Abstract
The individual amount of alcohol consumed acutely or chronically decides on harm or benefit to a person’s health. Available data suggest that one to two drinks in men and one drink in women will benefit the cardiovascular system over time, one drink being 17.6 ml 100 % alcohol. Moderate drinking can reduce the incidence and mortality of coronary artery disease, heart failure, diabetes, ischemic and hemorrhagic stroke. More than this amount can lead to alcoholic cardiomyopathy, which is defined as alcohol toxicity to the heart muscle itself by ethanol and its metabolites. Historical examples of interest are the Munich beer heart and the Tübingen wine heart. Associated with chronic alcohol abuse but having different etiologies are beriberi heart disease (vitamin B1 deficiency) and cardiac cirrhosis as hyperdynamic cardiomyopathies, arsenic poising in the Manchester beer epidemic, and cobalt intoxication in Quebec beer drinker’s disease. Chronic heavy alcohol abuse will also increase blood pressure and cause a downregulation of the immune system that could lead to increased susceptibility to infections, which in turn could add to the development of heart failure. Myocardial tissue analysis resembles idiopathic cardiomyopathy or chronic myocarditis. In the diagnostic work-up of alcoholic cardiomyopathy, the confirmation of alcohol abuse by carbohydrate deficient transferrin (CDT) and increased liver enzymes, and the involvement of the heart by markers of heart failure (e.g., NT-proBNP) and of necrosis (e.g., troponins or CKMb) is mandatory. Treatment of alcoholic cardiomyopathy consists of alcohol abstinence and heart failure medication.
Zusammenfassung
Die individuelle Menge akut oder chronisch getrunkenen Alkohols ist für den gesundheitlichen Schaden oder Nutzen entscheidend. Grenzdosen für Männer sollten 1–2 Getränke à 17,6 ml reinen Alkohols sein, für Frauen ein Getränk. Mäßiger Alkoholkonsum kann die Inzidenz und Mortalität von koronarer Herzerkrankung, Herzinsuffizienz, Diabetes mellitus, ischämischem und hämorrhagischem Schlaganfall vermindern. Größere Mengen Alkohol führen zur alkoholischen Kardiomyopathie, bedingt durch die Toxizität von C2H5OH und seinen Metaboliten auf den Herzmuskel. Historische Beispiele sind das Münchener Bier- und das Tübinger Weinherz. Nicht auf die reine Alkoholwirkung zurückzuführen sind aufgrund ihrer andersartigen Ätiologie das Beriberi-Herz bei Mangel an Thiamin (Vitamin B1) und die kardial mitbedingte Leberzirrhose als hyperdyname Kardiomyopathien, die Arsenvergiftung bei der Manchester Biertrinkerepidemie und die nach Quebec benannte Bierherzerkrankung infolge einer Kobaltintoxikation. Chronischer Alkoholabusus erhöht den Blutdruck und verursacht eine Downregulation des Immunsystems mit erhöhter Infektanfälligkeit. Histologisch ist die alkoholische nicht von der idiopathischen Kardiomyopathie und einer chronischen Myokarditis zu unterscheiden. Alkoholabusus wird durch Bestimmung des carbohydratdefizienten Transferrins (CDT) und erhöhter Leberenzyme bestätigt, die Herzinsuffizienz durch Biomarker wie NT-proBNP und die Myozytolyse durch Troponine und CKMb. Die Behandlung der alkoholischen Kardiomyopathie besteht in der Alkoholabstinenz und medikamentöser Therapie der Herzinsuffizienz.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Alcoholism—use and abuse
According to the definition of the World Health Organization (WHO), alcoholism is subgrouped in two categories: alcohol abuse and alcohol dependence [1]. This corresponds roughly with the concept of the American Psychiatric Association [2, 3]. Alcohol abuse describes the psychological dependence on ethanol for adequate functioning together with occasional heavy consumption, while alcohol dependence is defined as an increased alcohol tolerance together with physical symptoms upon withdrawal. In Western countries it is estimated that up to 10 % of the adult population suffers from alcoholism [4]. The highest prevalence is detected in the third to fifth decade of life, and alcoholism is seen in all races, ethnic groups, and socioeconomic strata.
