Abstract
Background
Lack of consensus continues regarding the benefit of anteriorly based surgical approaches for primary total hip arthroplasty (THA). The purpose of this study was to evaluate the risk of aseptic revision, septic revision, and dislocations for various approaches used in primary THAs from a community-based healthcare organization.
Questions/purposes
(1) What is the incidence of aseptic revision, septic revision, and dislocation for primary THA in a large community-based healthcare organization? (2) Does the risk of aseptic revision, septic revision, and dislocation vary by THA surgical approach?
Methods
The Kaiser Permanente Total Joint Replacement Registry was used to identify primary THAs performed between April 1, 2001 and December 31, 2011. Endpoints were septic revisions, aseptic revisions, and dislocations. The exposure of interest was surgical approach (posterior, anterolateral, direct lateral, direct anterior). Patient, implant, surgeon, and hospital factors were evaluated as possible confounders. Survival analysis was performed with marginal multivariate Cox models. Hazard ratios (HRs) and 95% confidence intervals (CIs) are reported. A total of 42,438 primary THAs were available for analysis of revision outcomes and 22,237 for dislocation. Median followup was 3 years (interquartile range, 1–5 years). The registry’s voluntary participation is 95%. The most commonly used approach was posterior (75%, N = 31,747) followed by anterolateral (10%, N = 4226), direct anterior (4%, N = 1851), and direct lateral (2%, N = 667).
Results
During the study period 785 hips (2%) were revised for aseptic reasons, 213 (0.5%) for septic reasons, and 276 (1%) experienced a dislocation. The revision rate per 100 years of observation was 0.54 for aseptic revisions, 0.15 for septic revisions, and 0.58 for dislocations. There were no differences in adjusted risk of revision (either septic or aseptic) across the different THA approaches. However, the anterolateral approach (adjusted HR, 0.29; 95% CI, 0.13–0.63, p = 0.002) and direct anterior approach (adjusted HR, 0.44; 95% CI, 0.22–0.87, p = 0.017) had a lower risk of dislocation relative to the posterior approach. There were no differences in any of the outcomes when comparing the direct anterior approach with the anterolateral approach.
Conclusions
Anterior and anterolateral surgical approaches had the advantage of a lower risk of dislocation without increasing the risk of early revision.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Introduction
Modifications of traditional anteriorly based surgical approaches were introduced in the early 2000s to reduce dislocations and facilitate early rehabilitation after surgery [5, 23, 25, 35]. A number of recent studies have compared the newer approaches with traditional lateral and posterior approaches [1, 12, 15, 18, 34, 49] but there is lack of consensus on whether there is any demonstrable difference in reducing muscle damage, improving postoperative gait, or facilitating earlier rehabilitation [21, 29, 38, 41, 42, 46].
The main advantage of anteriorly based approaches has been reduction in the incidence of hip dislocation [14, 43, 45, 51]. However, some studies have expressed concern regarding implant malposition that could compromise long-term survival of the implant [3, 33]. There are other complications of concern, not seen with traditional approaches, such as greater trochanter fracture, canal perforation, and remote site fractures [3, 11, 34, 37, 38]. The learning curve associated with newer approaches may also have negative implications on the results [10, 28, 50]. Only a few studies have specifically evaluated the impact of surgical approach on surgical outcomes including complications and short- and medium-term survivorship [2, 34, 39]. Finally, because most reported studies have been conducted either by single surgeons at a single center or performed in a controlled fashion [1–4, 6, 7], the generalizability of these results to the greater orthopaedic community and patients is limited.
The purpose of our study is to evaluate the risk of aseptic revision, septic revision, and dislocations in the various surgical approaches used for primary THAs performed in the setting of a community-based integrated healthcare system. Specifically, we asked: (1) What is the incidence of aseptic revision, septic revision, and dislocation in primary THA in a large community-based healthcare organization? (2) Does the risk of aseptic revision, septic revision, and dislocation vary by THA surgical approach?
Materials and Methods
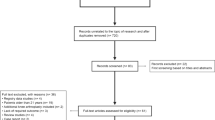
A retrospective analysis of a prospectively followed cohort was conducted. A total joint replacement registry (Kaiser Permanente Total Joint Replacement Registry) was used to identify primary THAs performed for any elective diagnosis between April 1, 2001 and December 31, 2011, in a large integrated US healthcare system. The study sample included cases from 50 medical centers with 336 surgeons in seven US geographical regions (southern and northern California, Colorado, Georgia, Hawaii, Northwest, mid-Atlantic). During the course of the study, the membership population in these regions was more than nine million people. When dislocation was the outcome, the sample was limited to operative dates from January 1, 2007 to December 31, 2011, for southern California, northern California, and Hawaii, which are the time periods and regions for which complete information regarding dislocations was available.
