Abstract
Background
There is insufficient evidence to guide ventilatory targets in acute brain injury (ABI). Recent studies have shown associations between mechanical power (MP) and mortality in critical care populations. We aimed to describe MP in ventilated patients with ABI, and evaluate associations between MP and clinical outcomes.
Methods
In this preplanned, secondary analysis of a prospective, multi-center, observational cohort study (ENIO, NCT03400904), we included adult patients with ABI (Glasgow Coma Scale ≤ 12 before intubation) who required mechanical ventilation (MV) ≥ 24 h. Using multivariable log binomial regressions, we separately assessed associations between MP on hospital day (HD)1, HD3, HD7 and clinical outcomes: hospital mortality, need for reintubation, tracheostomy placement, and development of acute respiratory distress syndrome (ARDS).
Results
We included 1217 patients (mean age 51.2 years [SD 18.1], 66% male, mean body mass index [BMI] 26.3 [SD 5.18]) hospitalized at 62 intensive care units in 18 countries. Hospital mortality was 11% (n = 139), 44% (n = 536) were extubated by HD7 of which 20% (107/536) required reintubation, 28% (n = 340) underwent tracheostomy placement, and 9% (n = 114) developed ARDS. The median MP on HD1, HD3, and HD7 was 11.9 J/min [IQR 9.2–15.1], 13 J/min [IQR 10–17], and 14 J/min [IQR 11–20], respectively. MP was overall higher in patients with ARDS, especially those with higher ARDS severity. After controlling for same-day pressure of arterial oxygen/fraction of inspired oxygen (P/F ratio), BMI, and neurological severity, MP at HD1, HD3, and HD7 was independently associated with hospital mortality, reintubation and tracheostomy placement. The adjusted relative risk (aRR) was greater at higher MP, and strongest for: mortality on HD1 (compared to the HD1 median MP 11.9 J/min, aRR at 17 J/min was 1.22, 95% CI 1.14–1.30) and HD3 (1.38, 95% CI 1.23–1.53), reintubation on HD1 (1.64; 95% CI 1.57–1.72), and tracheostomy on HD7 (1.53; 95%CI 1.18–1.99). MP was associated with the development of moderate-severe ARDS on HD1 (2.07; 95% CI 1.56–2.78) and HD3 (1.76; 95% CI 1.41–2.22).
Conclusions
Exposure to high MP during the first week of MV is associated with poor clinical outcomes in ABI, independent of P/F ratio and neurological severity. Potential benefits of optimizing ventilator settings to limit MP warrant further investigation.
Similar content being viewed by others
Introduction
Patients with acute brain injury (ABI) commonly require intubation and mechanical ventilation (MV) due to insufficient airway protective reflexes, impaired respiratory drive, and secondary pulmonary events such as aspiration/pneumonia, pulmonary edema, or acute respiratory distress syndrome (ARDS) [1,2,3,4,5,6]. However, there are insufficient data to guide optimal ventilatory targets for brain injured patients [7]. Patients with ABI have frequently been excluded from landmark studies guiding MV practices in critical care cohorts [8,9,10], and the impact of various MV parameters on clinical outcomes is insufficiently explored in this population.
The concept of mechanical power (MP) as a determinant of ventilator-induced lung injury (VILI) has gained increasing attention [11]. A summary variable comprised of all the MV components which can cause VILI, including pressure, volume, flow, and respiratory rate (RR), MP is thought to represent the total energy delivered to the respiratory system during each breathing cycle multiplied by RR. Recent studies have demonstrated an association between higher MP and mortality in mixed critical care populations [12], both with [13] and without ARDS [14], and in patients with hypoxemic-ischemic encephalopathy (HIE) after cardiac arrest [15]. However, limited data are available regarding the role of MP in other ABI populations, with only one retrospective, single-center study showing an association between MP in the first 24 h and mortality during the intensive care unit (ICU) stay [16].
We performed a preplanned secondary analysis of the “Extubation strategies in neuro-intensive care unit patients and associations with outcomes (ENIO)” study—a prospective, international, multi-center observational cohort study assessing factors associated with extubation failure [17]. Our goals were to describe MP in ABI during the first week of MV and evaluate associations between MP at three time points and clinical outcomes. We hypothesized that there is substantial practice variation based on region and presence of ARDS, and that MP is associated with hospital mortality, need for reintubation, tracheostomy placement, and development of moderate-severe ARDS.
Methods
Setting The present analysis utilized data from the ENIO study (NCT03400904), a prospective, international, multi-center observational cohort study that enrolled 1512 patients with ABI between 2018 and 2020 at 73 centers in 18 countries. The aims of the parent study were to describe current MV management and weaning practices, assess the incidence of extubation failure, rate of tracheostomy placement, and validate a score predictive of extubation success [17].
Ethical approval and reporting All centers were required to obtain regional or national IRB approval to participate in the ENIO study. The study was approved by the Steering Committee, no further IRB approval was necessary for the present analysis. We adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [18].
Study population The ENIO study included adults (≥ 18 years) with ABI who were admitted to the intensive care unit (ICU) with a Glasgow Coma Scale (GCS) ≤ 12 before endotracheal intubation, and required invasive MV ≥ 24 h. Subtypes of brain injuries considered were traumatic brain injury (TBI), aneurysmal subarachnoid hemorrhage (SAH), intracranial hemorrhage (ICH), acute ischemic stroke (AIS), central nervous system infections, and brain tumors. Patients were excluded if they met any of the following criteria: < 18 years of age, pregnancy, spinal cord injury above T4, resuscitated after cardiac arrest, Guillain–Barre syndrome, withdrawal of life-sustaining treatments (WLST) ≤ 24 h after ICU admission, terminal extubation in the setting of WLST during ICU course, baseline major respiratory co-morbidities (requiring chronic oxygen at home, chronic obstructive pulmonary disease grade III-IV according to the Gold classification), and major chest trauma (Abbreviated Injury Score ≥ 3).
For the present analysis, we additionally excluded patients with insufficient data to calculate MP on hospital day (HD) 1, or those who were on a spontaneous breathing mode on HD1.
Objectives The primary aim of this study was to assess the use of MP on HD1, HD3, and HD7 in mechanically ventilated, brain-injured patients; our secondary aim was to evaluate the associations between MP at the three time points and clinical outcomes.
Clinical outcomes included hospital mortality- defined as death during the first hospital stay following ABI—need for reintubation during the initial ICU stay, tracheostomy placement during the initial ICU stay, and development of moderate-severe ARDS based on the Berlin definition [19] during the ICU stay.
Data extraction Demographic and baseline data were collected at the time of enrollment. Ventilatory parameters, arterial blood gas values, and use of sedative medications (Propofol, Midazolam, Dexmedetomidine, Penthotal), were recorded at HD1, HD3 and HD7 after ICU admission. Markers of neurological severity documented included: initial GCS before intubation, anisocoria, placement of an intracranial pressure (ICP) monitor or external ventricular drainage (EVD), decompressive craniectomy (DC), and barbiturate coma. Ventilatory parameters recorded for each HD included: tidal volume (Vt), RR, positive end-expiratory pressure (PEEP), and plateau pressure (Pplat); also, the partial pressure of arterial oxygen/fraction of inspired oxygen (P/F) ratio and driving pressure (ΔP) were calculated for each HD. MP was calculated based on previously validated formulas [11, 20, 21]. Data on mortality, reintubation, tracheostomy and ARDS were prospectively captured during the index hospitalization, and follow-up was completed at hospital discharge.
