Abstract
Introduction
Nonvalvular atrial fibrillation (NVAF) is associated with a substantial economic burden, particularly in patients with comorbid conditions. This study compared healthcare resource utilization (HRU) and costs of rivaroxaban and warfarin in patients with NVAF, obesity, and diabetes.
Methods
A de-identified healthcare claims database was used to identify adult patients newly initiating rivaroxaban or warfarin and having at least one medical claim with a diagnosis of AF, obesity determined by validated algorithm, and at least one claim with a diagnosis of diabetes or for antidiabetic medication from December 2011 to March 2020. Propensity score matching was used to balance the treatment cohorts on the basis of demographics and baseline characteristics. All-cause and NVAF-related HRU rates and costs were compared between treatments using rate ratios, and mean cost differences were calculated on a per patient per year (PPPY) basis.
Results
A total of 9999 matched pairs of patients with NVAF, obesity, and diabetes were identified in the rivaroxaban and warfarin cohorts. Rate ratios of all-cause HRU were significantly reduced with rivaroxaban versus warfarin in all healthcare settings evaluated, except emergency room visits. The greatest impact was on physician office visits followed by hospital outpatient and inpatient visits. NVAF-related HRU was significantly lower for rivaroxaban versus warfarin in all care settings. Consistent with these findings, the length of hospital stay was significantly reduced by approximately 4 days among all patients for both all-cause and NVAF-related hospitalizations in the rivaroxaban cohort compared with the warfarin cohort. Rivaroxaban was associated with reductions in all-cause total healthcare costs by more than $5000 PPPY and NVAF-related medical costs by approximately $1100 PPPY.
Conclusion
In comparison with warfarin, rivaroxaban reduced HRU and costs, particularly hospital inpatient and outpatient visits and physician office visits, in patients with NVAF and comorbidities of obesity and diabetes.
Plain Language Summary
People who are overweight or obese are at risk of developing atrial fibrillation (AF) along with other medical conditions, such as diabetes. Standard therapy with oral anticoagulants or blood thinners is recommended to reduce the risk of stroke and systemic embolism in patients with nonvalvular AF (NVAF). In this study, we evaluated healthcare insurance claims for people with NVAF, obesity, and diabetes who started therapy with warfarin or rivaroxaban from 2011 to 2020 to compare the use and cost of healthcare services, such as hospitalizations and doctor visits, using diagnosis and procedure codes. The study included nearly 20,000 patients with similar characteristics. Patients who started treatment with rivaroxaban used fewer healthcare services for any cause and for those related to NVAF than those who started treatment with warfarin. The difference in use of services was largest for hospital outpatient and inpatient visits and doctor office visits; emergency room visits were only different for those related to NVAF. Length of hospital stay was also shorter for patients receiving rivaroxaban versus those receiving warfarin. These differences in healthcare service use translated into lower costs associated with rivaroxaban versus warfarin. The findings of this study suggest that treatment with rivaroxaban reduces the use of healthcare services compared with warfarin. This difference may be related, in part, to the reduced risks of stroke and systemic embolism observed in other real-world studies with rivaroxaban compared to warfarin. In addition, rivaroxaban does not require routine blood testing, which is required with warfarin treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The risk of nonvalvular atrial fibrillation (NVAF) is increased among individuals with obesity and diabetes. |
Obesity is a worldwide public health crisis that increases the risk of comorbidities and contributes substantially to healthcare expenditures. |
What did the study ask? |
This real-world study evaluated and compared healthcare resource utilization (HRU) and costs of rivaroxaban and warfarin in patients with NVAF, obesity, and diabetes. |
What were the study outcomes? |
All-cause HRU rate ratios were significantly reduced with rivaroxaban versus warfarin in all healthcare settings evaluated, except emergency room visits. |
NVAF-related HRU was significantly lower for rivaroxaban versus warfarin in all healthcare settings. |
Rivaroxaban was associated with reductions in all-cause and NVAF-related costs. |
What was learned from the study? |
HRU and costs were lower with rivaroxaban compared with warfarin in patients with NVAF and concurrent obesity and diabetes. |
Treatment differences in HRU and costs were mainly observed for hospital inpatient and outpatient visits and physician office visits, supporting the need for fewer healthcare interactions during rivaroxaban therapy compared with warfarin therapy. |
Introduction
Atrial fibrillation (AF) is associated with substantial burden to patients, caregivers, and the healthcare system, with increased risks of stroke, heart failure, cognitive and mental health problems, and death, which contribute to an annual hospitalization rate of up to 40% [1]. The incidence of chronic diseases, particularly cardiovascular diseases and diabetes, is increased in overweight or obese individuals [2]. Similarly, the risk of developing nonvalvular atrial fibrillation (NVAF) and thrombotic events is higher in obese individuals, and NVAF in obese patients is associated with more severe symptoms, more persistent AF, and poorer outcomes [3,4,5]. Obesity is the leading risk factor for type 2 diabetes, and prevalence rates of diabetes increase in parallel with rates of obesity [6, 7]. Diabetes is also a well-established risk factor for stroke among patients with AF [8]. The co-occurrence of diabetes and AF is associated with worsened symptoms of AF, an increased risk of all-cause and cardiovascular mortality, an increased risk of hospitalizations, and excess morbidity [9, 10]. Patients with obesity and diabetes have an increased risk of AF [11,12,13].