The Total Joint Replacement Registry uses standardized electronic and paper data collection forms. The forms are completed by the surgeons and staff in the operating room. The participation is voluntary and was 95% for the THAs in 2011 [40]. The forms capture information on patient demographics, surgical technique, implant characteristics, and patient outcome. Registry data are validated using the hospital utilization database and independent chart review.
All patients undergoing primary elective THA with any diagnosis were included in the study (N = 42,438). Revision procedures and same-day bilateral procedures were not included.
The exposure of interest in this study was surgical approach (posterior, anterolateral, direct lateral, direct anterior). Other variables were regarded as potential confounders of the relationship between surgical approach and the outcomes of interest. These potential confounders included patient, implant, surgeon, and hospital factors. Patient covariates evaluated were: age, sex, race (white, black, Hispanic, Asian, Native American, other/multi), body mass index, and American Society of Anesthesiologists score (1, 2, ≥ 3). Implant attributes evaluated included: fixation type (cemented, uncemented, hybrid), bearing surface (ceramic-on-ceramic, ceramic-on-constrained, ceramic-on-conventional polyethylene, ceramic-on-highly crosslinked polyethylene, ceramic-on-metal, metal-on-constrained polyethylene, metal-on-conventional poly-ethylene, metal-on-highly crosslinked polyethylene, and metal-on-metal), femoral head size (≤ 28 mm, 32 mm, 36 mm, > 36 mm), and whether a DePuy’s ASR Hip System (DePuy Orthopaedics, Inc, Warsaw, IN, USA) was used for the procedure. The DePuy ASR Hip System components were separated in the analysis to attempt to control for the unique increase in risk of revision of this component as a result of its August 2010 recall and implantation cessation in this organization in June 2010 [17].
The endpoints of this study were septic revisions, aseptic revisions, and dislocations. Revision was defined as any operation after the index THA where a component was replaced. Aseptic revisions were performed for any reason other than infection-related causes. Reasons for revision were recorded by the surgeons on the Total Joint Replacement Registry operative forms and confirmed by chart review by a trained clinical research associate (see Acknowledgments). Dislocations were identified based on International Classifications of Disease, 9th Revision, Clinical Modification (ICD-9-CM) codes 718.35, 835*, or 996.42. Dislocations were considered related to the index hip if they occurred within 1 year of the operation date.
Frequencies, proportions, mean, SDs, medians, and interquartile ranges (IQRs) were used to describe the study sample. Crude revision rates and revision rate per 100 years of observation were calculated. Survival analysis was performed with marginal multivariate Cox models using a robust standard error (SE) approach to account for surgeon clustering effects [30]. Adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of revision/dislocation for surgical approach are reported. All covariates were included in adjusted models. To account for missing values of some variables, multiple imputations were performed to create 50 versions of the analytic data set and then used Rubin’s rules to calculate the final parameter estimates and SEs from the output sets [44]. The imputation model included all covariates as well as the event indicator and the Nelson-Aalen estimator of the cumulative baseline hazard at the time of event or censoring for each case [48]. Significance tests for proportional hazards were based on plots of the standardized score process against time for each covariate and comparing the observed curve with 1000 simulated curves under the assumption of proportional hazards using the listwise deleted data [31]. A similar approach using cumulative sums of martingale residuals was adopted for tests of functional form. In the presence of a significant test, the form of the relationship was based on plots of the data (eg, omitted variable plots of martingale residuals to determine the functional form). We have sufficient power (1 − β ≥ 0.80) to detect a minimum difference (which we believe to be a clinically important effect size) of HR = 1.5 for the anterolateral and direct anterior approaches for aseptic revisions and anterolateral for septic revisions (all in comparison to the posterior approach). Data were analyzed using SAS (Version 9.2; SAS Institute, Cary, NC, USA) and α = 0 .05 was used as the threshold for statistical significance.
A total of 42,438 primary THAs were available for analysis of revision outcomes and 22,237 for the dislocation outcome. The cohort mean age was 66 years old (SD = 12) and was mostly female (58%) and white (75%). The most commonly used approach was posterior (75%, N = 31,747) followed by anterolateral (10%, N = 4226), direct anterior (4%, N = 1851), and direct lateral (2%, N = 667). The most common bearing surface was metal on highly crosslinked polyethylene (58%; N = 24,685). Uncemented implants were used in 83% (N = 35,024) of the cases and femoral head sizes ≥ 36 mm were used in 46% (N = 19,323) of the cases (Table 1).
