Abstract
Purpose of Review
The development of acute failure of the kidneys in the context of decompensated cirrhosis represents one of the most challenging scenarios in clinical medicine due to the severity and complexity of the coexistence of those 2 illnesses. Thus, managing those cases can be cumbersome.
Recent Findings
While the state of advanced cirrhosis and portal hypertension can lead to a unique type of acute kidney injury (AKI)—hepatorenal syndrome type 1 (HRS-1)—a number of other etiologies can cause AKI, such as prerenal or cardiorenal insults, acute tubular injury, and other parenchymal entities. As a result, medical management of AKI in cirrhosis should be dictated by the driving cause of AKI.
Summary
Intravenous albumin is the preferred volume expander for hypovolemic states. Decongestive therapies are indicated in tense ascites-associated abdominal compartment syndrome and/or cardiorenal syndrome type 1. Vasoconstrictor therapy aimed to a specific rise in mean arterial pressure constitutes the cornerstone of the management of HRS-1. Most tubular causes of AKI are managed with supportive care, whereas other tubulointerstitial and glomerular conditions may warrant other interventions such as drug discontinuation, immunosuppression, or antimicrobial/antiviral therapy. Ultimately, AKI unresponsive to medical management may progress, and patients may ultimately necessitate renal replacement therapy (RRT) to sustain life. However, RRT must be carefully considered in this patient population taking in consideration eligibility for liver transplantation, life expectancy, risks and morbidity associated with RRT, and patients’ wishes and those of their families or support network.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Individuals with cirrhosis are frequently affected with acute kidney injury (AKI). The incidence of in-hospital AKI in patients with cirrhosis ranges around 20–50% [1,2,3]. Many factors increase the risk for patients with cirrhosis to acquire AKI. Thus, the differential diagnosis for the etiology of AKI can be very broad in this setting. Although there are certain supportive care measures that apply to all causes of AKI, many of the conditions that lead to AKI in cirrhosis are treated in a manner which may not be applicable to other causes of AKI. Therefore, this review will outline the recommended management strategies in AKI in cirrhosis organized by the underlying etiology.
Prerenal azotemia
Prerenal azotemia encompasses a broad spectrum of causes of AKI that extend from straightforward volume depletion to those related to a hemodynamic derangement leading to decreased renal perfusion. In patients with decompensated cirrhosis, volume depletion is commonly encountered. Prerenal azotemia accounts for 15–30% of AKI in patients with cirrhosis [4, 5]. In one study, prerenal azotemia secondary to gastrointestinal hemorrhage was the most common cause of AKI in cirrhosis accounting for 69% of the cases [6]. Many factors inherent to cirrhosis can lead to volume depletion including diarrhea due to laxatives prescribed for hepatic encephalopathy (HE) prophylaxis, gastrointestinal hemorrhage from esophageal varices, urinary losses from diuretics, and poor oral intake in the context of infections such as spontaneous bacterial peritonitis (SBP) [7]. The combination of a peripheral vasodilatory state, poor effective arterial blood volume (EABV), and hypoalbuminemia predispose patients with cirrhosis to prerenal insults. In this regard, assessment of total blood volume distribution by radionuclide imaging demonstrated increased pooling of plasma volume in the splanchnic circulation of patients with cirrhosis in comparison to healthy controls [8].
In addition, cardiorenal syndrome type 1 (CRS-1), renal vein congestion, and intra-abdominal hypertension (IAH)/abdominal compartment syndrome (ACS) from tense ascites are conditions that contribute to the spectrum of prerenal causes of AKI in patients with decompensated cirrhosis. Although the evolution of advanced cirrhosis typically leads to a state of high-output heart failure, patients are at risk of evolving into cirrhotic cardiomyopathy (CCM) [9]. Individuals with alcoholic liver disease can at times present with ethanol-associated dilated cardiomyopathy [10, 11]. Thus, poor cardiac output as in CRS-1 can contribute to AKI in cirrhosis. In addition, porto-pulmonary hypertension can lead to renal vein congestion and impairment in renal perfusion. Needless to say, the management of volume depletion dramatically differs from that of CRS-1 or ACS. Thus, those treatment approaches are discussed separately (Fig. 1).
-
1.
Withdrawal of offending agents
Approach to volume management in patients with cirrhosis and acute kidney injury (AKI). Individuals with cirrhosis are vulnerable to acquiring states of volume depletion. Portal hypertension is associated with decreased effective arterial blood volume (EABV) which predisposes them to further reduction in renal perfusion. Gastrointestinal bleeding due to esophageal varices is a frequent cause of decompensation and hemodynamic instability. Prophylaxis for hepatic encephalopathy with laxatives can elicit diarrheal losses and hypovolemia. Infection, such as spontaneous bacterial peritonitis (SBP), can lead to systemic inflammatory response and inadequate organ perfusion. Refractory ascites often necessitates aggressive diuretic therapy and/or frequent paracentesis. During treatment of hepatorenal syndrome type 1 (HRS-1), concomitant administration of albumin may increase the efficacy of a vasoconstrictor. Based on these factors, the traditional dogma calls for standard resuscitation with intravenous (IV) albumin of all patients with cirrhosis and AKI. However, other factors could lead to volume overload and should be considered during initial assessment. Cirrhotic cardiomyopathy, alcoholic cardiomyopathy and porto-pulmonary hypertension can lead to fluid overload and renal vein congestion. Oliguria and hepatorenal physiology can be present upon arrival and lead to hypervolemia. Tense ascites can result in abdominal compartment syndrome. Therefore, on each case, consideration for diuretics and/or paracentesis has to be balanced against a potential effect of administration of IV albumin.
Regardless of the type of prerenal insult, there are a number of medications that can elicit alterations in renal hemodynamics and precipitate AKI. Therefore, exposure to those medications should be promptly identified and properly discontinued. Non-steroidal anti-inflammatory drugs (NSAIDs) are notorious for conferring a greater risk for AKI in patients with cirrhosis [12]. Prostaglandin release in cirrhosis is perceived as an adaptation that protects the renal circulation from a state of preponderance of vasoconstrictors that are released upon activation of the renin-angiotensin system (RAS) and the sympathetic nervous system (SNS). Consequently, NSAIDs can briskly precipitate AKI in cirrhosis. Laxatives and diuretics are often prescribed in cirrhosis to manage risk for HE and refractory ascites, respectively. In the setting of AKI, the use of these medications must be carefully evaluated due to the risk of volume depletion from excessive gastrointestinal fluid or urine losses. Furthermore, certain antihypertensives can precipitate AKI. Angiotensin-converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARB) are known to alter renal hemodynamics and reduce glomerular filtration rate (GFR). In addition, beta-blockers, often used in portal hypertension, have been shown to increase the risk for development of hepatorenal syndrome type 1 (HRS-1) presumably by reducing systemic mean arterial pressure (MAP). Therefore, these agents should be discontinued in patients with cirrhosis presenting with AKI [13,14,15].