Statistical analysis We summarized continuous variables using ranges, means (standard deviations, SD) or median (interquartile range, IQR) and categorical variables using percentages. Means, medians and frequencies were compared using the t-test, Wilcoxon-Mann–Whitney test, and chi-squares, respectively. We utilized multivariable log binomial regressions with robust standard errors to evaluate the associations between MP on HD1, HD3, and HD7 and (1) hospital mortality, (2) need for reintubation, (3) tracheostomy placement, and (4) development of moderate-severe ARDS. For development of moderate-severe ARDS, we assessed MP only on HD1 and HD3 as exposure variables, because we were not able to discern which proportion of patients developed ARDS before HD7. We built separate models for each outcome of interest, adjusting for baseline characteristics, comorbidities, body mass index (BMI), region, type of brain injury, markers of neurological severity, and arterial blood gas values (Additional file 1: Appendix). A priori confounders and variables that were statistically significant in univariate analyses (P < 0.05) were considered for inclusion in multivariable analyses. The linearity assumption of continuous variables was tested, and variable transformed with the appropriate fractional polynomials when the assumption was not met [22]. Adjusted risk ratios (aRR) were calculated in comparison to the median MP utilized on HD1. We utilized R Studio 2022.02.3 and Stata 15.1 for statistical analyses.
Results
Patient characteristics
Of 1512 patients enrolled in the ENIO study, we excluded 286 (17%) patients due to insufficient data to calculate MP, and another 9 (0.6%) who were on a spontaneous breathing mode on HD1 (Additional file 1: Figure S1). We included 1217 patients from 18 countries at 62 centers in the analysis; the mean age was 51 years (SD 18), the majority were male (66%, n = 805), and mean BMI was 26.3 (SD 5.18). Most patients were from Europe/Central Asia (69%, n = 845) or Latin America/Caribbean (19%, n = 236). The most common underlying diagnoses were TBI (48%, n = 588), ICH (31%, n = 382), and SAH (18%, n = 218). The initial GCS before intubation was ≤ 8 in 77% (n = 937), 28% (n = 338) had an episode of anisocoria during their hospitalization (Table 1).
Mortality at ICU discharge was 7% (n = 83), and increased to 11% (n = 139) by hospital discharge. WLST occurred in 29% (n = 41) of all hospital mortalities at a median of 17 days [IQR 7–34]. Among survivors, 34% (356/1034) had a GCS of 13–15 at the time of extubation. By HD3, 23% (n = 270) of patients were extubated and 8% (n = 101) were weaned to a spontaneous mode; by HD7, 44% (n = 536) were extubated and 10% (n = 120) were weaned to a spontaneous mode (Additional file 1: Figure S2). Among patients who were extubated by HD7, 20% (107/536) required reintubation. Among patients who underwent tracheostomy placement (28%, n = 340), most (79% n = 267/340) received a tracheostomy without a prior extubation trial. Overall, 9% (n = 114) developed ARDS (21% (n = 24) mild, 38% (n = 43) moderate, and 41% (n = 47) severe ARDS).
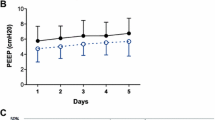
Ventilator settings and arterial blood gas values by HD are summarized in Table 2. Baseline characteristics and markers of disease severity stratified by HD are displayed in Additional file 1: Fig. S3, Table S1, and were largely similar across the time points.
Utilization of mechanical power and trajectories
The median MP on HD1, HD3, and HD7 was 11.9 J/min [IQR 9.2–15.1, range 3.1–44.4], 13 J/min [IQR 10–17, range 2.5–39.2], and 14 J/min [IQR 11–20, range 3.5–66.9] respectively. Across countries, median MP ranged from 8.9 to 18.2 J/min (HD 1), 7.2–17.6 J/min (HD3), and 8.3–19.2 J/min (HD7) (Additional file 1: Table S2, Figure S4). MP mainly varied based on the presence of ARDS, was higher in patients with higher ARDS severity, and did not substantially differ based on neurological severity (Table 3). MP on HD3 and HD7 was significantly higher in patients on sedative medications, compared to those who did not receive any sedation (Table 4).
Median MP was higher on HD1, HD3 and HD7 among patients with an initial P/F ratio ≤ 200 and whose P/F ratio remained ≤ 200 compared to those whose P/F ratio improved to > 200 by HD7 (Fig. 1a). Additionally, median MP was higher on HD1, HD3 and HD7 in patients with an initial P/F ratio > 200 whose P/F ratio worsened to ≤ 200 by HD7, compared to those whose P/F ratio remained > 200 by HD7 (Fig. 1b). Among patients with an initial GCS ≤ 8, the median MP on HD1, HD3 and HD7 was largely similar in patients whose GCS remained ≤ 8 and those whose GCS improved by the time of extubation (Fig. 1c).
Mechanical power trajectories. a Mechanical power based on trajectories of P/F ratio for patients with P/F ratio ≤ 200 on hospital day 1. b Mechanical power based on trajectories of P/F ratio for patients with P/F ratio > 200 on hospital day 1. c Mechanical power based on trajectories of GCS for patients with an initial GCS ≤ 8
Associations between mechanical power and clinical outcomes
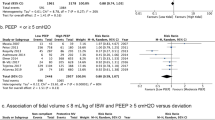
In separate multivariable models controlling for age, BMI, region, comorbidities, type of brain injury, neurological severity, same day P/F ratio, ventilator mode and sedation, MP on HD1, HD3, and HD7 was independently associated with hospital mortality, with greater aRR at higher MP (Fig. 2a, Additional file 1: Table S3a, omnibus p-values for non-linear trajectories were p < 0.001, p < 0.001, p = 0.003 respectively). Within the most commonly utilized range of 9–20 J/min, the aRR (compared to the HD1 median of 11.9 J/min) for HD1 was 1.22 (95% CI 1.14–1.30) at 17 J/min and 1.47 (95% CI 1.28–1.65) at 20 J/min. On HD3, the aRR was 1.38 (95% CI 1.23–1.53) at 17 J/min and 1.49 (95% CI 1.30–1.71) at 20 J/min, and on HD7, the aRR was 1.06 (95% CI 1.05–1.32) at 17 J/min and 1.23 (95% CI 1.07–1.42) at 20 J/min. (Table 5) The increment in aRR for each J/min was highest on HD1.
