Abstract
Background
Although total hip arthroplasty (THA) is a successful procedure, 4% to 11% of patients who undergo THA are readmitted to the hospital. Prior studies have reported rates and risk factors of THA readmission but have been limited to single-center samples, administrative claims data, or Medicare patients. As a result, hospital readmission risk factors for a large proportion of patients undergoing THA are not fully understood.
Questions/purposes
(1) What is the incidence of hospital readmissions after primary THA and the reasons for readmission? (2) What are the risk factors for hospital readmissions in a large, integrated healthcare system using current perioperative care protocols?
Methods
The Kaiser Permanente (KP) Total Joint Replacement Registry (TJRR) was used to identify all patients with primary unilateral THAs registered between January 1, 2009, and December 31, 2011. The KPTJRR’s voluntary participation is 95%. A logistic regression model was used to study the relationship of risk factors (including patient, clinical, and system-related) and the likelihood of 30-day readmission. Readmissions were identified using electronic health and claims records to capture readmissions within and outside the system. Odds ratio (OR) and 95% confidence intervals (CIs) were calculated. Of the 12,030 patients undergoing primary THAs included in the study, 59% (n = 7093) were women and average patient age was 66.5 years (± 10.7).
Results
There were 436 (3.6%) patients with hospital readmissions within 30 days of the index procedure. The most common reasons for readmission were infection and inflammatory reaction resulting from internal joint prosthetic (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM] 996.66, 7.0%); other postoperative infection (ICD-9-CM 998:59, 5.5%); unspecified septicemia (ICD-9-CM 038.9, 4.9%); and dislocation of a prosthetic joint (ICD-9-CM 996.42, 4.7%). In adjusted models, the following factors were associated with an increased likelihood of 30-day readmission: medical complications (OR, 2.80; 95% CI, 1.59-4.93); discharge to facilities other than home (OR, 1.89; 95% CI, 1.39–2.58); length of stay of 5 or more days (OR, 1.80; 95% CI, 1.22–2.65) versus 3 days; morbid obesity (OR, 1.74; 95% CI, 1.25–2.43); surgeries performed by high-volume surgeons compared with medium volume (OR, 1.53; 95% CI, 1.14–2.08); procedures at lower-volume (OR, 1.41; 95% CI, 1.07–1.85) and medium-volume hospitals (OR, 1.81; 95% CI, 1.20–2.72) compared with high-volume ones; sex (men: OR, 1.51; 95% CI, 1.18–1.92); obesity (OR, 1.32; 95% CI, 1.02–1.72); race (black: OR, 1.26; 95% CI, 1.02–1.57); increasing age (OR, 1.03; 95% CI, 1.01–1.04); and certain comorbidities (pulmonary circulation disease, chronic pulmonary disease, hypothyroidism, and psychoses).
Conclusions
The 30-day hospital readmission rate after primary THA was 3.6%. Modifiable factors, including obesity, comorbidities, medical complications, and system-related factors (hospital), have the potential to be addressed by improving the health of patients before this elective procedure, patient and family education and planning, and with the development of high-volume centers of excellence. Nonmodifiable factors such as age, sex, and race can be used to establish patient and family expectations regarding risk of readmission after THA. Contrary to other studies and the finding of increased hospital volume associated with lower risk of readmission, higher volume surgeons had a higher risk of patient readmission, which may be attributable to the referral patterns in our organization.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Introduction
In 2013, healthcare spending within the United States reached USD 2.9 trillion and accounted for 18% of the national gross domestic product [8]. With an aging population and an estimated 30 million Americans newly insured through the Affordable Healthcare Act, increased cumulative spending is projected to reach USD 5 trillion by 2022 [8]. Medicare hospital readmissions accounted for USD 12 billion in spending and an estimated 76% of patient readmissions are potentially preventable [19, 20]. Increasingly, payers and providers are recognizing the need to prevent complications, address increasing demand, lower costs, and improve quality of care.
