Abstract
Patients with traumatic brain injury (TBI) frequently require invasive mechanical ventilation and admission to an intensive care unit. Ventilation of patients with TBI poses unique clinical challenges, and careful attention is required to ensure that the ventilatory strategy (including selection of appropriate tidal volume, plateau pressure, and positive end-expiratory pressure) does not cause significant additional injury to the brain and lungs. Selection of ventilatory targets may be guided by principles of lung protection but with careful attention to relevant intracranial effects. In patients with TBI and concomitant acute respiratory distress syndrome (ARDS), adjunctive strategies include sedation optimization, neuromuscular blockade, recruitment maneuvers, prone positioning, and extracorporeal life support. However, these approaches have been largely extrapolated from studies in patients with ARDS and without brain injury, with limited data in patients with TBI. This narrative review will summarize the existing evidence for mechanical ventilation in patients with TBI. Relevant literature in patients with ARDS will be summarized, and where available, direct data in the TBI population will be reviewed. Next, practical strategies to optimize the delivery of mechanical ventilation and determine readiness for extubation will be reviewed. Finally, future directions for research in this evolving clinical domain will be presented, with considerations for the design of studies to address relevant knowledge gaps.

Similar content being viewed by others
References
Burns KEA, Rizvi L, Cook DJ, et al. Ventilator weaning and discontinuation practices for critically Ill patients. JAMA. 2021;325(12):1173–84. https://doi.org/10.1001/jama.2021.2384 (In English).
Asehnoune K, Roquilly A, Cinotti R. Respiratory management in patients with severe brain injury. Crit Care. 2018;22(1):76. https://doi.org/10.1186/s13054-018-1994-0 (In English).
Nyquist P, Stevens RD, Mirski MA. Neurologic injury and mechanical ventilation. Neurocrit Care. 2008;9(3):400–8. https://doi.org/10.1007/s12028-008-9130-7 (In English).
Stevens RD, Lazaridis C, Chalela JA. The role of mechanical ventilation in acute brain injury. Neurol Clin. 2008;26(2):543–63. https://doi.org/10.1016/j.ncl.2008.03.014.
Maramattom BV, Weigand S, Reinalda M, Wijdicks EF, Manno EM. Pulmonary complications after intracerebral hemorrhage. Neurocrit Care. 2006;5(2):115–9. https://doi.org/10.1385/ncc:5:2:115 (In English).
Fan TH, Huang M, Gedansky A, et al. Prevalence and outcome of acute respiratory distress syndrome in traumatic brain injury: a systematic review and meta-analysis. Lung. 2021;199(6):603–10. https://doi.org/10.1007/s00408-021-00491-1 (In English).
Rincon F, Ghosh S, Dey S, et al. Impact of acute lung injury and acute respiratory distress syndrome after traumatic brain injury in the United States. Neurosurgery. 2012;71(4):795–803. https://doi.org/10.1227/NEU.0b013e3182672ae5 (In English).
Robba C, Poole D, McNett M, et al. Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. 2020;46(12):2397–410. https://doi.org/10.1007/s00134-020-06283-0 (In English).
Piran P, Stevens RD. Lung-protective ventilation and adjunctive strategies to manage respiratory failure: are they safe in the neurological patient? Curr Opin Crit Care. 2021;27(2):115–9. https://doi.org/10.1097/mcc.0000000000000809 (In English).
Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–8. https://doi.org/10.1056/nejm200005043421801 (In English).
Papazian L, Aubron C, Brochard L, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019;9(1):69. https://doi.org/10.1186/s13613-019-0540-9.
Fan E, Del Sorbo L, Goligher EC, et al. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;195(9):1253–63. https://doi.org/10.1164/rccm.201703-0548ST (In English).
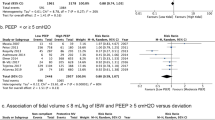
Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865–73. https://doi.org/10.1001/jama.2010.218 (In English).
Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369(5):428–37. https://doi.org/10.1056/NEJMoa1301082 (In English).