Associations between mechanical power (MP) and clinical outcomes at hospital day one, three and seven. EVD = Extraventricular Drain, GCS = Glasgow Coma Scale, ICP = Intracranial Pressure. a Associations between MP and mortality. The model was adjusted for the following covariates: age, region, comorbidities (heart failure, diabetes, pulmonary disease), body mass index, type of brain injury, neurological severity (initial GCS, anisocoria, ICP monitor in place, EVD in place, decompressive craniectomy, barbiturate coma), arterial blood gas values (same day P/F ratio), ventilator mode, and sedation (same day Propofol, Midazolam). b Associations between MP and need for reintubation. The model was adjusted for the following covariates: age, region, comorbidities (heart failure, hypertension, pulmonary disease), body mass index, type of brain injury, neurological severity (initial GCS, anisocoria, ICP monitor in place, EVD in place, decompressive craniectomy, barbiturate coma), swallowing function on the day of extubation, suctioning frequency on the day of extubation,, arterial blood gas values (same day P/F ratio), ventilator mode, and sedation (same day Propofol, Midazolam). c Associations between MP and tracheostomy placement. The model was adjusted for the following covariates: age, region, comorbidities (heart failure, hypertension pulmonary disease), body mass index, type of brain injury, neurological severity (initial GCS, anisocoria, ICP monitor in place, EVD in place, decompressive craniectomy, barbiturate coma), swallowing function on the day of extubation, suctioning frequency on the day of extubation,, arterial blood gas values (same day P/F ratio), ventilator mode, and sedation (same day Propofol, Midazolam). d Associations between MP and development of moderate to severe acute respiratory distress syndrome (ARDS). The model was adjusted for the following covariates: age, sex, region, baseline pulmonary or cardiac disease, type of brain injury, initial GCS, decompressive craniectomy, arterial blood gas values (same day PaO2 and PaCO2), ventilator mode and ventilator associated pneumonia
MP on all three hospital days was associated with need for reintubation after controlling for covariates, including factors associated with extubation failure in the main ENIO analysis (Fig. 2b, Additional file 1: Table S3b, omnibus p-values for non-linear trajectories were all < 0.001). Compared to the HD1 median, the aRR was strongest on HD1 :1.64 (95% CI 1.57–1.72) at 17 J/min and 2.05 (95% CI 1.92–2.20) at 20 J/min) and the increment in aRR for each J/min was steepest on HD1 and HD3. (Table 5).
MP on all three hospital days was associated with tracheostomy placement after controlling for covariates (Fig. 2c, Additional file 1: Table S3c, omnibus p-values for non-linear trajectories were p = 0.005, p = 0.019, and p = 0.001, respectively); the aRR was strongest on HD7:1.53 (95% CI 1.18–1.99) at 17 J/min and 1.71 (95% CI 1.23–2.39) at 20 J/min (Table 5).
MP on HD1 and HD3 was associated with moderate-severe ARDS after controlling for covariates (Fig. 2d, Table S3d, omnibus p-values for non-linear trajectories were p < 0.001 for both days). For HD1, aRR compared to the HD1 median was 2.07 (1.56–2.78) at 17 J/min and 2.88 (1.89–4.27) at 20 J/min; for HD3, aRR was 1.76 (1.41–2.22) at 17 J/min and 2.64 (1.79–3.90) at 20 J/min (Table 5).
Discussion
In this preplanned, secondary analysis of the ENIO study assessing use and effect of mechanical power in ABI, our main findings are: (1) MP varied widely by region, tended to be higher based on presence and severity of ARDS, and differed by trajectory of P/F ratio, (2) MP at all time points was associated with hospital mortality, need for reintubation, tracheostomy placement and development of moderate-severe ARDS, and (3) associations between MP and hospital mortality, reintubation, and ARDS were strongest during the early days of MV. To date, this is the largest observational investigation evaluating the use of MP in ABI and its association with clinical outcomes. We included patients from 62 institutions in 18 countries, representing current practices worldwide.
In critically ill patients with ABI, pathophysiological interactions between brain and lungs are complex and bi-directional [6]. ABI has been shown to induce or worsen lung injury via several mechanisms, including elevated ICP, systemic inflammatory response, hormonal dysregulation, and catecholamine surges [6, 23, 24]. Conversely, hypoxemia and systemic inflammation can precipitate secondary brain injury, and ventilatory strategies that have proven to be beneficial for management of ARDS, such as PEEP titration, low Vt, and prone ventilation, may affect ICP, and cerebral perfusion pressure. [6, 25, 26]. As ABI comprises up to 20% of patients requiring MV [27, 28], with little data to guide ventilator management accounting for brain-lung crosstalk [29], more information about use and effect of MV strategies is important to inform future studies, and establish optimal ventilatory targets for this population.
The substantial regional practice variations in utilization of MP in our study underscore the lack of definite knowledge and data on ventilator management in ABI. Results of a large, prospective multicenter observational study (NCT04459884) are forthcoming [30], and randomized controlled trials (RCTs) are needed to provide more clarity on this topic.
Overall, medians and ranges of MP observed in our study were similar to values described in another ABI cohort [16], but lower compared to those described in a large general critical care cohort [12] and a post-cardiac arrest cohort [15], possibly due to higher proportions of lung injury in these populations. Our results also suggest that MP utilization is mainly driven by concomitant lung injury and ARDS. The question of whether markers of neurological severity merit consideration in choosing ventilator settings warrants further exploration.
The associations between MP and clinical outcomes in the first week of mechanical ventilation, present as early as HD1, support the hypothesis that MV settings precipitate VILI. Different ventilator variables (Vt, [8, 31] Pplat [8], PEEP [32, 33], driving pressure [34,35,36]) have been associated with mortality and longer duration of MV, presumably by contributing to VILI. Strategies targeted at minimizing VILI, specifically the prophylactic utilization of low Vt, [31, 37,38,39], have shown promise in decreasing the risk of developing ARDS. However, titrating one single MV setting may not adequately protect the lungs if the total amount of total energy delivered to the lungs is similar [11]. MP, reflecting the combined effect of various MV settings, has recently emerged as a real-life marker of VILI and predictor of clinical outcomes [11,12,13, 16, 30, 40, 41].
Experimental research has linked MP to diffuse radiographic pulmonary edema, and increased in lung elastance [40], and has suggested correlations between MP and pulmonary neutrophilic inflammation [41]. A study including 8207 critically ill patients requiring MV for > 48 h showed an association between MP at 24–48 h and 30-day mortality, even at low Vt and driving pressure, and independent of ARDS [12]. A combined analysis of 4549 patients with ARDS demonstrated an association between MP within 24 h and 28-day mortality [13]. A recent, combined analysis of three RCTs also found an association between MP and mortality in non-ARDS populations, even after stratifying for individual components of MP [14]. In the cardiac arrest population, a sub-analysis of the targeted hypothermia versus targeted normothermia after out-of-hospital cardiac arrest (TTM-2) trial including 1848 patients with HIE showed an association between MP in the first 72 h of MV and 6-months mortality [15]. In other populations with ABI, only one retrospective study assessing 529 brain-injured patients demonstrated an association between MP in the first 24 h and ICU mortality, with MP being a stronger predictor of mortality compared to GCS [16].
Our findings are consistent with previous studies and complement this data by showing associations between MP and mortality in a large prospective cohort of ABI, measured at three different time points, controlling for BMI and same day P/F ratio. The associations in the early phases of MV, notable as early as HD1, suggest that there may be a critical time window during which MP could exert a deleterious effect. Also, the associations of MP with moderate-severe ARDS on HD1 and HD3 suggest that MP may be linked to poor outcomes by contributing to VILI. Additionally, we found that MP is associated with reintubation and tracheostomy placement. Our ability to predict which patients with ABI can be extubated remains limited [17, 42]. Recent studies have identified predictors of successful extubation, such as eye movements, gag, cough, secretion burden and GCS [17, 43,44,45]. To our knowledge, this is the first study showing an association between ventilatory settings and reintubation or tracheostomy placement in brain-injured patients. Of note, the majority of patients in our study who underwent tracheostomy placement did not have an extubation trial, likely because providers had higher concerns about their ability to wean from MV and tended to favor tracheostomy placement in those requiring more concerning ventilator settings. More interestingly, the association between MP and reintubation after adjusting for other factors associated with extubation failure in the main ENIO analysis, warrants further investigation. Early injurious effect of MV settings may render the lungs more vulnerable to subsequent ‘second hit-events’, such as aspiration or pneumonia, or contribute to pulmonary edema post extubation.