Within orthopaedics, the Centers for Medicare & Medicaid Services has focused on 30-day readmissions after elective total joint arthroplasty (TJA) as a quality indicator and has initiated a “no pay” policy for readmissions after these procedures [18, 29]. Although THA is an effective, high-volume procedure [11, 12, 15], 4% to 10.9% of patients are readmitted to the hospital after the procedure [5, 7, 30, 32–34]. Reported patient risk factors for readmission after THA include age, male sex, black race, weight (obese and underweight status), diabetic status, cardiac disease, patient comorbidities, general health status, longer hospital length of stay (LOS), discharge disposition, revision procedures, distance between hospital and home, and insurance coverage status [2, 5, 13, 26–28, 30, 31, 34].
Although prior studies have reported rate and risk factors of THA readmission, the findings have been limited as a result of single-center samples or reliance on administrative claims data. Single-center studies are usually undersized in samp le, lack the capability to capture readmissions outside their specific hospital system, and produce results that are not generalizable to other hospital settings. Medicare studies are also constrained because they are based on administrative claims databases with limited patient and clinical information. In addition, Medicare studies are restricted to patients aged 65 years and older. This is particularly important given that almost one-third of patients undergoing THA are younger than 65 years and constitute the fastest growing group in arthroplasty demand [16, 33]. A review of the literature on patient readmissions after THA shows that most previous US-based studies have been done at single institutions or use administrative data (Table 1). As a result, readmission risk factors for a large segment of the TJA population are not well understood.
Therefore, the purpose of our study was to examine the rate of hospital readmissions after primary THA as well as the reasons for readmission and the modifiable and nonmodifiable risk factors for hospital readmissions in a large, integrated healthcare system using current perioperative care protocols.
Materials and Methods
Kaiser Permanente’s (KP) Total Joint Replacement Registry (TJRR) was used to identify the study cohort [21, 23]. Kaiser Permanente is an integrated healthcare system that serves over nine million patients in seven geographical regions throughout the United States. Three of the eight regions (northern California, southern California, and Hawaii) participating in the Registry were used in our study; the three regions included 32 KP hospitals with patients from 176 surgeons. These regions were included because they share a common inpatient and outpatient electronic health record system and the majority of cases took place at KP hospitals. Non-KP hospitals were excluded from the analysis because a different inpatient electronic health record was used at these facilities during the study period and therefore complete information necessary to conduct this study was not available from these locations.
Inclusion criteria included primary unilateral THA for osteoarthritis and age 18 years or older during the time period from January 1, 2009, to December 31, 2011. Patients undergoing revisions or bilateral primary THAs were not included in the study. Individuals who died or terminated membership within 30 days of the operative date without a readmission during the same timeframe were also excluded and considered lost to followup (n = 36 [0.3%]). The KPTJRR’s voluntary participation is 95%. Readmissions were captured for all individuals who remain members using the comprehensive electronic health and claims records, which identify visits within and outside the KP system.
Patient, procedure, surgeon, and hospital variables were evaluated as risk factors for readmission. Patient-specific risk factors included: age (continuous); sex; race (white, black, Hispanic, Asian, other); body mass index (BMI; nonobese BMI < 30 kg/m2; obese BMI 30–34 kg/m2; morbidly obese BMI ≥ 35 kg/m2); American Society of Anesthesiologists (ASA) score (< 3 versus ≥ 3) [9]; comorbidities (determined using the Elixhauser comorbidity algorithm) [10]; in-hospital medical complications (including pneumonia, acute myocardial infarction, and acute stroke); and in-hospital surgical complications (including surgery and implant-related). The Agency for Healthcare Research and Quality Inpatient Quality Indicators Technical Specifications were used to identify in-hospital complications (Appendix 1; supplemental materials are available with the online version of CORR®) [1]. Procedure variables evaluated included discharge disposition (home versus other) and LOS (categorized into ≤ 2, ≤ 3, ≤ 4, and ≥ 5 days). Surgeon-related variables included whether the surgeon had a TJA fellowship and the surgeon’s average yearly volume of procedures performed (categorized as: low = < 20 cases/year, medium = 20–49 cases/year, or high = ≥ 50 cases/year). Hospital volume was also evaluated (categorized as: low = < 100 cases/year, medium = 100–199 cases/year, or high = ≥ 200 cases/year). Average surgeon and hospital yearly volumes were calculated using both primary and revision procedures (continuous) performed during the calendar year.