Mascia L, Pasero D, Slutsky AS, et al. Effect of a lung protective strategy for organ donors on eligibility and availability of lungs for transplantation: a randomized controlled trial. JAMA. 2010;304(23):2620–7. https://doi.org/10.1001/jama.2010.1796.
Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA. 2012;308(16):1651–9. https://doi.org/10.1001/jama.2012.13730.
Hawryluk GWJ, Aguilera S, Buki A, et al. A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2019;45(12):1783–94. https://doi.org/10.1007/s00134-019-05805-9 (In English).
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury. Neurosurgery. 2017;80(1):6–15. https://doi.org/10.1227/neu.0000000000001432 (In English).
Robba C, Ball L, Nogas S, et al. Effects of positive end-expiratory pressure on lung recruitment, respiratory mechanics, and intracranial pressure in mechanically ventilated brain-injured patients. Front Physiol. 2021;12:711273. https://doi.org/10.3389/fphys.2021.711273 (In English).
Cooper KR, Boswell PA, Choi SC. Safe use of PEEP in patients with severe head injury. J Neurosurg. 1985;63(4):552–5. https://doi.org/10.3171/jns.1985.63.4.0552 (In English).
Munshi L, Del Sorbo L, Adhikari NKJ, et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14(Supplemant_4):S280-s288. https://doi.org/10.1513/AnnalsATS.201704-343OT (In English).
Alhazzani W, Belley-Cote E, Møller MH, et al. Neuromuscular blockade in patients with ARDS: a rapid practice guideline. Intensive Care Med. 2020;46(11):1977–86. https://doi.org/10.1007/s00134-020-06227-8 (In English).
Goligher EC, Hodgson CL, Adhikari NKJ, et al. Lung recruitment maneuvers for adult patients with acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc. 2017;14(Supplement_4):S304–11. https://doi.org/10.1513/AnnalsATS.201704-340OT (In English).
Della Torre V, Badenes R, Corradi F, et al. Acute respiratory distress syndrome in traumatic brain injury: how do we manage it? J Thorac Dis. 2017;9(12):5368.
Nekludov M, Bellander BM, Mure M. Oxygenation and cerebral perfusion pressure improved in the prone position. Acta Anaesthesiol Scand. 2006;50(8):932–6. https://doi.org/10.1111/j.1399-6576.2006.01099.x (In English).
Bein T, Kuhr LP, Bele S, Ploner F, Keyl C, Taeger K. Lung recruitment maneuver in patients with cerebral injury: effects on intracranial pressure and cerebral metabolism. Intensive Care Med. 2002;28(5):554–8. https://doi.org/10.1007/s00134-002-1273-y (In English).
Sud S, Friedrich JO, Adhikari NKJ, et al. Comparative effectiveness of protective ventilation strategies for moderate and severe acute respiratory distress syndrome. A network meta-analysis. Am J Respir Crit Care Med. 2021;203(11):1366–77. https://doi.org/10.1164/rccm.202008-3039OC (In English).
Fuller BM, Mohr NM, Drewry AM, Carpenter CR. Lower tidal volume at initiation of mechanical ventilation may reduce progression to acute respiratory distress syndrome: a systematic review. Crit Care. 2013;17(1):R11. https://doi.org/10.1186/cc11936.
Mascia L, Zavala E, Bosma K, et al. High tidal volume is associated with the development of acute lung injury after severe brain injury: an international observational study. Crit Care Med. 2007;35(8):1815–20. https://doi.org/10.1097/01.Ccm.0000275269.77467.Df (In English).
Battisti-Charbonney A, Fisher J, Duffin J. The cerebrovascular response to carbon dioxide in humans. J Physiol. 2011;589(Pt 12):3039–48. https://doi.org/10.1113/jphysiol.2011.206052 (In English).
Smith AL, Neufeld GR, Ominsky AJ, Wollman H. Effect of arterial CO2 tension on cerebral blood flow, mean transit time, and vascular volume. J Appl Physiol. 1971;31(5):701–7. https://doi.org/10.1152/jappl.1971.31.5.701 (In English).