Obesity and associated medical conditions lead to substantial medical expenditures, which are expected to increase with the increasing prevalence of obesity worldwide [14,15,16]. The global economic impact of obesity was estimated at 2 trillion US dollars in 2014 [16]. A recent study using the 2001–2016 Medical Expenditure Panel Survey found that total direct medical costs of obesity in US adults doubled from 2001 ($124.2 billion) to 2016 ($260.6 billion), and total annual medical expenditures of obese adults ($5010) were double those of people of normal weight ($2504) [17]. Overweight and obese individuals have increased utilization of primary and secondary healthcare services compared with those of normal body weight [2, 17, 18]. In addition, obese individuals are prescribed nearly twice as many medications and are nearly four times more likely to be hospitalized compared with nonobese individuals [2]. Obesity may also increase societal costs associated with lost productivity, disability, and mortality [16].
Oral anticoagulation therapy with a direct oral anticoagulant (DOAC) is the standard of care to prevent embolic events in patients with NVAF [19]. Standard dosing of DOACs in patients with body mass index (BMI) of 40 kg/m2 or less was recommended by the International Society of Thrombosis and Haemostasis in 2016; however, the use of DOACs in morbidly obese patients (BMI > 40 kg/m2) was not recommended because of limited clinical evidence [20]. A number of studies and three systematic reviews have subsequently assessed the use of DOACs in patients with morbid obesity (body weight ≥ 120 kg or BMI ≥ 40 kg/m2) and support the benefit–risk profile of DOACs, particularly rivaroxaban and apixaban, in this population [21,22,23]. Rivaroxaban, an oral direct factor Xa inhibitor, was approved for the prevention of stroke and systemic embolism in patients with NVAF in November 2011 on the basis of the ROCKET-AF trial [24, 25].
There is a need to understand the healthcare resource utilization (HRU) and costs associated with anticoagulation therapy in patients with NVAF and common comorbidities. This study evaluated the HRU and costs of rivaroxaban compared with warfarin in patients with NVAF, obesity, and diabetes.
Methods
Study Design
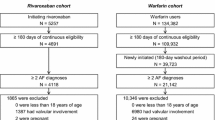
This retrospective cohort study was conducted from December 1, 2010 to March 1, 2020 (Fig. 1). The patient identification period began on December 1, 2011, aligning with the approval date of rivaroxaban in November 2011, and ended on March 1, 2020. The first pharmacy dispensing for rivaroxaban or warfarin during the patient identification period was defined as the index date. The baseline period was defined as a 12-month period with continuous health plan enrollment prior to the index date. This analysis was designed to evaluate and compare all-cause and NVAF-related HRU and costs between rivaroxaban and warfarin among patients with NVAF, obesity, and diabetes.
Study design. BMI body mass index, HRU healthcare resource utilization, NVAF nonvalvular atrial fibrillation. The identification period was from December 1, 2011 to March 1, 2020. The index event was the first pharmacy dispensing for rivaroxaban or warfarin during the identification period. The index date was the first claim date for rivaroxaban or warfarin. The baseline period was a 12-month period with continuous health plan enrollment prior to the index date, and criteria for inclusion could be met at any time during this time. Patients with stroke/systemic embolism or major bleeding within 30 days prior to the index date were excluded from the analysis
Data Sources
The outcomes in this study were assessed using Optum’s de-identified Clinformatics® Data Mart Database—Date of Death (DOD) database, an adjudicated US administrative health claims database. Members include people with private health insurance, who are fully insured in commercial plans or in administrative services only, and Medicare Advantage (starting January 2006). Commercial claims patients (age 0–65 years) make up the majority of the population, with some Medicare patients (age 65–90 years) also included. The database includes information from inpatient and outpatient medical services, prescriptions as dispensed, and outpatient laboratory tests processed by large national vendors who participate in data exchange with Optum.
Patients
Adult patients newly initiating rivaroxaban or warfarin were identified from the database with the following inclusion criteria: at least one pharmacy claim for rivaroxaban or warfarin (generic product identifier [GPI] code 83370060 and 83200030, respectively) during the patient identification period; at least 12 months continuous medical and pharmacy benefit enrollment prior to and on the index date; at least one medical claim with a diagnosis of AF during the 12-month baseline period prior to or on the index date (International Classification of Diseases [ICD]-9 code 427.31 and ICD-10 codes I48.0%–I48.2%, I48.91%); and at least 18 years of age on the index date.
