Abstract
Introduction
New target-specific oral anticoagulants may have benefits, such as shorter hospital length of stay, compared to warfarin in patients with nonvalvular atrial fibrillation (NVAF). This study aimed to assess, among patients with NVAF, the effect of rivaroxaban versus warfarin on health care costs in a cohort of rivaroxaban users and matched warfarin users.
Methods
Health care claims from the Humana database from 5/2011 to 12/2012 were analyzed. Adult patients newly initiated on rivaroxaban or warfarin with ≥2 atrial fibrillation (AF) diagnoses (The International Classification of Diseases, Ninth Revision, Clinical Modification: 427.31) and without valvular AF were identified. Based on propensity score methods, warfarin patients were matched 1:1 to rivaroxaban patients. Patients were observed up to end of data, end of insurance coverage, death, a switch to another anticoagulant, or treatment nonpersistence. Health care costs [hospitalization, emergency room (ER), outpatient, and pharmacy costs] were evaluated using Lin’s method.
Results
Matches were found for all rivaroxaban patients, and characteristics of the matched groups (n = 2253 per group) were well balanced. Estimated mean all-cause and AF-related hospitalization costs were significantly lower for rivaroxaban versus warfarin patients (all-cause: $5411 vs. $7427, P = 0.047; AF-related: $2872 vs. $4147, P = 0.020). Corresponding estimated mean all-cause outpatient visit costs were also significantly lower, but estimated mean pharmacy costs were significantly higher for rivaroxaban patients ($5316 vs. $2620, P < 0.001). Although estimated mean costs of ER visits were higher for rivaroxaban users compared to those of warfarin users, differences were not statistically significant. Including anticoagulant costs, mean overall total all-cause costs were comparable for rivaroxaban versus warfarin users due to cost offset from a reduction in the number and length of hospitalizations and number of outpatient visits ($17,590 vs. $18,676, P = 0.542).
Conclusion
Despite higher anticoagulant cost, mean overall total all-cause and AF-related cost remains comparable for patients with NVAF treated with rivaroxaban versus warfarin due to the cost offset from reduced health care resource utilization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is the most common heart rhythm disturbance, with a prevalence estimated between 2.7 and 6.1 million cases in the United States [1]. Compared to non-AF patients, AF patients have been found to be at a near five-fold higher risk of stroke and at an eight-fold higher risk of having multiple cardiovascular hospitalizations [2, 3]. The associated health care costs of patients with AF are high. The incremental cost burden of AF patients versus non-AF patients was estimated at $26 billion in the United States in 2010, with more than 50% of this amount being hospitalization costs [3, 4]. Moreover, the AF-related hospitalization rate increased by 23% among US adults from 2000 to 2010 [5].
Chronic anticoagulation has been the standard of care for patients with chronic nonvalvular atrial fibrillation (NVAF) in the previous decades and, until recently, warfarin and other vitamin K antagonists were the only available options [6, 7]. Recently, the target-specific oral anticoagulants rivaroxaban, dabigatran, and apixaban have been approved by the US Food and Drug Administration (FDA) for the treatment of NVAF [8–10]. These new agents have predictable pharmacokinetic properties, minimal food–drug interactions, and do not require frequent monitoring as compared to warfarin [11–14]. Recent studies have compared these new agents with warfarin and found that target-specific oral anticoagulants were a cost-effective option [15–17].
AF is a significant driver of hospitalizations [18] and a considerable burden for the health care system. Since the use of new target-specific oral anticoagulants may result in potential economic benefits, the aim of the present study was to compare health care costs between NVAF patients using rivaroxaban and a matched sample of patients using warfarin.
Methods
Data Source
The analysis was conducted using health insurance claims from the Humana database during the period from May 2011 through December 2012, in line with other retrospective studies [19–22]. The Humana database includes over 11.3 million lives of commercial and Medicare members, and covers all census regions in the United States. The database contains information on patient demographics; enrollment history; and claims for inpatient, outpatient, emergency room (ER), and other medical services. In addition, the Humana database contains information on pharmacy and laboratory claims. Data are de-identified and comply with the patient requirements of the Health Insurance Portability and Accountability Act (HIPAA). Institutional review board approval was not required for this study. This article does not contain any new studies with human or animal subjects performed by any of the authors.