During the 3 years (IQR, 1–5 years) median followup of the cohort, 2767 (7%) patients died and 4282 (10%) terminated their health plan membership.
Results
During the study period, 785 hips (2%) were revised for aseptic reasons, 213 (1%) for infection, and 276 (1%) experienced a dislocation (Table 2). The revision rate per 100 years of observation is 0.54 (95% CI, 0.5–0.57) for aseptic revisions, 0.15 (95% CI, 0.13–0.17) for septic revisions, and 0.58 (95% CI, 0.52–0.65) for dislocations.
There were no differences in adjusted risk of revision (either septic or aseptic) and THA approaches (Table 3). However, the anterolateral approach (HR, 0.29; 95% CI, 0.13–0.63, p = 0.002) and direct anterior approach (HR, 0.44; 95% CI, 0.22–0.87, p = 0.017) had a lower adjusted risk of dislocation relative to the posterior approach.
We compared anterolateral and direct anterior approaches as well and found that there were no significant differences in the risk of septic revision (HR, 0.78; 95% CI, 0.34–1.77, p = 0.558), aseptic revision (HR, 0.79; 95% CI, 0.46–1.35, p = 0.393), and dislocation (HR, 0.69; 95% CI, 0.24–1.97, p = 0.491), but the point estimates do favor the anterolateral approach.
Discussion
Anteriorly based surgical approaches (those approaches characterized by opening the joint capsule from the front of the joint) are being used increasingly in the community setting. However, we do not know whether these approaches reduce the risk of dislocation without increasing risk of early failure. In our large community-based sample, a lower risk of dislocation, with no evidence of difference in the risk of revision (either septic or aseptic), was observed in THAs performed with anterolateral and direct anterior approaches compared with a posterior approach.
Our study is limited to the three outcomes evaluated. We were not able to evaluate other postoperative outcomes potentially different between the approaches evaluated such as acetabular cup inclination, implant positioning, intraoperative complication (eg, limp, never injuries, intraoperative fractures), functional outcomes, patient-reported outcomes, or postoperative recovery. How dislocations were ascertained also is a potential limitation of our study. Dislocations were identified using a hospital utilization database using ICD-9-CM discharge diagnosis codes but as a result of the lack of laterality, specificity, and sometimes inaccuracies of ICD-9-CM codes, these events could potentially be inaccurate. However, we used the same algorithms used by large studies [7, 24] using administrative data in an attempt to use a comparable way to ascertain the outcome so our estimations could be compared with others. Additionally, missing data was a limitation of our study. This was handled by using multiple imputations, which estimated the values for the missing data points in an attempt to reduce bias and increase precision relative to removing cases with missing information. Although our proportion of loss to followup is small (4282 out of 42,438 hips [10%]), it is still a limitation of our study. However, because there was no differential loss to followup among the posterior, anterolateral, and direct lateral approaches, we do not believe that this introduced bias in our estimates of event rates across these groups. We had a median followup of 2 years (IQR, 0.8–4 years) on the patients who were lost to followup, which means these patients’ data contributed to our estimates for this amount of time as well. There was a slightly lower proportion of patients with direct anterior approaches who were lost to followup, which would increase the chances of us finding events on these cases during the followup, but because this was not the case, we believe that our estimations of dislocation risk may actually be conservative for this approach. The lack of information on surgeon experience or surgeon volume is also a potential limitation of our study because these may be confounders of the associations studied.
Few studies have investigated the influence of surgical approach on revision rate [2, 32, 39]. In our study, there were no differences in aseptic revision rates across the various approaches. The risk of aseptic revision for either the direct anterior or the anterolateral approaches was not different than the posterior approach. Our results are comparable to a prospective, nonrandomized, multicenter study of 1089 THAs comparing anterolateral with posterior approaches. At 5 years they observed no differences in revision rates between the groups [32, 39]. The Swedish Hip Register reported a complex relationship among surgical approach, implant used, and revision rate. A reduced risk of dislocation with increased risk of aseptic revision was observed in the anterolateral transgluteal approach as compared with the posterior approach with a specific implant type [32]. The authors attributed this to possible acetabular cup malpositioning (inclination angle of greater than 50°), which was more common with the anterolateral approach [9].