-
2.
Volume expansion for hypovolemia
Intravenous (IV) volume expansion is the cornerstone of the treatment of hypovolemia. In cirrhosis, IV albumin is more effective restoring EABV compared to crystalloids. A study compared the effect of fluid resuscitation with isotonic normal saline or albumin in healthy controls and patients with cirrhosis. Following IV saline (2 L in 4 h), a greater reduction in plasma renin activity (PRA) was observed in healthy subjects compared to that observed in patients with cirrhosis. In contrast, IV albumin (50 g in 2 h) reduced PRA in patients with cirrhosis to the same extent as in healthy controls [16]. Thus, albumin was deemed more effective than saline in restoring EABV in cirrhosis. Additional lines of evidence demonstrate that albumin is the preferred volume expander in cirrhosis. In a randomized controlled trial (RCT), albumin was superior to saline in reducing post-paracentesis circulatory dysfunction when greater than 6 L of ascitic fluid were drained. Specifically, no change in PRA was observed in albumin-treated subjects compared to a significant increase in PRA in the saline group at both 24 h and 6 days after paracentesis [17]. Furthermore, in patients with SBP, co-administration of albumin with antibiotics led to a reduction in the incidence of AKI as compared to placebo added to antibiotics [18].
In light of considerable benefits of albumin, the International Club of Ascites (ICA) recommends albumin-based volume expansion at a dose of 1 g/kg for 48 h as an initial strategy to revert hypovolemia in cirrhosis with AKI [14]. However, emerging reports suggest that this liberal recommendation may not be ideal. In a RCT comparing the effect of normalization of serum albumin versus standard of care (ATTIRE trial) [19], administration of albumin was associated with greater risk of pulmonary edema and no survival benefit. The median cumulative dose of albumin in the intervention arm was 200 g (IQR 14–280) throughout the duration of the 15-day trial. Moreover, in a RCT testing the benefit of terlipressin added to albumin against placebo added to albumin (CONFIRM trial) [20], subjects treated with terlipressin and albumin had a higher incidence of respiratory failure. The mean total dose of albumin for both treatment arms (prior to randomization and during the trial) was ~ 500–600 g [21]. While the amount of albumin given in the ATTIRE and CONFIRM trial exceeded that recommended dosage for a 48-h trial, patients who fail a 48-h trial may go on to continue receiving more albumin as part of HRS-1 management. Noninvasive modalities such as point-of-care echocardiography, lung ultrasonography, and other novel methodologies such as VeXUS [22] may prove useful to guide volume management in this patient population [23]. Nonetheless, a time-limited trial of tailored albumin resuscitation is deemed a reasonable approach if the clinical picture suggests a prerenal state.
For patients arriving with gastrointestinal hemorrhage, volume resuscitation with blood products should be entertained, although the ideal hemoglobin target is unknown. Identification and ligation of underlying bleeding vessels intended to minimize blood loss should be pursued in active gastrointestinal hemorrhage leading to hemodynamic instability [24].
-
3.
Decongestion
Decompensated cirrhosis with portal hypertension leads to ascites. In turn, ascites can lead to IAH and ACS. Elevated renal venous pressures impair renal perfusion and can cause and/or contribute to prerenal AKI. Renal vein congestion is not rare in advanced cirrhosis. In a cohort of 125 patients with cirrhosis, the mean central venous pressure was 12.8 mmHg [25]. In an another study, a renal vein diameter > 11 mm was associated with increased mortality independently of MELD–Na scores [26]. Decongestion with diuretics and/or large volume paracentesis (LVP) may relieve renal vein congestion and increase GFR and urine output [27, 28]. Despite lack of supporting evidence, concern for LVP precipitating AKI persists. In a recent study [29], evaluating the impact of LVP on kidney function among hospitalized patients with cirrhosis, kidney function improved in 10% of patients after LVP whereas it worsened in only 4%, supporting a role of decongestive therapies in patients with cirrhosis and IAH (Fig. 1).
Decreased peripheral vascular resistance and high-output heart failure are classic elements of cardiac physiology in advanced cirrhosis. As the disease evolves, decreased cardiac conductance and contractility lead to progression to CCM and CRS-1. Management of AKI in CCM has not been formally studied. Diuretics along with traditional heart failure medications can be considered [30]. The prognosis of patients with CCM after liver transplantation is uncertain [31].
The state of decompensated cirrhosis, portal hypertension, and deranged hemodynamics predispose a subset of patients to develop porto-pulmonary hypertension [32]. A direct role of porto-pulmonary hypertension in contributing to AKI remains unclear [33]. However, porto-pulmonary hypertension could potentiate right-sided heart failure, IAH, and renal vein congestion, thus precipitating prerenal AKI. In a prospective observational cohort of patients with porto-pulmonary hypertension, early administration of intravenous prostacyclin was associated with improved 5-year mortality as compared to control [34]. However, its role in the context of AKI has not been examined.
Hepatorenal syndrome type 1
HRS-1 is a unique form of AKI affecting individuals with advanced cirrhosis and portal hypertension. In response to elevated hepatic sinusoidal pressure and splanchnic vasodilation, the RAS and SNS are overactivated, leading to profound renal vasoconstriction and AKI. HRS-1 is potentially reversible with timely administration of vasoconstrictors and albumin [35,36,37,38,39,40,41,42,43]. Vasoconstrictors reverse splanchnic vasodilation and, in combination with IV albumin, restore the EABV, thereby reversing the neurohumoral responses that precipitated HRS-1. Intrarenal perfusion is thereby restored leading to improvement in GFR. Vasoconstrictors and albumin are the mainstay of HRS-1 treatment and are recommended in guidelines released by the European Association for the Study of the Liver (EASL), American Association for the Study of Liver Diseases (AASLD), and the American College of Gastroenterology (ACG) [42, 44, 45].