Pelosi P, Ferguson ND, Frutos-Vivar F, et al. Management and outcome of mechanically ventilated neurologic patients. Crit Care Med. 2011;39(6):1482–92. https://doi.org/10.1097/CCM.0b013e31821209a8 (In English).
Picetti E, Pelosi P, Taccone FS, Citerio G, Mancebo J, Robba C. VENTILatOry strategies in patients with severe traumatic brain injury: the VENTILO Survey of the European Society of Intensive Care Medicine (ESICM). Crit Care. 2020;24(1):158. https://doi.org/10.1186/s13054-020-02875-w (In English).
Tejerina EE, Pelosi P, Robba C, et al. Evolution over time of ventilatory management and outcome of patients with neurologic disease. Crit Care Med. 2021;49(7):1095–106. https://doi.org/10.1097/ccm.0000000000004921 (In English).
Ricard JD, Dreyfuss D, Saumon G. Ventilator-induced lung injury. Eur Respir J. 2003;22(42 suppl):2s–9s. https://doi.org/10.1183/09031936.03.00420103.
Beitler JR, Malhotra A, Thompson BT. Ventilator-induced lung injury. Clin Chest Med. 2016;37(4):633–46. https://doi.org/10.1016/j.ccm.2016.07.004 (In English).
Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126–36. https://doi.org/10.1056/NEJMra1208707.
Hager DN, Krishnan JA, Hayden DL, Brower RG. Tidal volume reduction in patients with acute lung injury when plateau pressures are not high. Am J Respir Crit Care Med. 2005;172(10):1241–5. https://doi.org/10.1164/rccm.200501-048CP (In English).
Laffey JG, Bellani G, Pham T, et al. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study. Intensive Care Med. 2016;42(12):1865–76. https://doi.org/10.1007/s00134-016-4571-5.
Amato MBP, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–55. https://doi.org/10.1056/NEJMsa1410639.
Dianti J, Matelski J, Tisminetzky M, et al. Comparing the effects of tidal volume, driving pressure, and mechanical power on mortality in trials of lung-protective mechanical ventilation. Respir Care. 2021;66(2):221–7. https://doi.org/10.4187/respcare.07876 (In English).
Goligher EC, Costa ELV, Yarnell CJ, et al. Effect of lowering VT on mortality in acute respiratory distress syndrome varies with respiratory system elastance. Am J Respir Crit Care Med. 2021;203(11):1378–85. https://doi.org/10.1164/rccm.202009-3536OC (In English).
Thiara S, Griesdale DE, Henderson WR, Sekhon MS. Effect of cerebral perfusion pressure on acute respiratory distress syndrome. Can J Neurol Sci. 2018;45(3):313–9. https://doi.org/10.1017/cjn.2017.292.
Tejerina E, Pelosi P, Muriel A, et al. Association between ventilatory settings and development of acute respiratory distress syndrome in mechanically ventilated patients due to brain injury. J Crit Care. 2017;38:341–5. https://doi.org/10.1016/j.jcrc.2016.11.010 (In English).
Gattinoni L, Collino F, Maiolo G, et al. Positive end-expiratory pressure: how to set it at the individual level. Ann Transl Med. 2017;5(14):288. https://doi.org/10.21037/atm.2017.06.64 (In English).
Rezoagli E, Bellani G. How I set up positive end-expiratory pressure: evidence- and physiology-based! Critical Care. 2019;23(1):412. https://doi.org/10.1186/s13054-019-2695-z.
Mascia L, Grasso S, Fiore T, Bruno F, Berardino M, Ducati A. Cerebro-pulmonary interactions during the application of low levels of positive end-expiratory pressure. Intensive Care Med. 2005;31(3):373–9. https://doi.org/10.1007/s00134-004-2491-2 (In English).
Nemer SN, Caldeira JB, Santos RG, et al. Effects of positive end-expiratory pressure on brain tissue oxygen pressure of severe traumatic brain injury patients with acute respiratory distress syndrome: a pilot study. J Crit Care. 2015;30(6):1263–6. https://doi.org/10.1016/j.jcrc.2015.07.019 (In English).