A number of previous studies have indicated that the approaches from the front of the joint have a distinct advantage of reducing the rate of postoperative dislocation [14, 43, 45]. Our findings confirm these observations. The rate of dislocation was lowest with the anterolateral approach and a substantially lower adjusted risk of dislocation for both the anterolateral and anterior approaches was observed compared with the posterior approach. As compared with some older studies [16, 36], the overall rate of dislocation after THA reported in contemporary joint arthroplasty registries has been low [4, 26]. This lower rate has been attributed to newer surgical approaches, use of larger diameter femoral heads, and improved posterior capsular repair after a posterior approach [8, 19, 20, 22, 27, 47]. Most published studies have indicated that use of larger femoral heads has resulted in overall reduction in rate of dislocation [14, 19, 20, 22, 47]. Although 45% of our patients had large femoral head size (36 mm or greater), this was controlled for in our statistical analysis. We believe that the lower risk dislocation in anterior approaches is the result of the nature of surgical approaches per se. Reliability of registry data must also be considered, as noted by Devane et al. [13], who reported that registry data included only the dislocation event that led to revision. The true rate of all dislocations, inclusive of those requiring closed reduction, in their study was almost two times higher (3%) [13] than reported in the registry data. We believe our data reflect a very close estimation of the true dislocation rate. Our findings were based on the stable patient population and a very robust data collection system.
The strengths of our study include a large and representative sample of patients and very robust follow up data collection process. Our data reflect outcomes in a community-based setting where some surgeons may have learned the newer anterior approaches either during their fellowship training or through training courses. Because many community-based surgeons are gradually adopting anterior approaches in their practices, we believe that our results reflect the risks and benefits of these approaches as applied in nonacademic settings. The data for this study were mostly extracted from a total joint replacement registry database, which prospectively collects the information using predetermined data capture templates and uses active surveillance techniques for detecting outcomes as well as confirmation of these outcomes by chart review. This guarantees the internal validity of the information being presented in this study. The results of our study support the idea that approaches from the front of the joint are associated with a lower risk of dislocation. It is conceivable that one can forego dislocation precautions during the postoperative period facilitating early rehabilitation; however, specific clinical studies should evaluate this premise.
References
Alecci V, Valente M, Crucil M, Minerva M, Pellegrino CM, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthop Traumatol. 2011;12:123–129.
Arthursson AJ, Furnes O, Espehaug B, Havelin LI, Soreide JA. Prosthesis survival after total hip arthroplasty—does surgical approach matter? Analysis of 19,304 Charnley and 6,002 Exeter primary total hip arthroplasties reported to the Norwegian Arthroplasty Register. Acta Orthop. 2007;78:719–729.
Bernasek TL, Lee W-S, Lee H-J, Lee J-S, Kim K-H, Yang J-J. Minimally invasive primary THA: anterolateral intermuscular approach versus lateral transmuscular approach. Arch Orthop Trauma Surg. 2011;130:1349–1354.
Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463.
Bertin KR, Röttinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res. 2004;429:248–255.
Bhandari M, Matta JM, Dodgin D, Clark C, Kregor P, Bradley G, Little L. Outcomes following the single-incision anterior approach to total hip arthroplasty: a multicenter observational study. Orthop Clin North Am. 2009;40:329–342.
Bozic KJ, Ong K, Lau E, Kurtz SM, Vail TP, Rubash HE, Berry DJ. Risk of complication and revision total hip arthroplasty among Medicare patients with different bearing surfaces. Clin Orthop Relat Res. 2010;468:2357–2362.
Brennan S, Khan F, Kiernan C, Queally J, McQuillan J, Gormley I, O’Byrne J. Dislocation of primary total hip arthroplasty and the risk of redislocation. Hip Int. 2012;22:500–504.
Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, Malchau H. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319–329.
D’Arrigo C, Speranza A, Monaco E, Carcangiu A, Ferretti A. Learning curve in tissue sparing total hip replacement: comparison between different approaches. J Orthop Traumatol. 2009;10:47–54.
De Geest T, Vansintjan P, De Loore G. Direct anterior total hip arthroplasty: complications and early outcome in a series of 300 cases. Acta Orthop Belg. 2013;79:66–73.
de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, Hutchison J, Grant A, Coyle D, Coyle K, Vale L. A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip. Health Technol Assess. 2008;12:iii–iv, ix–223.
Devane PA, Wraighte PJ, Ong DCG, Horne JG. Do joint registries report true rates of hip dislocation? Clin Orthop Relat Res. 2012;470:3003–3006.