Several factors must be considered when evaluating the applicability of findings from vasoconstrictor trials to the clinical management of patients with HRS-1. First, the timespan of these trials included evolving definitions of HRS-1 and changes in the recommendations for treatment of decompensated cirrhosis (e.g., albumin dosing). Prior to 2015, HRS-1 was defined as an increase in serum creatinine (sCr) ≥ 50% from baseline and to ≥ 1.5 mg/dL. In order to facilitate earlier diagnosis and treatment, the ICA changed the definition of HRS-1 in 2015 to an absolute rise in sCr ≥ 0.3 mg/dL from baseline and eliminated the 1.5 mg/dL threshold [14]. However, all prior vasoconstrictor trials, including the recent CONFIRM trial, used earlier definitions of HRS-1. Therefore, despite real-world observational data suggesting improved outcomes with earlier treatment, RCT data to support this practice is lacking [46]. Trial endpoints are another important factor to consider when evaluating the evidence for vasoconstrictors in HRS-1. These trials were not designed or powered to detect differences in survival. Rather, “HRS reversal” was typically used as the primary endpoint and defined with variable stringency based on improvements in sCr to a pre-specified value (e.g., ≤ 1.5 mg/dL) or towards the pre-treatment sCr (e.g., to within 0.3 mg/dL of baseline) [47, 48]. Finally, the risk for development of adverse effects of vasoconstrictor therapy are important to consider [49]. While data suggest that these regimens are generally well-tolerated, it should be recognized that patients with coronary artery disease or peripheral vascular disease were often excluded from trial participation [20, 50] Therefore, clinicians should be vigilant in monitoring for extracellular fluid volume overload and ischemic events.
-
1.
Albumin
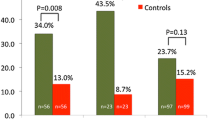
Albumin’s primary mechanism of action in HRS-1 is thought to be mediated by increased oncotic pressure leading to restoration of EABV. Although preclinical studies suggest that its antioxidant, anti-inflammatory, and immunomodulatory effects may also play a role [18, 19, 51], a clinical study failed to confirm this contention [52] Treatment of HRS-1 with albumin alone does not appear to be effective. A 2008 study by Martín-Llahí et al. demonstrated reversal of HRS in 44% of patients treated with terlipressin and albumin (n = 23) in comparison to 9% in patients treated with albumin alone (n = 23) [53]. Despite its lack of efficacy as monotherapy for HRS-1, albumin may augment the efficacy of vasoconstrictor therapy. Indeed, a 2002 prospective nonrandomized study demonstrated reversal of HRS in 77% in patients receiving terlipressin and albumin in comparison to only 25% in patients receiving terlipressin alone [54]. Various strategies for IV albumin dosing and monitoring have been used in RCTs for HRS-1 (Table 1). In general, 25% albumin is administered starting at 1 g/kg/d for 2 days (maximum of 100 g/d) and then 20–40 g/d. Clinicians should be aware that albumin administration may cause or exacerbate extracellular volume overload and pulmonary edema and that these effects may be potentiated by concomitant use of a vasoconstrictor [19, 20, 49].
-
2.
Vasoconstrictors
Terlipressin
Terlipressin is a synthetic vasopressin analog with preferential affinity for the V1 receptors [55] Terlipressin is the most studied drug for HRS-1 in RCTs and is recommended as first-line therapy where the drug is approved [42, 45, 49]. Terlipressin is typically initiated at 1–2-mg IV bolus every 4–12 h (Table 1) and can also be administered via continuous infusion. Efficacy of boluses and infusion seem comparable, whereas the safety profile of continuous infusion may be favorable [56]. In clinical trials, the dose of terlipressin was typically increased on day 3 or 4 of therapy in response to the rate of improvement in sCr. In contrast to norepinephrine (NE), terlipressin does not require administration by a central venous line or intensive care unit monitoring. High-dose NE administered via peripheral line has been linked to tissue ischemia [57]. Treatment of HRS-1 with terlipressin and albumin has been studied in 4 randomized, placebo-controlled clinical trials with variable rates of HRS-1 reversal (Table 1). In 2021, Wong et al.reported the results of the CONFIRM trial, the largest RCT of any vasoconstrictor agent for treatment of HRS-1 [20]. Patients with HRS-1 were randomized to receive IV albumin in combination with either bolus dose terlipressin (n = 199) or matching placebo (n = 101). In a departure from prior vasoconstrictor RCTs, the CONFIRM trial utilized a more stringent, multicomponent primary endpoint in order to demonstrate that treatment not only improved kidney function but also other meaningful outcomes such as short-term survival and avoidance of renal replacement therapy (RRT) [20, 58]. This primary endpoint, termed “verified HRS reversal,” was defined as two consecutive sCr values of ≤ 1.5 mg/dL at least 2 h apart up to day 14 and RRT-free survival for at least 10 additional days [20, 58]. Patients in the CONFIRM trial had relatively severe kidney dysfunction (mean sCr 3.5 mg/dL) and liver failure (mean MELD score ~ 33) at the time of randomization [20]. Verified HRS reversal was statistically significantly more common in the terlipressin group (32%) compared to placebo (17%). Notably, a higher rate of respiratory failure was observed in the terlipressin group (10%) in comparison to placebo (3%) [20]. Respiratory failure may relate to simultaneous increases in venous return and afterload that exceed the cardiac reserve. Larger cumulative albumin doses in CONFIRM may partially explain these findings.
Norepinephrine
NE exerts its hemodynamic effects by producing systemic vasoconstriction through stimulation of α-adrenergic receptors in the radial smooth muscle of arteries and arterioles and by increasing myocardial contractility through stimulation of the β-1 adrenergic receptors [59]. NE is typically administered by continuous infusion via central venous access starting at 0.5 mg/h and titrated to a maximum dose of 3 mg/h based on targeted increases in MAP (Table 1). The efficacy of NE for treatment of HRS-1 has been compared to terlipressin in 7 RCTs [47, 60,61,62,63,64,65]. In general, NE and bolus dose terlipressin had comparable rates of HRS-1 reversal and similar adverse event profiles. One study compared continuous infusion of terlipressin with NE in patients with acute on chronic liver failure (ACLF) and HRS-1 and reported superiority of terlipressin [47]. However, the study reported unusually low efficacy rate for NE. Therefore, more studies are needed to compare terlipressin infusion and NE in HRS-1.