While difficult to directly compare results due to differences in methodology, our findings suggest a consistent increase in risk of death at lower thresholds (13 J/min) compared to that identified in a general critical care population (17 J/min) [12]. These findings indicate that patients with ABI may be more prone to VILI and other potential detrimental effects of MV, possibly due to brain-lung crosstalk.
Our study has several limitations. First, this is an observational study, which limits conclusions regarding causality. MP is ultimately a composite of parameters that are thought to cause VILI but are also linked to higher disease severity at the same time. While we controlled for markers of disease severity and arterial blood gas values, additional aspects of the patients’ underlying condition and systemic illness may have contributed to ventilator settings and higher MP in patients with worse clinical outcomes. Therefore, we cannot rule out residual confounding or confounding by indication. Second, we assessed the associations between MP and clinical outcomes separately at three time points; we did not have data on MP during the entire period of MV and therefore could not assess the cumulative impact of MP on clinical outcomes. Additionally, since MP on HD1 may be correlated with high MP on subsequent days, it is not possible to determine whether the associations on HD1 are due to an early injurious effect or related to subsequently high MP levels and cumulative lung injury. Third, our sample size decreased over time; while measured clinical characteristics across the time points are similar, the sample may differ by unmeasured covariates, so comparisons across time points are limited. Additionally, due to the smaller sample size at the later time points, some confidence intervals for associations on HD3 and HD7 are wide, limiting our ability to draw conclusions. Forth, we had insufficient power to assess how associations between MP and clinical outcomes vary by ABI subtype due low sample size within each category. Given distinct underlying pathophysiologies for different ABI subtypes, further research is needed to investigate if the impact of MV varies between disease entities. Last, based on the data available, we could not discern how many patients demonstrated a spontaneous respiratory drive while on a controlled mode, and how their own respiratory efforts may have affected MP.
Despite these limitations, our findings can serve as groundwork for future research evaluating the impact of limiting exposure to high MP, cumulative impact of exposure to MP during MV, and assessing injurious MV thresholds in ABI compared to other critical care cohorts. Future studies are also needed to examine how different components of the MP formula contribute to clinical outcomes, including conducting risk prediction modeling [46]. Also, studies collecting more frequent measurements during MV are needed to assess the time varying exposure of MP controlling for time varying confounders such as sedation or hemodynamic data, potentially using G-estimation or other advanced epidemiologic methods [47]. Ultimately, randomized clinical studies are required to assess a causal relationship between MP and clinical outcomes.
Conclusions
Optimizing ventilator settings and limiting exposure to high MP during the first week of mechanical ventilation may be associated with better clinical outcomes in patients with ABI.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABI:
-
Acute brain injury
- AIS:
-
Acute ischemic stroke
- ARDS:
-
Acute respiratory distress syndrome
- BMI:
-
Body Mass Index
- ENIO:
-
Extubation strategies in neuro-intensive care unit patients and associations with outcomes
- EVD:
-
Extraventricular drain
- DC:
-
Decompressive craniectomy
- GCS:
-
Glasgow Coma Scale
- HD:
-
Hospital day
- HIE:
-
Hypoxemic-ischemic encephalopathy
- ICH:
-
Intracranial hemorrhage
- ICP:
-
Intracranial pressure
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- MP:
-
Mechanical power
- MV:
-
Mechanical ventilation
- ΔP :
-
Driving pressure
- PEEP:
-
Positive end-expiratory pressure
- P/F:
-
Partial pressure of arterial oxygen/fraction of inspired oxygen
- P Plat:
-
Plateau pressure
- RCT:
-
Randomized controlled trial
- RR:
-
Respiratory rate
- SAH:
-
Subarachnoid hemorrhage
- SD:
-
Standard deviation
- TBI:
-
Traumatic brain injury
- VILI:
-
Ventilator induced lung injury
- Vt:
-
Tidal volume
- WLST:
-
Withdrawal of life-sustaining treatments
References
Mascia L, Sakr Y, Pasero D, et al. Extracranial complications in patients with acute brain injury: a post-hoc analysis of the SOAP study. Intensive Care Med. 2008;34(4):720–7. https://doi.org/10.1007/s00134-007-0974-7.
Kahn JM, Caldwell EC, Deem S, Newell DW, Heckbert SR, Rubenfeld GD. Acute lung injury in patients with subarachnoid hemorrhage: incidence, risk factors, and outcome. Crit Care Med. 2006;34(1):196–202. https://doi.org/10.1097/01.ccm.0000194540.44020.8e.
Rincon F, Ghosh S, Dey S, et al. Impact of acute lung injury and acute respiratory distress syndrome after traumatic brain injury in the United States. Neurosurgery. 2012;71(4):795–803. https://doi.org/10.1227/NEU.0b013e3182672ae5.
Robba C, Rebora P, Banzato E, et al. Incidence, risk factors, and effects on outcome of ventilator-associated pneumonia in patients with traumatic brain injury: analysis of a large, multicenter, prospective, observational longitudinal study. Chest. 2020;158(6):2292–303. https://doi.org/10.1016/j.chest.2020.06.064.
Elmer J, Hou P, Wilcox SR, et al. Acute respiratory distress syndrome after spontaneous intracerebral hemorrhage*. Crit Care Med. 2013;41(8):1992–2001. https://doi.org/10.1097/CCM.0b013e31828a3f4d.
Matin N, Sarhadi K, Crooks CP, et al. Brain-lung crosstalk: management of concomitant severe acute brain injury and acute respiratory distress syndrome. Curr Treat Options Neurol. 2022;24(9):383–408. https://doi.org/10.1007/s11940-022-00726-3.
Robba C, Poole D, McNett M, et al. Mechanical ventilation in patients with acute brain injury: recommendations of the European society of intensive care medicine consensus. Intensive Care Med. 2020;46(12):2397–410. https://doi.org/10.1007/s00134-020-06283-0.
Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–8. https://doi.org/10.1056/NEJM200005043421801.
Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–68. https://doi.org/10.1056/NEJMoa1214103.
Moss M, Huang DT, National Heart, Lung, and Blood Institute PETAL Clinical Trials Network, et al. Early neuromuscular blockade in the acute respiratory distress syndrome. N Engl J Med. 2019;380(21):1997–2008. https://doi.org/10.1056/NEJMoa1901686.
Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567–75. https://doi.org/10.1007/s00134-016-4505-2.
Serpa Neto A, Deliberato RO, Johnson AEW, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44(11):1914–22. https://doi.org/10.1007/s00134-018-5375-6.
Costa ELV, Slutsky AS, Brochard LJ, et al. Ventilatory variables and mechanical power in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2021;204(3):303–11. https://doi.org/10.1164/rccm.202009-3467OC.
van Meenen DMP, Algera AG, Schuijt MTU, et al. Effect of mechanical power on mortality in invasively ventilated ICU patients without the acute respiratory distress syndrome: an analysis of three randomised clinical trials. Eur J Anaesthesiol. 2023;40(1):21–8. https://doi.org/10.1097/EJA.0000000000001778.