The endpoint of our study was any inpatient hospital readmission within 30 days of discharge after the hospital stay associated with patient index primary THA. The information was obtained from patient electronic medical records maintained by the healthcare system.
Means (SDs, frequencies, and proportions) were used to describe the study patient sample. If a different distribution was observed in readmission rates by the sample characteristics (p < 0.20), the risk factor was included in the final multivariate models. Collinearity was checked using tolerance values (< 0.1), outliers were reviewed, and model fit was checked using goodness-of-fit tests. A logistic regression, through a generalized linear model, was used to evaluate the relationship between 30-day readmission and the risk factors studied while accounting for the nesting of observations within the hospital variable. Crude and adjusted estimates of likelihood of readmission for each risk factor were provided. Odds ratio (OR), 95% confidence interval (CI), and p values based on a Wald test were reported. Missing data were minimal in the data set and cases with missing data (n = 215 [1.8%]) were excluded from the final model; variables with missing values are as specified in all tables. All tests were two-tailed, and α = 0.05 was considered statistically significant. Data were analyzed using SAS (Version 9.2; SAS Institute, Cary, NC, USA).
Of the 12,030 primary THAs included in our study, 59% (n = 7093) were performed in women. The average age of all patients in the cohort was 66.5 (SD = 10.7) years. Most patients had an ASA score less than or equal to 2 (n = 7507 [62%]) at the time of surgery. Prevalence of patient obesity (BMI ≥ 30 kg/m2) was 40% (n = 4836) and of diabetes was 19% (n = 2271; Table 2). Most patients had at least one comorbidity (n = 10,052 [84%]) with the most prevalent comorbidities being hypertension (n = 7308 [61%]), chronic pulmonary disease (n = 1794 [15%]), hypothyroidism (n = 1627 [14%]), and deficiency anemia (n = 1449 [12%]). The majority of THAs were performed in medium-volume hospitals (n = 7854 [65%]) by medium-volume surgeons (n = 6425 [53%]; Table 3). Patients’ average LOS was 2.9 (± 1.5) days, and 79% (n = 9455) were discharged home after their procedure. There were 580 (4.8%) surgical complications and 89 (0.7%) medical complications in our study cohort during the hospital stay associated with the index operation.
Results
Incidence of and Reasons for Hospital Readmissions After Primary THA
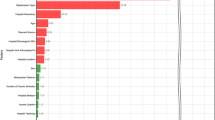
There were 436 (3.6%) patients with 471 total readmissions (some patients had multiple readmissions) within 30 days of the index procedure. The readmission rate in patients aged 65 and older was 4.6%. The most common reasons for readmission were infection and inflammatory reaction resulting from internal joint prosthesis (International Classification of Diseases, 9th Revision, Clinical Modifications [ICD-9-CM] 996.66; n = 33 of 471 [7.0%]), other postoperative infection (ICD-9-CM 998:59; n = 26 of 471 [5.5%]), unspecified septicemia (ICD-9-CM 038.9; n = 23 of 471 [4.9%]), dislocation of a prosthetic joint (ICD-9-CM 996.42; n = 22 of 471 [4.7%]), and a hematoma complicating the procedure (ICD-9-CM 998.12; n = 19 of 471 [4.0%]) (Appendix 2; supplemental materials are available with the online version of CORR®).
Risk Factors for Hospital Readmissions
After adjusting for all other variables, age, sex, race, BMI, surgeon volume, hospital volume, discharge disposition, medical complications, LOS at the index procedure, and comorbidities were associated with patient risk of 30-day readmission (Table 4). Specifically, for every added year in patient age, their likelihood of 30-day readmission was 3% higher (95% CI, 1–4). Men were 51% (95% CI, 18–92) more likely to be readmitted than women. Black patients had a 26% (95% CI, 2–57) higher likelihood of readmission than white patients. Obese patients had a 32% (95% CI, 2–72) higher likelihood of readmission than nonobese patients. Morbidly obese patients had a 74% (95% CI, 25–143) higher likelihood of readmission than nonobese patients. Patients who had their surgeries performed by medium-volume surgeons had a 35% (95% CI, 12–52) lower likelihood of readmission than those operated on by high-volume surgeons; patients of low-volume compared with high-volume surgeons did not have a different risk of readmission (OR, 0.74; 95% CI, 0.48–1.14). Patients who had procedures at lower volume hospitals had a 41% (95% CI, 7–85) higher risk of readmission and those at medium-volume had a 81% (95% CI, 20–172) higher risk of readmission than those at high-volume hospitals.