Midodrine and octreotide
Midodrine produces systemic vasoconstriction via selective α-1 adrenergic agonism and octreotide is a somatostatin analog that causes splanchnic vasoconstriction by inhibiting the release of endogenous vasodilators (e.g., glucagon) [66] Midodrine is typically initiated at 5–7.5 mg orally every 8 h, and octreotide is administered subcutaneously starting at 100–200 μg every 8 h. Midodrine and octreotide are then dose-escalated based on changes in MAP or sCr (Table 1). Midodrine and octreotide do not require central venous access or intensive care monitoring. In 1999, Angeli et al.reported the safety and efficacy of midodrine plus octreotide in combination with IV albumin in 5 patients with HRS-1. Midodrine and octreotide were dosed to achieve an increase in MAP ≥ 15 mmHg and resulted in improved renal plasma flow, GFR, and urine sodium excretion. Mortality was 1 of 5 patients in the midodrine and octreotide group compared to 7 of 8 patients receiving low-dose dopamine [66]. However, no subsequent trials have been reported demonstrating the benefit of midodrine and octreotide. The combination of midodrine and octreotide has been compared to terlipressin for treatment of HRS-1 in 1 RCT. Cavallin et al.randomized subjects to receive terlipressin (n = 27) via continuous infusion (3–12 mg/d) or dose-escalated midodrine and octreotide (n = 21) [48]. Both groups received IV albumin at a dose of 1 g/kg on day 1 and 20–40 g/d thereafter. Terlipressin was associated with statistically significant increases in MAP compared to midodrine and octreotide from day 3 through the end of treatment. The rate of complete response (decrease in sCr to ≤ 1.5 mg/dl) was 55% in the terlipressin group and was statistically significantly higher than the response in the midodrine and octreotide group (4.8%). Circulatory overload occurred in 4% of the terlipressin group and 5% of the midodrine and octreotide group [48]. The midodrine and octreotide regimen has also been compared to NE in two RCTs in patients with HRS-1. In a 2012 study of 23 patients with HRS-1, Tavakkoli et al.demonstrated similarly high rates of HRS reversal (> 70%) in subjects randomized to receive IV albumin in combination with a continuous infusion of NE or dose-escalated midodrine and octreotide [67]. A 2021 study by El-Desouki Mahmoud et al. randomized 60 patients with HRS-1 (per the 2015 ICA diagnostic criteria) to continuous NE infusion or dose-escalated midodrine and octreotide [50]. Both groups received IV albumin at a dose of 20–40 g daily. A statistically significantly higher rate of full response occurred in the NE group (58%) in comparison to the midodrine and octreotide group (42%). The need for mechanical ventilation due to causes including sepsis, HE, shock, pulmonary embolism, pulmonary edema, or multi-organ dysfunction was 27% in the NE group and 48% in the midodrine and octreotide group.
Taken together, data from the RCTs suggest that the midodrine and octreotide regimen is less effective in reversing HRS-1 in comparison to terlipressin or NE. Notably, the rate of circulatory overload and need for mechanical ventilation is comparable to both terlipressin and NE suggesting that close monitoring of volume status is required in patients receiving midodrine and octreotide despite being administered outside of an intensive care setting.
Practical considerations for the use of vasoconstrictor therapy
There are several important factors that impact the efficacy of vasoconstrictor regimens in clinical practice. First, many RCTs adjusted the dose of IV albumin and vasoconstrictor agent based on specific hemodynamic targets (e.g., CVP 10–12 cm H2O, MAP increase > 15 mmHg). In this regard, adjustment of the vasoconstrictor dose in response to changes in MAP is vital to recapitulating the efficacy demonstrated in RCTs. A meta-analysis of 21 studies of vasoconstrictors for HRS-1 demonstrated that improvement in kidney function was significantly correlated with the magnitude of MAP increase, regardless of the baseline blood pressure or vasoconstrictor regimen utilized [37]. Therefore, a reasonable goal would be to target a sustained increase in MAP of > 15 mmHg from baseline (Fig. 2) [68].
Etiology-driven medical management of acute kidney injury (AKI) in cirrhosis. Discontinuation of non-steroidal anti-inflammatory drugs (NSAIDs), beta-blockers, and renin-angiotensin system inhibitors/blockers is recommended regardless of AKI etiology. Diagnosis of hepatorenal syndrome type 1 (HRS-1) prompts consideration for vasoconstrictor therapy, a treatment modality that is unique to HRS-1. Liver transplantation is the ultimate treatment for HRS-1. In addition to the ICA criteria, additional phenotypical elements should be examined (e.g., presence of triggering infection, hyponatremia, baseline low-normal mean arterial pressure, findings in urinary sediment microscopy). Cirrhosis portends risk factors to acquire most types of AKI. Prerenal azotemia can occur as a result of gastrointestinal (GI) losses (e.g., from laxatives used for hepatic encephalopathy) and is managed with discontinuation of diuretics and administration of intravenous albumin ± intravenous fluids (IVF). Acute tubular injury (ATI) can occur as a result of ischemia (e.g., shock from GI bleeding) or toxic injury (e.g., bile acids) and is managed with supportive care. Abdominal compartment syndrome (ACS) can occur as a result of tense ascites and is managed with large-volume paracentesis. Cardiorenal syndrome type 1 (CRS-1) can occur as a result of cardiomyopathy (e.g., cirrhotic, alcoholic, and is managed with diuretics ± inotropes). ATI, ACS, and CRS-1 may overlap with HRS-1 and warrant concomitant therapy. Acute interstitial nephritis can occur from exposure to antibiotics (e.g., quinolones for spontaneous bacterial peritonitis (SBP) and is managed with drug discontinuation ± corticosteroids). Acute glomerulonephritis (GN) can occur in cirrhosis (e.g., IgA nephropathy, hepatitis C–associated membranoproliferative GN (HCV-MPGN) and can be managed with antivirals ± immunosuppressive therapy. Obstructive uropathy can occur as a result of midodrine-induced urinary retention.