Patient height and weight data were not available in the claims databases. Thus, the presence of obesity, defined as BMI ≥ 30 kg/m2, was determined on the basis of a proprietary validated BMI interpolation algorithm [26]. Using a novel automated weighted prediction approach (Super Learner algorithm), the predictions from four different machine learning algorithms (Catboost, random forest, least absolute shrinkage, and selection operator [LASSO] regression, and artificial neural networks) were leveraged through logistic regression. Features included diagnoses, procedures, and medication uses during the 12-month baseline period and patient demographics. The Optum DOD database was used for training and internally validating the algorithm. The IBM® MarketScan® Commercial Claims and Encounters database was used for external validation based on assessments of area under the receiver operating characteristic curve (ROC AUC), F1 score, accuracy, negative predictive value, specificity, positive predictive value or precision, and sensitivity or recall. Two predictive models were developed: model 1 included the selected features along with baseline BMI features for patients who had historical BMI data available (diagnosis codes are provided in Table S1 of the supplementary material), and model 2 included only the selected features and was trained on patients who did not have baseline BMI data. Internal validation of model 1 yielded ROC AUC of 88%, with accuracy ranging from 88% to 93% and specificity ranging from 92% to 95% for predicting BMI classifications of ≥ 30, ≥ 35, and ≥ 40 kg/m2. Model 2 was internally validated with ROC AUC of 73%, with accuracy ranging from 74% to 80% and specificity ranging from 72% to 86% [26].
Patients were also required to have at least one claim with a diagnosis of diabetes (ICD-9: 250.%; ICD-10: E10.%, E11.%, E13.%) or at least one claim for antidiabetic medication (GPI code 27% Healthcare Common Procedure Coding System codes J1815, J1817, E0784, S5550-S5571, G9147, S9353) during the 12-month baseline period prior to or on the index date.
Exclusion criteria included the following: a hospitalization or emergency room (ER) visit with a primary diagnosis code for stroke or systemic embolism, or an event of major bleeding defined by the Cunningham algorithm [27] within 30 days prior to index date; pharmacy claims for at least two oral anticoagulant medications on the index date; and at least one pharmacy claim for an oral anticoagulant at any time prior to the index date (Table S2 in the supplementary material). If patients had evidence of another indication for anticoagulation (i.e., acute venous thromboembolism, prophylaxis after hip/knee replacement surgery) during the baseline period or a diagnosis code for mitral stenosis or a diagnosis or procedure code for a mechanical heart valve procedure at any time prior to the index date, they were also excluded from the analysis (Table S2).
Outcomes
All-cause and NVAF-related (i.e., associated with a diagnosis code for NVAF in any position) HRU were evaluated for the following settings: inpatient hospitalization, including length of stay in days; proportion of patients with 30-day rehospitalization (all-cause hospitalization only); ER visits; hospital outpatient visits; physician office visits (primary and specialty care); and skilled nursing facility (SNF) visits. All-cause and NVAF-related medical costs were evaluated as total medical costs for inpatient hospitalization, ER visits, hospital outpatient visits, physician office visits (primary and specialty care), and SNF visits. Total pharmacy costs were evaluated for all-cause costs only. All-cause total healthcare costs were defined as all-cause medical costs plus all-cause pharmacy costs. Two analyses of HRU and costs were conducted on the basis of the duration of follow-up. The first was an intent-to-treat analysis, including data through the earliest of health plan disenrollment or latest data availability. A second analysis (sensitivity analysis) followed an as-treated approach, including data from treatment initiation (index date) to treatment discontinuation, health plan disenrollment, or end of study, whichever came first.
Statistical Analysis
The propensity of receiving rivaroxaban was predicted using a logistic regression model with potential confounders of age; gender; geographic region; health plan type; insurance type; index year; baseline comorbidities and comorbidity risk scores (i.e., Quan–Charlson comorbidity index [QCI] [28], CHA2DS2-VASc [29], and HAS-BLED [30]); baseline procedures (gastric bypass surgery and cardiovascular procedures); baseline medication use (non-oral anticoagulants, antihyperlipidemics, antihypertensives, antiplatelet agents); and baseline HRU and costs (Table S3 in the supplementary material).
To reduce potential bias and create more comparable cohorts based on baseline characteristics, propensity score matching was used in which rivaroxaban users were matched 1:1 with warfarin users without replacement on the logit of the propensity score using calipers of width equal to 20% of the standard deviation of the logit of the propensity score [31]. To indicate sufficient overlap and use of propensity score matching, calculation of equipoise greater than 50% was used.