Germany with a total population of 81 million inhabitants is a permissive society with respect to the drinking of alcohol. Alcohol consumption is part of the local culture. About 40 million individuals drink alcohol. The per capita alcohol consumption of 9.7 l pure ethanol and the early onset of regular or episodic intensive drinking among young people in Germany consequently leads to high alcohol-related morbidity and mortality [5].
More than 1.8 million individuals in Germany with a total population of 81 million inhabitants are alcohol dependant. For an additional 1.6 million persons the use of alcohol is harmful [6, 7]. In a world-wide setting, alcohol use disorders show similarities in developed countries, where alcohol is cheap and readily available [8]. The many complications of alcohol use and abuse are both mental and physical—in particular, gastrointestinal [9], neurological [10, 11], and cardiological [12, 13]. The relationship of alcohol with heart disease or dementia is complicated by the fact that moderate alcohol consumption was shown not only to be detrimental but to a certain degree also protective against cardiovascular disease [14] or to cognitive function in predementia.
We reviewed the effects of ethanol on the cardiovascular system in 1996 [15], including aspects of inflammation [16], rhythm disturbances [17], and hypertension [18]. In 2001 we updated the data on the ambivalent relationship between alcohol and the heart [19] and in 2008 added new evidence on a larger cohort of patients with different forms of cardiomyopathy and increased alcohol intake from the German competence network on heart failure [20].
This review revisits our past and deals with our current thinking on the epidemiology, pathophysiology, clinical characteristics, and treatments available for alcoholic cardiomyopathy.
Methods
This review assembles and selects pertinent literature on the ambivalent relationship of ethanol and the cardiovascular system, including guidelines, meta-analyses, Cochrane reviews, original contributions, and data from the Marburg Cardiomyopathy registry.
Drinks as measures of alcohol are often given in ounces (oz), whereby 1 oz equals 28.35 g or 29.57 ml.
Examples for 100 % alcohol in ml of one drink in consumed beverages are between 17.6 to 17.76 ml:
-
Beer: 12 fluid ounces of 5 % beer = 355 ml fluid = 17.5 ml 100 % alcohol.
-
Wine: 5 fluid ounces of 12 % wine = 148 ml fluid = 17.76 ml of 100 % alcohol.
-
Distilled spirits: 1.5 fluid ounces of ~40 % liquor = 44 ml = 17.6 ml of 100 % alcohol.
A historical perspective
For more than 3000 years, alcoholic beverages have been consumed in multiple societies through the centuries and cultures. The name alcohol is much younger than the many beverages containing it. Pulverized antimony was used as eye shadow by Egyptian women and named al-Kol. In the 16th century Paracelsus Theophrastus Bombastus from Hohenheim used this term for distilled liquor and called it alcohol [15]. The beneficial cardiovascular effects of alcohol have been appreciated, e. g., in medieval times, when people took advantage of the vasodilating properties of alcohol to treat angina pectoris or heart failure. So Hildegard von Bingen (1098–1179), one of the most prominent mysticians of her time, recommended her heart wine as a universal remedy. One liter of wine was cooked for 4 min with 10 fresh parsley stems, 1 spoon of vinegar, and 300 g honey and then filtered [11]. This recipe is still in use today.
Over the centuries “the good and the bad” of alcohol were evaluated clinically and scientifically. As early as 1855, Wood incriminated alcohol as a cause of heart failure. In 1861, Friedrich reported idiopathic hypertrophy as associated with alcoholism. In 1873, Walshe described myocardial cirrhosis in alcoholics, which includes a spectrum of hepatic derangements that occur in the setting of right-sided heart failure. Conversely cirrhosis (fibrosis) was found both in heart and liver. High cardiac output in patients with liver cirrhosis may have contributed to this cardiomyopathy in a vicious circle. The term “wine heart” (Tübinger Weinherz) originated in 1877 by Münzinger [21], a German pathologist at Tübingen university. This entity we would call nowadays “alcoholic cardiomyopathy” with histologic features of dilatation, myofibrillar necrosis and fibrosis (Fig. 1a), and ultrastructural changes such as reduction of myofibrils and mitochondriosis in a great variability of size and form (Fig. 1b; [22]).
