Abstract
Krüppel-like factor 4 (KLF4), a zinc finger transcription factor, is found in different human tissues and shows diverse regulatory activities in a cell-dependent manner. In the brain, KLF4 controls various neurophysiological and neuropathological processes, and its contribution to various neurological diseases has been widely reported. Parkinson’s disease (PD) is an age-related neurodegenerative disease that might have a connection with KLF4. In this review, we discussed the potential implication of KLF4 in fundamental molecular mechanisms of PD, including aberrant proteostasis, neuroinflammation, apoptosis, oxidative stress, and iron overload. The evidence collected herein sheds new light on KLF4-mediated pathways, which manipulation appears to be a promising therapeutic target for PD management. However, there is a gap in the knowledge on this topic, and extended research is required to understand the translational value of the KLF4-oriented therapeutical approach in PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kruppel-like factor 4 (KLF4), a zinc finger transcription family member, was originally isolated from an NIH3T3 cDNA library in 1996 [1, 2]. KLF4 is a highly conserved factor found in many organisms, from zebrafish to humans, and it is expressed in numerous human tissues, such as intestinal epithelial cells, skin, and neural stem cells [3,4,5]. KLF4 plays a significant role in controlling multiple biological pathways, including proliferation, embryogenesis, differentiation, neuroinflammation, oxidative stress, and apoptosis [6,7,8,9,10]. In the CNS, KLF4 controls the proliferation, migration, and differentiation of neural stem cells (NSCs), axon regeneration, and migration of radial neurons by regulating STAT3 [11, 12]. KLF4 downregulation is critical for neural differentiation, and overexpression of KLF4 in NSCs impedes their proliferation and differentiation. Moreover, KLF4 has a higher expression in the embryonic brain, where it is involved in the self-renewal of embryonic stem cells and is gradually downregulated postnatally. In this regard, KLF4 dysregulation may lead to hydrocephalus [13]. Additionally, overexpression of KLF4 in the endothelial cells of the microvasculature in the CNS can result in the development of cerebral cavernous malformation [14]. Recently, the protective role of KLF4 via the Nrf2/Trx1 downstream pathway against the blood–brain barrier destruction after cerebral ischemia–reperfusion was demonstrated [15]. These findings align with the context-dependent function KLF4. Interestingly, a review of the literature by Cheng et al. indicates the implication of KLF4 to different neurological diseases like Parkinson’s disease (PD), Alzheimer’s disease (AD), epilepsy, schizophrenia, and hydrocephalus making it a potential therapeutic target for their management [16]. In neurodegenerative diseases, KLF4 has been found to regulate neuroinflammation, neuronal apoptosis, axon regeneration, and iron accumulation, all of which are relevant to the pathogenesis of AD [17, 18].
Huntington’s disease (HD) is a progressive neurological condition that arises from an abnormal increase in the number of CAG repeats within the huntingtin gene [19]. KLF4 is a reprogramming factor that is utilized in the generation of iPSCs from fibroblasts or peripheral blood mononuclear cells of individuals with HD [20]. iPSCs have been generated from somatic cells of HD patients and can serve as a valuable tool for studying the disease and developing potential therapies [20,21,22]. Furthermore, KLF4 is mentioned as one of the endogenous pluripotency-associated markers that are reactivated and expressed in the HD-iPSC lines.
PD is a progressive neurodegenerative disease with an alarming negative impact on individuals and healthcare systems in developed and developing countries [23, 24]. The current understanding of the underlying mechanisms of PD is mainly focused on the progressive degeneration of dopaminergic neurons in the substantia nigra, leading to a decrease in dopamine levels in the brain. Subsequently, it results in cardinal motor symptoms, including tremors, rigidity, balance issues, and loss of spontaneous movement [25, 26]. Despite the clear hallmarks of PD, the etiology of the disease is still obscure. The most prominent pathological feature is the aggregation of normal and abnormal strains of a presynaptic protein α-synuclein. The oligomeric forms of α-synuclein, which trigger inflammation and cause the death of neurons, are the most toxic species [27]. There is strong evidence that these α-synuclein inclusions are cell-to-cell propagated in a prion-like manner [28]. Microglia-mediated neuroinflammation is another critical PD hallmark for its pathogenesis [29]. In addition, oxidative stress, iron overload, mitochondrial dysfunction, impaired autophagy, and apoptosis contribute to the progressive degeneration of dopaminergic neurons in PD [30,31,32,33]. A review of the literature on this area found that KLF4 is associated with neurodegenerative diseases, including PD. Given that KLF4 regulates neuron apoptosis, synaptic regeneration, oxidative stress, autophagy, and neuroinflammatory responses, the knowledge about the relationship between KLF4 and PD pathogenesis may enable the identification of novel targets for PD treatment [16]. PD etiology and pathological heterogeneity require a variety of models replicating different aspects of PD in animals to understand the critical pathomechanisms of the disease. Most of them are based on the environmental contribution to the pathological features of PD through various neurotoxins.
MPTP and its metabolite MPP + , rotenone (ROT), and 6-OHDA are commonly used to induce parkinsonian traits and recapitulate the key pathological hallmarks of PD in animal models [34]. Significantly, these neurotoxin-based models have been demonstrated to stimulate KLF4 expression [35,36,37,38], which suggests its potential contribution to the pathogenesis of PD, thus making KLF4 a potential target in the battle against PD.
In this review, we critically discussed a few available data on the controlling role of KLF4 in autophagy, neuronal apoptosis, oxidative stress, neuroinflammation, and other related mechanisms to show the relation between KLF4 and the pathogenesis of PD, which may underlie the cellular and molecular hallmarks of the disease. Overall, the involvement of KLF4 in neuroprotection and antioxidant defense suggests its potential as a therapeutic target for PD. Further research is needed to elucidate the precise mechanisms by which KLF4 exerts its neuroprotective effects and to explore its therapeutic potential in PD models and clinical settings.