Descriptive statistics were used to summarize demographics and baseline characteristics for each treatment cohort. Standardized differences in baseline characteristics of less than 10% were considered a negligible imbalance. Rates of all-cause and NVAF-related HRU and costs were calculated as the number of events or costs incurred over the follow-up period divided by the patient-years of observation. HRU was compared between treatment cohorts using rate ratios, and mean cost differences per patient per year (PPPY) between cohorts were calculated. All costs were inflated to 2020 US dollars based on the medical care component of the Consumer Price Index. For both HRU and costs, nonparametric bootstrap procedures were used to estimate 95% confidence intervals and P values.
Compliance with Ethics Guidelines
This study is based on de-identified data collected from a healthcare claims database and does not contain any experimental data with human or animal participants; this analysis was deemed exempt from institutional review board oversight and informed consent was not obtained as per guidance from the Office for Human Research Protections [32].
Results
Patient Characteristics
Among 258,475 adult patients who had at least one claim for either rivaroxaban or warfarin, at least one claim for AF, and at least 12 months of continuous health plan enrollment, obesity (BMI ≥ 30 kg/m2) was identified in 103,342 (40.0%) patients using the BMI algorithm tool (Table 1). Of these, 57,340 (55.5%) were identified as having diabetes. Exclusion criteria removed 26,262 patients, leaving an analysis population of 31,078 patients, of which 12,663 initiated rivaroxaban and 18,415 initiated warfarin (Table 1).
Demographics and baseline clinical characteristics before and after propensity score matching are shown in Table 2. Rivaroxaban patients were younger than warfarin patients and had lower scores for QCI [28], CHA2DS2-VASc [29], and HAS-BLED [30]. Baseline HRU and costs were generally lower for rivaroxaban compared with warfarin, except ER visits and pharmacy fills. Matching provided 9999 pairs of patients with AF, obesity, and diabetes that were well balanced (Table 2). The mean (standard deviation [SD]) follow-up time from index date to the earlier of health plan disenrollment or end of study was 2.3 (1.9) years for the rivaroxaban cohort and 2.5 (2.0) years for the warfarin cohort.
Outcomes
In the intent-to-treat analysis, rate ratios for all-cause HRU were significantly lower in the rivaroxaban cohort compared with the warfarin cohort for all settings, except ER visits (Table 3). The proportion of patients with 30-day rehospitalization was significantly lower with rivaroxaban versus warfarin (24% vs 26%; odds ratio = 0.93; P = 0.0189). The mean (SD) length of hospital stay was 16 (34) days for rivaroxaban and 21 (41) days for warfarin for all patients (P < 0.0001) and 25 (40) days versus 31 (47) days, respectively, for patients with at least one hospitalization (P < 0.0001).
Similar results were obtained for NVAF-related HRU, with rate ratios significantly lower in the rivaroxaban cohort versus the warfarin cohort for inpatient hospitalizations, ER visits, hospital outpatient visits, and physician office visits (Table 3). NVAF-related mean (SD) lengths of hospital stay were significantly shorter with rivaroxaban versus warfarin for all patients (15 [34] days vs 19 [40] days) and patients with at least one hospitalization (28 [42] days vs 33 [48] days).
The as-treated sensitivity analysis results for all-cause and NVAF-related HRU rate ratios were consistent with the intent-to-treat analysis, with the additional finding that ER visits were significantly lower in the rivaroxaban cohort versus the warfarin cohort (P < 0.05; Table 3). The length of hospital stay was significantly shorter for rivaroxaban compared with warfarin. For all-cause hospitalizations, the length of stay was 2 days shorter both in all patients and in patients with at least one hospitalization. For NVAF-related hospitalizations, the length of stay was 2 and 3 days shorter, respectively.
In the intent-to-treat analysis, all-cause total medical costs were $7816 PPPY lower in the rivaroxaban cohort compared with the warfarin cohort, with significantly lower costs in all settings, except ER visits (Fig. 2a). Total pharmacy costs were higher for rivaroxaban versus warfarin by $2542 PPPY, but the difference was offset by the larger reduction in medical costs (Fig. 2b). The total healthcare costs of medical and pharmacy costs combined were lower by $5266 PPPY for rivaroxaban compared with warfarin (P < 0.0001). NVAF-related medical costs were approximately half of the all-cause medical costs and were also lower for rivaroxaban versus warfarin ($1056 PPPY; P = 0.01; Fig. 2c). The drivers of medical costs related to NVAF were inpatient hospitalizations and physician office visits, with the latter being higher in the rivaroxaban cohort compared with the warfarin cohort.