A second factor to consider when treating patients with a vasoconstrictor regimen is that the severity of liver disease and the degree of baseline kidney dysfunction both impact the likelihood of successful treatment [69]. For example, in a retrospective study of 298 patients with HRS-1 treated with terlipressin and IV albumin, Piano et al. demonstrated a stepwise reduction in the response to therapy from ACLF grade 1 (ACLF-1) to ACLF-3 across all levels of baseline sCr [69]. Notably, the likelihood of HRS reversal was < 30% in patients with ACLF-3 despite more robust improvements in MAP in comparison to patients with ACLF-1 and ACLF-2 [69]. In a post hoc analysis of data from a RCT of terlipressin for HRS-1, a multivariate analysis demonstrated that pre-treatment sCr was the only significant predictor of response. The likelihood of HRS reversal was highest in patients with pre-treatment sCr < 3.0 mg/dL and was negligible in patients with pre-treatment sCr > 5.0 mg/dL [70]. Taken together, these data suggest that patients with severe kidney dysfunction (sCr > 5 mg/dL) or severe liver dysfunction (ACLF-3) are unlikely to respond to vasoconstrictor therapy and clinicians should carefully weigh the risk of adverse effects against the low likelihood of HRS reversal.
-
3.
Transjugular intrahepatic portosystemic shunt
Decompression of the portal vein by placement of transjugular intrahepatic portosystemic shunt (TIPS) is used in patients with refractory ascites and recurrent esophageal bleeding. In patients without AKI, TIPS has been associated with improvement in kidney function and it has been suggested that TIPS could be used to reverse HRS-1 [71, 72]. A systematic review and meta-analysis of 128 patients with HRS across 9 studies demonstrated a 93% rate of kidney function improvement in patients with HRS-1 [72]. Notably, TIPS was associated with an increased risk for HE [72]. In addition to the risk of HE, TIPS placement could exacerbate kidney dysfunction due to contrast-induced AKI or alteration in systemic hemodynamics [73]. Due to insufficient evidence, TIPS was not recommended for treatment of HRS-1 in separate North American practice guidelines from the AASLD and the Advancing Liver Therapeutic Approaches consortium [45, 73].
Parenchymal causes of AKI
Parenchymal causes of AKI are not only limited to the traditional causes such as acute tubular injury (ATI) and acute interstitial nephritis (AIN), but also include cirrhosis-specific (viral-associated, IgA) glomerulonephritis (GN). The clinical presentation should dictate the suspicion. Ischemic ATI can be the consequence of a prolonged state of volume depletion. As a result, all the etiologies listed as potential cause of prerenal azotemia can lead to ischemic ATI if they are not addressed and resolved in a timely fashion. In addition, ischemic ATI can directly occur in patients with sepsis secondary to SBP and other infections or in cases of septic or hemorrhagic shock. In addition, antibiotics like fluoroquinolones and vancomycin that are commonly used for prophylaxis or treatment of SBP can precipitate toxic ATI [74, 75]. Beyond the history, patients with ATI typically present with no other unique clinical features. However, muddy brown granular casts are often present on urinary sediment microscopy. On the other hand, acute GN may present with hematuria, dysmorphic erythrocyturia, and/or cellular casts, whereas AIN may present with sterile pyuria and cellular casts as well. Hypertension may be a feature of certain forms of acute GN (Fig. 2).
-
1.
Supportive therapy for ATI
Supportive care is a critical component of the management of ATI. The goal is to maintain adequate fluid, electrolyte, and acid–base balance throughout the course of the AKI. To accomplish it, careful monitoring of volume status is required by daily evaluation of fluid intake and output. Cautious administration of fluids should be considered, especially in patients with oliguria and risk of volume overload [7]. Electrolytes and acid–base status must be checked daily. Careful vigilance for development of uremia may be challenging because of confounding HE. Ultimately, the need for renal replacement therapy (RRT) should be assessed continuously [40, 76].
-
2.
Pharmacological therapy for acute GN
Although viral (hepatitis B and C) associated GN are reported in patients with cirrhosis, they commonly present with a subacute or chronic clinical course rather than AKI. However, severe cases, particularly those associated with crescentic glomerular lesions or cryoglobulinemia, can present with AKI [77, 78]. Similarly, IgA nephropathy, the most common cause of GN in cirrhosis, typically presents as an indolent or a chronic condition. However, very rarely, it can present as a rapidly progressive GN [79]. Therefore, antiviral, and immunosuppressive therapies may need to be employed to treat AKI in a patient with cirrhosis in the appropriate context.
-
3.
Drug discontinuation with/without immunosuppression for AIN
Limited literature exits regarding management of AIN in patients with decompensated cirrhosis. Extrapolating from reports in the general population, urine microscopy with leukocyturia in the absence of urinary tract infection should raise suspicion for AIN. Early identification, withdrawal of offending agents (e.g., penicillins, fluoroquinolones, proton-pump inhibitor), and initiation of corticosteroids within 7 days of drug withdrawal with persistent AKI remain the cornerstone of management [74].
Obstructive uropathy
Rare cases of tense ascites presenting as bilateral hydronephrosis and bladder outlet obstruction have been reported in patients with decompensated cirrhosis [80]. Placement of an indwelling bladder catheter and a kidney ultrasound verifying the cause of obstruction should be considered. Particular attention should be paid to medications like anticholinergics and antipsychotics that could cause detrusor sphincter dyssynergia and bladder outlet obstruction. Urinary retention and bladder outlet obstruction due to midodrine have been reported in patients with spinal cord injury [81]. Hence, midodrine should be administered with caution in patients with cirrhosis and concerns for bladder outlet obstruction.
