of the SMN1 gene.
The potentially devastating effects of SMA are associated with substantial clinical and economic burdens on patients, families, caregivers, and health care systems [21], although only a few studies have examined this burden in the real world [21,22,23,24,25]. Given the evolving treatment landscape of SMA, studies using real-world data that assess outcomes after treatment with DMTs are needed. This study focused on describing and comparing real-world health care resource utilization (HCRU) and costs between patients with SMA treated with DMTs in the United States.
Methods
Data Source
This study used data from HealthVerity claims database, spanning January 1, 2017 to March 31, 2021. Specifically, data from HealthVerity Private Source 20 (PS20), Private Source 17 (PS17), and structured electronic medical records (EMRs) were used. PS20 and PS17 are closed claims datasets with over 115 million and 96 million patients, respectively. They include medical and pharmacy claims with information on inpatient and outpatient diagnoses, procedures, physician-administered medications, and the costs of paid claims and pharmacy transactions from retail and specialty pharmacies. The EMR dataset contained information from over 7000 ambulatory care practices across the United States and included structured data on diagnoses, laboratory results, and treatments, as well as unstructured physician notes on family history and clinical observations. All data were linked via a unique, anonymized patient identifier. PS20, PS17, and structured EMR data were used to describe patient characteristics, while PS20 data were used to describe HCRU and costs. The database is nationally representative in terms of age, sex, and geographic region.
Because this study used prior collected and anonymized data, institutional review board and Declaration of Helsinki approval was not required.
Study Population
Patients were included in the study if they met the following criteria: (1) had ≥ 1 diagnosis of SMA (International Classification of Disease, 10th revision [ICD-10-CM] codes G12.0, G12.1, G12.9); (2) had ≥ 1 pharmacy and/or medical claim for onasemnogene abeparvovec, nusinersen, and/or risdiplam (see claims codes for SMA treatment in Table S1 in the supplementary material); (3) were aged ≤ 2 years at the index date; (4) had ≥ 1 clinical activity in PS20 claims; and (5) had continuous enrollment for ≥ 1 month prior to and ≥ 2 months after the index date.
The index was defined as the date of initiation of monotherapy or first treatment switch after the earliest SMA diagnosis. The baseline period was defined as 1 month before the index date. The study period spanned from the index date until the earlier of the end of data availability (i.e., March 31, 2021) or 1 year of follow-up.
Study Covariates and Outcomes
Patient characteristics assessed during the baseline period included sex, age at the index date and at SMA diagnosis, region of residence, type of health care insurance plan (e.g., Medicaid, private/commercial, unknown) at the index date, SMA type, weight at the index date, newborn screening, and SMA-related comorbidities (see claims code for comorbidities in Table S2 in the supplementary material). SMA type was identified using an established claims-based algorithm based on the age of the patient and symptoms, procedures, and use of durable medical equipment [22, 23]. Newborn screening was a binary variable based on whether patients were born at or after the implementation of newborn screening for SMA in patients’ birth states [26,27,28].
SMA-related HCRU and costs, defined as claims with a diagnosis of SMA, were estimated during the study period. SMA-related HCRU included inpatient visits, total days of hospitalization, outpatient visits, skilled nursing facility (SNF) visits, emergency department (ED) visits, home health visits, specific services and procedures, and mobility device use. Annualized numbers of HCRU were estimated for each patient by dividing the total number of events during the follow-up period by the duration of follow-up in years. The annualized numbers of HCRU were used to permit comparison with different follow-up times. The mean, standard deviation (SD), median, and interquartile range (IQR) of follow-up time were summarized for each treatment group. The percentages of patients with any medical visits were also evaluated in the study period by visit type.