Overview of KLF4
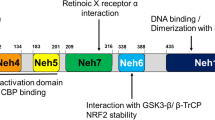
Shields et al. identified and characterized the nuclear transcription factor KLF4 in 1996 [1]. KLF4 was first recognized in the intestine thereafter, and it turned out that this transcription factor was expressed in different human tissues and organs [3,4,5]. KLF4 is a reprogramming factor directly connected to the Sp/Klf family, a group of 26 transcription factors essential for cellular pathways [39,40,41,42]. KLF4 is a highly conserved gene across all vertebrate lineage. In humans, the gene was detected on chromosome 9q31, which possesses a 6.3 kb chromosome region and contains five exons [43,44,45]. In mice, KLF4 was found on chromosome 4, which covers the 3.5 kb region detected by northern blot analysis [46]. The structure of the carboxy-terminal of KLF4 has DNA binding sites within Cys2His2 (C2H2) zinc finger motifs, which modulate transcription through binding to CACCC-box and GC-rich elements [40, 47]. On the other hand, the amino-terminal of KLF4 has a highly variable regulatory site for transcription and contains both the transactivation domain as well as repression domain that justifies its dual function [43, 48]. KLF4 acts as a complex, versatile transcription factor that switches between different modes, including trans activator, trans repressor, oncogene, and tumor suppressor. It also regulates adaptive responses to various intracellular and extracellular stresses, like environmental changes, DNA damage, and oxidative stress [7, 49,50,51,52]. KLF4 is responsible for numerous cellular and biological processes via inducing cell cycle arrest, genomic stability, growth arrest, stem cell self-renewal, and apoptosis [53].
Reports depicted a high expression of KLF4 in neural stem cells and different parts of the brain, like the hypothalamus, hippocampus, and cerebral cortex [11, 13, 18, 54, 55]. Many studies demonstrated KLF4 regulatory role in neuronal apoptosis, neuroinflammation, and nerve regeneration [17, 18, 55, 56]. KLF4 is involved in the regulation of neuroinflammation in AD. Neuroinflammation, a key factor in the development of AD, involves the activation of glial cells and the release of pro-inflammatory cytokines. Research has shown that there is a direct relationship between the expression of KLF4 and the occurrence of neuroinflammation induced by Aβ42. Oligomeric Aβ42 can increase KLF4 expression in microglial BV2 cells, mediated by activated P53 [17, 18]. Furthermore, in a study by Ahn et al., KLF4 expression was examined in the spinal cords of rats with EAE. The authors found increased KLF4 expression in the spinal cords of EAE rats compared to control rats. This suggests that KLF4 may play a role in the inflammatory response in the CNS during EAE and potentially in MS [57]. Chahoki et al. reported that the dysregulation of KLF4 and its correlation with miR-25-3p in EAE indicates a potential role for KLF4 in the pathogenesis of MS and highlights the complex interplay between transcription factors and microRNAs in autoimmune diseases. Additionally, KLF4 is involved in T cell development and has been shown to regulate Th17 cell differentiation, which plays a pathogenic role in EAE [58]. Additionally, Moore and colleagues demonstrated that the decrease in KLF4 expression led to the growth of axons in retinal ganglion cells following injury to the optic nerve [59]. Given the multifunctionality of KLF4 within CNS, its implication for the management of neurodegenerative disease can be considered (Fig. 1).
Multifunctionality of KLF4 and its implication to neurodegeneration management. Neuroinflammation plays a crucial role in the development of PD. It refers to the inflammation that occurs in the central nervous system as a result of molecules released from immune cells present in the brain or circulating in the blood. KLF4 plays a role in controlling oxidative stress and apoptosis in PD. It promotes oxidative stress and apoptosis, potentially through the inhibition of antioxidant enzymes
Relevance of KLF4 in Parkinson’s Disease
Role of KLF4 in Neuroinflammation
Neuroinflammation is a key contributor to the development and progression of PD [60, 61]. It is characterized by the activation of microglia and the release of pro-inflammatory molecules [62]. Chronic inflammation plays a role in the deterioration of dopaminergic neurons in the substantia nigra, which is responsible for the motor symptoms observed in PD [63]. Microglia can polarize into two phenotypes: M1 and M2 [64]. M1 microglia have a pro-inflammatory phenotype and release cytokines such as IL-1β and iNOS, which contribute to neuronal damage [65]. On the other hand, M2 microglia have an anti-inflammatory phenotype and release cytokines such as arginase-1 and CD163, which promote tissue repair and neuroprotection [66]. KLF4 has been recognized as a critical factor in controlling the polarization of microglial cells towards the M2 phenotype [67]. It promotes the expression of M2 markers, such as arginase-1, and inhibits the expression of M1 markers, such as iNOS and pro-inflammatory cytokines [68]. This shift towards the M2 phenotype is associated with a reduction in neuroinflammation and an improvement in neuronal survival. The activation of the PI3K/AKT pathway plays a vital role in limiting pro-inflammatory responses and promoting anti-inflammatory responses in macrophages [69]. The PI3K/AKT pathway is one of the signaling pathways that regulates the activation of KLF4 in microglia [70]. Activation of the PI3K/AKT pathway phosphorylates and activates AKT, which further activates KLF4 [71]. This suggests that the PI3K/AKT/KLF4 signaling axis plays a crucial role in regulating microglial polarization and neuroinflammation. In the study of El-Deeb et al., Flibanserin (Flib), a 5HT1A receptor modulator, was found to activate the PI3K/AKT pathway and induce the expression of KLF4 in a rat model of PD induced by Rotenone. The administration of Flib led to the activation of KLF4, which caused a transformation of microglial polarization from the inflammatory M1 phenotype to the anti-inflammatory M2 phenotype. This shift was associated with a reduction in pro-inflammatory markers and an improvement in motor function and neuronal integrity [72]. Overall, KLF4 plays a crucial role in regulating neuroinflammation by modulating microglial polarization. Activation of KLF4 promotes the M2 phenotype, which has anti-inflammatory and neuroprotective effects. Targeting the PI3K/AKT/KLF4 signaling axis may have therapeutic potential for neuroinflammatory diseases, including Parkinson’s disease.