Robba C, Badenes R, Battaglini D, et al. Ventilatory settings in the initial 72 h and their association with outcome in out-of-hospital cardiac arrest patients: a preplanned secondary analysis of the targeted hypothermia versus targeted normothermia after out-of-hospital cardiac arrest (TTM2) trial. Intensive Care Med. 2022;48(8):1024–38. https://doi.org/10.1007/s00134-022-06756-4.
Jiang X, Zhu Y, Zhen S, Wang L. Mechanical power of ventilation is associated with mortality in neurocritical patients: a cohort study. J Clin Monit Comput. 2022;36(6):1621–8. https://doi.org/10.1007/s10877-022-00805-5.
Cinotti R, Mijangos JC, Pelosi P, et al. Extubation in neurocritical care patients: the ENIO international prospective study. Intensive Care Med. 2022;48(11):1539–50. https://doi.org/10.1007/s00134-022-06825-8.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet Lond Engl. 2007;370(9596):1453–7. https://doi.org/10.1016/S0140-6736(07)61602-X.
Ranieri VM, Rubenfeld GD, ARDS Definition Task Force, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–33. https://doi.org/10.1001/jama.2012.5669.
Becher T, van der Staay M, Schädler D, Frerichs I, Weiler N. Calculation of mechanical power for pressure-controlled ventilation. Intensive Care Med. 2019;45(9):1321–3. https://doi.org/10.1007/s00134-019-05636-8.
Giosa L, Busana M, Pasticci I, et al. Mechanical power at a glance: a simple surrogate for volume-controlled ventilation. Intensive Care Med Exp. 2019;7:61. https://doi.org/10.1186/s40635-019-0276-8.
Royston P. Model selection for univariable fractional polynomials. Stata J. 2017;17(3):619–29.
Mrozek S, Constantin JM, Geeraerts T. Brain-lung crosstalk: Implications for neurocritical care patients. World J Crit Care Med. 2015;4(3):163–78. https://doi.org/10.5492/wjccm.v4.i3.163.
Ziaka M, Exadaktylos A. Brain–lung interactions and mechanical ventilation in patients with isolated brain injury. Crit Care. 2021;25(1):358. https://doi.org/10.1186/s13054-021-03778-0.
Kim JA, Wahlster S, LaBuzetta JN, et al. Focused management of patients with severe acute brain injury and ARDS. Chest. 2022;161(1):140–51. https://doi.org/10.1016/j.chest.2021.08.066.
Wright JM, Gerges C, Shammassian B, et al. Prone position ventilation in neurologically Ill patients: a systematic review and proposed protocol. Crit Care Med. 2021;49(3):e269–78. https://doi.org/10.1097/CCM.0000000000004820.
Esteban A, Frutos-Vivar F, Muriel A, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013;188(2):220–30. https://doi.org/10.1164/rccm.201212-2169OC.
Burns KEA, Rizvi L, Cook DJ, et al. Ventilator weaning and discontinuation practices for critically Ill patients. JAMA. 2021;325(12):1173–84. https://doi.org/10.1001/jama.2021.2384.
Tejerina E, Pelosi P, Muriel A, et al. Association between ventilatory settings and development of acute respiratory distress syndrome in mechanically ventilated patients due to brain injury. J Crit Care. 2017;38:341–5. https://doi.org/10.1016/j.jcrc.2016.11.010.
Robba C, Citerio G, Taccone FS, et al. Multicentre observational study on practice of ventilation in brain injured patients: the VENTIBRAIN study protocol. BMJ Open. 2021;11(8):e047100. https://doi.org/10.1136/bmjopen-2020-047100.
Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA. 2012;308(16):1651–9. https://doi.org/10.1001/jama.2012.13730.
Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303(9):865–73. https://doi.org/10.1001/jama.2010.218.
Cavalcanti AB, Suzumura ÉA, Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA. 2017;318(14):1335–45. https://doi.org/10.1001/jama.2017.14171.
Amato MBP, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–55. https://doi.org/10.1056/NEJMsa1410639.
Neto AS, Hemmes SNT, Barbas CSV, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med. 2016;4(4):272–80. https://doi.org/10.1016/S2213-2600(16)00057-6.
De Jong A, Cossic J, Verzilli D, et al. Impact of the driving pressure on mortality in obese and non-obese ARDS patients: a retrospective study of 362 cases. Intensive Care Med. 2018;44(7):1106–14. https://doi.org/10.1007/s00134-018-5241-6.
Gajic O, Dara SI, Mendez JL, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2004;32(9):1817–24. https://doi.org/10.1097/01.ccm.0000133019.52531.30.
Determann RM, Royakkers A, Wolthuis EK, et al. Ventilation with lower tidal volumes as compared with conventional tidal volumes for patients without acute lung injury: a preventive randomized controlled trial. Crit Care Lond Engl. 2010;14(1):R1. https://doi.org/10.1186/cc8230.
Neto AS, Simonis FD, Barbas CSV, et al. Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome: a systematic review and individual patient data analysis. Crit Care Med. 2015;43(10):2155–63. https://doi.org/10.1097/CCM.0000000000001189.
Cressoni M, Gotti M, Chiurazzi C, et al. mechanical power and development of ventilator-induced lung injury. Anesthesiology. 2016;124(5):1100–8. https://doi.org/10.1097/ALN.0000000000001056.
Scharffenberg M, Wittenstein J, Ran X, et al. Mechanical power correlates with lung inflammation assessed by positron-emission tomography in experimental acute lung injury in pigs. Front Physiol. 2021;12:717266. https://doi.org/10.3389/fphys.2021.717266.
Bösel J, Niesen WD, Salih F, et al. Effect of early vs standard approach to tracheostomy on functional outcome at 6 months among patients with severe stroke receiving mechanical ventilation: the SETPOINT2 randomized clinical trial. JAMA. 2022;327(19):1899–909. https://doi.org/10.1001/jama.2022.4798.
McCredie VA, Ferguson ND, Pinto RL, et al. Airway management strategies for brain-injured patients meeting standard criteria to consider extubation. A prospective cohort study. Ann Am Thorac Soc. 2017;14(1):85–93. https://doi.org/10.1513/AnnalsATS.201608-620OC.
Godet T, Chabanne R, Marin J, et al. Extubation failure in brain-injured patients: risk factors and development of a prediction score in a preliminary prospective cohort study. Anesthesiology. 2017;126(1):104–14. https://doi.org/10.1097/ALN.0000000000001379.
Anderson CD, Bartscher JF, Scripko PD, et al. Neurologic examination and extubation outcome in the neurocritical care unit. Neurocrit Care. 2011;15(3):490–7. https://doi.org/10.1007/s12028-010-9369-7.
Steyerberg EW, Vickers AJ, Cook NR, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiol Camb Mass. 2010;21(1):128–38. https://doi.org/10.1097/EDE.0b013e3181c30fb2.
Mansournia MA, Etminan M, Danaei G, Kaufman JS, Collins G. Handling time varying confounding in observational research. BMJ. 2017;359:j4587. https://doi.org/10.1136/bmj.j4587.
Acknowledgements
We would like to thank the collaborators who contributed to the ENIO study as well as all patients. We also thank Mr. Eduardo Nunez and Dr. Aaron Bochner for their advice on the statistical analysis and interpretation.