SMA-related total health care, medical, and pharmacy costs were also assessed from a US third-party payer perspective during the study period. Specific cost categories included inpatient, outpatient, SNF, ED, home health, specific services and procedures, mobility device use, and pharmacy costs for SMA treatment(s). SMA treatment costs of nusinersen and onasemnogene abeparvovec were calculated on the basis of the dose information reported in the data and the wholesale acquisition cost (nusinersen, $127,500/12 mg; onasemnogene abeparvovec, $2,125,000/dose in 2019 US dollars [USD]) [29]. Annualized costs were calculated for each patient by dividing the total costs accrued during the follow-up period by the duration of follow-up in years. Costs were adjusted to 2021 USD according to the Personal Consumption Expenditure Price Index (Health Care) from the US Bureau of Economic Analysis [30].
Statistical Analyses
Continuous variables were summarized using means and SDs; categorical variables were summarized using counts and proportions. Both unadjusted and adjusted comparisons between treatment groups were conducted. Propensity score weighting was used to adjust for differences in the baseline characteristics between treatment groups [31, 32]. Adjusted comparisons controlled for baseline covariates selected on the basis of clinical relevance, including patient age at the index date, sex, and SMA type. Means and frequencies of baseline characteristics, before and after weighting, were compared using standardized mean differences (SMDs). SMDs below the commonly accepted threshold of 0.1 indicated that the characteristics of the two groups were balanced [33].
Baseline characteristics, HCRU, and costs were compared between treatment groups before and after weighting using Wilcoxon rank sum for continuous variables and chi-square tests for categorical variables. For categorical variables with counts less than five, Fisher’s exact test was used before weighting. Mean differences for SMA-related HCRU and costs were calculated as the difference between the nusinersen monotherapy and onasemnogene abeparvovec groups. All analyses were conducted using R (v3.6.1; R Core Team). A p < 0.05 was the threshold for statistical significance based on two-sided tests.
Results
Sample Selection
Of 74 patients who met the sample selection criteria and were included in the study, 62 (83.8%) received nusinersen monotherapy and 12 (16.2%) received onasemnogene abeparvovec (nine received onasemnogene abeparvovec monotherapy and three received nusinersen followed by onasemnogene abeparvovec) (Fig. 1). No patients received risdiplam and met the inclusion criteria during the study period.
Sample selection flowchart. SMA, spinal muscular atrophy. aThe index date was defined as the date of monotherapy initiation (for single-agent treatment) or the date of first treatment switch (for multiple treatments). bAge at the index date was estimated on the basis of the gap between year/month of birth and year/month of index date. Month of birth was assumed to be (1) the month of first service date if the first service date happened in the same year of birth, or (2) July of the birth year if the year of first service date was different from the year of birth, due to lack of data. cClinical activity was identified using both medical claims and pharmacy data
Patient Characteristics
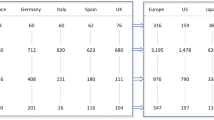
The demographics and clinical characteristics of patients in the nusinersen monotherapy and onasemnogene abeparvovec groups are listed in Table 1. Before weighting, patients treated with onasemnogene abeparvovec were on average older at index (mean age of onasemnogene abeparvovec vs. nusinersen, 14.2 vs. 13.1 months) and at SMA diagnosis (mean age of onasemnogene abeparvovec vs. nusinersen, 8.2 vs. 7.4 months), less likely to be female (onasemnogene abeparvovec vs. nusinersen, 25% vs. 50%) and have SMA type 2 (vs. type 1) (onasemnogene abeparvovec vs. nusinersen, 58.3% vs. 88.7%), and more likely to have newborn screening for SMA (onasemnogene abeparvovec vs. nusinersen, 8.3% vs. 1.6%) compared with those treated with nusinersen monotherapy (SMDs > 0.1). Region of residence was similar between nusinersen monotherapy and onasemnogene abeparvovec-treated patients. About half of patients treated with nusinersen monotherapy and 41.7% of onasemnogene abeparvovec-treated patients were enrolled in Medicaid. Of SMA-related comorbidities, acute respiratory failure, dysphagia, failure to thrive, and scoliosis were more common among the nusinersen monotherapy versus the onasemnogene abeparvovec group. All patients in the onasemnogene abeparvovec group had index years between 2019 and 2021 compared with 32.3% of the nusinersen monotherapy group.