When microglial cells are stimulated with lipopolysaccharide (LPS), KLF4 expression increases, and it translocates to the nucleus [73]. In the nucleus, KLF4 interacts with specific promoter elements of pro-inflammatory cytokine genes, such as TNF-α, MCP-1, and IL-6, and upregulates their expression [74, 75]. This leads to increased production of these cytokines, which are known to play a key role in neuroinflammation [73]. Additionally, KLF4 is also involved in the upregulation of iNOS and Cox-2, which are enzymes involved in the inflammatory response [73, 76]. Knockdown of KLF4 in microglial cells results in decreased expression of iNOS and Cox-2, leading to a decrease in NO production [77]. Kaushik et al. showed that the expression of the transcription factor Klf4 increased in BV-2 microglial cells in response to LPS treatment. The increase in KLF4 expression was dose-dependent and time-dependent, with higher doses of LPS and longer treatment times leading to higher levels of KLF4 expression. They also found that LPS treatment induced the expression of inflammatory mediators, including iNOS, Cox-2, and pro-inflammatory cytokines, in BV-2 cells. Furthermore, they demonstrated that KLF4 knockdown resulted in decreased expression of iNOS and reduced production of NO, indicating the role of KLF4 in mediating inflammation. Overall, these results suggest that KLF4 plays an important role in the inflammatory response of microglial cells to LPS stimulation [73]. In addition, KLF4 has been implicated in the regulation of inflammatory mediators, such as TNF-α and IL-6, which are known to contribute to neuroinflammation [78]. Furthermore, KLF4 has been shown to modulate the expression of genes involved in the inflammatory response.
miR-214-3p is a microRNA that has been implicated in various human diseases, including PD [79]. Zhou and colleagues demonstrated that in models of PD, the expression of SNHG14 was increased, while the expression of miR-214-3p was decreased. The knockdown of SNHG14 alleviated MPP+-induced damage in SK-N-SH cells by increasing cell viability, reducing cell apoptosis, and suppressing pro-inflammatory cytokine production. In terms of its mechanism, SNHG14 directly binds to and sequesters miR-214-3p, resulting in an increase in the levels of miR-214-3p. Subsequently, miR-214-3p interacts directly with the 3′ untranslated region (3′UTR) of KLF4 and reduces its expression. The silencing of SNHG14 in SK-N-SH cells provides protection against MPP + -induced cytotoxicity by upregulating miR-214-3p and subsequently downregulating KLF4 expression. In this study, the levels of TNF-α, IL-6, and IL-1β were evaluated in MPP+-stimulated SK-N-SH cells. This suggests that SNHG14 may play a role in regulating neuroinflammation by modulating the release of TNF-α and IL-6 2. The findings support the potential therapeutic targeting of SNHG14 in PD to alleviate neuroinflammation [80].
BIG1, also known as Brefeldin A-inhibited guanine nucleotide-exchange factor 1 (ARFGEF1), is a protein involved in cellular processes such as cell migration, neurite outgrowth, and regulation of inflammatory cytokines [81, 82]. You et al. showed that BIG1 plays a role in LPS-mediated neuroinflammation and migration in BV2 cells. The inhibition of BIG1 resulted in a decrease in the levels of pro-inflammatory cytokines (such as TNF-a, IL-1b, IL-6) and an increase in the levels of the anti-inflammatory cytokine IL-10. BIG1 knockdown also inhibited the production of NO and the expression of iNOS and COX-2. Furthermore, BIG1 knockdown suppressed cell migration in the presence of LPS. On the other hand, overexpression of BIG1 showed the opposite effects, promoting neuroinflammation and cell migration. Mechanistically, it was found that BIG1 regulated the PI3K/Akt/NF-kB signaling pathway, and the activation of this pathway reversed the protective effects of BIG1 knockdown. Furthermore, the research revealed that KLF4 played a role in the transcriptional regulation of BIG1 and that the overexpression of BIG1 reversed the effects of KLF4 knockdown in terms of neuroinflammation and migration. In summary, the potential therapeutic implications of targeting BIG1 in neurodegenerative diseases, specifically those associated with neuroinflammation like PD, include the reduction of pro-inflammatory cytokine production, inhibition of cell migration, and modulation of the PI3K/Akt/NF-κB signaling pathway. However, more research is required to fully comprehend the effectiveness of targeting BIG1 as a therapeutic strategy in these diseases [83].
Role of KLF4 in Oxidative Stress
Oxidative stress is a crucial factor in the development of PD [24]. Oxidative stress is a condition characterized by an unequal balance between the generation of ROS and the capacity of the body’s antioxidant defense mechanisms to counteract them [84]. It contributes to the degeneration of dopaminergic neurons through various mechanisms, including mitochondrial dysfunction, neuroinflammation, and the oxidation of dopamine [85].
In PD, increased levels of ROS and oxidative stress can lead to damage to mitochondrial lipids, proteins, and DNA, impairing mitochondrial function and leading to cell and tissue damage [85]. Studies have also shown that genetic mutations associated with PD, such as those in the Parkin, PINK1, DJ-1, SNCA, LRRK2, and GBA genes, result in mitochondrial dysfunction and increased oxidative stress [86,87,88]. Moreover, various animal models of PD, including those induced by neurotoxins and genetic modifications, have provided evidence for the role of oxidative stress in the initiation and advancement of the disease [89].
SOD1 is an important enzyme that plays a critical role in protecting against oxidative stress [90]. It is the most important enzyme in various tissues, including neuronal cells, and helps to prevent cell damage and apoptosis [91]. In their study, Chen et al. discovered that the presence of the transcription factor KLF4 contributes to the neurotoxicity caused by MPP + . They observed that the expression of KLF4 increased over time and with higher doses of MPP + in M17 cells. Moreover, when KLF4 was overexpressed, it intensified the neurotoxic effects of MPP + , resulting in heightened vulnerability of the cells and increased oxidative stress. In contrast, inhibiting the expression of KLF4 reduced the harmful effects of MPP + . The study also demonstrated that the suppression of SOD1 by KLF4 played a crucial role in the development of oxidative stress and neurotoxicity caused by MPP + . Overexpression of KLF4 resulted in reduced SOD1 expression, while knockdown of KLF4 increased SOD1 expression. Additionally, KLF4 overexpression promotes cell vulnerability and LDH release, indicating increased oxidative damage [92]. These findings suggest that KLF4 may be a potential therapeutic target for the treatment of PD.
Aprepitant is a selective NK1 receptor antagonist that has shown potential therapeutic effects in various neurological diseases, including PD [93, 94]. The NK1 is a G-protein coupled receptor that is involved in various physiological and pathological processes. It is primarily activated by the substance P (SP), a neuropeptide that plays a role in neuroinflammation and neurodegenerative disorders [95, 96]. ERK5 is a member of the mitogen-activated protein kinase (MAPK) family [97]. It is involved in essential cellular functions such as cell growth, differentiation, and survival [98]. El-Deeb et al. showed that treatment with aprepitant had a neuroprotective effect in a rotenone-induced PD model. aprepitant improved motor function and reduced behavioral and motor disturbances in the rats. It also decreased striatal and substantia nigra neuronal cell death and preserved tyrosine hydroxylase (TH) immunoreactivity, which is indicative of dopaminergic neuron viability. Histopathological examination revealed that aprepitant treatment resulted in a higher count of intact neurons and milder glial cell infiltrates compared to the rotenone group. Immunohistochemical examination showed that aprepitant increased TH immunoreactivity and the count of TH-positive neurons in the substantia nigra region. Furthermore, aprepitant modulated the ERK5/KLF4 signaling pathway. It increased the levels of phosphorylated ERK5 (pERK5) and KLF4. These effects were associated with improvements in oxidative stress markers, such as increased reduced GSH levels and decreased MDA levels. In summary, KLF4 plays a role in regulating oxidative stress through the induction of antioxidant enzymes. Aprepitant, through the activation of ERK5/KLF4 signaling, can modulate oxidative stress and autophagy, leading to neuroprotective effects in PD models [38].