Renal replacement therapy
In patients with decompensated cirrhosis, AKI often progresses to life-threatening kidney failure which creates the dilemma of initiating RRT in patients with exceptionally poor short-term prognosis in the absence of liver transplantation [42]. Early studies suggested that in patients with HRS-1, RRT was associated with lower short-term survival. However, more recent evidence suggests that RRT initiation should not depend on the etiology of AKI for 2 reasons. First, the outcomes in patients with liver failure and AKI due to either ATI or HRS-1 are comparably poor. A study of 472 cirrhotic patients that required RRT for AKI demonstrated that the 6-month mortality for patients not listed for LT was 85% and did not differ between ATI and HRS-1 [82]. Notably, older age, higher MELD score, and presence of critical illness were more robust predictors of mortality than the etiology of AKI [82]. Second, differentiation between ATI and HRS-1 cannot be reliably performed using currently available diagnostic approaches. [43, 83] Therefore, the decision to initiate RRT must consider conventional and liver failure–specific indications for RRT, the patient’s eligibility for liver transplantation, and the patient’s goals of care (Fig. 3). Prior to initiation of RRT, clinicians must weigh the potential benefit of RRT against the risk for RRT-related complications in the context of cirrhosis. Patients with cirrhosis are susceptible to complications which may limit both the safety and feasibility of RRT. Thrombocytopenia and coagulopathy may increase the risk of bleeding, especially during placement of central venous access. RRT may exacerbate pre-existing hemodynamic instability due to third-spacing, hemorrhage, or cardiac dysfunction [84, 85]. Filter clotting may be increased in cirrhosis, whereas systemic anticoagulation may exacerbate gastrointestinal bleeding. In addition, impaired hepatic citrate metabolism may limit the safety of regional citrate anticoagulation [85, 86].
Approach to initiation of renal replacement therapy (RRT) in patients with liver failure and acute kidney injury (AKI) unresponsive to medical management. *Liver failure–specific indications for RRT include severe hyponatremia or volume overload resulting in elevated intracranial pressure and risk of brainstem herniation. **Palliative care consultation should not be limited to individuals who are ineligible for liver transplantation.
The conventional indications for RRT in patients with AKI include hyperkalemia or volume overload refractory of medical therapy, uremia, or severe acidemia. An additional indication that specific to cirrhosis may be severe hyponatremia [84, 85]. Intermittent hemodialysis (IHD) and continuous renal replacement therapy (CRRT) are the main RRT modalities. CRRT is preferred in patients with hemodynamic instability. In contrast to IHD, CRRT allows for gradual correction of hyponatremia and does not increase intracranial pressure. Intraoperative CRRT can be performed during liver transplantation to manage perioperative volume overload and to mitigate life-threatening hyperkalemia due to large blood transfusions and liver allograft reperfusion [86,87,88]. RRT is generally appropriate as a bridge to transplantation in patients who are eligible for LT [44, 45, 89, 90]. In patients who are not listed for liver transplant, a time-limited trial of RRT may be reasonable to allow time for re-assessment of transplant candidacy, provide supportive care, and evaluate for recovery of kidney function. Palliative care consultation should be considered, and the goals of care should be addressed with the patient, family, and primary treating team prior to initiation of RRT [89, 90].
References
Tariq R, et al. Incidence, Mortality and predictors of acute kidney injury in patients with cirrhosis: a systematic review and meta-analysis. J Clin Transl Hepatol. 2020;8(2):135–42.
Gessolo Lins PR, et al. Risk factors, mortality and acute kidney injury outcomes in cirrhotic patients in the emergency department. BMC Nephrol. 2018;19(1):277.
Khatua CR, et al. Acute kidney injury in hospitalized cirrhotic patients: Risk factors, type of kidney injury, and survival. JGH Open. 2021;5(2):199–206.
Prakash J, et al. Clinical spectrum of renal disorders in patients with cirrhosis of liver. Ren Fail. 2011;33(1):40–6.
Shetty S, et al. Acute kidney injury in patients with cirrhosis of liver: Clinical profile and predictors of outcome. Indian J Gastroenterol. 2018;37(3):248–54.
Warner NS, et al. Acute kidney injury and chronic kidney disease in hospitalized patients with cirrhosis. J Investig Med. 2011;59(8):1244–51.
Russ KB, Stevens TM, Singal AK. Acute kidney injury in patients with cirrhosis. J Clin Transl Hepatol. 2015;3(3):195–204.
Kiszka-Kanowitz M, et al. Blood volume distribution in patients with cirrhosis: aspects of the dual-head gamma-camera technique. J Hepatol. 2001;35(5):605–12.
Wiese S, et al. Cirrhotic cardiomyopathy: pathogenesis and clinical relevance. Nat Rev Gastroenterol Hepatol. 2014;11(3):177–86.
Maisch B. Alcoholic cardiomyopathy : The result of dosage and individual predisposition. Herz. 2016;41(6):484–93.
Gavazzi A, et al. Alcohol abuse and dilated cardiomyopathy in men. Am J Cardiol. 2000;85(9):1114–8.
Elia C, et al. Severe acute kidney injury associated with non-steroidal anti-inflammatory drugs in cirrhosis: A case-control study. J Hepatol. 2015;63(3):593–600.
Wong F. Acute kidney injury in liver cirrhosis: new definition and application. Clin Mol Hepatol. 2016;22(4):415–22.
Angeli P, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. Gut. 2015;64(4):531–7.
Wong F. Diagnosing and treating renal disease in cirrhotic patients. Minerva Gastroenterol Dietol. 2016;62(3):253–66.
Wong PY, et al. Studies on the renin-angiotensin-aldosterone system in patients with cirrhosis and ascites: Effect of saline and albumin infusion. Gastroenterology. 1979;77(6):1171–6.
Sola-Vera J, et al. Randomized trial comparing albumin and saline in the prevention of paracentesis-induced circulatory dysfunction in cirrhotic patients with ascites. Hepatology. 2003;37(5):1147–53.
Sort P, et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341(6):403–9.
China L, et al. A randomized trial of albumin infusions in hospitalized patients with cirrhosis. N Engl J Med. 2021;384(9):808–17.
Wong F, et al. Terlipressin plus albumin for the treatment of type 1 hepatorenal syndrome. N Engl J Med. 2021;384(9):818–28.
Allegretti AS, et al. Respiratory events with terlipressin and albumin in hepatorenal syndrome: A review and clinical guidance. Liver Int. 2022;42(10):2124–30.
Argaiz ER, Koratala A, Reisinger N. Comprehensive assessment of fluid status by point-of-care ultrasonography. Kidney360. 2021;2(8):1326–38.
Velez JCQ, et al. Point-of-care echocardiography unveils misclassification of acute kidney injury as hepatorenal syndrome. Am J Nephrol. 2019;50(3):204–11.
Bucsics T, Krones E. Renal dysfunction in cirrhosis: acute kidney injury and the hepatorenal syndrome. Gastroenterology report. 2017;5(2):127–37.
Premkumar M, et al. Noninvasive estimation of intravascular volume status in cirrhosis by dynamic size and collapsibility indices of the inferior vena cava using bedside echocardiography. JGH Open. 2019;3(4):322–8.