Study Design
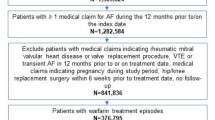
A retrospective matched-cohort design was used to quantify the difference in health care costs between patients with NVAF who used rivaroxaban versus warfarin among rivaroxaban-treated-like patients. Patients included in the study were newly initiated on rivaroxaban or warfarin after November 2011 (the time of rivaroxaban approval for NVAF in the United States), were 18 years of age or older, had a baseline period of at least 6 months of continuous health plan enrollment before the index date (i.e., the date of the first rivaroxaban or warfarin dispensing), and had at least two primary or secondary AF diagnoses [The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM): 427.31] during the baseline or the follow-up period. Patients were excluded if they were diagnosed at baseline with valvular involvement [ICD-9-CM: 394.x-397.x, 424.x, 746.0x-746.7x, V42.2, V43.3; Current Procedural Terminology, 4th Edition (CPT-4): 33400-33478], pregnancy (ICD-9-CM: V22, V23, V27, 630.x-676.x), malignant cancer (ICD-9-CM: 140.x-208.xx, 230.x-234.x), or transient cause of AF (ICD-9-CM: 415.x, 429.4; CPT-4: 33400-33999).
Similarly to three recent phase III clinical trials on the target-specific oral anticoagulants rivaroxaban, dabigatran, and apixaban (i.e., ROCKET AF, NCT00403767; RE-LY, NCT00262600; ARISTOTLE, NCT00412984), patients in the current study who were treated with rivaroxaban after its approval in November 2011, but with previous use of warfarin, were classified in the rivaroxaban cohort [23–25]. In each of the phase III trials, a total of 50–62% of patients had used warfarin before enrollment and randomization.
The observation period spanned from the date of the first dispensing (i.e., the first filled pharmacy prescription) of rivaroxaban or warfarin, defined as the index date, to the earliest among the end of data availability, end of insurance coverage, death, a switch to another anticoagulant, or 14 days after treatment nonpersistence (i.e., 14 days after the end of the days of supply of the first dispensing for which the next dispensing of the index medication, if any, was more than 60 days later). The nonpersistence criterion increased the certainty that health care costs were evaluated during exposure to the medications of interest.
Study Endpoints
The primary endpoint of this study was all-cause health care costs, which included hospitalizations, ER visits, outpatient visits, and pharmacy costs. Health care costs were calculated as the sum of the following elements: amount paid by insurance, copay amount, coinsurance amount, deductible amount, and secondary insurance amount. AF-related costs were also evaluated. Costs for AF-related hospitalizations, ER visits, and outpatient visits were defined as costs associated with claims that had a primary or secondary diagnosis for AF. AF-related pharmacy costs were the costs of anticoagulant or antiplatelet agents that were dispensed.
Statistical Analysis
Propensity score matching was performed to adjust for confounding bias. Patients in the warfarin group were matched 1:1 to patients in the rivaroxaban group based on random selection among propensity score calipers of 5%. Propensity scores were calculated using a multivariate logistic regression model that incorporated the following baseline characteristics: age, gender, type of insurance, comorbidity index scores (i.e., Quan-Charlson Comorbidity Index, CHADS2 score, CHA2DS2-VASc score, ATRIA score, and HAS-BLED score), baseline resource utilization, baseline costs, the month of the index date, and specific comorbidities (>5%; Table 1).
Patients’ baseline characteristics evaluated during the 6 months prior to the index date were summarized using means [±standard deviation (SD)] for continuous variables, and frequencies and percentages for categorical variables. Baseline characteristics were compared between cohorts using standardized differences. Baseline characteristics with standardized differences of less than 10% were considered well balanced [26–28].
Health care costs (i.e., hospitalizations, ER visits, outpatient visits, and pharmacy costs) between rivaroxaban and warfarin users were reported and compared using Lin’s method to account for death and the censored observation periods of patients [29]. For the calculation of health care costs based on Lin’s method, the follow-up period of each patient was partitioned in small intervals (i.e., days in the current study), and health care costs were calculated across all patients still observed (i.e., in plan and not censored) for a given interval. Hospitalizations, ER visits, outpatient visits, and pharmacy costs were estimated as the sum over intervals of the Kaplan–Meier estimator for the conditional probability of surviving to the start of the interval multiplied by the average studied outcome over the interval.
Health care costs were compared between cohorts through mean differences. Nonparametric bootstrap procedures with 999 replications were used to evaluate confidence intervals and to compare rivaroxaban and warfarin mean all-cause and AF-related costs. All costs were inflation adjusted to 2012 US dollars based on the medical care component of the Consumer Price Index. Statistical significance was assessed at a significance level of 0.05. All statistical analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Patient Characteristics
A total of 2253 rivaroxaban and 10,796 warfarin users were identified (Fig. 1). All rivaroxaban users were propensity matched with the same number of warfarin users to form the study cohorts. Overall, baseline characteristics were well balanced (i.e., standardized difference below 10%) between rivaroxaban and warfarin users. The baseline characteristics of the matched cohorts are summarized in Table 1. Mean age of both cohorts was 74 years, and 46% of patients were female. All comorbidity index scores between cohorts were similar, with standardized differences below 10%, and the most prevalent comorbidities were hypertension, hyperlipidemia, diabetes, and abdominal surgery (>30%). A total of 517 (23%) rivaroxaban users had previous use of warfarin at baseline. The mean observation period was 114.0 and 123.7 days for rivaroxaban and warfarin users (standardized difference = 10.5%), respectively.