Role of KLF4 in Apoptosis
Apoptosis, which refers to the process of programmed cell death, has a significant impact on PD [99]. Apoptotic cell death of DArgic (DA) neurons is a key feature of PD [99]. The selective loss of these neurons leads to the motor symptoms associated with the disease [99]. Various factors, such as mitochondrial dysfunction, oxidative stress, and protein misfolding, contribute to the activation of apoptotic pathways in DA neurons [100, 101]. Autoimmune cells, such as T cells and B cells, have been suggested to play a role in the development of PD [102]. These cells can recognize α-synuclein, a protein associated with PD, and promote neuroinflammation, leading to the apoptosis of DA neurons [102]. Apoptosis in PD involves the activation of initiator caspases, such as caspase-9 and caspase-8 [103]. Caspase-9 is responsible for initiating the intrinsic pathway, which is also referred to as the mitochondria-mediated pathway. On the other hand, caspase-8 is involved in the activation of the extrinsic apoptotic pathway, which is receptor-mediated [104]. Both pathways ultimately lead to the activation of executioner caspases, such as caspase-3 and caspase-6 [104]. Activation of caspase-3 and caspase-6, which are responsible for executing the process of cell death, results in the characteristic changes observed in apoptosis, such as the cleavage and fragmentation of DNA. This fragmentation of DNA plays a role in the degeneration of dopaminergic neurons in PD [104].
NEAT1 is a long non-coding RNA (lncRNA) that has been implicated in various cellular processes and diseases such as PD [105, 106]. Liu et al. reported that in the MPTP-treated mice, the number of TH+ cells (dopaminergic neurons) in the midbrain was significantly reduced compared to the control group. In the midbrain of mice with PD, the levels of NEAT1 and KLF4 were found to be elevated. This was accompanied by an increase in apoptosis-related proteins, including cleaved-caspase-3 and Bax, and a decrease in the expression of the anti-apoptotic protein Bcl-2. Similarly, in SH-SY5Y cells treated with the neurotoxin MPP + , the expression levels of NEAT1 and KLF4 were also increased in a dose-dependent manner. Similarly, the levels of apoptosis-related proteins were also altered in a dose-dependent manner. Knockdown of NEAT1 in MPP + -treated SH-SY5Y cells resulted in increased cell viability and decreased apoptosis. Moreover, the researchers discovered that KLF4 is a direct target of miR-124, and miR-124 has the ability to bind specifically to NEAT1. When KLF4 expression is increased, it counteracts the impact of NEAT1 knockdown on cell viability and apoptosis in SH-SY5Y cells treated with MPP + . In conclusion, this study proposes that NEAT1 could potentially facilitate apoptosis induced by MPTP/MPP + in PD by regulating the miR-124/KLF4 axis. Reducing the expression of NEAT1 improved cell survival and inhibited apoptosis, suggesting a possible therapeutic approach for PD [107].
miR-212 is a microRNA that has been shown to play a protective role in various neurological disorders, including PD [108]. Song et al. demonstrated that miR-212 exerts a neuroprotective effect against neuronal damage induced by PD. Their study revealed that miR-212 expression was reduced in SH-SY5Y cells treated with MPP + , which is commonly used as an in vitro model of PD. However, when miR-212 was overexpressed, it mitigated the detrimental effects of MPP + on SH-SY5Y cells. The experiment demonstrated that there was an increase in cell survival, a decrease in caspase-3 activity, LDH release, ROS production, TNF-α and IL-1β expression, as well as elevated SOD levels. The research also showed that miR-212 directly targets KLF4 and suppresses its expression. When KLF4 expression was restored in MPP + -induced SH-SY5Y cells, it reversed the protective effects of miR-212. Furthermore, it was discovered that the Notch signaling pathway plays a role in controlling the miR-212/KLF4 axis in MPP + -induced SH-SY5Y cells. To summarize, miR-212 reduces neuronal damage caused by MPP + in SH-SY5Y cells by targeting KLF4 and modulating the Notch signaling pathway [109]. These results indicate that targeting miR-212 could be a promising approach for treating PD.
MicroRNA-7 (miR-7) is a small RNA molecule that does not code for proteins and has been implicated in several biological processes, such as cell transformation, brain metastasis, growth regulation, and cancer progression [110, 111]. Kong et al. indicated that miR-7 plays a protective role in PD by preventing cell apoptosis. They used a human neuroblastoma cell line (SH-SY5Y) and treated it with MPP+, which is known to induce cell death in PD. The study demonstrated that when miR-7 levels were increased in SH-SY5Y cells, it resulted in enhanced cell viability and reduced cell apoptosis when exposed to MPP + treatment. Additionally, the research revealed that miR-7 directly targets KLF4. When KLF4 expression was reduced, it inhibited cell apoptosis, whereas overexpression of KLF4 negated the protective effect of miR-7 [112]. The results indicate that miR-7 provides protection against cell apoptosis caused by MPP + through its targeting of KLF4. Furthermore, KLF4, one of the Yamanaka transcription factors, has shown clinical relevance in PD [113]. While the clinical relevance of KLF4 in PD is promising, there are still limitations and challenges that need to be addressed. The long-term survival, functionality, and efficacy of the transplanted cells are still unknown [113].
Overall, KLF4 is a versatile transcription factor that plays important roles in various diseases. Its functions and effects can vary depending on the specific disease context and cellular environment. More investigation is required to gain a comprehensive understanding of the mechanisms involved in the functions of KLF4 and its potential as a target for therapeutic interventions in clinical settings.