Patients with medical complications during index THA had a 180% (95% CI, 59–393) higher risk of readmission and those discharged to other facilities instead of to home had a 89% (95% CI, 39–158) higher likelihood of readmission. Patients with a LOS of 5 or more days were 80% (95% CI, 22–165) more likely to be readmitted than those with a LOS of 3 days. Patients with pulmonary circulation disease (OR, 1.7; 95% CI, 1.08–2.70), chronic pulmonary disease (OR, 1.27; 95% CI, 1.08–1.48), hypothyroidism (OR, 1.31; 95% CI, 1.06–1.63), or psychoses (OR, 1.32; 95% CI, 1.03–1.69) had a higher likelihood of readmission compared with patients without these comorbidities.
Discussion
In a large cohort of patients undergoing primary THA in a US integrated healthcare system, the overall 30-day hospital readmission rate was 3.6%. Unlike prior US studies, our findings were based on prospective data collection and complete capture of hospital readmissions with a known minimal loss to followup. Our sample also included patients younger than age 65 years, who are more representative of the general US THA population. The large sample size, taken over a contemporary time period, more closely reflects current perioperative management of patients undergoing THA. Risk factors of hospital readmission included patient, surgeon, and hospital factors—specifically, age, sex (men), race (black), BMI (> 35 kg/m2), surgeon volume (high), hospital volume (low), discharge disposition (other than home), medical complications during the index THA hospitalization, LOS of the index procedure (> 4 days), and some comorbidities that were associated with likelihood of 30-day hospital readmission. Infection was the most common reason for readmission.
The study’s limitations include findings restricted to the US geographic area inclusion criterion (northern California, southern California, and Hawaii). Another limitation was the use of the ICD-9 codes to identify the reason for hospital readmissions. Keeney et al reported 79% of ICD-9 total joint arthroplasty 90-day readmission. ICD-9 diagnostic codes were in moderate concordance with diagnosis documented in the medical record [14]. Although medical diagnoses were more reliable, ICD-9 codes related to surgical site infection were the least reliable [14]. Similarly, Saucedo et al reported discordance rates of 25% for total joint arthroplasty readmission diagnoses based on ICD-9 codes versus physician reviewed diagnoses [25]. Bozic et al reported similar limitations in ICD-9 codes for revision total hip arthroplasty with good concordance for dislocation, periprosthetic joint infection, and mechanical loosening but low concordance for prosthetic implant failure/breakage and other mechanical complication [3]. Limitations of ICD-9 codes for specific diagnoses must be taken into account when interpreting findings based on administrative claims codes. The 30-day all-cause hospital readmission rates in our study were lower than those reported in other studies [5, 6, 17, 24, 30, 32, 33]. This lower rate may reflect differences in case complexity or indications for the index THA. Differences may also be related to the integrated nature of the organization’s healthcare delivery model and quality improvement initiatives in arthroplasty management supported by the organization [22]. Understanding the reasons for readmissions and patients at risk for these problems is critical for reducing hospital readmissions. The most common reasons for readmission in our study were infection, hematomas, and wound complications. As a result, we developed patient risk calculators for patients and surgeons to identify individualized patient risk of infection for treatment decision-making to identify which patients are at risk for infection to improve on their medical conditions before surgery where it was possible to do so and to set patient expectations based on their own personal risk profile. In addition to personalized risk factors, patients are also managed with standardized preoperative infection control protocols to further reduce risk of infection.