After weighting, the proportions of female patients, SMA type, and some SMA-related comorbidities (acute respiratory failure and muscle weakness) were similar between the nusinersen monotherapy and onasemnogene abeparvovec groups (SMDs < 0.1) (Table 1). Compared with patients treated with nusinersen monotherapy, those treated with onasemnogene abeparvovec were younger at index date (mean age of onasemnogene abeparvovec vs. nusinersen, 12.3 vs. 13.4 months) and slightly older at SMA diagnosis (mean age of onasemnogene abeparvovec vs. nusinersen, 7.9 vs. 7.2 months). Onasemnogene abeparvovec-treated patients were more likely to reside in the South (onasemnogene abeparvovec vs. nusinersen, 75.4% vs. 52.9%) and have dyspnea and respiratory anomalies (onasemnogene abeparvovec vs. nusinersen, 60.0% vs. 39.9%) and feeding difficulties and mismanagement (onasemnogene abeparvovec vs. nusinersen, 61.5% vs. 47.7%), but were less likely to be enrolled in Medicaid (onasemnogene abeparvovec vs. nusinersen, 23.5% vs. 48.4%). Patients treated with onasemnogene abeparvovec were also less likely to demonstrate dysphagia (onasemnogene abeparvovec vs. nusinersen, 8.6% vs. 30.0%), failure to thrive (onasemnogene abeparvovec vs. nusinersen, 13.7% vs. 26.4%), and scoliosis (onasemnogene abeparvovec vs. nusinersen, 0.0% vs. 13.4%).
SMA-Related HCRU
Generally greater percentages of HCRU were observed for patients treated with nusinersen monotherapy compared with those treated with onasemnogene abeparvovec during the study period, both before and after weighting. Before weighting, greater percentages of the nusinersen monotherapy group incurred all categories of HCRU compared with the onasemnogene abeparvovec group, except for outpatient visits (100% for both groups). Particularly, the proportion of patients having any inpatient visits was significantly greater for the nusinersen monotherapy group (nusinersen vs. onasemnogene abeparvovec, 72.6% vs. 25.0%, p < 0.05) (Table 2). Similarly, the nusinersen monotherapy group had greater annualized numbers of all categories of HCRU except for other visits (onasemnogene abeparvovec vs. nusinersen, 5.8 vs. 5.1). Before weighting, a greater percentage of nusinersen monotherapy-treated vs. onasemnogene abeparvovec-treated patients required mechanical ventilation support (nusinersen vs. onasemnogene abeparvovec, 69.4% vs. 33.3%, p < 0.05), braces for mobility (nusinersen vs. onasemnogene abeparvovec, 51.6% vs. 16.7%; p < 0.05), nutritional support (nusinersen vs. onasemnogene abeparvovec, 74.2% vs. 50.0%), and speech therapy (nusinersen vs. onasemnogene abeparvovec, 59.7% vs. 41.7%). Onasemnogene abeparvovec-treated patients were more likely to require sleep studies than nusinersen monotherapy-treated patients (nusinersen vs. onasemnogene abeparvovec, 12.9% vs. 25.0%).