Health Care Costs
Table 2 [30] presents estimated mean health care costs. The estimated mean all-cause and AF-related hospitalization costs were significantly lower for patients treated with rivaroxaban compared to patients treated with warfarin (all-cause: $5411 vs. $7427, P = 0.047; AF-related: $2872 vs. $4147, P = 0.020). Similarly, estimated mean all-cause outpatient visit costs were significantly lower for rivaroxaban users ($6025 vs. $7999, P = 0.040), while mean AF-related outpatient visit costs were lower but not statistically significant for rivaroxaban users ($1799 vs. $2845, P = 0.167).
Estimated mean pharmacy costs were significantly higher for rivaroxaban patients compared to warfarin patients (all-cause: $5316 vs. $2620, P < 0.001; AF-related: $2355 vs. $121, P < 0.001). Estimated mean ER visit costs were also higher for rivaroxaban users compared to warfarin users, but the differences were not statistically significant (all-cause: $838 vs. $630, P = 0.201; AF-related: $369 vs. $208, P = 0.054). The estimated mean all-cause total cost was lower for rivaroxaban users compared to warfarin users, but not statistically different ($17,590 vs. $18,676, P = 0.542), while the estimated mean AF-related total cost was not significantly higher for rivaroxaban users ($7394 vs. $7319, P = 0.943).
Discussion
This retrospective matched-cohort analysis compared health care costs between a sample of NVAF patients treated with the target-specific oral anticoagulant rivaroxaban and a matched sample of NVAF patients treated with warfarin based on real-world data. Rivaroxaban was associated with a significant reduction in all-cause and AF-related estimated costs of hospitalization compared to warfarin (27% and 31%, respectively). Significant differences between costs incurred by rivaroxaban and warfarin users were also found for estimated all-cause and AF-related outpatient visits (25% and 37%, respectively). Estimated pharmacy costs were significantly lower for warfarin users compared to rivaroxaban users (51% lower costs for all-cause pharmacy costs and 95% for AF-related pharmacy costs).
Patients in the current study treated with rivaroxaban who had previous use of warfarin were classified in the rivaroxaban cohort. Since the results of the ROCKET AF trial suggested that rivaroxaban users who were naïve to warfarin experienced better primary efficacy and safety endpoints relative to warfarin-exposed patients [24], including warfarin-experienced patients in the rivaroxaban cohort likely produced more conservative estimates of differences between groups in the current study. The proportion of rivaroxaban patients with prior use of warfarin in the current study at 23% was lower than the proportion reported in the ROCKET AF trial, where 62% of rivaroxaban patients had previous use of vitamin K antagonists [24]. Since the current study was conducted with real-world data, it may be more representative of the real rivaroxaban patient population than a clinical trial with more strict inclusion criteria.
Recent studies have found that patients with NVAF who used target-specific oral anticoagulants had lower health care costs than patients who used warfarin during hospitalizations [31, 32]. More specifically, Fonseca et al. examined total hospital costs associated with warfarin and dabigatran use in a treatment-naïve NVAF population. The authors reported total hospitalization costs of $14,794 for dabigatran users and $16,826 for warfarin users (P < 0.01) [31]. Laliberté et al. [32], who studied a Premier database sample of NVAF patients administered rivaroxaban or warfarin during a hospitalization, also found significantly lower hospitalization costs for rivaroxaban compared to warfarin users ($11,993 vs. $13,255, respectively; P < 0.001). Although patients with NVAF in the current study were not administered rivaroxaban or warfarin in a hospital setting, significantly lower hospitalization costs were also found for rivaroxaban compared to warfarin users ($5411 vs. $7427, respectively; P = 0.047) during the observation period. In addition, in the current study, total health care costs were not significantly different between rivaroxaban and warfarin users despite the significantly higher pharmacy costs of rivaroxaban users. This suggests an offset of the higher cost of rivaroxaban therapy compared to warfarin.