Conclusion
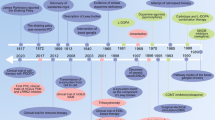
KLF4, as a transcription factor, regulates various cellular activities like cell growth, proliferation, and differentiation. Recently, concerns have arisen regarding the potential contribution of KLF4 to PD pathophysiology. Although the etiology of the disease is still obscure, the deregulation of the signaling pathways involved in cell survival and death, mitochondrial dysfunction, autophagy, oxidative stress, iron accumulation, and neuroinflammation are regarded to be involved in PD. In this review, we have collected relevant data. We discussed the modulating role of KLF4 on aberrant α-synuclein clearance, neuroinflammation, neuronal death, oxidative stress, and iron accumulation to elucidate the potential implication of KLF4 in PD pathogenesis. These findings support the idea that targeting KLF4 represents a prospective therapeutic strategy for PD also against deteriorated dopaminergic transmission in the brain (Fig. 2). However, limitations related to a low number of available data should be acknowledged. Given the context-dependent functions of KLF4, there is a gap in the knowledge of its role in PD pathogenesis. Thus, extensive research is required to understand the translational value of the KLF4-oriented therapeutic approach in PD.
Potential KLF4-based strategies for treating PD. A KLF4 knockdown diminished cell death in MPP+-treated SH-SY5Y cells, while apoptosis was accelerated by overexpression KLF4. B In the KLF4-HCP1 signaling pathway, KLF4-mediated glucocorticoid-induces increases in the expression of HCP1, which causes iron accumulation. C Upregulation of KLF4 notably subsided the preservative impact of miR-7 on MPP+-induced apoptosis in SH-SY5Y cells. D KLF4 mRNA was induced by L-DOPA. E Upregulation of KLF4 increased the neurotoxicity of MPP+ in the form of rising cell vulnerability and oxidative stress. F miR-212-mediated protection impacts were abated after KLF4 expression restoration in MPP+-induced SH-SY5Y cells, represented as lessened cell viability and increased cell death. G NEAT1 knockdown can prevent MPTP-induced autophagy in vivo which lessens dopaminergic neuronal damage in a mouse model, and NEAT1 knockdown prevented the advent of PD by downregulating KLF4 in SH-SY5Y cells. HCP1, Heme Carrier Protein 1; MPP+, 1-methyl-4-phenylpyridinium; miR, miRNA; NEAT1, nuclear paraspeckle assembly transcript 1; KLF4, Krüppel-like factor 4
Data Availability
The literature analyzed during the current study is available at locations cited in the reference section.
Abbreviations
- CNS:
-
Central nervous system
- STAT3:
-
Signal transducer and activator of transcription 3
- Nrf2:
-
Nuclear factor erythrocyte-associated factor 2
- Trx 1:
-
Thioredoxin-1
- iPSCs:
-
Induced pluripotent stem cells
- MPTP:
-
1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine
- MPP + :
-
1-Methyl-4-phenylpyridinium
- 6-OHDA:
-
6-Hydroxydopamine
- Sp/Klf:
-
Specificity protein/Krüppel-like factor
- Aβ42:
-
Amyloid β 42
- BV2 cells:
-
A unique type of microglial cells derived from C57/BL6 murine
- EAE:
-
Experimental autoimmune encephalomyelitis
- MS:
-
Multiple sclerosis
- IL-1β:
-
Interleukin-1β
- iNOS:
-
Inducible nitric oxide synthase
- PI3K/AKT pathway:
-
Phosphatidylinositol-3-kinase/protein kinase B pathway
- MCP-1:
-
Monocyte chemoattractant protein-1
- Cox-2:
-
Cyclooxygenase-2
- NO:
-
Nitric oxide
- SNHG14:
-
Small nucleolar RNA host gene 14
- NF-kB:
-
Nuclear factor kappa B
- ROS:
-
Reactive oxygen species
- PINK1:
-
PTEN-induced putative kinase 1
- SNCA:
-
Synuclein Alpha
- LRRK2:
-
Leucine-rich repeat kinase 2
- GBA:
-
Glucocerebrosidase
- SOD1:
-
Superoxide dismutase 1
- LDH:
-
Lactate dehydrogenase
- NK1 receptor:
-
Neurokinin-1 receptor
- ERK5:
-
Extracellular signal-regulated kinase 5
- GSH:
-
Glutathione
- MDA:
-
Malondialdehyde
- NEAT1:
-
Nuclear-enriched abundant transcript 1
- Bcl2:
-
B-cell lymphoma 2
- Bax:
-
Bcl-2-associated X protein
References
Shields JM, Christy RJ, Yang VW (1996) Identification and characterization of a gene encoding a gut-enriched Krüppel-like factor expressed during growth arrest. J Biol Chem 271(33):20009–20017
Xiang F et al (2021) 3, 3’-Diindolylmethane enhances paclitaxel sensitivity by suppressing DNMT1-mediated KLF4 methylation in breast cancer. Front Oncol 11:627856
Zheng H et al (2009) gene expression is inhibited by the notch signaling pathway that controls goblet cell differentiation in mouse gastrointestinal tract. Am J Physiol-Gastrointest Liver Physiol 296(3):G490–G498
Luo D-D, Zhao F (2022) KLF4 suppresses the proliferation and metastasis of NSCLC cells via inhibition of MSI2 and regulation of the JAK/STAT3 signaling pathway. Transl Oncol 22:101396
Morales-Martinez M et al (2020) MicroRNA-7 regulates migration and chemoresistance in non-Hodgkin lymphoma cells through regulation of KLF4 and YY1. Front Oncol 10:588893
Ghaleb AM et al (2005) Krüppel-like factors 4 and 5: the yin and yang regulators of cellular proliferation. Cell Res 15(2):92–96
Rowland BD, Peeper DS (2006) KLF4, p21 and context-dependent opposing forces in cancer. Nat Rev Cancer 6(1):11–23
Kaushik DK et al (2010) Krüppel-like factor 4, a novel transcription factor regulates microglial activation and subsequent neuroinflammation. J Neuroinflammation 7(1):1–20
Mamonkin M et al (2013) Differential roles of KLF4 in the development and differentiation of CD8+ T cells. Immunol Lett 156(1–2):94–101
Miao X, Wu X, Shi W (2017) MicroRNA-346 regulates neural stem cell proliferation and differentiation by targeting KLF4. Am J Transl Res 9(12):5400
Qin S, Zhang C-L (2012) Role of Krüppel-like factor 4 in neurogenesis and radial neuronal migration in the developing cerebral cortex. Mol Cell Biol 32(21):4297–4305