Brower RG, Lanken PN, MacIntyre N, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351(4):327–36. https://doi.org/10.1056/NEJMoa032193 (In English).
Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(6):637–45. https://doi.org/10.1001/jama.299.6.637 (In English).
Mercat A, Richard JC, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(6):646–55. https://doi.org/10.1001/jama.299.6.646 (In English).
Fan E, Checkley W, Stewart TE, et al. Complications from recruitment maneuvers in patients with acute lung injury: secondary analysis from the lung open ventilation study. Respir Care. 2012;57(11):1842–9. https://doi.org/10.4187/respcare.01684.
Battaglini D, Siwicka Gieroba D, Brunetti I, et al. Mechanical ventilation in neurocritical care setting: a clinical approach. Best Pract Res Clin Anaesthesiol. 2021;35(2):207–20. https://doi.org/10.1016/j.bpa.2020.09.001.
Boone MD, Jinadasa SP, Mueller A, et al. The effect of positive end-expiratory pressure on intracranial pressure and cerebral hemodynamics. Neurocrit Care. 2017;26(2):174–81. https://doi.org/10.1007/s12028-016-0328-9 (In English).
Frost EA. Effects of positive end-expiratory pressure on intracranial pressure and compliance in brain-injured patients. J Neurosurg. 1977;47(2):195–200. https://doi.org/10.3171/jns.1977.47.2.0195 (In English).
McGuire G, Crossley D, Richards J, Wong D. Effects of varying levels of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure. Crit Care Med. 1997;25(6):1059–62. https://doi.org/10.1097/00003246-199706000-00025 (In English).
Georgiadis D, Schwarz S, Baumgartner RW, Veltkamp R, Schwab S. Influence of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure in patients with acute stroke. Stroke. 2001;32(9):2088–92. https://doi.org/10.1161/hs0901.095406 (In English).
Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567–75. https://doi.org/10.1007/s00134-016-4505-2.
Giosa L, Busana M, Pasticci I, et al. Mechanical power at a glance: a simple surrogate for volume-controlled ventilation. Intensive Care Med Exp. 2019;7(1):61. https://doi.org/10.1186/s40635-019-0276-8.
Serpa Neto A, Deliberato RO, Johnson AEW, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44(11):1914–22. https://doi.org/10.1007/s00134-018-5375-6.
Zhang Z, Zheng B, Liu N, Ge H, Hong Y. Mechanical power normalized to predicted body weight as a predictor of mortality in patients with acute respiratory distress syndrome. Intensive Care Med. 2019;45(6):856–64. https://doi.org/10.1007/s00134-019-05627-9.
Jiang X, Zhu Y, Zhen S, Wang L. Mechanical power of ventilation is associated with mortality in neurocritical patients: a cohort study. J Clin Monit Comput. 2022. https://doi.org/10.1007/s10877-022-00805-5.
Robba C, Citerio G, Taccone FS, et al. Multicentre observational study on practice of ventilation in brain injured patients: the VENTIBRAIN study protocol. BMJ Open. 2021;11(8):e047100. https://doi.org/10.1136/bmjopen-2020-047100 (In English).
Chesnut R, Aguilera S, Buki A, et al. A management algorithm for adult patients with both brain oxygen and intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2020;46(5):919–29. https://doi.org/10.1007/s00134-019-05900-x (In English).
Chesnut RM, Marshall LF, Klauber MR, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34(2):216–22. https://doi.org/10.1097/00005373-199302000-00006 (In English).
Steyerberg EW, Mushkudiani N, Perel P, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5(8):e165. https://doi.org/10.1371/journal.pmed.0050165 (discussion e165. (In English)).
McHugh GS, Engel DC, Butcher I, et al. Prognostic value of secondary insults in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24(2):287–93. https://doi.org/10.1089/neu.2006.0031 (In English).
