Abstract
Background
Although glucose has a well-recognized protumoral role and the pancreas is a critical organ in adjusting glucose metabolism, the clinical value of hyperglycemia in pancreatic neuroendocrine neoplasms (pNENs) remains largely unidentified.
Methods
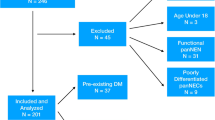
A retrospective study including 335 patients with pathologically confirmed pNENs was conducted. A baseline fasting blood glucose concentration ≥5.6 mmol/L was defined as hyperglycemia (otherwise, normal). Survival and regression analyses were performed.
Results
Compared with patients with normal glucose, patients with hyperglycemia (47.8%) had a higher proportion of preexisting diabetes mellitus (DM) (36.9% vs. 4.6%, p < 0.001), lymph node involvement (31.0% vs. 14.6%, p = 0.002), distant metastasis (34.4% vs. 22.9%, p = 0.019), and carbohydrate antigen 19-9 (CA19-9) ≥ 37 U/mL (16.6% vs. 7.2%, p = 0.009). Hyperglycemia was associated with CA19-9 ≥ 37 U/mL (Odds Ratio (OR) = 3.19, 95% CI: 1.11–9.17, p = 0.031), lymph node involvement (OR = 2.32, 95% CI: 1.02–5.28, p = 0.045), nonfunctional tumors (OR = 9.90, 95% CI: 2.11–46.34, p = 0.004), and preexisting diabetes (OR = 18.24, 95% CI: 4.06–81.95, p < 0.001). Hyperglycemia was an independent determinant for overall survival in the multivariate analysis (hazard ratio (HR) = 2.65, 95% CI: 1.31–5.34, p = 0.006).
Conclusion
Hyperglycemia is an independent predictor of overall survival and is associated with preexisting DM or lymphatic metastasis in patients with pNENs. Patients with hyperglycemia and resectable pNENs may benefit from radical resection with dissection of regional lymph nodes.



Similar content being viewed by others
References
J.C. Yao, et al., One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J. Clin. Oncol.: Off. J. Am. Soc. Clin. Oncol. 26(18), 3063–72 (2008). https://doi.org/10.1200/JCO.2007.15.4377
A.K. Lam, H. Ishida, Pancreatic neuroendocrine neoplasms: Clinicopathological features and pathological staging. Histol. Histopathol. 36(4), 367–382 (2021). https://doi.org/10.14670/HH-18-288
H. Ishida, A. K. Lam, Pancreatic neuroendocrine neoplasms: The latest surgical and medical treatment strategies based on the current World Health Organization classification. Crit. Rev. Oncol. Hematol. 145,102835 (2020). https://doi.org/10.1016/j.critrevonc.2019.102835
R.E. Rosenblum et al. Predictors of recurrence and survival in patients with surgically resected pancreatic neuroendocrine tumors. Pancreas 49(2), 249–254 (2020). https://doi.org/10.1097/MPA.0000000000001477
W.Q. Wang et al. A novel risk factor panel predicts early recurrence in resected pancreatic neuroendocrine tumors. J. Gastroenterol. 56(4), 395–405 (2021). https://doi.org/10.1007/s00535-021-01777-0
J.D. Mizrahi, R. Surana, J.W. Valle, R.T. Shroff, Pancreatic cancer. Lancet 395(10242), 2008–2020 (2020). https://doi.org/10.1016/S0140-6736(20)30974-0
G. Luo, K. Jin, S. Deng, H. Cheng, Z. Fan, Y. Gong, Y. Qian, Q. Huang, Q. Ni, C. Liu, X. Yu, Roles of CA19-9 in pancreatic cancer: Biomarker, predictor and promoter. Biochim. Biophys Acta Rev. Cancer 1875(2), 188409 (2021). https://doi.org/10.1016/j.bbcan.2020.188409. Reviews on cancer
T. Feola, G. Puliani, F. Sesti, R. Modica, R. Centello, R. Minotta, G. Cannavale, S. Di Meglio, V. Di Vito, R. Lauretta, M. Appetecchia, A. Colao, A. Lenzi, A.M. Isidori, A. Faggiano, E. Giannetta, Risk factors for gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs): a three-centric case-control study. J. Endocrinol. Invest. 45(4), 849–857 (2022). https://doi.org/10.1007/s40618-021-01715-0
M. Gallo, R.M. Ruggeri, G. Muscogiuri, G. Pizza, A. Faggiano, A. Colao, N. Group, Diabetes and pancreatic neuroendocrine tumours: Which interplays, if any? Cancer Treat. Rev. 67,1–9 (2018). https://doi.org/10.1016/j.ctrv.2018.04.013
E. Leoncini, G. Carioli, C. La Vecchia, S. Boccia, G. Rindi, Risk factors for neuroendocrine neoplasms: a systematic review and meta-analysis. Ann. Oncol.: Off. J. Eur. Soc. Med. Oncol. 27(1), 68–81 (2016). https://doi.org/10.1093/annonc/mdv505