All-cause a medical costs, b total costs, and c NVAF-relateda medical costs (2020 US dollars) for patients with NVAF, obesity, and diabetes newly initiating rivaroxaban or warfarin. ER emergency room, NVAF nonvalvular atrial fibrillation, PPPY per patient per year, SNF skilled nursing facility. aNVAF-related was defined as an encounter associated with an AF diagnosis in any position
The total cost advantage of rivaroxaban versus warfarin was maintained in the as-treated sensitivity analysis. All-cause total healthcare costs were reduced by $5459 for rivaroxaban versus warfarin, with total medical costs reduced by $10,879 and pharmacy costs increased by $5399 (Table 4). NVAF-related medical costs were reduced by $3466 in the rivaroxaban cohort compared with the warfarin cohort. For both all-cause and NVAF-related costs on an as-treated basis, medical costs were driven by inpatient hospitalizations and physician office visits. However, NVAF-related physician office visit costs were significantly higher in the rivaroxaban cohort versus the warfarin cohort ($518 PPPY; P = 0.0013).
Discussion
This real-world study compared HRU and costs of oral anticoagulation therapy with rivaroxaban versus warfarin in patients with NVAF who have concurrent obesity and diabetes. All-cause HRU was reduced with rivaroxaban versus warfarin in all settings, except ER visits. NVAF-related HRU remained significantly lower for rivaroxaban versus warfarin in all settings, particularly physician office visits and hospital outpatient visits. The length of hospital stay was significantly reduced by approximately 4–5 days in the rivaroxaban cohort compared with the warfarin cohort for both all-cause and NVAF-related hospitalizations. All-cause total healthcare costs were reduced by more than $5000 PPPY with rivaroxaban, and NVAF-related medical costs were reduced by approximately $1100 PPPY with rivaroxaban. The difference was driven mainly by lower costs for inpatient hospitalizations and physician office visits for rivaroxaban versus warfarin.
The efficacy of rivaroxaban and warfarin in overweight and obese patients with NVAF was analyzed using data from the ROCKET-AF trial, in which stroke and systemic embolism outcomes were lower compared with normal weight patients in both rivaroxaban and warfarin treatment groups [33]. Among patients with diabetes in ROCKET-AF, similar rates of stroke/systemic embolism were observed compared with patients who did not have diabetes [33, 34]. In addition, previously published real-world evidence studies demonstrated similar or improved effectiveness and safety of rivaroxaban versus warfarin in obese patients with NVAF [35,36,37,38,39]. Studies have also demonstrated the effectiveness and safety of rivaroxaban in patients with NVAF and concurrent diabetes [34, 40,41,42,43,44,45].
Our study findings are aligned with other retrospective analyses among patients with NVAF overall and in obese patients [35, 46, 47]. Among 2253 matched pairs of patients with NVAF newly initiating rivaroxaban or warfarin, all-cause and NVAF-related hospitalization costs were significantly lower with rivaroxaban compared with warfarin [47]. All-cause costs of outpatient visits were also significantly lower with rivaroxaban versus warfarin, while NVAF-related outpatient visit costs were lower but not statistically significant. Lower HRU and costs were also demonstrated with rivaroxaban versus warfarin in patients with NVAF who were morbidly obese despite similar effectiveness and safety of the anticoagulants [35]. Lower costs were driven by a lower hospitalization rate, shorter length of stay, and less outpatient and physician office service encounters for rivaroxaban versus warfarin [35]. Another recently published study evaluated HRU and costs in patients with NVAF and obesity who were newly initiating rivaroxaban or warfarin [46]. At 12 and 36 months, rivaroxaban was associated with lower all-cause and NVAF-related HRU driven primarily by lower outpatient visits. All-cause and NVAF-related costs were also lower with rivaroxaban versus warfarin as a result of lower hospitalization costs. Outpatient office visits and other visit costs were also lower with rivaroxaban versus warfarin. This claims-based study was extended to evaluate HRU and costs for patients with NVAF, obesity, and polypharmacy (defined as five or more concurrent outpatient prescriptions) [48]. Rivaroxaban was associated with significantly lower 12- and 36-month HRU and 12-month costs, driven by lower hospitalizations [48]. The lower hospitalization rates and shorter lengths of hospital stay associated with rivaroxaban versus warfarin suggest fewer healthcare interactions in patients treated with rivaroxaban [35, 47, 48]. These findings may be related to lack of need for routine monitoring and fewer drug–drug interactions with rivaroxaban in comparison to nearly monthly international normalized ratio monitoring that occurs with warfarin [35, 46, 48].