ENIO Study Group Collaborators
Paër-sélim Abback: Department of Anesthesiology and Critical Care, Beaujon Hospital, DMU Parabol, AP-HP.Nord, 100 Boulevard du General Leclerc, 92100, Clichy, France; Anaïs Codorniu: Department of Anesthesiology and Critical Care, Beaujon Hospital, DMU Parabol, AP-HP.Nord, 100 Boulevard du General Leclerc, 92100, Clichy, France; Giuseppe Citerio: Neurointensive Care Unit, Ospedale San Gerardo, Azienda Socio-Sanitaria Territoriale di Monza, 23 Via Aliprandi, 20900, Monza, Italy; Vittoria Ludovica Sala: NeuroIntensive Care Unit, ASST-Monza via Pergolesi, Monza, Italy; Marinella Astuto: Anesthesia and Intensive Care Unit, A.O.U. Policlinico “G. Rodolico - S. Marco”, Via Santa Sofia 78, Catania, 95123, Italy; Eleonora Tringali: Anesthesia and Intensive Care Unit, A.O.U. Policlinico “G. Rodolico - S. Marco”, Via Santa Sofia 78, Catania, 95123, Italy; Daniela Alampi: Sapienza Rome University, A.O.U. Sant’Andrea, Via di grottarossa,1035/1039, Rome, 00 189, Italy; Monica Rocco: Sapienza Rome University, A.O.U. Sant’Andrea, Via di grottarossa,1035/1039, Rome, 00 189, Italy; Jessica Giuseppina Maugeri: Arnas Garibaldi Catania, Piazza S.Maria di Gesu’ 5, Catania, 95123, Italy; Agrippino Bellissima: Arnas Garibaldi Catania, Piazza S.Maria Di Gesu' 5, Catania, 95123, Italy; Matteo Filippini: University Division of Anesthesiology and Critical Care Medicine, ASST Spedali Civili, Brescia, Italy, Piazzale Spedali Civili, 1 - Brescia, 25123, Italy; Nicoletta Lazzeri: University Division of Anesthesiology and Critical Care Medicine, ASST Spedali Civili, Brescia, Italy, Piazzale Spedali Civili, 1 - Brescia, 25123, Italy; Andrea Cortegiani: Policlinico Paolo Giaccone, Università degli Studi di Palermo, Via del vespro 129, Palermo, 90127, Italy; Mariachiara Ippolito: Policlinico Paolo Giaccone, Università degli Studi di Palermo, Via del vespro 129, Palermo, 90127, Italy; Chiara Robba: San Martino Policlinico Hospital - IRCCS for Oncology and Neurosciences -, 10 Largo Rosanna Benzi, 16100, Genoa, Italy; Denise Battaglini: San Martino Policlinico Hospital - IRCCS for Oncology and Neurosciences -, 10 Largo Rosanna Benzi, 16100, Genoa, Italy; Patrick Biston: CHU Charleroi - Hôpital Civil Marie-Curie, 140 Chaussée de Bruxelles, 6042 Lodelinsart, Charleroi, Belgium; Mohamed Fathi Al-Gharyani: Benghazi Medical Center, Eastern Selmain-Benghazi-Libya, Benghazi, Libya; Russell Chabanne: Clermont-Ferrand University Hospital, Neurocritical Care Unit, Perioperative Medicine Department, 58 rue Montalembert, 63000, Clermont-Ferrand, France; Léo Astier: Clermont-Ferrand University Hospital, Neurocritical Care Unit, Perioperative Medicine Department, 58 rue Montalembert, 63000, Clermont-Ferrand, France; Benjamin Soyer: AP-HP, Hôpital Lariboisière, Department of Anesthesia and Critical Care, DMU Parabol, 2 rue Ambroise Paré, 75010, Paris, France; Samuel Gaugain: AP-HP, Hôpital Lariboisière, Department of Anesthesia and Critical Care, DMU Parabol, 2 rue Ambroise Paré, 75010, Paris, France; Alice Zimmerli: Department of Intensive Care Medicine, Inselspital, Bern University Hospital, University of Bern, Freiburgstrasse, Bern, 3010, Switzerland; Urs Pietsch: Department of Anaesthesiology and Intensive Care Medicine, Cantonal Hospital St Gallen, Rorschacher Strasse 95, 9007, St. Gallen, Switzerland; Miodrag Filipovic: Department of Anaesthesiology and Intensive Care Medicine, Cantonal Hospital St Gallen, Rorschacher Strasse 95, 9007, St. Gallen, Switzerland; Giovanna Brandi: Institute for Intensive Care Medicine, University Hospital of Zurich, Rämistrasse 100, 8091, Zurich, Switzerland; Giulio Bicciato: Institute for Intensive Care Medicine, University Hospital of Zurich, Rämistrasse 100, 8091, Zurich, Switzerland; Ainhoa Serrano: Hospital Clinico Universitario Valencia, Avenida Blasco Ibañez, 17, 46010, Valencia, Spain; Berta Monleon: Hospital Clinico Universitario Valencia, Avenida Blasco Ibañez, 17, 46010, Valencia, Spain; Peter van Vliet: Haaglanden Medical Center, Lijnbaan 32, 2512 VA, The Hague, Netherlands; Benjamin Marcel Gerretsen: Haaglanden Medical Center, Lijnbaan 32, 2512 VA, The Hague, Netherlands; Iris Xochitl Ortiz-Macias: Hospital Civil de Guadalajara “Fray Antonio Alcalde”, Hospital No. 278, Col. El Retiro, 44280, Guadalajara, Mexico; Jun Oto: Tokushima University Hospital, 2-50-1, Kuramoto-cho,Tokushima-shi, Tokushima, 7700042, Japan; Noriya Enomoto: Tokushima Prefectural Central Hospital, 1-10-3, Kuramoto-cho, Tokushima-shi, Tokushima, 7708539, Japan; Tomomichi Matsuda: Sapporo Higashi Tokushukai Hospital, 3-1, Kita 33-jo Higashi 14-chome, Higashi-ku, Sapporo, 0650033, Japan; Nobutaka Masui: Sapporo Higashi Tokushukai Hospital, 3-1, Kita 33-jo Higashi 14-chome, Higashi-ku, Sapporo, 0650033, Japan; Pierre Garçon: Service de Réanimation, 2-4 Cours de la Gondoire, 77600, Jossigny, France; Jonathan Zarka: Service de Réanimation, 2-4 Cours de la Gondoire, 77600, Jossigny, France; Wytze J. Vermeijden: Dep of Intensive Care, Medisch Spectrum Twente MST, 7512 KZ, Enschede, The Netherlands; Alexander Daniel Cornet: Dep of intensive care, Medisch Spectrum Twente MST, 7512 KZ, Enschede, The Netherlands; Sergio Reyes Inurrigarro: UMAE Hospital de Traumatologia y Ortopedia IMSS, Diagonal Defensores de la Republica esquin 6 poniente, 72090, Puebla, Mexico; Rafael Cirino Lara Domínguez: UMAE Hospital de Traumatologia y Ortopedia IMSS, Diagonal Defensores de la Republica esquin 6 poniente, 72090, Puebla, Mexico; Maria Mercedes Bellini: Hospital Maciel, 25 de Mayo 174, 11000, Montevideo, Uruguay; Maria Milagros Gomez Haedo: Hospital Maciel, 25 de Mayo 174, 11000, Montevideo, Uruguay; Laura Lamot: Hospital Municipal Leonidas Lucero, Bahia Blanca, B8000, Buenos Aires, Argentina; Jose Orquera: Sanatorio Pasteur, Chacabuco 675, 4700, Catamarca, Argentina; Matthieu Biais: Pellegrin SAR Tripode, Place Amelie Raba Leon 33076 Bordeaux, France; Delphine