X. Zhuge, Y. Wang, X. Chen, C. Guo, Diabetes in patients with pancreatic neuroendocrine neoplasms. Front Endocrinol. 11, 615082 (2020). https://doi.org/10.3389/fendo.2020.615082
L. de Mestier, A.L. Vedie, M. Faron, J. Cros, V. Rebours, O. Hentic, C. Do Cao, P. Bardet, P. Levy, A. Sauvanet, P. Ruszniewski, P. Hammel, The postoperative occurrence or worsening of diabetes mellitus may increase the risk of recurrence in resected pancreatic neuroendocrine tumors. Neuroendocrinology 110(11–12), 967–976 (2020). https://doi.org/10.1159/000505158
Y. Gong, Z. Fan, P. Zhang, Y. Qian, Q. Huang, S. Deng, G. Luo, H. Cheng, K. Jin, Q. Ni, X. Yu, C. Liu, High pre-operative fasting blood glucose levels predict a poor prognosis in patients with pancreatic neuroendocrine tumour. Endocrine 71(2), 494–501 (2021). https://doi.org/10.1007/s12020-020-02469-0
G. Muscogiuri, B. Altieri, M. Albertelli, A. Dotto, R. Modica, L. Barrea, G. Fanciulli, T. Feola, R. Baldelli, R.M. Ruggeri, M. Gallo, V. Guarnotta, P. Malandrino, E. Messina, M.A. Venneri, E. Giannetta, D. Ferone, A. Colao, A. Faggiano; N. group, Epidemiology of pancreatic neuroendocrine neoplasms: a gender perspective. Endocrine 69(2), 441–450 (2020). https://doi.org/10.1007/s12020-020-02331-3
G. Luo, C. Liu, M. Guo, H. Cheng, Y. Lu, K. Jin, L. Liu, J. Long, J. Xu, R. Lu, Q. Ni, X. Yu, Potential biomarkers in lewis negative patients with pancreatic cancer. Ann. Surg. 265(4), 800–805 (2017). https://doi.org/10.1097/SLA.0000000000001741
G. Luo et al. Modified Staging Classification for Pancreatic Neuroendocrine Tumors on the Basis of the American Joint Committee on Cancer and European Neuroendocrine Tumor Society Systems. J. Clin. Oncol.: Off. J. Am. Soc. Clin. Oncol. 35(3), 274–280 (2017). https://doi.org/10.1200/JCO.2016.67.8193
I.D. Nagtegaal, R.D. Odze, D. Klimstra, V. Paradis, M. Rugge, P. Schirmacher, K.M. Washington, F. Carneiro, I.A. Cree; W.H.O.C.o.T.E. Board, The 2019 WHO classification of tumours of the digestive system. Histopathology 76(2), 182–188 (2020). https://doi.org/10.1111/his.13975
C. American Diabetes Association Professional Practice, 2, Classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diabetes Care 45(Suppl 1), S17–S38 (2022). https://doi.org/10.2337/dc22-S002
S. Bose, A. Le, Glucose metabolism in cancer. Adv Exp Med Biol. 10633, 3–12 (2018). https://doi.org/10.1007/978-3-319-77736-8_1
N. Hay, Reprogramming glucose metabolism in cancer: can it be exploited for cancer therapy? Nat. Rev. Cancer 16(10), 635–49 (2016). https://doi.org/10.1038/nrc.2016.77
M. Elgendy et al. Combination of hypoglycemia and metformin impairs tumor metabolic plasticity and growth by modulating the PP2A-GSK3beta-MCL-1 axis. Cancer cell 35(5), 798–815 e5 (2019). https://doi.org/10.1016/j.ccell.2019.03.007
G.W. Krampitz, J.A. Norton, G.A. Poultsides, B.C. Visser, L. Sun, R.T. Jensen, Lymph nodes and survival in pancreatic neuroendocrine tumors. Arch. Surg. 147(9), 820–7 (2012). https://doi.org/10.1001/archsurg.2012.1261
X.F. Zhang, F. Xue, D.H. Dong, A.G. Lopez-Aguiar, G. Poultsides, E. Makris, F. Rocha, Z. Kanji, S. Weber, A. Fisher, R. Fields, B.A. Krasnick, K. Idrees, P.M. Smith, C. Cho, M. Beems, Y. Lv, S.K. Maithel, T.M. Pawlik, New nodal staging for primary pancreatic neuroendocrine tumors: a multi-institutional and national data analysis. Ann. Surg. 274(1), e28–e35 (2021). https://doi.org/10.1097/SLA.0000000000003478
Y.M. Hashim, K.M. Trinkaus, D.C. Linehan, S.S. Strasberg, R.C. Fields, D. Cao, W.G. Hawkins, Regional lymphadenectomy is indicated in the surgical treatment of pancreatic neuroendocrine tumors (PNETs). Ann. Surg. 259(2), 197–203 (2014). https://doi.org/10.1097/SLA.0000000000000348
Z. Zhang, M. Liu, S. Ji, G. Luo, W. Xu, W. Liu, Q. Hu, Q. Sun, Z. Ye, Y. Qin, G. Fan, X. Yu, X. Xu, Prognostic value and clinical predictors of lymph node metastases in pancreatic neuroendocrine tumors. Pancreas 49(3), 381–386 (2020). https://doi.org/10.1097/MPA.0000000000001493