Fan Y et al (2017) Krüppel-like factors and vascular wall homeostasis. J Mol Cell Biol 9(5):352–363
Qin S et al (2011) Dysregulation of Kruppel-like factor 4 during brain development leads to hydrocephalus in mice. Proc Natl Acad Sci 108(52):21117–21121
Burgos K et al (2014) Profiles of extracellular miRNA in cerebrospinal fluid and serum from patients with Alzheimer’s and Parkinson’s diseases correlate with disease status and features of pathology. PLoS ONE 9(5):e94839
Huang T et al (2023) Protective effects of KLF4 on blood-brain barrier and oxidative stress after cerebral ischemia-reperfusion in rats through the Nrf2/Trx1 pathway. Cytokine 169:156288
Cheng Z et al (2018) The role of KLF(4) in Alzheimer’s disease. Front Cell Neurosci 12:325
Cheng Z et al (2018) The role of KLF4 in Alzheimer’s disease. Front Cell Neurosci 12:325
Li L et al (2017) Krüppel-like factor 4 regulates amyloid-β (Aβ)-induced neuroinflammation in Alzheimer’s disease. Neurosci Lett 643:131–137
Hyeon JW, Kim AH, Yano H (2021) Epigenetic regulation in Huntington’s disease. Neurochem Int 148:105074
Chiu F-L et al (2015) Elucidating the role of the A2A adenosine receptor in neurodegeneration using neurons derived from Huntington’s disease iPSCs. Hum Mol Genet 24(21):6066–6079
Jeon I et al (2012) Neuronal properties, in vivo effects, and pathology of a Huntington’s disease patient-derived induced pluripotent stem cells. Stem cells 30(9):2054–2062
Im W et al (2009) Stem cells transplantation and Huntington’s disease. Int J Stem Cells 2(2):102–108
Zaman V et al (2021) Cellular and molecular pathophysiology in the progression of Parkinson’s disease. Metab Brain Dis 36:815–827
Zamanian MY et al (2023) Neuroprotective and anti-inflammatory effects of pioglitazone on Parkinson’s disease: a comprehensive narrative review of clinical and experimental findings. CNS Neurol Disord Drug Targets 22(10):1453–1461
Bonner N et al (2020) Patients’ experiences of Parkinson’s disease: a qualitative study in glucocerebrosidase and idiopathic Parkinson’s disease. J Patient-Rep Outcomes 4:1–14
Hsieh L-F et al (2022) Ultrasonographic imaging findings of the shoulder in patients with Parkinson disease. J Orthop Sci 28(5):1004–1010
Oliveira LMA et al (2021) Alpha-synuclein research: defining strategic moves in the battle against Parkinson’s disease. npj Parkinson’s Dis 7(1):65–73
Kujawska M, Jodynis-Liebert J (2018) What is the evidence that Parkinson’s disease is a prion disorder, which originates in the gut? Int J Mol Sci 19(11):3573–3584
Kujawska M, Domanskyi A, Kreiner G (2021) Editorial: Common Pathways linking neurodegenerative diseases—the role of inflammation. Front Cell Neurosci 15:754051
Jayaraj RL et al (2022) Effect of citronellol on oxidative stress, neuroinflammation and autophagy pathways in an in vivo model of Parkinson’s disease. Heliyon 8(11):e11434
Sayed AS et al (2022) Xanthotoxin modulates oxidative stress, inflammation, and MAPK signaling in a rotenone-induced Parkinson’s disease model. Life Sci 310:121129
Qu L et al (2022) Lysosomal K+ channel TMEM175 promotes apoptosis and aggravates symptoms of Parkinson’s disease. EMBO Rep 23(9):e53234
Leathem A et al (2022) Evidence for oxidative pathways in the pathogenesis of PD: are antioxidants candidate drugs to ameliorate disease progression? Int J Mol Sci 23(13):6923
Kujawska M, Jodynis-Liebert J (2018) Polyphenols in Parkinson’s disease: a systematic review of in vivo studies. Nutrients 10(5):642
Kong B et al (2016) microRNA-7 protects against 1-Methyl-4-Phenylpyridinium iodide-induced cell apoptosis in SH-SY5Y cells by directly targeting Krupple-like factor 4. DNA Cell Biol 35(5):217–225
Song Y, Liu Y, Chen X (2018) MiR-212 Attenuates MPP(+)-induced neuronal damage by targeting KLF4 in SH-SY5Y cells. Yonsei Med J 59(3):416–424
Chen J et al (2013) Induction of KLF4 contributes to the neurotoxicity of MPP + in M17 cells: a new implication in Parkinson’s disease. J Mol Neurosci 51(1):109–117
El-Deeb AM et al (2023) Novel trajectories of the NK1R antagonist aprepitant in rotenone-induced Parkinsonism-like symptoms in rats: involvement of ERK5/KLF4/p62/Nrf2 signaling axis. Chem Biol Interact 380:110562
Zhang W et al (1998) The gut-enriched Krüppel-like factor suppresses the activity of the CYP1A1 promoter in an Sp1-dependent fashion. J Biol Chem 273(28):17917–17925
Shields JM, Yang VW (1998) Identification of the DNA sequence that interacts with the gut-enriched Krüppel-like factor. Nucleic Acids Res 26(3):796–802
Nandan MO, Yang VW (2009) The role of Krüppel-like factors in the reprogramming of somatic cells to induced pluripotent stem cells. Histol Histopathol 24(10):1343
Takahashi K, Yamanaka S (2006) Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126(4):663–676
Yet S-F et al (1998) Human EZF, a Krüppel-like zinc finger protein, is expressed in vascular endothelial cells and contains transcriptional activation and repression domains. J Biol Chem 273(2):1026–1031
Jenkins TD et al (1998) Transactivation of the human keratin 4 and Epstein-Barr virus ED-L2 promoters by gut-enriched Krüppel-like factor. J Biol Chem 273(17):10747–10754
Shie J-L et al (2000) Role of gut-enriched Kruppel-like factor in colonic cell growth and differentiation. Am J Physiol-Gastrointest Liver Physiol 279(4):G806–G814
Garrett-Sinha LA et al (1996) A gene for a novel zinc-finger protein expressed in differentiated epithelial cells and transiently in certain mesenchymal cells. J Biol Chem 271(49):31384–31390
Pearson R et al (2008) Krüppel-like transcription factors: a functional family. Int J Biochem Cell Biol 40(10):1996–2001