In evaluating 30-day hospital readmissions, our study identified both modifiable and nonmodifiable readmission risk factors. Modifiable risk factors such as BMI can be addressed before surgery through referral to weight management programs and reduction in BMI. Patients with comorbidities such as pulmonary disease, hypothyroidism, and psychoses often can be improved on preoperatively through medical management of these conditions. Within our system, patients’ laboratory results, comorbidities, and other risk factors for poor outcomes are identified preoperatively and managed by care managers to reduce patient risk. For patients with medical complications during the surgery or index hospital stay, LOS and followup must be closely monitored to reduce the risk of readmission. Hospital and surgeon system factors are also critical and modifiable. Our study found higher hospital volume was associated with lower readmission rates. This suggests high-volume centers such as centers of excellence, which are currently in development in one of our regions, is a potential way to reduce these events from occurring. Contrary to other studies and somewhat counterintuitive given our findings of increased hospital volume associated with lower risk of readmission, we also found that higher volume surgeons had a higher risk of patient readmission [4]. This may be partly attributable to the referral patterns in our organization. In a group medical practice environment, it is possible that complex cases are channeled to high-volume hip specialists, resulting in the observed finding. Differences in volume and readmission findings may result from definitions and/or cutoff points in high- and low-volume surgery, variation in hospital settings, differences in study samples, or other factors. Identification of nonmodifiable risk factors in this study such as age, race, and gender are also important in providing information to patients and surgeons that may determine LOS, set patient expectations, and improve followup care.
The strengths of this study included the assessment of a cohort whose demographic composition was representative of the larger US THA population [22] and the complete capture of rehospitalization data, which has high validity as a result of the prospective nature of the data collection process and the registry’s surveillance of cohort attrition. Furthermore, our study sample was large and had power to investigate clinically meaningful relationships, including those with small effect sizes. The choice of the recent time period, January 1, 2009, to December 31, 2011, implies that the study results reflect current clinical practice and can be relied on for making changes in clinical pathways and/or policy decisions. In conclusion, the 30-day hospital readmission rate after primary THA was 3.6%. Modifiable factors, including obesity, comorbidities, medical complications, and system-related factors (hospital and surgeon volume), have the potential to be addressed by identifying patient-personalized risk of specific adverse events before surgery, improving the health of patients before this elective procedure, enhancing patient and family education and planning based on personalized risk, and developing high-volume centers of excellence. Nonmodifiable factors such as age, sex, and race can be used to help set patient and family expectations before surgery regarding risk of readmission after THA. Future studies are needed to evaluate the success of patient optimization and other interventions to reduce hospital readmissions.
References
Agency for Healthcare Research and Quality. Patient Safety indicator #12, technical specifications: postoperative pulmonary embolism or deep vein thrombosis rate [monograph on the Internet]. Available at: http://www.qualityindicators.ahrq.gov/Downloads/Modules/PSI/V44/TechSpecs/PSI%2012%20Postoperative%20PE%20or%20DVT%20Rate.pdf. Accessed March 1, 2015.
Avram V, Petruccelli D, Winemaker M, de Beer J. Total joint arthroplasty readmission rates and reasons for 30-day hospital readmission. J Arthroplasty. 2013;29:465–468.
Bozic KJ, Chiu VW, Takemoto SK, Greenbaum JN, Smith TM, Jerabek SA, Berry DJ. The validity of using administrative claims data in total joint arthroplasty outcomes research. J Arthroplasty. 2010;25(Suppl):58–61.
Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am. 2010;92:2643–2652.
Clement RC, Derman PB, Graham DS, Speck RM, Flynn DN, Levin LS, Fleisher LA. Risk factors, causes, and the economic implications of unplanned readmissions following total hip arthroplasty. J Arthroplasty. 2013;28(Suppl):7–10.
Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR, Li Y. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA. 2011;305:1560–1567.
Cram P, Lu X, Kates SL, Li Y, Miller BJ. Outliers: hospitals with consistently lower and higher than predicted joint arthroplasty readmission rates. Geriatr Orthop Surg Rehabil. 2011;2:135–147.
Cuckler GA, Sisko AM, Keehan SP, Smith SD, Madison AJ, Poisal JA, Wolfe CJ, Lizonitz JM, Stone DA. National health expenditure projections, 2012–22: slow growth until coverage expands and economy improves. Health Aff (Millwood). 2013;32:1820–1831.
Dripps RD, Lamont A, Eckenhoff JE. The role of anesthesia in surgical mortality. JAMA. 1961;178:261–266.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86:963–974.
Harris WH, Sledge CB. Total hip and total knee replacement (1). N Engl J Med. 1990;323:725–731.
Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res. 2011;470:490–496.