a Left ventricle from a 49-year-old man with chronic alcohol abuse. Myofibers show partly hypertrophy and atrophy. Fibrosis is present as reparative interstitial and perivascular fibrosis. HE ×320. b Electron microscopy of an endomyocardial septal biopsy from a patient with alcoholic cardiomyopathy demonstrating myofibrillar reduction and variable mitochondriae in size but increased in number. ×2190. (With kind permission from H. Frenzel and B. Schwartzkopff [22])
In Munich, the annual consumption of beer reached 245 l per capita and year in the last quarter of the 19th century. In 1884, the pathologist and veterinarian Otto von Bollinger (Fig. 2a) described the “Munich beer heart” with fibrosis, hypertrophy, and fatty degeneration in postmortem cardiac tissue of alcoholics who consumed an estimated average of 432 liters of beer per year (Fig. 2b; [23]). At that time every 10th necropsy in men at the Munich pathology institute named cardiac dilatation and fatty degeneration as “Bierherz” being its underlying cause. For comparison, the mean annual beer consumption in Bavaria is nowadays estimated to be 145 l and in the rest of Germany around 100 l beer per person and year [24].
In 1887, Maguire reported on 2 patients with severe alcohol consumption who benefitted from abstinence. He suggested that alcohol was poisoning the heart. In 1890, Strümpell listed alcoholism as a cause of cardiac dilatation and hypertrophy, as did Sir William Osler in 1892 in his textbook Principles and Practices of Medicine. In 1893, Graham Steell, well known for the Graham Steell murmur due to pulmonary regurgitation in pulmonary hypertension or in mitral stenosis, reported 25 cases in whom he recognized alcoholism as one of the causes of muscle failure of the heart. He found it “a comparatively common one” [25]. In his 1906 textbook The Study of the Pulse, William MacKenzie described cases of heart failure attributed to alcohol and first used the term “alcoholic heart disease” [26].
In his 1972 review article, Bridgen was the first to introduce the term alcoholic cardiomyopathy [27].
Nutritional causes of “alcoholic” cardiomyopathy
Beriberi heart disease
Thiamine deficiency is common feature in a malnourished and/or alcoholic population. Thus, the concept of beriberi heart disease dominated thinking about alcohol and the heart for decades and caused many to doubt that alcohol was actually cardiotoxic [28]. But vitamin B1 (thiamine) deficiency is accompanied by an elevated cardiac output and diminished peripheral vascular resistance [29, 30]. According to its central hemodynamics, it can be classified as hyperdynamic cardiomyopathy or high output failure with a cardiac output >8 l/min or a cardiac index >3.9 l/min/m2 [31, 32]. In contrast, alcoholic cardiomyopathy is characterized by a low cardiac output, associated with systemic vasoconstriction [4]. However, the high output state can lead to cardiac dilation, thus, representing a characteristic subentity of cardiomyopathy different from low output dilated cardiomyopathy. Therefore, thiamine deficiency per se is just a historical nutritional anomaly in the history of alcoholic cardiomyopathy.
Manchester arsenic-in-beer epidemic
In 1900, the Manchester arsenic-in-beer epidemic was a serious food poisoning outbreak affecting several thousand people across the North-West and Midlands of England, with many cases proving fatal. The arsenic had come from the glucose for which sulphuric acid was used in the sugar production process of a company in Leeds. Brewers had been using this sugar, thus, unknowingly poisoning the beer and as a result their customers for many years even prior to the epidemic [33]. Arsenic poising caused a multisystem disease in over 6000 cases with more than 70 deaths [34]. The syndrome included the usual signs and symptoms of arsenic poisoning, with skin, nervous system, and gastrointestinal manifestations. Unusual in arsenic poisoning, but especially prominent in this epidemic, were the cardiovascular findings. In his clinical description, Ernest Reynolds wrote that “cases were associated with so much heart failure and so little pigmentation that they were diagnosed as beri-beri …”. He also found that “undoubtedly the principal cause of death has been cardiac failure. In postmortem examinations, the only prominent signs were the interstitial nephritis and the dilated flabby heart” (p. 169, [35]). This outbreak had been the first known trace metal cardiotoxic syndrome.