Georges: Pellegrin SAR Tripode, Place Amelie Raba Leon 33076 Bordeaux, France; Arvind Baronia: Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGIMS), Lucknow, Department of Critical Care Medicine, Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGIMS), Lucknow, 226014, India; Roberto Carlos Miranda-Ackerman: Hospital San Javier, Av Pablo Casals 640, Prados Providencia, Jalisco, 44670, Guadalajara, Mexico; Francisco José Barbosa-Camacho: Hospital San Javier, Av Pablo Casals 640, Prados Providencia, Jalisco, 44670, Guadalajara, Mexico; John Porter: St George’s Hospital, Blackshaw Road, SW17 0QT, London, United Kingdom; Miguel Lopez-Morales: St George's Hospital, Blackshaw Road, SW17 0QT, London, United Kingdom; Thomas Geeraerts: Toulouse University Hospital, Place du Dr Baylac, F-31059, Toulouse, France; Baptiste Compagnon: Toulouse University Hospital, Place du Dr Baylac, F-31059, Toulouse, France; David Pérez-Torres: Servicio de Medicina Intensiva, Hospital Universitario Río Hortega, Calle Dulzaina, 2, 47012, Valladolid, Spain; Estefanía Prol-Silva: Servicio de Medicina Intensiva, Hospital Universitario Río Hortega, Calle Dulzaina, 2, 47012, Valladolid, Spain; Hana Basheer Yahya: Zliten Medical Centre, Khaam, 218, Zliten, Libya; Ala Khaled: Abo Selim Trauma Hospital, Abo Selim Main, Tripoli, Libya; Mohamed Ghula: Abo Selim Trauma Hospital, Abo Selim Main, Tripoli, Libya; Cracchiolo Neville Andrea: Terapia Intensiva Con Trauma Center, ARNAS Ospedale Civico Palermo, Piazza n Leotta 4, 90127, Italy; Palma Maria Daniela: Terapia Intensiva Con Trauma Center, Arans Ospedale Civico Palermo, Piazza n Leotta 4, 90127o, Italy; Cristian Deana: Academic Hospital of Udine, Piazzale S.Maria della Misericordia, 15, Udine, 33100, Chieti, Italy; Luigi Vetrugno: University of Chieti-Pescara, Via dei Vestini n 33, Chieti, Italy; Manuel J. Rivera Chavez: Hospital de Alta Especialidad del Bajio, Blvd.Milenio #130 Col. San Carlos la Roncha, 37660, Leon, Guanajuato, Mexico; Rocio Mendoza Trujillo: Hospital de Alta Especialidad del Bajio, Blvd.Milenio #130 Col. San Carlos la Roncha, 37660, Leon, Guanajuato, Mexico; Vincent Legros: Department of Anesthesiology and Critical Care, University Hospital of Reims, Hopital Maison Blanche, 45 Rue Cognacq Jay, 51100, Reims, France; Benjamin Brochet: Department of Anesthesiology and Critical Care, University Hospital of Reims, Hopital Maison Blanche, 45 Rue Cognacq Jay, 51100, Reims, France; Olivier Huet: Department of Anesthesiology and Critical Care, La Cavale Blanche, Boulevard Tanguy Prigent, 29200, Brest, France; Marie Geslain: Department of Anesthesiology and Critical Care, La Cavale Blanche, Boulevard Tanguy Prigent, 29200, Brest, France; Mathieu van der Jagt: Erasmus MC Rotterdam, DrMolewaterplein 40, 3015CE, The Netherlands; Job van Steenkiste: Erasmus MC Rotterdam, Dr Molewaterplein 40, 3015CE, Netherlands; Hazem Ahmed: Seoul Clinic, 20th Ramadan Road, Tripoli, Libya; Alexander Edward Coombs: University Hospital Plymouth, Department of Intensive Care Medicine, Derriford Road, PL6 8DH, Plymouth, United Kingdom; Jessie Welbourne: University Hospital Plymouth, Department of Intensive Care Medicine, Derriford Road, PL6 8DH, Plymouth, United Kingdom; Ana Alicia Velarde Pineda: Hospital General Regional # 180 IMSS, Carretera a San Sebastian # 1000 Col. Las cumbres 2 Tlajomulco de Zúñiga, 45650, Guadalajara, Mexico; Víctor Hugo Nubert Castillo: Hospital General Regional # 180 IMSS, Carretera a San Sebastian # 1000 Col. Las cumbres 2 Tlajomulco de Zúñiga, 45650, Guadalajara, Mexico; Mohammed A. Azab: Cairo University, 12613, Cairo, Egypt; Ahmed Y. Azzam: Cairo University, 12613, Cairo, Egypt; David Michael Paul van Meenen: Amsterdam UMC, Meibergdreef 9, 1105AZ, Amsterdam, The Netherlands; Gilberto Adrian Gasca: Hospital Regional de Alta Especialidad de Ixtapaluca, Carretera Federal Mexico -Puebla Km. 34.5, Pueblo de Zoquiapan, 56530, Ixtapaluca, Mexico; Alfredo Arellano: Hospital Regional de Alta Especialidad de Ixtapaluca, Carretera Federal Mexico -Puebla Km. 34.5, Pueblo de Zoquiapan, 56530, Ixtapaluca, Mexico; Forttino Galicia-Espinosa: UMAE Hospital de Traumatología y Ortopedia No 21, IMSS Monterrey, Av. J.M. Pino Suárez S/N esq. 15 de Mayo, 64000, Monterrey, Mexico; José Carlos García-Ramos: UMAE Hospital de Traumatología y Ortopedia No 21, IMSS Monterrey, Av. J.M. Pino Suárez S/N esq. 15 de Mayo, 64000, Monterrey, Mexico; Ghanshyam Yadav: Trauma ICU, Department of Anesthesia, IMS, BHU, 221005, Varanasi, India; Amarendra Kumar Jha: Trauma ICU, Department of Anesthesia, IMS, BHU, 221005, Varanasi, India; Vincent Robert-Edan: Nantes-Laennec, 1 Bd Jacques Monod, 44093, Nantes, France; Pierre-Andre Rodie-Talbere: Nantes-Laennec, 1 Bd Jacques Monod, 44093, Nantes, France; Gaurav Jain: Critical Care Unit, Dept. Of Anaesthesiology and Critical Care, All India Institute of Medical Sciences, Virbhadra Marg, Rishikesh, 249203, Rishikesh, India; Sagarika Panda: Critical Care Unit, Dept. Of Anaesthesiology and Critical Care, All India Institute of Medical Sciences, Virbhadra Marg, Rishikesh, 249203, Rishikesh, India; Sonika Agarwal: HIMS, B18/8, HIMS Campus, 248140, Dehradun, India; Yashbir Deewan: HIMS, B18/8, HIMS Campus, 248140, Dehradun, India; Gilberto Adrian Gasca: Hospital Regional de Alta Especialidad de Ixtapaluca, Carretera Federal Mexico -Puebla Km. 34.5, Pueblo de Zoquiapan, 56530, Ixtapaluca, Mexico; Alfredo Arellano: Hospital Regional de Alta Especialidad de Ixtapaluca, Carretera Federal Mexico -Puebla Km. 34.5, Pueblo de Zoquiapan, 56530, Ixtapaluca, Mexico; Syed Tariq Reza: Dhaka Medical College Hospital, Department of Anaesthesia, Analgesia, Palliative & Intensive Care, Dhaka Medical College Hospital, 1000, Dhaka, Bangladesh; Md. Mozaffer Hossain: Dhaka Medical College Hospital, Department of Anaesthesia, Analgesia, Palliative & Intensive Care, Dhaka Medical College Hospital, 