Ób D, Nickson C, Pilcher DV, Udy AA. Early hyperoxia in patients with traumatic brain injury admitted to intensive care in Australia and New Zealand: a retrospective multicenter cohort study. Neurocrit Care. 2018;29(3):443–51. https://doi.org/10.1007/s12028-018-0553-5 (In English).
Brenner M, Stein D, Hu P, Kufera J, Wooford M, Scalea T. Association between early hyperoxia and worse outcomes after traumatic brain injury. Arch Surg. 2012;147(11):1042–6. https://doi.org/10.1001/archsurg.2012.1560 (In English).
Roberts BW, Kilgannon JH, Hunter BR, et al. Association between early hyperoxia exposure after resuscitation from cardiac arrest and neurological disability: prospective multicenter protocol-directed cohort study. Circulation. 2018;137(20):2114–24. https://doi.org/10.1161/circulationaha.117.032054 (In English).
Haugaard N. Cellular mechanisms of oxygen toxicity. Physiol Rev. 1968;48(2):311–73. https://doi.org/10.1152/physrev.1968.48.2.311 (In English).
Muizelaar JP, Marmarou A, Ward JD, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75(5):731–9. https://doi.org/10.3171/jns.1991.75.5.0731 (In English).
Popugaev KA, Lubnin AY. Postoperative care in neurooncology. In: Wartenberg KE, Shukri K, Abdelhak T, editors. Neurointensive care: a clinical guide to patient safety. Cham: Springer; 2015. p. 95–123.
Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426. https://doi.org/10.1183/13993003.02426-2016.
Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–96. https://doi.org/10.1056/NEJMoa1503326 (In English).
Rappaport SH, Shpiner R, Yoshihara G, Wright J, Chang P, Abraham E. Randomized, prospective trial of pressure-limited versus volume-controlled ventilation in severe respiratory failure. Crit Care Med. 1994;22(1):22–32. https://doi.org/10.1097/00003246-199401000-00009 (In English).
Prella M, Feihl F, Domenighetti G. Effects of short-term pressure-controlled ventilation on gas exchange, airway pressures, and gas distribution in patients with acute lung injury/ARDS: comparison with volume-controlled ventilation. Chest. 2002;122(4):1382–8. https://doi.org/10.1378/chest.122.4.1382 (In English).
Chiumello D, Pelosi P, Calvi E, Bigatello LM, Gattinoni L. Different modes of assisted ventilation in patients with acute respiratory failure. Eur Respir J. 2002;20(4):925–33. https://doi.org/10.1183/09031936.02.01552001 (In English).
Silva PL, Rocco PRM. The basics of respiratory mechanics: ventilator-derived parameters. Ann Transl Med. 2018;6(19):376. https://doi.org/10.21037/atm.2018.06.06 (In English).
Stocchetti N, Maas AI, Chieregato A, van der Plas AA. Hyperventilation in head injury: a review. Chest. 2005;127(5):1812–27. https://doi.org/10.1378/chest.127.5.1812 (In English).
Curley G, Kavanagh BP, Laffey JG. Hypocapnia and the injured brain: more harm than benefit. Crit Care Med. 2010;38(5):1348–59. https://doi.org/10.1097/CCM.0b013e3181d8cf2b (In English).
Godoy DA, Seifi A, Garza D, Lubillo-Montenegro S, Murillo-Cabezas F. Hyperventilation therapy for control of posttraumatic intracranial hypertension. Front Neurol. 2017;8:250. https://doi.org/10.3389/fneur.2017.00250 (In English).
Chang JJ, Youn TS, Benson D, et al. Physiologic and functional outcome correlates of brain tissue hypoxia in traumatic brain injury. Crit Care Med. 2009;37(1):283–90. https://doi.org/10.1097/CCM.0b013e318192fbd7 (In English).
Taran S, Pelosi P, Robba C. Optimizing oxygen delivery to the injured brain. Curr Opin Crit Care. 2022;28(2):145–56. https://doi.org/10.1097/mcc.0000000000000913 (In English).
Okonkwo DO, Shutter LA, Moore C, et al. Brain oxygen optimization in severe traumatic brain injury phase-II: a phase II randomized trial. Crit Care Med. 2017;45(11):1907–14. https://doi.org/10.1097/ccm.0000000000002619 (In English).