Keeney JA, Adelani MA, Nunley RM, Clohisy JC, Barrack RL. Assessing readmission databases: how reliable is the information? J Arthroplasty. 2012;27(Suppl):72–76.e71–72.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612.
Lavernia CJ, Villa JM, Iacobelli DA. Readmission rates in the state of Florida: a reflection of quality? Clin Orthop Relat Res. 2013;471:3856–3862.
McNair PD, Luft HS, Bindman AB. Medicare’s policy not to pay for treating hospital-acquired conditions: the impact. Health Aff (Millwood). 2009;28:1485–1493.
Medicare Payment Advisory Commission. Report to the Congress: Promoting Greater Efficiency in Medicare. Washington, DC, USA: Medicare Payment Advisory Committee; 2007.
Medicare Report to the Congress. Medicare and the Health Care Delivery System. Washington, DC, USA: Medicare Payment Advisory Committee; 2013.
Paxton EW, Inacio MC, Khatod M, Yue EJ, Namba RS. Kaiser Permanente National Total Joint Replacement Registry: aligning operations with information technology. Clin Orthop Relat Res. 2010;468:2646–2663.
Paxton EW, Kiley ML, Love R, Barber TC, Funahashi TT, Inacio MC. Kaiser Permanente implant registries benefit patient safety, quality improvement, cost-effectiveness. Jt Comm J Qual Patient Saf. 2013;39:246–252.
Paxton EW, Namba RS, Maletis GB, Khatod M, Yue EJ, Davies M, Low RB, Jr., Wyatt RW, Inacio MC, Funahashi TT. A prospective study of 80,000 total joint and 5000 anterior cruciate ligament reconstruction procedures in a community-based registry in the United States. J Bone Joint Surg Am. 2010;92(Suppl 2):117–132.
Pugely AJ, Callaghan JJ, Martin CT, Cram P, Gao Y. Incidence of and risk factors for 30-day readmission following elective primary total joint arthroplasty: analysis from the ACS-NSQIP. J Arthroplasty. 2013;28:1499–1504.
Saucedo J, Marecek GS, Lee J, Huminiak L, Stulberg SD, Puri L. How accurately are we coding readmission diagnoses after total joint arthroplasty? J Arthroplasty. 2013;28:1076–1079.
Saucedo JM, Marecek GS, Wanke TR, Lee J, Stulberg SD, Puri L. Understanding readmission after primary total hip and knee arthroplasty: who’s at risk? J Arthroplasty. 2013;29:256–260.
Schairer WW, Sing DC, Vail TP, Bozic KJ. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res. 2013;472:464–470.
Soohoo NF, Farng E, Lieberman JR, Chambers L, Zingmond DS. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2363–2371.
US Department of Health and Human Services. 45 CFR Parts 160 and 164. Modifications to the HIPAA privacy, security, enforcement, and breach notification rules under the Health Information Technology for Economic and Clinical Health Act and the Genetic Information Nondiscrimination Act; other modifications to the HIPAA rules; final rule. Fed Register. 2013;78:5566–5702.
Vorhies JS, Wang Y, Herndon J, Maloney WJ, Huddleston JI. Readmission and length of stay after total hip arthroplasty in a national Medicare sample. J Arthroplasty. 2011;26(Suppl):119–123.
Voskuijl T, Hageman M, Ring D. Higher Charlson comorbidity index scores are associated with readmission after orthopaedic surgery. Clin Orthop Relat Res. 2014;472:1638–1644.
Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012;94:e103.
Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007;89:526–533.
Zmistowski B, Restrepo C, Hess J, Adibi D, Cangoz S, Parvizi J. Unplanned readmission after total joint arthroplasty: rates, reasons, and risk factors. J Bone Joint Surg Am. 2013;95:1869–1876.
Acknowledgments
We thank all Kaiser Permanente orthopaedic surgeons and the staff of the Department of Surgical Outcomes and Analysis who contributed to the success of the National Total Joint Replacement Registry.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that a waiver of informed consent for the study was obtained.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Paxton, E.W., Inacio, M.C.S., Singh, J.A. et al. Are There Modifiable Risk Factors for Hospital Readmission After Total Hip Arthroplasty in a US Healthcare System?. Clin Orthop Relat Res 473, 3446–3455 (2015). https://doi.org/10.1007/s11999-015-4278-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4278-x