Although no data have specifically examined HRU and costs associated with anticoagulation therapy in patients with NVAF and diabetes, the Nationwide Inpatient Sample registry data found that 29% of AF-related hospitalizations occurred in patients with concurrent diabetes, and there was a temporal increase in the AF hospitalization rate among patients with diabetes [49]. No differences in costs were identified for patients with AF with and without diabetes, but there was a higher 30-day readmission risk for patients with diabetes. In our analysis, rivaroxaban was associated with a significantly lower 30-day rehospitalization rate. On the basis of results obtained using the National Readmission Database, readmitted patients with AF had a higher burden of comorbidities, and diabetes was among the most common comorbidities of hospitalized patients [50]. A higher burden of comorbidities was also predictive of higher cost of hospitalization for AF [50].
This study included the use of a geographically diverse healthcare claims database that represents both commercially insured and Medicare Advantage beneficiaries across the USA and 12 months of continuous health plan enrollment to better understand patient characteristics and outcomes over time. Propensity score matching was used to reduce selection biases, but there may be residual confounding as some factors were not available in the claims data; for example, we did not control for diabetes control, exercise, and smoking status. In this analysis, BMI was calculated using a validated machine learning algorithm, which allowed us to leverage the BMI information from claims data to assess HRU and costs. However, the algorithm may misclassify patients’ BMI category. Other limitations of administrative claims data include coding errors and inconsistencies. The time in therapeutic international normalized ratio range was not assessed for warfarin patients because of limited laboratory data. HRU and costs were limited to the patient population studied and may not be generalizable to the broader US population, such as those who are uninsured or have a different insurance coverage (e.g., Medicaid). Moreover, prescription claims do not indicate that the medication was taken as prescribed, and medications provided as samples by physicians or over-the-counter medications are not captured in these data. Costs provided in the Optum DOD database are standardized costs, which may underestimate the actual costs for commercial plans and overestimate the actual costs for Medicare Advantage plans. Finally, even with propensity score matching to balance the study cohorts, residual confounding cannot be excluded.
Conclusions
The results of this analysis provide valuable information on HRU and costs among patients with NVAF, obesity, and diabetes, showing that rivaroxaban is associated with lower HRU and costs compared with warfarin.
References
Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2020;42(5):373–498.
Raebel MA, Malone DC, Conner DA, Xu S, Porter JA, Lanty FA. Health services use and health care costs of obese and nonobese individuals. Arch Intern Med. 2004;164(19):2135–40.
Nalliah CJ, Sanders P, Kottkamp H, Kalman JM. The role of obesity in atrial fibrillation. Eur Heart J. 2016;37(20):1565–72.
Darvall KA, Sam RC, Silverman SH, Bradbury AW, Adam DJ. Obesity and thrombosis. Eur J Vasc Endovasc Surg. 2007;33(2):223–33.
Pouwels S, Topal B, Knook MT, et al. Interaction of obesity and atrial fibrillation: an overview of pathophysiology and clinical management. Expert Rev Cardiovasc Ther. 2019;17(3):209–23.
Smith BA. The epidemic of obesity and diabetes: trends and treatments. Tex Heart Inst J. 2011;38(2):142–4.
Bhupathiraju SN, Hu FB. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ Res. 2016;118(11):1723–35.
Stroke Risk in Atrial Fibrillation Working Group. Independent predictors of stroke in patients with atrial fibrillation: a systematic review. Neurology. 2007;69(6):546–54.
Echouffo-Tcheugui JB, Shrader P, Thomas L, et al. Care patterns and outcomes in atrial fibrillation patients with and without diabetes: ORBIT-AF Registry. J Am Coll Cardiol. 2017;70(11):1325–35.
Papazoglou AS, Kartas A, Samaras A, et al. Prognostic significance of diabetes mellitus in patients with atrial fibrillation. Cardiovasc Diabetol. 2021;20(1):40.
Kim YG, Han KD, Choi JI, et al. The impact of body weight and diabetes on new-onset atrial fibrillation: a nationwide population based study. Cardiovasc Diabetol. 2019;18(1):128.
Grundvold I, Bodegard J, Nilsson PM, et al. Body weight and risk of atrial fibrillation in 7,169 patients with newly diagnosed type 2 diabetes; an observational study. Cardiovasc Diabetol. 2015;14:5.
Singleton MJ, German CA, Soliman EZ, et al. Body mass index, sex, and incident atrial fibrillation in biabetes: the ACCORD trial. JACC Clin Electrophysiol. 2020;6(13):1713–20.
Finkelstein EA, Khavjou OA, Thompson H, et al. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42(6):563–70.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief. 2020;360:1–8.
Tremmel M, Gerdtham UG, Nilsson PM, Saha S. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14(4):435.
Cawley J, Biener A, Meyerhoefer C, et al. Direct medical costs of obesity in the United States and the most populous states. J Manag Care Spec Pharm. 2021;27(3):354–66.
Edwards CH, Aas E, Kinge JM. Body mass index and lifetime healthcare utilization. BMC Health Serv Res. 2019;19(1):696.