Wei D et al (2005) Emerging role of KLF4 in human gastrointestinal cancer. Carcinogenesis 27(1):23–31
Hu D et al (2015) Interplay between arginine methylation and ubiquitylation regulates KLF4-mediated genome stability and carcinogenesis. Nat Commun 6(1):8419
Evans PM, Liu C (2008) Roles of Krüppel-like factor 4 in normal homeostasis, cancer and stem cells. Acta Biochim Biophys Sin 40(7):554–564
Ghaleb A et al (2007) Krüppel-like factor 4 exhibits antiapoptotic activity following γ-radiation-induced DNA damage. Oncogene 26(16):2365–2373
Chen ZY et al (2005) Destabilization of Kruppel-like factor 4 protein in response to serum stimulation involves the ubiquitin-proteasome pathway. Can Res 65(22):10394–10400
Gamper AM et al (2012) Regulation of KLF4 turnover reveals an unexpected tissue-specific role of pVHL in tumorigenesis. Mol Cell 45(2):233–243
Pérez-Monter C et al (2011) The Krüppel-like factor 4 controls biosynthesis of thyrotropin-releasing hormone during hypothalamus development. Mol Cell Endocrinol 333(2):127–133
Li H et al (2017) Physiological stress-induced corticosterone increases heme uptake via KLF4-HCP1 signaling pathway in hippocampus neurons. Sci Rep 7(1):1–10
Cui DM et al (2017) KLF 4 Knockdown attenuates TBI-induced neuronal damage through p53 and JAK-STAT 3 signaling. CNS Neurosci Ther 23(2):106–118
Ahn M et al (2015) Immunohistochemical study of Krüppel-like factor 4 in the spinal cords of rats with experimental autoimmune encephalomyelitis. Acta Histochem 117(6):521–527
Zare-Chahoki A et al (2021) Inflammation in an animal model of multiple sclerosis leads to MicroRNA-25–3p dysregulation associated with inhibition of Pten and Klf4. Iran J Aller, Asthma Immunol 326(5950):298–301
Moore DL et al (2009) KLF family members regulate intrinsic axon regeneration ability. Science 326(5950):298–301
Wang Q, Liu Y, Zhou J (2015) Neuroinflammation in Parkinson’s disease and its potential as therapeutic target. Transl Neurodegen 4:1–9
Hirsch EC, Standaert DG (2021) Ten unsolved questions about neuroinflammation in Parkinson’s disease. Mov Disord 36(1):16–24
Song GJ, Suk K (2017) Pharmacological modulation of functional phenotypes of microglia in neurodegenerative diseases. Front Aging Neurosci 9:139
Kao Y-C et al (2019) High fat diet suppresses peroxisome proliferator-activated receptors and reduces dopaminergic neurons in the substantia nigra. Int J Mol Sci 21(1):207
Zhang B et al (2019) Targeting MAPK pathways by naringenin modulates microglia M1/M2 polarization in lipopolysaccharide-stimulated cultures. Front Cell Neurosci 12:531
Xu N et al (2017) Spared nerve injury increases the expression of microglia M1 markers in the prefrontal cortex of rats and provokes depression-like behaviors. Front Neurosci 11:209
Therajaran P et al (2020) Microglial polarization in posttraumatic epilepsy: potential mechanism and treatment opportunity. Epilepsia 61(2):203–215
Clausen B et al (1999) Conditional gene targeting in macrophages and granulocytes using LysMcre mice. Transgenic Res 8:265–277
Sahu SK et al (2017) MicroRNA 26a (miR-26a)/KLF4 and CREB-C/EBPβ regulate innate immune signaling, the polarization of macrophages and the trafficking of Mycobacterium tuberculosis to lysosomes during infection. PLoS Pathog 13(5):e1006410
Vergadi E et al (2017) Akt signaling pathway in macrophage activation and M1/M2 polarization. J Immunol 198(3):1006–1014
Dong X et al (2019) MicroRNA-9-5p downregulates Klf4 and influences the progression of hepatocellular carcinoma via the AKT signaling pathway. Int J Mol Med 43(3):1417–1429
Lv S et al (2018) Histone methyltransferase KMT2D sustains prostate carcinogenesis and metastasis via epigenetically activating LIFR and KLF4. Oncogene 37(10):1354–1368
El-Deeb NK et al (2022) Crosstalk between PI3K/AKT/KLF4 signaling and microglia M1/M2 polarization as a novel mechanistic approach towards flibanserin repositioning in Parkinson’s disease. Int Immunopharmacol 112:109191
Kaushik DK et al (2010) Krüppel-like factor 4, a novel transcription factor regulates microglial activation and subsequent neuroinflammation. J Neuroinflammation 7:1–20
Hamik A et al (2007) Kruppel-like factor 4 regulates endothelial inflammation. J Biol Chem 282(18):13769–13779
Shen B et al (2009) Kruppel-like factor 4 is a novel mediator of Kallistatin in inhibiting endothelial inflammation via increased endothelial nitric-oxide synthase expression. J Biol Chem 284(51):35471–35478
Alder JK et al (2008) Kruppel-like factor 4 is essential for inflammatory monocyte differentiation in vivo. J Immunol 180(8):5645–5652
Feinberg MW et al (2005) Kruppel-like factor 4 is a mediator of proinflammatory signaling in macrophages. J Biol Chem 280(46):38247–38258
Wang C et al (2016) Correlation of A2bAR and KLF4/KLF15 with obesity-dyslipidemia induced inflammation in Uygur population. Mediators Inflamm 21:56–67
Li L et al (2022) Long noncoding RNA BACE1-antisense transcript plays a critical role in Parkinson’s disease via microRNA-214-3p/Cell death-inducing p53-target protein 1 axis. Bioengineered 13(4):10889–10901
Zhou S et al (2020) Knockdown of SNHG14 alleviates MPP+-induced injury in the cell model of Parkinson’s disease by targeting the miR-214-3p/KLF4 axis. Front Neurosci 14:930
Hong S et al (2019) Brefeldin A–sensitive ER-Golgi vesicle trafficking contributes to NLRP3-dependent caspase-1 activation. FASEB J 33(3):4547–4558
Padilla PI et al (2004) Nuclear localization and molecular partners of BIG1, a brefeldin A-inhibited guanine nucleotide-exchange protein for ADP-ribosylation factors. Proc Natl Acad Sci 101(9):2752–2757
You Z et al (2022) The novel KLF4/BIG1 regulates LPS-mediated neuro-inflammation and migration in BV2 cells via PI3K/Akt/NF-kB signaling pathway. Neuroscience 488:102–111
