Abstract
Background
Intrahepatic cholangiocarcinoma (ICC) is the second most common primary liver tumor. The resectability rate is low because at the time of diagnosis this disease is frequently beyond the limits of surgical therapy. Curative resection (R0) is the most effective treatment and the only therapy associated with prolonged disease-free survival. Based on the gross appearance of the tumor the Liver Cancer Study Group of Japan (LCSGJ) defined three types: mass-forming type (MF), periductal infiltrating type (PI), intraductal growth (IG) type. The prognostic significance of gross type has been demonstrated in Eastern countries, but this issue has not been clarified in Western countries. The aim of this study was to identify the prognostic factors for survival in a group of patients submitted to surgical resection for ICC.
Methods
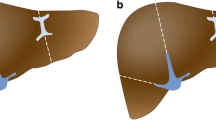
Between 1990 and 2007 a total of 81 consecutive patients with ICC were submitted to surgery. Patients with peritoneal carcinomatosis, extensive vascular involvement, or multiple intrahepatic metastases were excluded from surgical resection. Tumors were classified according to TMN stage (6th edition, 2002) and LCSGJ gross type classification. Tumor gross appearance on the cut surface was categorized into the following types according to the classification proposed by the Liver Cancer Study Group of Japan: MF, PI, or IG type.
Results
During the study period 52 patients were submitted to surgical resection with curative intent, whereas in 29 patients surgery was limited to explorative laparotomy. Curative resection (R0) was achieved in 43 patients (83%); and a major hepatic resection was performed in 63% (33/52) of the patients. Extrahepatic bile duct resection was carried out in 36% (19/52) of cases. According to the LCSGJ classification, the MF type was present in 34 patients (65%), the MF + PI type in 13 (25%), the PI type in 3 (6%), and the IG type in 2 (4%). Overall median survival time was 40 months, with a 1-, 3-, and 5-year actuarial survival rates of 83%, 50%, 20%, respectively. Survival was significantly related to the macroscopic gross type, with a median survival of 50 months for patients with the MF type, 19 months for the MF + PI type, 15 months for the PI type, and 17 months for the IG type. At univariate analysis, the macroscopic gross appearance of the tumor, the presence of lymph node metastasis, involvement of extrahepatic bile ducts, the presence of macroscopic vascular invasion, and positive resection margins were significant related to survival. At multivariate analysis, macroscopic vascular invasion and lymph nodes metastases were significant related to survival with hazard ratios of 4.11 and 2.79, respectively. Further statistical analyses were carried out to identify the relation between macroscopic gross type and prognosis. We identified that the MF + PI type tumors were significantly associated with negative prognostic factors, such as the involvement of extrahepatic bile ducts, the presence of lymph nodes metastases, the presence of macroscopic vascular invasion, the presence of perineural invasion, and higher T stage.
Conclusions
Curative resection of ICC is the only therapy that can achieve long-term survival. The best results were observed in patients who underwent R0 resection for MF tumors without lymph node metastases or vascular invasion. Important predictive factors related to poor survival are MF + PI macroscopic tumor type, lymph node metastases, and vascular invasion. In these patients, other therapeutic approaches (i.e., adjuvant or neoadjuvant therapy) should be evaluated to improve results.