Doblar DD, Santiago TV, Kahn AU, Edelman NH. The effect of positive end-expiratory pressure ventilation (PEEP) on cerebral blood flow and cerebrospinal fluid pressure in goats. Anesthesiology. 1981;55(3):244–50. https://doi.org/10.1097/00000542-198109000-00010 (In English).
Roth C, Ferbert A, Deinsberger W, et al. Does prone positioning increase intracranial pressure? A retrospective analysis of patients with acute brain injury and acute respiratory failure. Neurocrit Care. 2014;21(2):186–91. https://doi.org/10.1007/s12028-014-0004-x (In English).
Oddo M, Crippa IA, Mehta S, et al. Optimizing sedation in patients with acute brain injury. Crit Care. 2016;20(1):128. https://doi.org/10.1186/s13054-016-1294-5.
Roberts DJ, Hall RI, Kramer AH, Robertson HL, Gallagher CN, Zygun DA. Sedation for critically ill adults with severe traumatic brain injury: a systematic review of randomized controlled trials. Crit Care Med. 2011;39(12):2743–51. https://doi.org/10.1097/CCM.0b013e318228236f (In English).
Chanques G, Constantin JM, Devlin JW, et al. Analgesia and sedation in patients with ARDS. Intensive Care Med. 2020;46(12):2342–56. https://doi.org/10.1007/s00134-020-06307-9 (In English).
Loh N-HW, Nair P. Propofol infusion syndrome. Contin Educ Anaesthesia Crit Care Pain. 2013;13(6):200–2. https://doi.org/10.1093/bjaceaccp/mkt007.
White PF, Schlobohm RM, Pitts LH, Lindauer JM. A randomized study of drugs for preventing increases in intracranial pressure during endotracheal suctioning. Anesthesiology. 1982;57(3):242–4. https://doi.org/10.1097/00000542-198209000-00019 (In English).
Renew JR, Ratzlaff R, Hernandez-Torres V, Brull SJ, Prielipp RC. Neuromuscular blockade management in the critically Ill patient. J Intensive Care. 2020;8(1):37. https://doi.org/10.1186/s40560-020-00455-2.
Hsiang JK, Chesnut RM, Crisp CB, Klauber MR, Blunt BA, Marshall LF. Early, routine paralysis for intracranial pressure control in severe head injury: is it necessary? Crit Care Med. 1994;22(9):1471–6. https://doi.org/10.1097/00003246-199409000-00019 (In English).
Hess DR. Recruitment maneuvers and PEEP titration. Respir Care. 2015;60(11):1688–704. https://doi.org/10.4187/respcare.04409.
Krebs J, Tsagogiorgas C, Pelosi P, et al. Open lung approach with low tidal volume mechanical ventilation attenuates lung injury in rats with massive brain damage. Crit Care. 2014;18(2):R59. https://doi.org/10.1186/cc13813 (In English).
Wolf S, Schürer L, Trost HA, Lumenta CB. The safety of the open lung approach in neurosurgical patients. Acta Neurochir Suppl. 2002;81:99–101. https://doi.org/10.1007/978-3-7091-6738-0_26 (In English).
Goligher EC, Tomlinson G, Hajage D, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome and posterior probability of mortality benefit in a post hoc bayesian analysis of a randomized clinical trial. JAMA. 2018;320(21):2251–9. https://doi.org/10.1001/jama.2018.14276 (In English).
Bein T, Scherer MN, Philipp A, Weber F, Woertgen C. Pumpless extracorporeal lung assist (pECLA) in patients with acute respiratory distress syndrome and severe brain injury. J Trauma. 2005;58(6):1294–7. https://doi.org/10.1097/01.ta.0000173275.06947.5c (In English).
Biscotti M, Gannon W, Abrams D, et al. Extracorporeal membrane oxygenation use in patients with traumatic brain injury. Perfusion. 2015;30(5):407–9. https://doi.org/10.1177/0267659114554327.