Matsumoto N, et al. Renal vein dilation predicts poor outcome in patients with refractory cirrhotic ascites. Hepatol Res. 2018;48(3):E117-e125.
Savino JA, et al. Manipulation of ascitic fluid pressure in cirrhotics to optimize hemodynamic and renal function. Ann Surg. 1988;208(4):504–11.
Umgelter A, et al. Renal resistive index and renal function before and after paracentesis in patients with hepatorenal syndrome and tense ascites. Intensive Care Med. 2009;35(1):152–6.
Seethapathy H, et al. Acute kidney injury following paracentesis among inpatients with cirrhosis. Kidney international reports. 2020;5(8):1305–8.
Carvalho MVH, et al. Cirrhotic cardiomyopathy: the liver affects the heart. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas. 2019;52(2):e7809.
Sonny A, et al. Impact and persistence of cirrhotic cardiomyopathy after liver transplantation. Clin Transplant. 2016;30(9):986–93.
Zardi EM, et al. Portopulmonary hypertension and hepatorenal syndrome. Two faces of the same coin. Eur J Intern Med. 2017;43:22–7.
Lebrec D, et al. Pulmonary hypertension complicating portal hypertension. Am Rev Respir Dis. 1979;120(4):849–56.
Awdish RL, Cajigas HR. Early initiation of prostacyclin in portopulmonary hypertension: 10 years of a transplant center’s experience. Lung. 2013;191(6):593–600.
Ghosh S, et al. Noradrenaline vs terlipressin in the treatment of type 2 hepatorenal syndrome: a randomized pilot study. Liver Int. 2013;33(8):1187–93.
Fabrizi F, Aghemo A, Messa P. Hepatorenal syndrome and novel advances in its management. Kidney Blood Press Res. 2013;37(6):588–601.
Velez JCQ, Nietert PJ. Therapeutic response to vasoconstrictors in hepatorenal syndrome parallels increase in mean arterial pressure: a pooled analysis of clinical trials. Am J Kidney Dis. 2011;58(6):928–38.
Sagi SV, et al. Terlipressin therapy for reversal of type 1 hepatorenal syndrome: a meta-analysis of randomized controlled trials. J Gastroenterol Hepatol. 2010;25(5):880–5.
Gluud LL, et al. Systematic review of randomized trials on vasoconstrictor drugs for hepatorenal syndrome. Hepatology. 2010;51(2):576–84.
Ginès P, Schrier RW. Renal failure in cirrhosis. N Engl J Med. 2009;361(13):1279–90.
Gluud LL, et al. Terlipressin for hepatorenal syndrome. Cochrane Database Syst Rev. 2012;(9):Cd005162.
Angeli P, Bernardi M, Villanueva C, Francoz C, Mookerjee RP, Trebicka J, Krag A, Laleman W. P Gines EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69(2):406–60.
Velez JCQ, Therapondos G, Juncos LA. Reappraising the spectrum of AKI and hepatorenal syndrome in patients with cirrhosis. Nat Rev Nephrol. 2020;16(3):137–55.
Bajaj JS, et al. Acute-on-chronic liver failure clinical guidelines. Am J Gastroenterol. 2022;117(2):225–52.
Biggins SW, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021;74(2):1014–48.
Moore K, et al. Real-world treatment patterns and outcomes using terlipressin in 203 patients with the hepatorenal syndrome. Aliment Pharmacol Ther. 2020;52(2):351–8.
Arora V, et al. Terlipressin is superior to noradrenaline in the management of acute kidney injury in acute on chronic liver failure. Hepatology. 2020;71(2):600–10.
Cavallin M, et al. Terlipressin plus albumin versus midodrine and octreotide plus albumin in the treatment of hepatorenal syndrome: A randomized trial. Hepatology. 2015;62(2):567–74.
Belcher JM, et al. Terlipressin and the treatment of hepatorenal syndrome: how the CONFIRM trial moves the story forward. Am J Kidney Dis. 2022;79(5):737–45.
El-Desoki Mahmoud EI, et al. Norepinephrine is more effective than midodrine/octreotide in patients with hepatorenal syndrome-acute kidney injury: a randomized controlled trial. Front Pharmacol. 2021;12:675948.
Garcia-Martinez R, et al. Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology. 2013;58(5):1836–46.
China L, et al. Targeted albumin infusions do not improve systemic inflammation or cardiovascular function in decompensated cirrhosis. Clin Transl Gastroenterol. 2022;13(5):e00476.
Martín-Llahí M, et al. Terlipressin and albumin vs albumin in patients with cirrhosis and hepatorenal syndrome: a randomized study. Gastroenterology. 2008;134(5):1352–9.
Ortega R, et al. Terlipressin therapy with and without albumin for patients with hepatorenal syndrome: results of a prospective, nonrandomized study. Hepatology. 2002;36(4 Pt 1):941–8.
Jamil K, Pappas SC, Devarakonda KR. In vitro binding and receptor-mediated activity of terlipressin at vasopressin receptors V1 and V2. J Exp Pharmacol. 2018;10:1–7.
Cavallin M, et al. Terlipressin given by continuous intravenous infusion versus intravenous boluses in the treatment of hepatorenal syndrome: A randomized controlled study. Hepatology. 2016;63(3):983–92.
Cape KM, et al. Implementation of a protocol for peripheral intravenous norepinephrine: does it save central line insertion, is it safe? J Pharm Pract. 2022;35(3):347–51.
Jamil K, et al. Verified hepatorenal syndrome reversal as a robust multi-component primary end point: the CONFIRM study trial design. Open Access J Clin Trials. 2019;11:67–73.
Jha A, et al. Vasoconstrictor therapy in shock. BJA Educ. 2021;21(7):270–7.
Alessandria C, et al. Noradrenalin vs terlipressin in patients with hepatorenal syndrome: a prospective, randomized, unblinded, pilot study. J Hepatol. 2007;47(4):499–505.
Sharma P, et al. An open label, pilot, randomized controlled trial of noradrenaline versus terlipressin in the treatment of type 1 hepatorenal syndrome and predictors of response. Am J Gastroenterol. 2008;103(7):1689–97.
Singh V, et al. Noradrenaline vs. terlipressin in the treatment of hepatorenal syndrome: a randomized study. J Hepatol. 2012;56(6):1293–12988.