Similar content being viewed by others
References
Harrison LE, Fong Y, Klimstra DS et al (1998) Surgical treatment of 32 patients with peripheral intrahepatic cholangiocarcinoma. Br J Surg 85:1068–1070
Yamamoto M, Takasaki K, Yoshikawa T et al (1998) Does gross appearance indicate prognosis in intrahepatic cholangiocarcinoma? J Surg Oncol 69:162–167
Madariaga JR, Iwatsuki S, Todo S et al (1998) Liver resection for hilar and peripheral cholangiocarcinomas: a study of 62 cases. Ann Surg 227:70–79
Yamanaka N, Okamoto E, Ando T et al (1995) Clinicopathologic spectrum of resected extraductal mass-forming intrahepatic cholangiocarcinoma. Cancer 76:2449–2456
Lieser MJ, Barry MK, Rowland C et al (1998) Surgical management of intrahepatic cholangiocarcinoma: a 31-year experience. J Hepatobiliary Pancreat Surg 5:41–47
Lang H, Sotiropoulos GC, Fruhauf NR et al (2005) Extended hepatectomy for intrahepatic cholangiocellular carcinoma (ICC): when is it worthwhile? Single center experience with 27 resections in 50 patients over a 5-year period. Ann Surg 241:134–143
Cherqui D, Tantawi B, Alon R et al (1995) Intrahepatic cholangiocarcinoma: results of aggressive surgical management. Arch Surg 130:1073–1078
Seyama Y, Makuuchi M (2007) Current surgical treatment for bile duct cancer. World J Gastroenterol 13:1505–1515
Liver Cancer Study Group of Japan (2003) General rules for clinical and pathological study of primary liver cancer. 2nd English edition. Kanehara, Tokyo
Nozaki Y, Yamamoto M, Ikai I et al (1998) Reconsideration of the lymph node metastasis pattern (N factor) from intrahepatic cholangiocarcinoma using the International Union Against Cancer TNM staging system for primary liver carcinoma. Cancer 83:1923–1929
Isaji S, Kawarada Y, Taoka H et al (1999) Clinicopathological features and outcome of hepatic resection for intrahepatic cholangiocarcinoma in Japan. J Hepatobiliary Pancreat Surg 6:108–116
Morimoto Y, Tanaka Y, Ito T et al (2003) Long-term survival and prognostic factors in the surgical treatment for intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Surg 10:432–440
Ohtsuka M, Ito H, Kimura F et al (2002) Results of surgical treatment for intrahepatic cholangiocarcinoma and clinicopathological factors influencing survival. Br J Surg 89:1525–1531
Anonymous (2000) The Brisbane 2000 terminology of liver anatomy and resections. HPB 2:333–339
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Sobin LH, Wittekind C (eds) (2002) TNM classification of malignant tumours, 6th edn. Wiley, New York
Kawarada Y, Yamagiwa K, Das BC (2002) Analysis of the relationships between clinicopathologic factors and survival time in intrahepatic cholangiocarcinoma. Am J Surg 183:679–685
Suzuki S, Sakaguchi T, Yokoi Y et al (2002) Clinicopathological prognostic factors and impact of surgical treatment of mass-forming intrahepatic cholangiocarcinoma. World J Surg 26:687–693
DeOliveira ML, Cunningham SC, Cameron JL et al (2007) Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg 245:755–762
Okabayashi T, Yamamoto J, Kosuge T et al (2001) A new staging system for mass-forming intrahepatic cholangiocarcinoma: analysis of preoperative and postoperative variables. Cancer 92:2374–2383
Uenishi T, Yamazaki O, Yamamoto T et al (2005) Serosal invasion in TNM staging of mass-forming intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Surg 12:479–483
Lang H, Lang H, Sotiropoulos GC et al (2006) Surgical therapy of intrahepatic cholangiocellular carcinoma. Chirurg 77:53–60
Isa T, Kusano T, Shimoji H et al (2001) Predictive factors for long-term survival in patients with intrahepatic cholangiocarcinoma. Am J Surg 181:507–511
Nagakawa T, Kayahara M, Ikeda S et al (2002) Biliary tract cancer treatment: results from the Biliary Tract Cancer Statistics Registry in Japan. J Hepatobiliary Pancreat Surg 9:569–575
Ikai I, Arii S, Ichida T et al (2005) Report of the 16th follow-up survey of primary liver cancer. Hepatol Res 32:163–172
Miwa S, Miyagawa S, Kobayashi A et al (2006) Predictive factors for intrahepatic cholangiocarcinoma recurrence in the liver following surgery. J Gastroenterol 4:893–900
Nakagawa T, Kamiyama T, Kurauchi N et al (2005) Number of lymph node metastases is a significant prognostic factor in intrahepatic cholangiocarcinoma. World J Surg 29:728–733
Yamamoto M, Takasaki K, Yoshikawa T (1999) Lymph node metastasis in intrahepatic cholangiocarcinoma. Jpn J Clin Oncol 29:147–150
Tsuji T, Hiraoka T, Kanemitsu K et al (2001) Lymphatic spreading pattern of intrahepatic cholangiocarcinoma. Surgery 129:401–407
Hirohashi K, Uenishi T, Kubo S et al (2002) Histologic bile duct invasion by a mass-forming intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Surg 9:233–236
Shimada K, Sano T, Sakamoto Y et al (2007) Surgical outcomes of the mass-forming plus periductal infiltrating types of intrahepatic cholangiocarcinoma: a comparative study with the typical mass-forming type of intrahepatic cholangiocarcinoma. World J Surg 31:2016–2022
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guglielmi, A., Ruzzenente, A., Campagnaro, T. et al. Intrahepatic Cholangiocarcinoma: Prognostic Factors After Surgical Resection. World J Surg 33, 1247–1254 (2009). https://doi.org/10.1007/s00268-009-9970-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-9970-0