Bruzek AK, Vega RA, Mathern BE. Extracorporeal membrane oxygenation support as a life-saving measure for acute respiratory distress syndrome after craniectomy. J Neurosurg Anesthesiol. 2014;26(3):259–60. https://doi.org/10.1097/ANA.0b013e3182a5d0fd (In English).
Fletcher Sandersjöö A, Bartek J, Thelin EP, et al. Predictors of intracranial hemorrhage in adult patients on extracorporeal membrane oxygenation: an observational cohort study. J Intensive Care. 2017;5(1):27. https://doi.org/10.1186/s40560-017-0223-2.
Chiarini G, Cho SM, Whitman G, Rasulo F, Lorusso R. Brain injury in extracorporeal membrane oxygenation: a multidisciplinary approach. Semin Neurol. 2021;41(4):422–36. https://doi.org/10.1055/s-0041-1726284 (In English).
Kurihara C, Walter JM, Karim A, et al. Feasibility of venovenous extracorporeal membrane oxygenation without systemic anticoagulation. Ann Thorac Surg. 2020;110(4):1209–15. https://doi.org/10.1016/j.athoracsur.2020.02.011 (In English).
Frisvold SK, Robba C, Guérin C. What respiratory targets should be recommended in patients with brain injury and respiratory failure? Intensive Care Med. 2019;45(5):683–6. https://doi.org/10.1007/s00134-019-05556-7.
Marklund N. The neurological wake-up test-a role in neurocritical care monitoring of traumatic brain injury patients? Front Neurol. 2017;8:540. https://doi.org/10.3389/fneur.2017.00540 (In English).
Marra A, Ely EW, Pandharipande PP, Patel MB. The ABCDEF bundle in critical care. Crit Care Clin. 2017;33(2):225–43. https://doi.org/10.1016/j.ccc.2016.12.005 (In English).
Thille AW, Harrois A, Schortgen F, Brun-Buisson C, Brochard L. Outcomes of extubation failure in medical intensive care unit patients. Crit Care Med. 2011;39(12):2612–8. https://doi.org/10.1097/CCM.0b013e3182282a5a (In English).
Thille AW, Richard JC, Brochard L. The decision to extubate in the intensive care unit. Am J Respir Crit Care Med. 2013;187(12):1294–302. https://doi.org/10.1164/rccm.201208-1523CI (In English).
Coplin WM, Pierson DJ, Cooley KD, Newell DW, Rubenfeld GD. Implications of extubation delay in brain-injured patients meeting standard weaning criteria. Am J Respir Crit Care Med. 2000;161(5):1530–6. https://doi.org/10.1164/ajrccm.161.5.9905102 (In English).
Thille AW, Cortés-Puch I, Esteban A. Weaning from the ventilator and extubation in ICU. Curr Opin Crit Care. 2013;19(1):57–64. https://doi.org/10.1097/MCC.0b013e32835c5095.
Asehnoune K, Mrozek S, Perrigault PF, et al. A multi-faceted strategy to reduce ventilation-associated mortality in brain-injured patients. The BI-VILI project: a nationwide quality improvement project. Intensive Care Med. 2017;43(7):957–70. https://doi.org/10.1007/s00134-017-4764-6 (In English).
Godet T, Chabanne R, Marin J, et al. Extubation failure in brain-injured patients: risk factors and development of a prediction score in a preliminary prospective cohort study. Anesthesiology. 2017;126(1):104–14. https://doi.org/10.1097/aln.0000000000001379 (In English).
McCredie VA, Ferguson ND, Pinto RL, et al. Airway management strategies for brain-injured patients meeting standard criteria to consider extubation. A prospective cohort study. Ann Am Thorac Soc. 2017;14(1):85–93. https://doi.org/10.1513/AnnalsATS.201608-620OC (In English).
Dos Reis HFC, Gomes-Neto M, Almeida MLO, et al. Development of a risk score to predict extubation failure in patients with traumatic brain injury. J Crit Care. 2017;42:218–22. https://doi.org/10.1016/j.jcrc.2017.07.051 (In English).