Zamanian M et al (2017) Short-term effects of troxerutin (vitamin P4) on muscle fatigue and gene expression of Bcl-2 and Bax in the hepatic tissue of rats. Can J Physiol Pharmacol 95(6):708–713
Zamanian MY et al (2023) Targeting Nrf2 signaling pathway and oxidative stress by resveratrol for Parkinson’s disease: an overview and update on new developments. Mol Biol Rep 50(6):5455–5464
Trinh J, Farrer M (2013) Advances in the genetics of Parkinson disease. Nat Rev Neurol 9(8):445–454
Hernandez DG, Reed X, Singleton AB (2016) Genetics in Parkinson disease: Mendelian versus non-Mendelian inheritance. J Neurochem 139:59–74
Bozi M et al (2014) Genetic assessment of familial and early-onset Parkinson’s disease in a Greek population. Eur J Neurol 21(7):963–968
Hauser DN, Hastings TG (2013) Mitochondrial dysfunction and oxidative stress in Parkinson’s disease and monogenic parkinsonism. Neurobiol Dis 51:35–42
Fukui M, Zhu BT (2010) Mitochondrial superoxide dismutase SOD2, but not cytosolic SOD1, plays a critical role in protection against glutamate-induced oxidative stress and cell death in HT22 neuronal cells. Free Radical Biol Med 48(6):821–830
Zhang C et al (2019) γ-Oryzanol mitigates oxidative stress and prevents mutant SOD1-related neurotoxicity in Drosophila and cell models of amyotrophic lateral sclerosis. Neuropharmacology 160:107777
Chen J et al (2013) Induction of KLF4 contributes to the neurotoxicity of MPP+ in M17 cells: a new implication in Parkinson’s disease. J Mol Neurosci 51(1):109–117
Robinson P, Coveñas R, Muñoz M (2023) Combination therapy of chemotherapy or radiotherapy and the neurokinin-1 receptor antagonist aprepitant: a new antitumor strategy? Curr Med Chem 30(16):1798–1812
Martinez AN, Philipp MT (2016) Substance P and antagonists of the neurokinin-1 receptor in neuroinflammation associated with infectious and neurodegenerative diseases of the central nervous system. J Neurol Neuromed 1(2):29
Thornton E, Vink R (2015) Substance P and its tachykinin NK1 receptor: a novel neuroprotective target for Parkinson’s disease. Neural Regen Res 10(9):1403
Thornton E et al (2014) The NK1 receptor antagonist N-acetyl-L-tryptophan reduces dyskinesia in a hemi-parkinsonian rodent model. Parkinsonism Relat Disord 20(5):508–513
Yoshizumi M et al (2012) The role of big mitogen-activated protein kinase 1 (BMK1)/extracellular signal-regulated kinase 5 (ERK5) in the pathogenesis and progression of atherosclerosis. J Pharmacol Sci 120(4):259–263
Drew BA, Burow ME, Beckman BS (2012) MEK5/ERK5 pathway: the first fifteen years. Biochim Biophys Acta (BBA)-Rev Cancer 1825(1):37–48
See WZC, Naidu R, Tang KS (2022) Cellular and molecular events leading to paraquat-induced apoptosis: mechanistic insights into Parkinson’s disease pathophysiology. Mol Neurobiol 59(6):3353–3369
Zhu JH et al (2003) Localization of phosphorylated ERK/MAP kinases to mitochondria and autophagosomes in Lewy body diseases. Brain Pathol 13(4):473–481
Wood-Kaczmar A et al (2008) PINK1 is necessary for long term survival and mitochondrial function in human dopaminergic neurons. PLoS ONE 3(6):e2455
Zheng Z et al (2022) Mechanisms of autoimmune cell in DA neuron apoptosis of Parkinson’s disease: recent advancement. Oxid Med Cell Long 3(6):e2455
Viswanath V et al (2001) Caspase-9 activation results in downstream caspase-8 activation and bid cleavage in 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine-induced Parkinson’s disease. J Neurosci 21(24):9519–9528
Erekat NS (2018) Apoptosis and its ROLE in Parkinson’s disease. Exon Publications 21(24):9519–9528
Yan W et al (2018) LncRNA NEAT1 promotes autophagy in MPTP-induced Parkinson’s disease through stabilizing PINK1 protein. Biochem Biophys Res Commun 496(4):1019–1024
Li K, Wang Z (2023) lncRNA NEAT1: key player in neurodegenerative diseases. Ageing Res Rev 86:101878
Liu J et al (2020) Long non-coding RNA NEAT1 mediates MPTP/MPP+-induced apoptosis via regulating the miR-124/KLF4 axis in Parkinson’s disease. Open Life Sci 15(1):665–676
Hadar A et al (2018) SIRT1, miR-132 and miR-212 link human longevity to Alzheimer’s disease. Sci Rep 8(1):8465
Song Y, Liu Y, Chen X (2018) MiR-212 attenuates MPP+-induced neuronal damage by targeting KLF4 in SH-SY5Y cells. Yonsei Med J 59(3):416–424
Zhao J et al (2015) MicroRNA-7: a promising new target in cancer therapy. Cancer Cell Int 15(1):1–8
Kalinowski FC et al (2014) microRNA-7: a tumor suppressor miRNA with therapeutic potential. Int J Biochem Cell Biol 54:312–317
Kong B et al (2016) microRNA-7 protects against 1-methyl-4-phenylpyridinium iodide-induced cell apoptosis in SH-SY5Y cells by directly targeting Krüpple-like factor 4. DNA Cell Biol 35(5):217–225
Aguirre M et al (2023) Application of the Yamanaka transcription factors Oct4, Sox2, Klf4, and c-Myc from the laboratory to the clinic. Genes 14(9):1697
Acknowledgements
The figure was created with BioRender.com.
Author information
Authors and Affiliations
Contributions
M.Y.Z, M.G, and M.K: conception, design, writing, revising, and approval of the manuscript. R.A, G.S.B, A.S, and R.M.R.P: data collection, manuscript drafting, and table creation. R.Z, T.O, and A.J: drafting, editing of the manuscript, and graphic drawing. All authors have read and agreed to the submitted version of the manuscript.
Corresponding authors
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zamanian, M.Y., Golmohammadi, M., Amin, R.S. et al. Therapeutic Targeting of Krüppel-Like Factor 4 and Its Pharmacological Potential in Parkinson’s Disease: a Comprehensive Review. Mol Neurobiol 61, 3596–3606 (2024). https://doi.org/10.1007/s12035-023-03800-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03800-2