Dudda M, Gueleryuez A, Gautier E, Busato A, Roeder C. Risk factors for early dislocation after total hip arthroplasty: a matched case-control study. J Orthop Surg (Hong Kong). 2010;18:179–183.
Edmunds CT, Boscainos PJ. Effect of surgical approach for total hip replacement on hip function using Harris hip scores and Trendelenburg’s test. A retrospective analysis. Surgeon. 2011;9:124–129.
Engh CA Jr, Hopper RH Jr, Engh CA Sr. Distal ingrowth components. Clin Orthop Relat Res. 2004;420:135–141.
FDA. Medical Devices Recalls. Recalls specific to metal-on-metal hip implant systems. DePuy ASR™ XL Acetabular System. Available at: http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/MetalonMetalHipImplants/ucm241770.htm. Accessed August 13, 2012.
Goosen JH, Kollen BJ, Castelein RM, Kuipers BM, Verheyen CC. Minimally invasive versus classic procedures in total hip arthroplasty: a double-blind randomized controlled trial. Clin Orthop Relat Res. 2011;469:200–208.
Hailer NP, Weiss RJ, Stark A, Karrholm J. The risk of revision due to dislocation after total hip arthroplasty depends on surgical approach, femoral head size, sex, and primary diagnosis. An analysis of 78,098 operations in the Swedish Hip Arthroplasty Register. Acta Orthop. 2012;83:442–448.
Howie DW, Holubowycz OT, Middleton R. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012;94:1095–1102.
Inaba Y, Kobayashi N, Yukizawa Y, Ishida T, Iwamoto N, Saito T. Little clinical advantage of modified Watson-Jones approach over modified mini-incision direct lateral approach in primary total hip arthroplasty. J Arthroplasty. 2011;26:1117–1122.
Jameson SS, Baker PN, Charman SC, Deehan DJ, Reed MR, Gregg PJ, Van der Meulen JH. The effect of aspirin and low-molecular-weight heparin on venous thromboembolism after knee replacement: a non-randomised comparison using National Joint Registry Data. J Bone Joint Surg Br. 2011;94:914–918.
Jerosch J, Theising C, Fadel ME. Antero-lateral minimal invasive (ALMI) approach for total hip arthroplasty technique and early results. Arch Orthop Trauma Surg. 2006;126:164–173.
Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2001;83:1622–1629.
Kennon R, Keggi J, Zatorski L, Keggi K. Anterior approach for total hip arthroplasty: beyond the minimally invasive technique. J Bone Joint Surg Am. 2004;86(Suppl 2):91–97.
Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23.
Kwon M, Kuskowski M, Mulhall K, Macaulay W, Brown T, Saleh K. Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res. 2006;447:34–38.
Laffosse J, Chiron P, Accadbled F, Molinier F, Tricoire J, Puget J. Learning curve for a modified Watson-Jones minimally invasive approach in primary total hip replacement: analysis of complications and early results versus the standard-incision posterior approach. Acta Orthop Belg. 2006;72:693–701.
Lamontagne M, Varin D, Beaulé PE. Does the anterior approach for total hip arthroplasty better restore stair climbing gait mechanics? J Orthop Res. 2011;29:1412–1417.
Lee EW, Wei LJ, Amato DA. Cox-type regression analysis for large number of small groups of correlated failure time observations. In: Klein JP, Goel PK, eds. Survival Analysis: State of the Art. Dordrecht, The Netherlands: Kluwer; 1992.
Lin DY, Wei LJ, Ying Z. Checking the cox model with cumulative sums of Martingale-based residuals. Biometrika. 1993;80:557–572.
Lindgren V, Garellick G, Kärrholm J, Wretenberg P. The type of surgical approach influences the risk of revision in total hip arthroplasty: a study from the Swedish Hip Arthroplasty Register of 90,662 total hipreplacements with 3 different cemented prostheses. Acta Orthop. 2012;83:559–565.
Mandereau C, Brzakala V, Matsoukis J. Functional recovery, complications and CT positioning of total hip replacement performed through a Röttinger anterolateral mini-incision. Review of a continuous series of 103 cases. Orthop Traumatol Surg Res. 2012;98:8–16.
Martin R, Clayson PE, Troussel S, Fraser BP, Docquier PL. Anterolateral minimally invasive total hip arthroplasty: a prospective randomized controlled study with a follow-up of 1 year. J Arthroplasty. 2011;26:1362–1372.