The magnitude of the differences in HCRU between the two treatment groups was slightly attenuated after weighting. Still, greater percentages of the nusinersen monotherapy group incurred any inpatient (nusinersen vs. onasemnogene abeparvovec, 72.9% vs. 48.1%), ED (nusinersen vs. onasemnogene abeparvovec, 70.5% vs. 69.0%), SNF (nusinersen vs. onasemnogene abeparvovec, 10.0% vs. 0.0%), or skilled nursing in-home visits (nusinersen vs. onasemnogene abeparvovec, 5.7% vs. 0.0%) than the onasemnogene abeparvovec group after weighting (Table 2). Similarly, after weighting, patients treated with nusinersen monotherapy had greater mean annualized numbers of inpatient (nusinersen vs. onasemnogene abeparvovec, 5.3 vs. 1.8 visits/year), ED (nusinersen vs. onasemnogene abeparvovec, 3.0 vs. 1.5 visits/year, p < 0.05), and SNF visits (nusinersen vs. onasemnogene abeparvovec, 1.2 vs. 0.0 visits/year) than those treated with onasemnogene abeparvovec. The mean annualized number of outpatient visits was similar between the two treatment groups (nusinersen vs. onasemnogene abeparvovec, 48.4 vs. 48.1 visits/year). Patients treated with nusinersen monotherapy had slightly lower numbers of home visits (nusinersen vs. onasemnogene abeparvovec, 6.5 vs. 8.3 visits/year) and other visits (nusinersen vs. onasemnogene abeparvovec, 5.0 vs. 6.7 visits/year). After weighting, greater percentages of patients treated with nusinersen monotherapy versus onasemnogene abeparvovec received mechanical ventilation support (nusinersen vs. onasemnogene abeparvovec, 69.9% vs. 54.1%), nutritional support (nusinersen vs. onasemnogene abeparvovec, 74.0% vs. 65.0%) and lower percentages of patients treated with nusinersen monotherapy versus onasemnogene abeparvovec required sleep studies (11.9% vs. 51.1%, respectively), orthopedic surgery (6.1% vs. 13.7%, respectively), and a pediatric wheelchair (23.0% vs. 53.8%, respectively) during the study period.
SMA-Related Health Care Costs
Except for SMA treatment costs, nusinersen monotherapy-treated patients incurred generally greater health care costs compared with onasemnogene abeparvovec-treated patients, both before and after weighting. Before weighting, patients treated with onasemnogene abeparvovec had lower total SMA-related medical costs with a mean difference of − $61,888, compared with patients treated with nusinersen monotherapy ($12,432 and $74,320, respectively). After weighting, patients treated with onasemnogene abeparvovec consistently incurred lower total SMA-related medical costs annually, with a mean difference of − $49,007 (nusinersen vs. onasemnogene abeparvovec, $78,446 vs. $29,438, p < 0.05), primarily driven by lower inpatient costs with a mean difference of − $46,975 (nusinersen vs. onasemnogene abeparvovec, $68,106 vs. $21,130, p < 0.05) and lower ED costs with a mean difference of − $1547 (nusinersen vs. onasemnogene abeparvovec, $2058 vs. $511, p < 0.05) (Table 3). Outpatient and SNF costs were all numerically lower among onasemnogene abeparvovec-treated patients compared with nusinersen monotherapy-treated patients, before and after weighting (Fig. 2).
Patients treated with nusinersen monotherapy incurred significantly lower SMA treatment costs than those treated with onasemnogene abeparvovec, with a mean difference of $1,548,684 after weighting (p < 0.05). Overall, onasemnogene abeparvovec-treated patients had significantly greater total annualized costs (medical and pharmacy) than nusinersen monotherapy-treated patients, with a mean difference of $1,499,676 after weighting (p < 0.05), largely driven by SMA treatment costs.
After weighting, patients treated with nusinersen monotherapy incurred significantly greater costs related to mechanical ventilation support (nusinersen vs. onasemnogene abeparvovec, $15,109 vs. $4536; mean difference − $10,573, p < 0.05), nutritional support (nusinersen vs. onasemnogene abeparvovec, $31,860 vs. $6460; mean difference − $25,399, p < 0.05), and braces (nusinersen vs. onasemnogene abeparvovec, $392 vs. $132; mean difference − $260; p < 0.05) compared with those treated with onasemnogene abeparvovec. Although patients treated with onasemnogene abeparvovec had greater costs related to speech therapy, sleep studies, and pediatric wheelchair use, the mean differences were small ($560, $507, and $652, respectively) and not statistically significant.