G. Luo, K. Jin, H. Cheng, C. Liu, M. Guo, Y. Lu, C. Yang, J. Xu, W. Wang, H. Gao, S. Zhang, J. Long, J. Xu, Q. Ni, J. Chen, X. Yu, Carbohydrate antigen 19-9 as a prognostic biomarker in pancreatic neuroendocrine tumors. Oncol. Lett. 14(6), 6795–6800 (2017). https://doi.org/10.3892/ol.2017.7071
L. Chen, Y. Zhang, M. Chen, J. Chen, Prognostic value of carcinoembryonic antigen, alpha fetoprotein, carbohydrate antigen 125 and carbohydrate antigen 19-9 in gastroenteropancreatic neuroendocrine neoplasms. Chin. J. Gastrointest. Surg. 20(9), 1002–1008 (2017)
J. Murai, S. Soga, H. Saito, M. Otsuki, T. Kitada, Y. Saisho, H. Nakamura, S. Kasayama, M. Koga, Study on the mechanism causing elevation of serum CA19-9 levels in diabetic patients. Endocr. J. 60(7), 885–91 (2013). https://doi.org/10.1507/endocrj.ej12-0364
H. Yu, R. Li, L. Zhang, H. Chen, Y. Bao, W. Jia, Serum CA19-9 level associated with metabolic control and pancreatic beta cell function in diabetic patients. Exp. Diabetes Res. 2012, 745189 (2012). https://doi.org/10.1155/2012/745189
S.H. Kim, C.O. Baek, K.A. Lee, T.S. Park, H.S. Baek, H.Y. Jin, Clinical implication of elevated CA 19-9 level and the relationship with glucose control state in patients with type 2 diabetes. Endocrine 46(2), 249–55 (2014). https://doi.org/10.1007/s12020-013-0058-0
Z. Fan, Y. Gong, Q. Huang, C. Yang, H. Cheng, K. Jin, K. Fan, Q. Ni, X. Yu, G. Luo, C. Liu, Diabetes is associated with the metastasis of pancreatic neuroendocrine tumors. Pancreas 49(6), 751–756 (2020). https://doi.org/10.1097/MPA.0000000000001564
S. Pusceddu et al. Metformin with everolimus and octreotide in pancreatic neuroendocrine tumor patients with diabetes. Future Oncol. 12(10), 1251–60 (2016). https://doi.org/10.2217/fon-2015-0077
S. Pusceddu et al. Impact of diabetes and metformin use on enteropancreatic neuroendocrine tumors: post hoc analysis of the CLARINET study. Cancers 14(1), 69 (2021). https://doi.org/10.3390/cancers14010069
S. Pusceddu et al. Metformin use is associated with longer progression-free survival of patients with diabetes and pancreatic neuroendocrine tumors receiving everolimus and/or somatostatin analogues. Gastroenterology 155(2), 479–489 e7 (2018). https://doi.org/10.1053/j.gastro.2018.04.010
N. Sadeghi, J.L. Abbruzzese, S.C. Yeung, M. Hassan, D. Li, Metformin use is associated with better survival of diabetic patients with pancreatic cancer. Clin. Cancer Res.: Off. J. Am. Assoc. Cancer Res. 18(10), 2905–12 (2012). https://doi.org/10.1158/1078-0432.CCR-11-2994
Acknowledgements
We would like to thank American Journal Experts (www.aje.com) for English language editing.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers 81625016, 81871940, 81902417), the Scientific Innovation Project of Shanghai Education Committee (2019-01-07-00-07-E00057), Clinical and Scientific Innovation Project of Shanghai Hospital Development Center (SHDC12018109), the Shanghai Natural Science Foundation (grant number 17ZR1406300), the Shanghai Cancer Center Foundation for Distinguished Young Scholars (grant number YJJQ201803), and the Fudan University Personalized Project for “Double Top” Original Research (grant number XM03190633).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. G.L. and X.Y.: conceptualization and funding acquisition. P.Z., Z.X., and H.X.: resources and investigation and data curation. G.L. and X.Y.: project administration. G.L. and Q.N.: review and editing. P.Z., Z.X., and H.X.: formal analysis and software and writing—original draft. All authors read and approved the final paper.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The study was approved by the Institutional Review Board of Fudan University Shanghai Cancer Center.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, P., Xiao, Z., Xu, H. et al. Hyperglycemia is associated with adverse prognosis in patients with pancreatic neuroendocrine neoplasms. Endocrine 77, 262–271 (2022). https://doi.org/10.1007/s12020-022-03100-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03100-0