Recent cost-effectiveness studies have also been conducted to compare new target-specific agents with warfarin [15, 16, 33–35]. Harrington et al. [16] constructed a Markov decision analysis model using data from clinical trials and found that new agents (apixaban 5 mg, dabigatran 150 mg, and rivaroxaban 20 mg) were all cost-effective alternatives to warfarin. In the base case, warfarin had both the lowest cost and the lowest quality-adjusted life-years estimate compared to all three new agents. Moreover, rivaroxaban was consistently reported as a cost-effective alternative to warfarin among AF populations in recent publications [15, 16, 33, 35]. Rivaroxaban was also shown to be cost-effective compared to warfarin in a Singapore health care setting, which suggests that the cost-effectiveness of rivaroxaban versus warfarin is global [36]. To be cost-effective means that the new product provides sufficient benefits to justify the added cost. The results of the current study provide additional real-world evidence, and suggest that the use of rivaroxaban may be cost-saving or cost-neutral as compared to warfarin. The overall nondrug lower costs for rivaroxaban users suggest that treatment with rivaroxaban results in less interaction with health care systems, especially in terms of hospitalizations, compared to treatment with warfarin. Therefore, the use of rivaroxaban may have clinical benefits without incurring higher overall health care costs.
This matched-cohort analysis has a number of limitations. First, in spite of information accuracy and completeness required by administrative databases for payment purposes, billing inaccuracies and missing data may still occur. Second, a general limitation of observational studies is that adjustments can be made only for observable factors; adjustments cannot be made for unmeasured confounders. Third, this study was conducted with data obtained from the time period immediately after rivaroxaban became available, and utilization patterns may have changed over time. Fourth, these findings only apply to rivaroxaban since the other target-specific oral anticoagulants were not evaluated. Lastly, the observational design of the study was susceptible to additional potential biases, such as information or classification bias (e.g., identification of false positive or negative AF events). Despite these limitations, observational studies that use statistical techniques to adjust for potentially observed confounding factors through matching techniques provide valuable information, with real-life scenarios and high generalizability.
Conclusion
In this real-world study, the estimated cost burden associated with rivaroxaban for all-cause and AF-related hospitalization costs, as well as all-cause outpatient visit costs, was significantly lower than that associated with warfarin in patients with NVAF. With the inclusion of drug costs, both all-cause and AF-related total costs were comparable between groups. Despite higher anticoagulant cost, overall total all-cause and AF-related cost remains comparable due to the cost offset from reduced health care resource utilization.
References
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, et al. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–245.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983–8.
Kim MH, Johnston SS, Chu B-C, Dalal MR, et al. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4(3):313–20.
Wu EQ, Birnbaum HG, Mareva M, Tuttle E, et al. Economic burden and co-morbidities of atrial fibrillation in a privately insured population. Curr Med Res Opin. 2005;21(10):1693–9.
Patel NJ, Deshmukh A, Pant S, Singh V, et al. Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010: implications for healthcare planning. Circulation. 2014;129(23):2371–9.
Ageno W, Gallus AS, Wittkowsky A, Crowther M, et al. Oral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e44S–88S.
Mantha S, Cabral K, Ansell J. New avenues for anticoagulation in atrial fibrillation. Clin Pharmacol Ther. 2013;93(1):68–77.
U.S. Food and Drug Administration. FDA approves Pradaxa to prevent stroke in people with atrial fibrillation. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm230241.htm. Accessed Feb 2015.
U.S. Food and Drug Administration. FDA approves Xarelto to prevent stroke in people with common type of abnormal heart rhythm. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm278646.htm. Accessed Feb 2015.
U.S. Food and Drug Administration. FDA approves Eliquis to reduce the risk of stroke, blood clots in patients with non-valvular atrial fibrillation. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm333634.htm. Accessed Feb 2015.
Hankey GJ, Eikelboom JW. Novel oral anticoagulants for atrial fibrillation. Curr Atheroscler Rep. 2013;15(8):344.
Aditya S. Oral and parenteral anticoagulants: new kids on the block. J Postgrad Med. 2012;58(4):275–85.
Ansell J, Hirsh J, Hylek E, Jacobson A, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133(6 Suppl):160S–98S.
Shafeeq H, Tran TH. New oral anticoagulants for atrial fibrillation: are they worth the risk? P T. 2014;39(1):54–64.
Lee S, Anglade MW, Pham D, Pisacane R, et al. Cost-effectiveness of rivaroxaban compared to warfarin for stroke prevention in atrial fibrillation. Am J Cardiol. 2012;110(6):845–51.
Harrington AR, Armstrong EP, Nolan PE, Malone DC. Cost-effectiveness of apixaban, dabigatran, rivaroxaban, and warfarin for stroke prevention in atrial fibrillation. Stroke. 2013;44(6):1676–81.