Discussion
There is limited real-world evidence on the economic outcomes of patients with SMA after treatment with DMTs. This study assessed SMA-related HCRU and health care costs for pediatric patients with SMA aged up to 2 years at the time of DMT treatment initiation or switch. Between January 1, 2017 and March 31, 2021, approximately 84% of patients were treated with nusinersen monotherapy and 16% with onasemnogene abeparvovec (including 4% of patients who received nusinersen followed by onasemnogene abeparvovec). This distribution was expected given the earlier FDA approval date of nusinersen (2016) compared with onasemnogene abeparvovec (2019). We did not identify any patients who received risdiplam, possibly because risdiplam was only approved in adults and children 2 months of age and older during the study period and its approval date (August 7, 2020) was close to the end of the study period, so patients receiving risdiplam did not meet the inclusion criterion of at least 2 months’ follow-up.
The current findings of high HCRU and health care costs associated with SMA reflect a common theme of the costliness of this disease as reported in previous US-based studies on its economic burden [21, 22, 24, 25, 32,33,34]. For example, a study by Belter et al. [34] assessed the all-cause inpatient and outpatient utilization and costs for untreated patients with SMA using 2012–2016 claims data (Truven Health Analytics MarketScan). They reported that the mean annualized inpatient and outpatient costs were $118,609 and $55,538 (2019 USD), respectively, for infants aged < 1 year, and were $26,940 and $73,093 for children aged 1–3 years. Inpatient costs were the primary cost driver for untreated infant patients, similar to the present results, although outpatient costs were the main cost driver for children over the age of 1 year. Another study by Lee et al. [35], using 2005–2013 hospitalization data from the Healthcare Cost and Utilization Project and the Center for Health Information and Analysis, reported that the mean annualized inpatient cost for children with severe, untreated SMA was $104,197 (2017 USD), although they did not report the patients’ ages.
The inpatient and outpatient costs estimated in these prior studies of untreated patients with SMA (i.e., during the pre-DMT era) are generally greater than those observed for the present cohort treated with onasemnogene abeparvovec (mean costs after weighting $21,130 [inpatient] and $7430 [outpatient]) or nusinersen monotherapy (mean costs after weighting $68,106 [inpatient] and $7971 [outpatient]). The difference in costs could be explained by differing outcome measures (types of HCRU and costs), year of costs, and the ages and disease severity of the study populations. For example, all-cause HCRU and costs were examined in the prior studies versus SMA-related HCRU and costs in our study. In addition, our study included patients ≤ 2 years old with SMA types 1 or 2, who may have differing HCRU and costs compared with more broadly defined age or disease severity groups. Nonetheless, our findings indicate that treatment with DMTs manages SMA symptom progression and reduces the associated economic burden, as reflected in lower inpatient and outpatient costs for patients treated with DMTs. In addition, as the baseline period in our study was only 1 month, the HCRU and costs during the baseline period were not directly comparable with the annualized HCRU and costs of untreated patients in prior studies over longer follow-up periods.
Few studies have reported HCRU and costs among DMT-treated patients with SMA in the United States, although Droege et al. [22] estimated SMA-related HCRU and costs for patients with SMA type 1 who were treated with nusinersen using data from Symphony Health’s Integrated Dataverse open claims database. They reported that mean annualized total medical costs (excluding nusinersen-related treatment costs) were $92,618, similar to but somewhat greater than the medical costs of the nusinersen monotherapy-treated patients in our study ($78,446 after weighting).