1000, Dhaka, Bangladesh; Christos Papadas: ICU of Asklepieio G.H.A, V.Paulou 1, 16673, Athens, Greece; Vasiliki Chantziara: Saint Savvas Hospital, 151 Alexandras Avenue, 11522, Athens, Greece; Chrysanthi Sklavou: SAINT SAVVAS hospital, 151 Alexandras Avenue, 11522, Athens, Greece; Yannick Hourmant: Department of Anesthesiology and Critical Care, Hôtel-Dieu, 1 Place Alexis Ricordeau, 44093, Nantes, France; Nicolas Grillot: Department of Anesthesiology and Critical Care, Hôtel-Dieu, 1 place Alexis Ricordeau, 44093, Nantes, France; Job van Steenkiste: Erasmus Medical Centre, Doctor Molewaterplein 40, 3015GD, Rotterdam, Netherlands; Mathieu van der Jagt: Erasmus Medical Centre, Doctor Molewaterplein 40, 3015GD, Rotterdam, Netherlands; Romain Pirracchio: Department of Anesthesia and Perioperative Care, University of California, UCSF, 1001 Potrero Ave, CA 94110, San Francisco, United States of America; Abdelraouf Akkari: Qatar-1, HMC-Doha-Qatar, Doha, Qatar; Mohamed Abdelaty: Qatar-2, HMC-Doha-Qatar, Doha, Qatar; Ahmed Hashim: Qatar-2, HMC-Doha-Qatar, Doha, Qatar; Yoann Launey: Department of Anesthesiology and Critical Care, Hopital Pontchaillou, 2 rue Henri le Guilloux, 35000, Rennes, France; Elodie Masseret: Department of Anesthesiology and Critical Care, Hopital Pontchaillou, 2 rue Henri le Guilloux, 35000, Rennes, France; Sigismond Lasocki: Department of Anesthesiology and Critical Care, 4 rue Larrey, 49100, Angers, France; Soizic Gergaud: Department of Anesthesiology and Critical Care, 4 rue Larrey, 49100, Angers, France; Nicolas Mouclier: Department of Anesthesiology and Critical Care, Hôtel-Dieu, 1 place Alexis Ricordeau, 44093, Nantes, France; Sulekha Saxena: King George’s Medical University, Department of Critical Care Medicine, 226014, India; Avinash Agrawal: King George’s Medical University, Department of Critical Care Medicine, 226014, India; Shakti Bedanta Mishra: IMS and SUM Hospital, K8 Kalinga Nagar, 751003, Bhubaneswar, India; Samir Samal: IMS and SUM Hospital, K8 Kalinga Nagar, 751003, Bhubaneswar, India; Julio Cesar Mijangos: Hospital Civil de Guadalajara “Fray Antonio Alcalde” Hospital No. 278, Col. El Retiro, 44280, Guadalajara, Mexico; Mattias Haënggi: Inselspital, Bern University Hospital, Freiburgstrasse, 3010, Bern, Switzerland; Mohan Gurjar: Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGIMS), 226014, Lucknow, India; Marcus J. Schultz: Department of Intensive Care, Amsterdam University Medical Centers, 1105 AZ, Amsterdam, Netherlands; Callum Kaye: Aberdeen Royal Infirmary, Foresthill, AB25 2ZN, Aberdeen, United Kingdom; Daniela Agustin Godoy: Sanatorio Pasteur, Chacabuco 675, 4700, Catamarca, Argentina; Pablo Alvarez: Hospital Maciel, ASSE, Street 25 de Mayo 174, 11000, Montevideo, Uruguay; Aikaterini Ioakeimidou: Asklepieio G.H.A, V.Paulou 1, 16673, Athens, Greece; Yoshitoyo Ueno: Tokushima University Hospital, 2-50-1, Kuramotocho, 7700042, Tokushima, Japan; Rafael Badenes: Hospital Clínico Universitario Valencia, Valencia, Spain; Abdurrahmaan Ali Suei Elbuzidi: Qatar-1, Hamad Medical Corporation, Doha, Qatar; Michaël Piagnerelli: Hôpital Civil Marie-Curie, Université libre de Bruxelles, 140 Chaussée de Bruxelles, 6042 Lodelinsart, Charleroi, Belgium; Muhammed Elhadi: Faculty of Medicine, University of Tripoli, Furnaj, University road, 13275, Tripoli, Libya; Syed Tariq Reza: Dhaka Medical College Hospital, 1000, Dhaka, Bangladesh; Mohammed Atef Azab: Cairo University, Cairo, Giza, 12613, Egypt; Jean Catherine Digitale: University of California, UCSF, 550 16th St, CA 94158, San Francisco, United States of America; Nicholas Fong: University of California, UCSF 1001 Potrero Ave, CA 94110, San Francisco, United States of America; Ricardo Campos Cerda: Critical Care Unit, Hospital General Regional no. 46, Instituto Mexicano del Seguro Social, 2063 Lazaro Cárdenas Av, 44910, Guadalajara, Mexico; Norma de la Torre Peredo: Critical Care Unit, Hospital General Regional No. 46, Instituto Mexicano del Seguro Social, 2063 Lazaro Cárdenas Av, 44910, Guadalajara, Mexico.
Funding
The authors received no direct funding for this work. SW is supported by institutional research grants and the National Institutes of Health. MS receives support from NIMH K01MH115789. ST is supported by the Eliot Phillipson Clinician Scientist Training Program and Clinician Investigator Program at the University of Toronto. RDS is supported on NIA R33AG071744.
Author information
Authors and Affiliations
Consortia
Contributions
SW and CR had full access to all of the data for this analysis, and take responsibility for the integrity of the data and the accuracy of the data analysis. RC and KA designed and oversaw the parent trial (ENIO). All authors contributed substantially to the study design, analysis, as well as interpretation of this analysis. MS and ST performed the statistical analysis, with input from SW, JAT and CR. SW, MS, and CR wrote the manuscript and all authors edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants centers were required to obtain regional or national ethics/institutional review board approval to participate in the parent study (ENIO, NCT03400904). The study was approved by the Steering Committee, no further IRB approval was necessary for the present analysis (which is a sub-analysis of the parent trial).
Consent for publication
Not applicable. We do not report any individual or identifiable patient data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Appendix.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wahlster, S., Sharma, M., Taran, S. et al. Utilization of mechanical power and associations with clinical outcomes in brain injured patients: a secondary analysis of the extubation strategies in neuro-intensive care unit patients and associations with outcome (ENIO) trial. Crit Care 27, 156 (2023). https://doi.org/10.1186/s13054-023-04410-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04410-z