Abstract
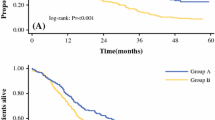
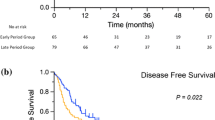
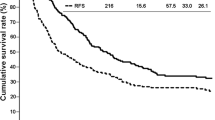
Currently, the only available curative treatment for intrahepatic cholangiocarcinoma (ICC) is surgical resection, but the survival outcomes are still disappointing. This study aimed to present the surgical outcomes of a large series of ICC patients and investigate the prognostic factors for recurrence and survival. From January 2003 to December 2013, a series of consecutive patients with ICC who underwent curative-intent resection were enrolled. Historical patient records and follow-up results were collected and analyzed. A total of 1842 patients were included in the study, of which 328 (17.8%) experienced complications after surgery with a mortality of 0.3%. The overall survival rates of the entire cohort at 1, 3, and 5 years were 72.5%, 46.9%, and 37.3%, respectively, while the disease-free survival rates at 1, 3, and 5 years were 55.8%, 39.0%, and 23.7%, respectively. Elevated alpha-fetoprotein level, elevated carbohydrate antigen 19–9 level, tumor size > 10 cm, lymphadenectomy, positive lymph node, macrovascular invasion, microvascular invasion, and adjuvant transarterial chemoembolization after surgery were independent predictors for recurrence, while hepatolithiasis, viral hepatitis, elevated carbohydrate antigen 19–9 level, tumor size > 10 cm, lymphadenectomy, positive lymph node, and macrovascular and microvascular invasion were independent prognostic factors for overall survival. Liver resection is safe to treat ICC even when combined with lymphadenectomy. Adequate regional lymphadenectomy should be recommended for all resectable ICC patients to obtain final pathological examination which is essential for predicting recurrence and survival.


Similar content being viewed by others
Data Availability
Clinical data of patients is attached as supplementary material.
References
Tsilimigras DI, Rittal M, Dimitrios M et al (2020) A machine-based approach to preoperatively identify patients with the most and least benefit associated with resection for intrahepatic cholangiocarcinoma: an international multi-institutional analysis of 1146 patients. Ann Surg Oncol 27:1110–1119
Clements O, Eliahoo J, Kim JU et al (2020) Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: a systematic review and meta-analysis. J Hepatol 72:95–103
Guglielmi A, Ruzzenente A, Campagnaro T et al (2009) Intrahepatic cholangiocarcinoma: prognostic factors after surgical resection. World J Surg 33:1247–1254
Berretta M, Cavaliere C, Alessandrini L et al (2017) Serum and tissue markers in HCC and cholangiocarcinoma: clinical and prognostic implications. Oncotarget 8:14192–14220
Altman AM, Kizy S, Marmor S et al (2018) Current survival and treatment trends for surgically resected intrahepatic cholangiocarcinoma in the United States. J Gastrointest Oncol 9:942–952
Ke Q, Lin N, Deng M et al (2020) The effect of adjuvant therapy for patients with intrahepatic cholangiocarcinoma after surgical resection: a systematic review and meta-analysis. PLoS One 15:e0229292
Mazzaferro V, Gorgen A, Roayaie S et al (2020) Liver resection and transplantation for intrahepatic cholangiocarcinoma. J Hepatol 72:364–377
Hyder O, Marques H, Pulitano C et al (2014) A nomogram to predict long-term survival after resection for intrahepatic cholangiocarcinoma: an eastern and western experience. JAMA Surg 149:432–438
DeOliviera ML, Cunningham SC, Cameron JL et al (2007) Cholangiocarcinoma: thirty-one year experience with 564 patients at a single institution. Ann Surg 245:755–762
Paik KY, Jung JC, Heo JS et al (2008) What prognostic factors are important for resected intrahepatic cholangiocarcinoma? J Gastroenterol Hepatol 23:766–770