Badawy S, Meckawy N, Ahmed A. Norepinephrine versus terlipressin in patients with type 1 hepatorenal syndrome refractory to treatment with octreotide, midodrine, and albumin ( a prospective randomized comparative study). Egypt J Cardiothoracic Anesth. 2013;7(1):13–8.
Goyal O, et al. Noradrenaline is as effective as terlipressin in hepatorenal syndrome type 1: a prospective, randomized trial. J Assoc Physicians India. 2016;64(9):30–5.
Saif RU, et al. Noradrenaline versus terlipressin in the management of type 1 hepatorenal syndrome: A randomized controlled study. Indian J Gastroenterol. 2018;37(5):424–9.
Angeli P, et al. Reversal of type 1 hepatorenal syndrome with the administration of midodrine and octreotide. Hepatology. 1999;29(6):1690–7.
Tavakkoli H, Yazdanpanah K, Mansourian M. Noradrenalin versus the combination of midodrine and octreotide in patients with hepatorenal syndrome: randomized clinical trial. Int J Prev Med. 2012;3(11):764–9.
Velez JCQ. Hepatorenal syndrome type 1: from diagnosis ascertainment to goal-oriented pharmacologic therapy. Kidney360. 2022;3(2):382–95.
Piano S, et al. Association between grade of acute on chronic liver failure and response to terlipressin and albumin in patients with hepatorenal syndrome. Clin Gastroenterol Hepatol. 2018;16(11):1792-1800 e3.
Boyer TD, et al. Predictors of response to terlipressin plus albumin in hepatorenal syndrome (HRS) type 1: relationship of serum creatinine to hemodynamics. J Hepatol. 2011;55(2):315–21.
Allegretti AS, et al. Changes in kidney function after transjugular intrahepatic portosystemic shunts versus large-volume paracentesis in cirrhosis: a matched cohort analysis. Am J Kidney Dis. 2016;68(3):381–91.
Song T, Rössle M, He F, Liu F, Guo X, Qi X. Transjugular intrahepatic portosystemic shunt for hepatorenal syndrome: A systematic review and meta-analysis. Dig Liver Dis. 2018;50:323–30.
Boike JR, et al. North American practice-based recommendations for transjugular intrahepatic portosystemic shunts in portal hypertension. Clin Gastroenterol Hepatol. 2022;20(8):1636–62.
Hajji M, et al. Nephrotoxicity of ciprofloxacin: five cases and a review of the literature. Drug Saf - Case Rep. 2018;5(1):17–17.
Velez JCQ, et al. Vancomycin-associated acute kidney injury with a steep rise in serum creatinine. Nephron. 2018;139(2):131–42.
Garcia-Tsao G, Parikh CR, Viola A. Acute kidney injury in cirrhosis. Hepatology. 2008;48(6):2064–77.
Gordovskaia NB, et al. Hepatitis C virus-related cryoglobulinemic vasculitis with renal involvement: current possibilities of treatment. Ter Arkh. 2013;85(6):78–84.
Roccatello D, et al. Multicenter study on hepatitis C virus-related cryoglobulinemic glomerulonephritis. Am J Kidney Dis. 2007;49(1):69–82.
Kaneko T, et al. Two cases of rapidly progressive nephritic syndrome complicated with alcoholic liver cirrhosis. Nihon Jinzo Gakkai Shi. 2011;53(1):60–7.
Jain D, Dorairajan S, Misra M. Ascites, a new cause for bilateral hydronephrosis: case report. Sci World J. 2009;9:1035–9.
Vaidyanathan S, Soni BM, Hughes PL. Midodrine: insidious development of urologic adverse effects in patients with spinal cord injury: a report of 2 cases. Adv Ther. 2007;24(4):712–20.
Allegretti AS, et al. Prognosis of patients with cirrhosis and AKI who initiate RRT. Clin J Am Soc Nephrol. 2018;13(1):16–25.
Koola JD, et al. Development of an automated phenotyping algorithm for hepatorenal syndrome. J Biomed Inform. 2018;80:87–95.
Gonwa TA, Wadei HM. The challenges of providing renal replacement therapy in decompensated liver cirrhosis. Blood Purif. 2012;33(1–3):144–8.
Matuszkiewicz-Rowinska J, Wieliczko M, Malyszko J. Renal replacement therapy before, during, and after orthotopic liver transplantation. Ann Transplant. 2013;18:248–55.
Parmar A, et al. An evaluation of intraoperative renal support during liver transplantation: a matched cohort study. Blood Purif. 2011;32(3):238–48.
Douthitt L, et al. Perioperative use of continuous renal replacement therapy for orthotopic liver transplantation. Transplant Proc. 2012;44(5):1314–7.
Townsend DR, et al. Intraoperative renal support during liver transplantation. Liver Transpl. 2009;15(1):73–8.
Regner KR, Singbartl K. Kidney injury in liver disease. Crit Care Clin. 2016;32(3):343–55.
Velez JCQ. Patients with hepatorenal syndrome should be dialyzed? PRO. Kidney360. 2021;2(3):406–9.
Solanki P, et al. Beneficial effects of terlipressin in hepatorenal syndrome: a prospective, randomized placebo-controlled clinical trial. J Gastroenterol Hepatol. 2003;18(2):152–6.
Sanyal AJ, et al. A randomized, prospective, double-blind, placebo-controlled trial of terlipressin for type 1 hepatorenal syndrome. Gastroenterology. 2008;134(5):1360–8.
Boyer TD, et al. Terlipressin plus albumin is more effective than albumin alone in improving renal function in patients with cirrhosis and hepatorenal syndrome type 1. Gastroenterology. 2016;150(7):1579-1589.e2.
Acknowledgements
We thank Serenella A. Velez for her contribution drafting some of the illustrations.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. R. R. declares that he has no conflict of interest.
S. R. K. declares that she has no conflict of interest.
J. C. Q. V has participated in Advisory Board engagements for Mallinckrodt Pharmaceuticals (maker of terlipressin), Bayer, Travere Therapeutics, and Calliditas.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Liver.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Regner, K.R., Kanduri, S.R. & Velez, J.C.Q. Management of AKI in Patients with Cirrhosis. Curr Treat Options Gastro 20, 295–315 (2022). https://doi.org/10.1007/s11938-022-00398-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-022-00398-7