Despite greater SMA treatment costs, patients treated with onasemnogene abeparvovec had lower SMA-related HCRU and medical costs compared with those treated with nusinersen monotherapy during the study period. For example, lower percentages of patients treated with onasemnogene abeparvovec had any inpatient (48% vs. 73% after weighting), SNF (0% vs. 10%), and in-home skilled nursing (0% vs. 6%) visits compared with those treated with nusinersen monotherapy. Patients treated with onasemnogene abeparvovec also had fewer annual inpatient admissions, ED visits, and SNF visits, and significantly fewer outpatient and in-home visits. In addition, onasemnogene abeparvovec-treated patients were less likely to require mechanical ventilation support, nutritional support, gastrostomy, and braces but more likely to participate in sleep studies and use a wheelchair compared with nusinersen monotherapy patients. Compared with patients treated with nusinersen monotherapy, onasemnogene abeparvovec-treated patients had significantly lower costs related to mechanical ventilation support, nutritional support, gastrostomy, and braces, but greater costs related to sleep studies and speech therapy. These findings were generally consistent before and after weighting, although their magnitude was attenuated post-weighting. As the follow-up period (up to 1 year) was relatively short in our study, future studies with longer follow-up data will be helpful to further assess the long-term economic impact of DMTs.
The results of this study are subject to several limitations, some of which are common to retrospective cohort studies using claims or EMR data. Secondary claims data are subject to coding errors or omission. The diagnoses of diseases may be incorrectly coded or the diagnosis code may be included as a rule-out criterion. Key variables that may impact the evaluation of HCRU and costs, such as SMA type, newborn screening status, and SMA treatment costs, were not directly available in the data. Therefore, proxy measures were constructed using claims-based algorithms. While propensity score weighting was used to balance the key baseline characteristics between treatment groups, there is a possibility of residual confounding. Differences in the HCRU and costs between treatment groups could be due to heterogeneity in unobserved or unbalanced baseline characteristics. Because of the limited data availability for patients receiving recently approved DMTs, HCRU and health care costs were examined in the first year of treatment. Data with a longer follow-up period will be helpful to evaluate the economic burden associated with SMA over more extended time periods. In addition, the extrapolation of the annualized HCRU and health care costs for patients with a follow-up of < 1 year assumed that the accumulation of HCRU and costs are linear over time. Once violated, the estimates may be not reliable, especially for patients with limited data over a short follow-up period (e.g., 2 or 3 months). This is less likely to be an issue in our study given that the median follow-up was 12 months and over 75% of patients had ≥ 9 months’ follow-up. Finally, SMA-related societal costs (e.g., loss of productivity and informal care), which were not included in this study because of the lack of such data in claims, are expected to decrease after treatment with DMTs.
Conclusions
SMA types 1 and 2 are rapidly progressing, devastating diseases associated with substantial utilization of HCRU and greater health care costs, but can be treated with innovative DMTs. The results of this real-world study indicated SMA-related HCRU and medical costs were lower for patients treated with onasemnogene abeparvovec compared with patients receiving nusinersen monotherapy. Future studies to examine SMA treatment patterns as the clinical landscape continues to evolve, and to evaluate the long-term economic burden associated with SMA management, are recommended.
References
Prior T, Leach M, Finanger E. Spinal muscular atrophy. In: Adam M, Everman D, Mirzaa G, editors. GeneReviews. Seattle: University of Washington; 2022.
Lefebvre S, Bürglen L, Reboullet S, et al. Identification and characterization of a spinal muscular atrophy-determining gene. Cell. 1995;80(1):155–65.
Schmalbruch H, Haase G. Spinal muscular atrophy: present state. Brain Pathol. 2001;11(2):231–47.
Groen EJN, Talbot K, Gillingwater TH. Advances in therapy for spinal muscular atrophy: promises and challenges. Nat Rev Neurol. 2018;14(4):214–24.
Waldrop MA, Kolb SJ. Current treatment options in neurology-SMA therapeutics. Curr Treat Options Neurol. 2019;21(6):25.
Ben-Shachar S, Orr-Urtreger A, Bardugo E, et al. Large-scale population screening for spinal muscular atrophy: clinical implications. Genet Med. 2011;13(2):110–4.
D’Amico A, Mercuri E, Tiziano FD, et al. Spinal muscular atrophy. Orphanet J Rare Dis. 2011;6(1):1–10.