Ibrahim AS, Aly MG, Abdel-Rahman KA, Mohamed MA, Mehany MM, Aziz EM. Semi-quantitative cough strength score as a predictor for extubation outcome in traumatic brain injury: a prospective observational study. Neurocrit Care. 2018;29(2):273–9. https://doi.org/10.1007/s12028-018-0539-3 (In English).
Namen AM, Ely EW, Tatter SB, et al. Predictors of successful extubation in neurosurgical patients. Am J Respir Crit Care Med. 2001;163(3 Pt 1):658–64. https://doi.org/10.1164/ajrccm.163.3.2003060 (In English).
Cinotti R, Bouras M, Roquilly A, Asehnoune K. Management and weaning from mechanical ventilation in neurologic patients. Ann Transl Med. 2018;6(19):7.
Nelson E, Powell JR, Conrad K, et al. Phenobarbital pharmacokinetics and bioavailability in adults. J Clin Pharmacol. 1982;22(2–3):141–8. https://doi.org/10.1002/j.1552-4604.1982.tb02662.x (In English).
Hughes MA, Glass PS, Jacobs JR. Context-sensitive half-time in multicompartment pharmacokinetic models for intravenous anesthetic drugs. Anesthesiology. 1992;76(3):334–41. https://doi.org/10.1097/00000542-199203000-00003 (In English).
Cammarano WB, Pittet JF, Weitz S, Schlobohm RM, Marks JD. Acute withdrawal syndrome related to the administration of analgesic and sedative medications in adult intensive care unit patients. Crit Care Med. 1998;26(4):676–84. https://doi.org/10.1097/00003246-199804000-00015 (In English).
Reade MC, O’Sullivan K, Bates S, Goldsmith D, Ainslie WR, Bellomo R. Dexmedetomidine vs. haloperidol in delirious, agitated, intubated patients: a randomised open-label trial. Critical Care. 2009;13(3):R75. https://doi.org/10.1186/cc7890.
Dupuis S, Brindamour D, Karzon S, et al. A systematic review of interventions to facilitate extubation in patients difficult-to-wean due to delirium, agitation, or anxiety and a meta-analysis of the effect of dexmedetomidine. Can J Anaesth. 2019;66(3):318–27. https://doi.org/10.1007/s12630-018-01289-1 (In English).
Thille AW, Muller G, Gacouin A, et al. Effect of postextubation high-flow nasal oxygen with noninvasive ventilation vs high-flow nasal oxygen alone on reintubation among patients at high risk of extubation failure: a randomized clinical trial. JAMA. 2019;322(15):1465–75. https://doi.org/10.1001/jama.2019.14901 (In English).
Hernández G, Vaquero C, Colinas L, et al. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA. 2016;316(15):1565–74. https://doi.org/10.1001/jama.2016.14194 (In English).
Hernández G, Vaquero C, González P, et al. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA. 2016;315(13):1354–61. https://doi.org/10.1001/jama.2016.2711.
McCredie VA, Alali AS, Scales DC, et al. Effect of early versus late tracheostomy or prolonged intubation in critically Ill patients with acute brain injury: a systematic review and meta-analysis. Neurocrit Care. 2017;26(1):14–25. https://doi.org/10.1007/s12028-016-0297-z (In English).
Funding
There were no sources of funding.
Author information
Authors and Affiliations
Contributions
ST: manuscript organization, outline generation, review of the literature, writing of successive versions. S-MC: review of the literature, critical review of manuscript drafts. RD.S: manuscript conception and organization, critical review of manuscript drafts, reworking of final version for submission.
Corresponding author
Ethics declarations
Conflict of interest
None directly or indirectly linked to this work.
Ethical approval/informed consent
Ethical approval and informed consent were not required for this review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taran, S., Cho, SM. & Stevens, R.D. Mechanical Ventilation in Patients with Traumatic Brain Injury: Is it so Different?. Neurocrit Care 38, 178–191 (2023). https://doi.org/10.1007/s12028-022-01593-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-022-01593-1