In 2013, the issue of arsenic in beer and wine was again prominent, when Mehmet Coelhan, a researcher at the Weihenstephan research center at the Technical University of Munich, reported at a meeting of the American Chemical Society that many of the nearly 360 beers tested in Germany had trace amounts of arsenic. The source was identified to be the filter of choice for wine and beer, i.e., diatomaceous earth [36]. The German word for it is Kieselguhr, a beige powder made up of the skeletons of diatoms. The trace amounts of arsenic have not been comparable to the arsenic-in-beer endemic in Manchester but may still reach up to 10-times the amount admitted for arsenic in drinking water in the European Union and the US.
Quebec‘s beer drinker disease
In the mid-1960s, another unexpected heart failure epidemic among chronic, heavy beer drinkers occurred in two cities in the USA, in Quebec, Canada, and in Belgium. It was characterized by congestive heart failure, pericardial effusion, and an elevated hemoglobin concentration. The explanation proved to be the addition of small amounts of cobalt chloride. Cobalt was used as a foam stabilizer by certain breweries in Canada and in the USA. In 1966 McDermott et al. [37] described the syndrome as myocardosis with heart failure, Kestelott et al. [38] added pericardial involvement and named it alcoholic pericardiomyopathy, and Morin and Daniel [39] in Quebec tracked down the etiology to cobalt intoxication to what become known as Quebec beer-drinkers cardiomyopathy. Human pathology was first described by Bonefant et al. [40]. Animal models investigated ultrastructure [41] and treatment e. g. by selenium [42]. Removal of the cobalt additive ended the epidemic in all locations. Cobalt poisoning and alcohol together acted synergistically in these patients. As the syndrome could be attributed to the toxicity of this trace element, the additive was prohibited thereafter.
Not alcohol but cobalt itself recently caused severe heart failure in a 55-year-old man, who was referred to the university hospital in Marburg to rule out coronary artery disease as the cause of his heart failure. He had become almost deaf and blind, with fever of unknown cause, hypothyroidism, and enlarged lymph nodes. Both his hips had been replaced, the left side by a CoCrMo Protasul metal prosthesis. Remembering a similar case in an episode of the TV series Dr. House, the team of J. Schäfer suspected cobalt intoxication as the cause of heart failure, which clinically mimicked Quebec‘s beer drinker disease [43]. One should note, however, that cobalt is needed in minute amounts of 0.0003 mg/day in vitamin B12 (cobalamine) to avoid megaloblastic anemia.
Cardiac cirrhosis or cirrhotic cardiomyopathy
The heart and liver interact in several different ways. Acute or chronic right heart failure leads to elevation of liver enzymes most likely due to liver congestion, whereas cirrhosis due to cardiac disease is infrequent. Chronic liver disease such as cirrhosis may in turn affect the heart and the whole cardiovascular system, leading to a syndrome named cirrhotic cardiomyopathy (CCM). Thus, CCM has been introduced as an new entity separate of the cirrhosis etiology. Increased cardiac output due to hyperdynamic circulation, left ventricular dysfunction (systolic and diastolic), and certain electrophysiological abnormal findings are pathophysiological features of the disease. The underlying mechanisms might include the impaired β‑receptor and calcium signaling, altered cardiomyocyte membrane physiology, elevated sympathetic nervous tone and increased activity of vasodilatory pathways [44]. In pathophysiological terms, heart failure in liver cirrhosis belongs to the hyperdynamic cardiomyopathies.
Hypertension
As early as in 1915, Lian [45] reported in middle-aged French servicemen during the first world war that heavy drinking could lead to hypertension. It took almost 60 years before further attention was paid to the complex interaction between the heart and the peripheral vasculature in various cross-sectional and prospective epidemiologic studies, which have empirically confirmed this early report. One is aware today that alcohol may cause an acute but transient vasodilation, which may lead to an initial fall in blood pressure probably mediated by the atrial natriuretic peptide (ANP) [46]. But also short- and long-term pressor effects mediated by the renin–aldosterone system and plasma vasopressin have been described [47, 48].