Limone BL, Baker WL, Kluger J, Coleman CI. Novel anticoagulants for stroke prevention in atrial fibrillation: a systematic review of cost-effectiveness models. PLoS One. 2013;8(4):e62183.
Wattigney WA, Mensah GA, Croft JB. Increasing trends in hospitalization for atrial fibrillation in the United States, 1985 through 1999: implications for primary prevention. Circulation. 2003;108(6):711–6.
Hayes MS, Ward MA, Slabaugh SL, Xu Y. Lessons from the leucovorin shortages between 2009 and 2012 in a Medicare advantage population: where do we go from here? Am Health Drug Benefits. 2014;7(5):264–70.
Dufour R, Joshi AV, Pasquale MK, Schaaf D, et al. The prevalence of diagnosed opioid abuse in commercial and Medicare managed care populations. Pain Pract. 2014;14(3):E106–15.
Wei W, Zhou S, Miao R, Pan C, et al. Much ado about nothing? A real-world study of patients with type 2 diabetes switching basal insulin analogs. Adv Ther. 2014;31(5):539–60.
Pasquale MK, Dufour R, Joshi AV, Reiners AT, et al. Inefficiencies in osteoarthritis and chronic low back pain management. Am J Manag Care. 2013;19(10):816–23.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Patel MR, Mahaffey KW, Garg J, Pan G, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Granger CB, Alexander JH, McMurray JJV, Lopes RD, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Cohen J. Statistical Power Analysis for the Behavioral Sciences. Toronto: Toronto Academic Press Inc; 1977. p. 19–24.
Normand ST, Landrum MB, Guadagnoli E, Ayanian JZ, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54(4):387–98.
Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228–34.
Lin DY, Feuer EJ, Etzioni R, Wax Y. Estimating medical costs from incomplete follow-up data. Biometrics. 1997;53(2):419–34.
Efron B, Tibshirani RJ. An Introduction to the Bootstrap. 1st ed. New York: Chapman & Hall; 1993. p. 436.
Fonseca E, Walker DR, Hill J, Hess GP. Dabigatran etexilate is associated with shorter hospital length of stay compared to warfarin in patients with nonvalvular atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2012;5:A282.
Laliberté F, Pilon D, Raut MK, Nelson WW, et al. Is rivaroxaban associated with lower inpatient costs compared to warfarin among patients with non-valvular atrial fibrillation? Curr Med Res Opin. 2014;30:1–10.
Kleintjens J, Li X, Simoens S, Thijs V, et al. Cost-effectiveness of rivaroxaban versus warfarin for stroke prevention in atrial fibrillation in the Belgian healthcare setting. Pharmacoeconomics. 2013;31(10):909–18.
Kamel H, Easton JD, Johnston SC, Kim AS. Cost-effectiveness of apixaban vs warfarin for secondary stroke prevention in atrial fibrillation. Neurology. 2012;79(14):1428–34.
Rognoni C, Marchetti M, Quaglini S, Liberato NL. Apixaban, dabigatran, and rivaroxaban versus warfarin for stroke prevention in non-valvular atrial fibrillation: a cost-effectiveness analysis. Clin Drug Investig. 2014;34(1):9–17.
Wang Y, Xie F, Kong MC, Lee LH, et al. Cost-effectiveness of dabigatran and rivaroxaban compared with warfarin for stroke prevention in patients with atrial fibrillation. Cardiovasc Drugs Ther. 2014;28(6):575–85.
Acknowledgments
Sponsorship and article processing charges for this study were funded by Janssen Scientific Affairs, LLC, Raritan, NJ, USA. All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. Editorial assistance was provided by Alanna Franchetti, ELS, of MedErgy (Yardley, PA, USA), and was funded by Janssen Scientific Affairs.
Conflict of interest
François Laliberté Michel Cloutier, Guillaume Germain, and Patrick Lefebvre are employees of Analysis Group, Inc. Analysis Group, Inc. is a consulting company that has received research grants from Janssen Scientific Affairs, LLC. Concetta Crivera, Winnie W. Nelson, William H. Olson, and Jeffrey Schein are employees of Janssen Scientific Affairs, LLC. Julie Vanderpoel was an employee of Janssen Scientific Affairs, LLC at the time this study was conducted.
Compliance with ethics guidelines
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Laliberté, F., Cloutier, M., Crivera, C. et al. Effect of Rivaroxaban Versus Warfarin on Health Care Costs Among Nonvalvular Atrial Fibrillation Patients: Observations from Rivaroxaban Users and Matched Warfarin Users. Adv Ther 32, 216–227 (2015). https://doi.org/10.1007/s12325-015-0189-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-015-0189-1