January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart Rhythm Society in collaboration with the Society of Thoracic Surgeons. Circulation. 2019;140(2):e125–51.
Martin K, Beyer-Westendorf J, Davidson BL, Huisman MV, Sandset PM, Moll S. Use of the direct oral anticoagulants in obese patients: guidance from the SSC of the ISTH. J Thromb Haemost. 2016;14(6):1308–13.
Sebaaly J, Kelley D. Direct oral anticoagulants in obesity: an updated literature review. Ann Pharmacother. 2020;54(11):1144–58.
Grymonprez M, De Backer TL, Steurbaut S, Boussery K, Lahousse L. Non-vitamin K antagonist oral anticoagulants (NOACs) versus warfarin in patients with atrial fibrillation and (morbid) obesity or low body weight: a systematic review and meta-analysis. Cardiovasc Drugs Ther. 2021. https://doi.org/10.1007/s10557-020-07122-6.
Buck MM, Haddon AM, Paneccasio A, et al. Safety and efficacy of rivaroxaban and apixaban in patients with increased body mass: a systematic review. Clin Drug Investig. 2021;41(4):353–69.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Xarelto® (rivaroxaban) tablets, for oral use. Prescribing information. Titusville: Janssen Pharmaceuticals, Inc.; 2021.
Wu B, Chow W, Sakthivel M, et al. Body mass index variable interpolation to expand the utility of real-world administrative healthcare claims database analyses. Adv Ther. 2021;38(2):1314–27.
Cunningham A, Stein CM, Chung CP, Daugherty JR, Smalley WE, Ray WA. An automated database case definition for serious bleeding related to oral anticoagulant use. Pharmacoepidemiol Drug Saf. 2011;20(6):560–6.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82.
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137(2):263–72.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–100.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–79.
Office for Human Research Protections. Coded private information or specimens use in research, guidance. 2008. https://www.hhs.gov/ohrp/regulations-and-policy/guidance/research-involving-coded-private-information/index.html. Accessed 5 Oct 2021.
Balla SR, Cyr DD, Lokhnygina Y, et al. Relation of risk of stroke in patients with atrial fibrillation to body mass index (from patients treated with rivaroxaban and warfarin in the rivaroxaban once daily oral direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation trial). Am J Cardiol. 2017;119(12):1989–96.
Bansilal S, Bloomgarden Z, Halperin JL, et al. Efficacy and safety of rivaroxaban in patients with diabetes and nonvalvular atrial fibrillation: the Rivaroxaban Once-daily, Oral, Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF Trial). Am Heart J. 2015;170(4):675-82.e8.
Peterson ED, Ashton V, Chen YW, Wu B, Spyropoulos AC. Comparative effectiveness, safety, and costs of rivaroxaban and warfarin among morbidly obese patients with atrial fibrillation. Am Heart J. 2019;212:113–9.
Costa OS, Beyer-Westendorf J, Ashton V, et al. Effectiveness and safety of rivaroxaban versus warfarin in obese nonvalvular atrial fibrillation patients: analysis of electronic health record data. Curr Med Res Opin. 2020;36(7):1081–8.
Briasoulis A, Mentias A, Mazur A, Alvarez P, Leira EC, Vaughan Sarrazin MS. Comparative effectiveness and safety of direct oral anticoagulants in obese patients with atrial fibrillation. Cardiovasc Drugs Ther. 2021;35(2):261–72.
Perales IJ, San Agustin K, DeAngelo J, Campbell AM. Rivaroxaban versus warfarin for stroke prevention and venous thromboembolism treatment in extreme obesity and high body weight. Ann Pharmacother. 2020;54(4):344–50.
Kushnir M, Choi Y, Eisenberg R, et al. Efficacy and safety of direct oral factor Xa inhibitors compared with warfarin in patients with morbid obesity: a single-centre, retrospective analysis of chart data. Lancet Haematol. 2019;6(7):e359–65.
Itzhaki Ben Zadok O, Eisen A. Use of non-vitamin K oral anticoagulants in people with atrial fibrillation and diabetes mellitus. Diabet Med. 2018;35(5):548–56.
Patti G, Di Gioia G, Cavallari I, Nenna A. Safety and efficacy of nonvitamin K antagonist oral anticoagulants versus warfarin in diabetic patients with atrial fibrillation: a study-level meta-analysis of phase III randomized trials. Diabetes Metab Res Rev. 2017;33(3):e2876.
Coleman CI, Bunz TJ, Eriksson D, Meinecke AK, Sood NA. Effectiveness and safety of rivaroxaban vs warfarin in people with non-valvular atrial fibrillation and diabetes: an administrative claims database analysis. Diabet Med. 2018;35(8):1105–10.