Darras BT. Spinal muscular atrophies. Pediatr Clin North Am. 2015;62(3):743–66.
Ioos C, Leclair-Richard D, Mrad S, et al. Respiratory capacity course in patients with infantile spinal muscular atrophy. Chest. 2004;126(3):831–7.
Dangouloff T, Servais L. Clinical evidence supporting early treatment of patients with spinal muscular atrophy: current perspectives. Ther Clin Risk Manag. 2019;15:1153.
SPINRAZA. Highlights of prescribing information. Biogen; 2023 [updated 2023 February; cited 2023 March 31]. https://www.spinraza.com/content/dam/commercial/spinraza/caregiver/en_us/pdf/spinraza-prescribing-information.pdf.
ZOLGENSMA. Highlights of prescribing information. Novartis Gene Therapies, Inc.; 2023 [updated 2023 February; cited 2023 March 31]. https://www.novartis.com/us-en/sites/novartis_us/files/zolgensma.pdf.
EVRYSDI. Highlights of prescribing information. Genentech, Inc.; 2023 [updated 2023 March; cited 2023 March 31]. https://www.gene.com/download/pdf/evrysdi_prescribing.pdf.
Finkel RS, Mercuri E, Darras BT, et al. Nusinersen versus sham control in infantile-onset spinal muscular atrophy. N Engl J Med. 2017;377(18):1723–32.
Ratni H, Ebeling M, Baird J, et al. Discovery of risdiplam, a selective survival of motor neuron-2 (SMN2) gene splicing modifier for the treatment of spinal muscular atrophy (SMA). J Med Chem. 2018;61(15):6501–17.
Mercuri E, Deconinck N, Mazzone ES, et al. Safety and efficacy of once-daily risdiplam in type 2 and non-ambulant type 3 spinal muscular atrophy (SUNFISH part 2): a phase 3, double-blind, randomised, placebo-controlled trial. Lancet Neurol. 2022;21(1):42–52.
Mendell JR, Al-Zaidy S, Shell R, et al. Single-dose gene-replacement therapy for spinal muscular atrophy. N Engl J Med. 2017;377(18):1713–22.
Mendell JR, Al-Zaidy SA, Lehman KJ, et al. Five-year extension results of the phase 1 START trial of onasemnogene abeparvovec in spinal muscular atrophy. JAMA Neurol. 2021;78(7):834–41.
Day JW, Finkel RS, Chiriboga CA, et al. Onasemnogene abeparvovec gene therapy for symptomatic infantile-onset spinal muscular atrophy in patients with two copies of SMN2 (STR1VE): An open-label, single-arm, multicentre, phase 3 trial. Lancet Neurol. 2021;20(4):284–93.
Mercuri E, Muntoni F, Baranello G, et al. Onasemnogene abeparvovec gene therapy for symptomatic infantile-onset spinal muscular atrophy type 1 (STR1VE-EU): an open-label, single-arm, multicentre, phase 3 trial. Lancet Neurol. 2021;20(10):832–41.
Armstrong EP, Malone DC, Yeh W-S, et al. The economic burden of spinal muscular atrophy. J Med Econ. 2016;19(8):822–6.
Droege M, Sproule D, Arjunji R, et al. Economic burden of spinal muscular atrophy in the United States: a contemporary assessment. J Med Econ. 2020;23(1):70–9.
Gauthier-Loiselle M, Cloutier M, Toro W, et al. Nusinersen for spinal muscular atrophy in the United States: findings from a retrospective claims database analysis. Adv Ther. 2021;38:5809–28.
Dabbous O, Seda J, Sproule D. Economic burden of infant-onset (type 1) spinal muscular atrophy: a retrospective claims database analysis. Value Health. 2018;21:S251.
Goble J, Dai D, Boulos F, et al. The economic burden of spinal muscular atrophy patients in a commercially-insured population in the United States. Neurology. 2019;92(15_suppl):P1.6–054.