Matta J, Ferguson T. The anterior approach for hip replacement. Orthopedics. 2005;28:959–960.
Morrey B. Instability after total hip arthroplasty. Orthop Clin North Am. 1992;23:237–248.
Mouilhade F, Matsoukis J, Oger P, Mandereau C, Brzakala V, Dujardin F. Component positioning in primary total hip replacement: a prospective comparative study of two anterolateral approaches, minimally invasive versus gluteus medius hemimyotomy. Orthop Traumatol Surg Res. 2011;97:14–21.
Müller M, Tohtz S, Springer I, Dewey M, Perka C. Randomized controlled trial of abductor muscle damage in relation to the surgical approach for primary total hip replacement: minimally invasive anterolateral versus modified direct lateral approach. Arch Orthop Trauma Surg. 2011;131:179–189.
Palan J, Beard D, Murray D, Andrew J, Nolan J. Which approach for total hip arthroplasty: anterolateral or posterior? Clin Orthop Relat Res. 2009;467:473–477.
Paxton EW, Kiley ML, Love R, Barber TC, Funahashi TT, Inacio MC. Kaiser Permanente implant registries benefit patient safety, quality improvement, cost-effectiveness. Jt Comm J Qual Patient Saf. 2013;39:246–252.
Pospischill M, Kranzl A, Attwenger B, Knahr K. Minimally invasive compared with traditional transgluteal approach for total hip arthroplasty: a comparative gait analysis. J Bone Joint Surg Am. 2010;92:328–337.
Queen RM, Butler RJ, Watters TS, Kelley SS, Attarian DE, Bolognesi MP. The effect of total hip arthroplasty surgical approach on postoperative gait mechanics. J Arthroplasty. 2011;26(Suppl):66–71.
Restrepo C, Mortazavi SM, Brothers J, Parvizi J, Rothman RH. Hip dislocation: are hip precautions necessary in anterior approaches? Clin Orthop Relat Res. 2011;469:417–422.
Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY, USA: John Wiley & Sons, Inc; 1987.
Skoldenberg OG, Salemyr MO, Boden HS, Ahl TE, Adolphson PY. The effect of weekly risedronate on periprosthetic bone resorption following total hip arthroplasty: a randomized, double-blind, placebo-controlled trial. J Bone Joint Surg Am. 2011;93:1857–1864.
Smith AJ, Wylde V, Berstock JR, Maclean AD, Blom AW. Surgical approach and patient-reported outcomes after total hip replacement. Hip Int. 2012;22:255–261.
Stroh D, Issa K, Johnson A, Delanois R, Mont M. Reduced dislocation rates and excellent functional outcomes with large-diameter femoral heads. J Arthroplasty. 2013;28:1415–1420.
White IR, Royston P. Imputing missing covariate values for the Cox model. Stat Med. 2009;28:1982–1998.
Yang B, Li H, He X, Wang G, Xu S. Minimally invasive surgical approaches and traditional total hip arthroplasty: a meta-analysis of radiological and complications outcomes. PLoS One. 2012;7:e37947.
Yi C, Agudelo J, Dayton M, Morgan S. Early complications of anterior supine intermuscular total hip arthroplasty. Orthopedics. 2013;36:e276–281.
Zimmerma S, Hawkes WG, Hudson JI, Magaziner J, Hebel JR, Towheed T, Gardner J, Provenzano G, Kenzora JE. Outcomes of surgical management of total HIP replacement in patients aged 65 years and older: cemented versus cementless femoral components and lateral or anterolateral versus posterior anatomical approach. J Orthop Res. 2002;20:182–191.
Acknowledgments
We acknowledge all the Kaiser Permanente orthopaedic surgeons who contribute to the total joint replacement registry and the Surgical Outcomes and Analysis Department, which coordinates registry operations (including the adjudication of complications presented in this study). We thank all Kaiser Permanente orthopaedic surgeons and the staff of the Department of Surgical Outcomes and Analysis who have contributed to the success of the National Total Joint Replacement Registry.
Author information
Authors and Affiliations
Corresponding author
Additional information
No authors or any member of any author’s immediate family, has any funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Southern California Permanente Medical Group, Irvine, CA, USA.
About this article
Cite this article
Sheth, D., Cafri, G., Inacio, M.C.S. et al. Anterior and Anterolateral Approaches for THA Are Associated With Lower Dislocation Risk Without Higher Revision Risk. Clin Orthop Relat Res 473, 3401–3408 (2015). https://doi.org/10.1007/s11999-015-4230-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4230-0