Inoue K, Makuuchi M, Takayama T et al (2000) Long-term survival and prognostic factors in the surgical treatment of mass-forming type cholangiocarcinoma. Surgery 127:498–505
Valverde A, Bonhomme N, Farges O et al (1999) Resection of intrahepatic cholangiocarcinoma: a Western experience. J Hepatobiliary Pancreat Surg 6:122–127
Shimada K, Sano T, Sakamoto Y et al (2007) Surgical outcomes of the mass-forming plus periductal infiltrating types of intrahepatic cholangiocarcinoma: a comparative study with the typical mass-forming type of intrahepatic cholangiocarcinoma. World J Surg 31:2016–2022
Chen MF, Jan YY, Jeng LB et al (1999) Intrahepatic cholangiocarcinoma in Taiwan. J Hepatobiliary Pancreat Surg 6:136–141
Endo I, Gonen M, Yopp AC et al (2008) Intrahepatic cholangiocarcinoma: rising frequency, improved survival, and determinants of outcome after resection. Ann Surg 248:84–96
Kitagawa Y, Nagino M, Kamiya J et al (2001) Lymph node metastasis from hilar cholangiocarcinoma: audit of 110 patients who underwent regional and paraaortic node dissection. Ann Surg 233:385–392
Ueno M, Morizane C, Ikeda M et al (2019) A review of changes to and clinical implications of the eighth TNM classification of hepatobiliary and pancreatic cancers. Jpn J Clin Oncol 49:1073–1082
Jutric Z, Johnston WC, Hoen HM et al (2016) Impact of lymph node status in patients with intrahepatic cholangiocarcinoma treated by major hepatectomy: a review of the National Cancer Database. HPB 18:79–87
Wu R, Zhang G, Feng J et al (2020) Proposal of the optimal numbers of examined and positive lymph nodes to the 8th edition of American Joint Committee on Cancer (AJCC) staging for 758 patients with distal cholangiocarcinoma. PLoS One 15:e0234464
Zhou R, Lu D, Li W et al (2019) Is lymph node dissection necessary for resectable intrahepatic cholangiocarcinoma? A systematic review and meta-analysis. HPB 21:784–792
Shimada M, Yamashita Y, Aishima S et al (2001) Value of lymph node dissection during resection of intrahepatic cholangiocarcinoma. Br J Surg 88:1463–1466
Morine Y, Shimada M (2015) The value of systematic lymph node dissection for intrahepatic cholangiocarcinoma from the viewpoint of liver lymphatics. J Gastroenterol 50:13–27
Kizy S, Altman AM, Marmor S et al (2019) Surgical resection of lymph node positive intrahepatic cholangiocarcinoma may not improve survival. HPB 21:235–241
Csa B, Fr C, Acd E et al (2022) Survival benefit of adequate lymphadenectomy in patients undergoing liver resection for clinically node negative intrahepatic cholangiocarcinoma. J Hepatol 78:356–363
Chen C, Su J, Wu H et al (2023) Prognostic value of lymphadenectomy in node-negative intrahepatic cholangiocarcinoma: a multicenter, retrospectively study. Eur J Surg Oncol 49:780–787
Valle J, Wasan H, Palmer DH et al (2010) Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med 362:1273–1281
Cherqui D, Bassam Tantawi B, Alon R et al (1995) Intrahepatic cholangiocarcinoma. Results of aggressive surgical treatment. Arch Surg 130:1073–1078
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation and data collection were performed by Xiaodong Shi and Jianbing Xuan. Liang Huang and Jianjun Yan provided methodology. The first draft of the manuscript was written by Xingwu Zhu and Maixuan Qiu, and was revised by Jing Li. All the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the Ethics Committee of the Eastern Hepatobiliary Hospital, and it followed the standards of the Declaration of Helsinki.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, X., Shi, X., Qiu, M. et al. Liver Resection for Intrahepatic Cholangiocarcinoma: Clinical Outcomes and Prognostic Factors in a Series of 1842 Patients at a Single Center. Indian J Surg 85, 1427–1433 (2023). https://doi.org/10.1007/s12262-023-03815-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-023-03815-y