Hale JE, Darras BT, Swoboda KJ, et al. Massachusetts’ findings from statewide newborn screening for spinal muscular atrophy. Int J Neonatal Screen. 2021;7(2):26.
Utah Department of Health & Human Services. All Utah newborns now tested for spinal muscular atrophy. [updated 2018 January 31; cited 2023 January 30]. https://health.utah.gov/featured-news/all-utah-newborns-now-tested-for-spinal-muscular-atrophy.
NewSTEPs. Newborn screening status for all disorders [updated 2023 March 31; cited 2023 January 30]. https://www.newsteps.org/resources/data-visualizations/newborn-screening-status-all-disorders?q=resources/newborn-screening-status-all-disorders.
Merative. Micromedex (electronic version). [updated 2023; cited 2023 January 30]. https://www.micromedexsolutions.com.
United States Bureau of Economic Analysis. Personal consumption expenditures price index. [updated 2023 March 31; cited 2022 December 6]. https://www.bea.gov/data/personal-consumption-expenditures-price-index.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–79.
Normand ST, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54(4):387–98.
Belter L, Cruz R, Kulas S, et al. Economic burden of spinal muscular atrophy: an analysis of claims data. J Mark Access Health Policy. 2020;8(1):1843277.
Lee M, França UL, Graham RJ, et al. Pre-nusinersen hospitalization costs of children with spinal muscular atrophy. Pediatr Neurol. 2019;92:3–5.
Acknowledgements
Author Contributions
Walter Toro, Min Yang, Mihaela Georgieva, Wei Song, Anish Patel, Nicole LaMarca, and Omar Dabbous were involved in the conception and design of the study and interpretation of the data; Anya (Xinyi) Jiang and Angela Zhao conducted the analysis and interpretation of the data. All authors participated in the drafting of the paper and revised it critically for intellectual content. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
Funding for this study and the article fees, including the Rapid Service and Open Access Fee, were provided by Novartis Gene Therapies, Inc.
Medical Writing and Editorial Assistance
Medical writing assistance was provided by Shelley Batts, PhD, an independent contractor for Analysis Group, Inc., and funded by Novartis Gene Therapies, Inc. Editorial support was provided by Amanda Prawdzik, of Kay Square Scientific, and funded by Novartis Gene Therapies, Inc. These data were presented as a poster at the Academy of Managed Care Pharmacy’s 2023 Annual Meeting & Expo.
Data Availability
The data that support the findings of this study are available from HealthVerity. Restrictions apply to the availability of these data, which were used under license for this study.
Ethical Approval
This article is based on a claims database analysis and does not contain any new studies with human participants or animals performed by any of the authors. The authors had permission to access the HealthVerity claims database until the completion of the study. Institutional Review Board approval and accordance to the Declaration of Helsinki was not required.
Conflict of Interest
Walter Toro, Anish Patel, and Omar Dabbous are employees of Novartis Gene Therapies, Inc., and hold stock and options. Nicole LaMarca was an employee of Novartis Gene Therapies, Inc., during the time of the study and writing of the manuscript. She is currently employed by Sarepta Therapeutics. Min Yang, Wei Song, Anya (Xinyi) Jiang, and Angela Zhao are employees of Analysis Group, Inc., which has received consulting fees from Novartis Gene Therapies, Inc., for the conduct of this study. Mihaela Georgieva was an employee of Analysis Group, Inc., which received consulting fees from Novartis Gene Therapies, Inc., for the conduct of this study, during the time of the study and writing of the manuscript. She is currently employed by Moderna.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Toro, W., Yang, M., Georgieva, M. et al. Health Care Resource Utilization and Costs for Patients with Spinal Muscular Atrophy: Findings from a Retrospective US Claims Database Analysis. Adv Ther 40, 4589–4605 (2023). https://doi.org/10.1007/s12325-023-02621-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02621-y