Baker WL, Beyer-Westendorf J, Bunz TJ, et al. Effectiveness and safety of rivaroxaban and warfarin for prevention of major adverse cardiovascular or limb events in patients with non-valvular atrial fibrillation and type 2 diabetes. Diabetes Obes Metab. 2019;21(9):2107–14.
Chan YH, Lee HF, Li PR, et al. Effectiveness, safety, and major adverse limb events in atrial fibrillation patients with concomitant diabetes mellitus treated with non-vitamin K antagonist oral anticoagulants. Cardiovasc Diabetol. 2020;19(1):63.
Coleman CI, Costa OS, Brescia CW, Vardar B, Abdelgawwad K, Sood N. Thromboembolism, bleeding and vascular death in nonvalvular atrial fibrillation patients with type 2 diabetes receiving rivaroxaban or warfarin. Cardiovasc Diabetol. 2021;20(1):52.
Berger JS, Laliberte F, Kharat A, et al. Healthcare resource utilization and costs of rivaroxaban versus warfarin among non-valvular atrial fibrillation (NVAF) patients with obesity in a US population. J Med Econ. 2021;24(1):550–62.
Laliberte F, Cloutier M, Crivera C, et al. Effect of rivaroxaban versus warfarin on health care costs among nonvalvular atrial fibrillation patients: observations from rivaroxaban users and matched warfarin users. Adv Ther. 2015;32(3):216–27.
Laliberte F, Ashton V, Kharat A, et al. Economic burden of rivaroxaban and warfarin among nonvalvular atrial fibrillation patients with obesity and polypharmacy. J Comp Eff Res. 2021. https://doi.org/10.2217/cer-2021-0150.
Kumar N, Echouffo-Tcheugui JB. Diabetes and atrial fibrillation in hospitalized patients in the United States. Clin Cardiol. 2021;44(3):340–8.
Tripathi B, Atti V, Kumar V, et al. Outcomes and resource utilization associated with readmissions after atrial fibrillation hospitalizations. J Am Heart Assoc. 2019;8(19):e013026.
Acknowledgements
Funding
This work was supported by Janssen Scientific Affairs, LLC. The study sponsor also funded the journal’s Rapid Service Fee.
Medical Writing and Other Assistance
Medical writing support was provided by Michelle McDermott, PharmD, of Cello Health Communications/MedErgy (Yardley, PA), which was funded by Janssen Scientific Affairs, LLC (Titusville, NJ). Data programming support was provided by Rachapudi Sai Sarath, Mu Sigma Business Solutions Pvt. Ltd., Bengaluru, India, and was funded by Janssen Scientific Affairs, LLC (Titusville, NJ).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors' Contributions
Matthew R. Weir, Yen-Wen Chen, Jinghua He, Brahim Bookhart, Alicia Campbell, and Veronica Ashton contributed to study conception/design and data interpretation. Yen-Wen Chen and Jinghua He contributed to collection and assembly of data, and data analysis. All authors reviewed and approved the final content of this manuscript.
Disclosures
Matthew R. Weir has served as a scientific advisor for Janssen, AstraZeneca, NovoNordisk, Merck, Boehringer Ingelheim, Bayer, and Vifor. Yen-Wen Chen is a full-time employee of Janssen Scientific Affairs, LLC. Jinghua He is a full-time employee of Janssen Scientific Affairs, LLC. Brahim Bookhart is a full-time employee of Janssen Scientific Affairs, LLC. Alicia Campbell is a full-time employee of Janssen Scientific Affairs, LLC. Veronica Ashton is a full-time employee of Janssen Scientific Affairs, LLC.
Compliance with Ethics Guidelines
This study is based on de-identified data collected from a healthcare claims database and does not contain any experimental data with human or animal participants; this analysis was deemed exempt from institutional review board oversight and informed consent was not obtained as per guidance from the Office for Human Research Protections [32].
Data Availability
Data for this study were available to the authors via third-party license from Optum, a commercial data provider in the United States, and Janssen Pharmaceuticals, which has a license for analysis of Optum’s de-identified Clinformatics® Data Mart Database—Date of Death database. As such, the authors cannot provide the raw data; however, other researchers may access the data by purchase through Optum, and the inclusion criteria specified in the methods would allow them to identify the same cohort of patients. Interested individuals may visit www.optum.com/contact.html for more information on accessing Optum’s de-identified Clinformatics® Data Mart Database—Date of Death database.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third-party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Weir, M.R., Chen, YW., He, J. et al. Healthcare Resource Utilization and Costs of Rivaroxaban Versus Warfarin Among Nonvalvular Atrial Fibrillation Patients with Obesity and Diabetes. Diabetes Ther 12, 3167–3186 (2021). https://doi.org/10.1007/s13300-021-01161-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01161-4