The long-term hypertensive effect of alcohol has been confirmed in many studies [49–52]. Remarkably, alcohol also interacts with brain stem receptors and exerts thereby central hypertensive effects [18]. The apparent threshold amount of drinking associated with higher blood pressure is approximately 3 drinks/day. Most studies show no increase in blood pressure with lighter drinking; several show an unexplained J‑shaped curve in women with lowest blood pressures in lighter drinkers. There seems to be independence from adiposity, salt intake, education, smoking, beverage type (wine, liquor, or beer), and several other potential confounders.
Clinical observation confirmed that several days to weeks of drinking show higher and weeks of abstinence lower pressures. Alcohol intake may also interfere with the drug and dietary treatment of hypertension. This altogether supports a causal relationship between alcohol consumption and a hypertensive state.
Alcoholic cardiomyopathy: Cytotoxicity of alcohol on heart muscle
The 1989 landmark report of Urbano-Marquez et al. [53] showed a clear relation of lifetime alcohol consumption to structural and functional myocardial and skeletal muscle abnormalities in alcoholics. The amount of consumed alcohol was large—the equivalent of >80 g alcohol/day for 20 years. Further evidence came from data on acute alcohol effects [54] and from clinical observation [55–57].
In 1996, cardiomyopathies were defined as diseases ”affecting the myocardium with associated cardiac dysfunction“ [58] and primary and secondary forms were distinguished in this context. After consumption of large quantities of alcohol over years the clinical picture of heavy alcohol drinkers could be indistinguishable from other forms of dilated or familial cardiomyopathy. Alcohol is still suspected to be the major cause or contributory factor of secondary nonischemic dilated cardiomyopathy being involved in up to one third of all cases of dilated cardiomyopathy [59–61]. In alcoholic cardiomyopathy, dilation and impaired contraction of the left or both ventricles is observed [4]. Left ventricular enddiastolic diameters are increased compared to age- and weight-matched controls [62], the left ventricular mass index is increased [63], and the left ventricular ejection fraction is well below normal (<45 %). Thus, the diagnosis of alcoholic cardiomyopathy is still based on the coincidence of heavy alcohol consumption and a global myocardial dysfunction, which cannot be explained by any other underlying myocardial disease [64]. However, the prevalence of alcoholic cardiomyopathy may be underestimated, as autopsy findings reveal pathologic changes of the heart in individuals with no clinical symptoms [65], when analyzing in large cross-sectional studies.
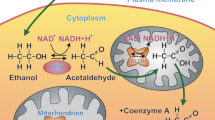
Further evidence suggests that not only ethanol but also the first metabolite acetaldehyde may directly interfere with cardiac and skeletal muscle homeostasis [53, 66]. In vitro studies have further elucidated the direct effect of ethanol on electromechanical coupling, indicating a decrease in myofilament–calcium sensitivity during alcohol consumption, changes in the transmembrane action potential, the amplitude of the cytosolic calcium transients, and the shortening of the action potential duration [67–71]. Isolated cardiomyocytes of alcohol-fed rats did not maintain ATP levels upon energy demand due to an inadequate increase in mitochondrial ATP-synthase activity, which led altogether to further myocyte loss [72, 73]. Ultrastructural disarray of the contractile apparatus [74] is associated with a depressed myofibrillar and sarcoplasmic protein synthesis in cardiac muscle after ethanol exposure [75–77]. This reduces contractile cardiac filaments with subsequent negative inotropic effects on heart contractility [78, 79]. An apoptotic effect of ethanol on cardiac muscle has also been described, which could be counteracted by insulin-like growth factor (IGF)-I [80] and confirmed in later studies [81, 82]. In a study in rats that were fed with two different doses of alcohol (5 mM [low alcohol], 100 mM [high alcohol] or in pair-fed nonalcohol controls for 4–5 months), caspase-3 activity as putative marker of apoptosis was decreased in the low alcohol diet, which went along with increased or normal contractility, whereas high doses of ethanol showed increased caspase activity, wall thinning, and a reduction of shortening velocity [83]. Of note, rats are a relatively alcohol resistant species.
Alcohol and myocarditis
Alcohol abuse coinciding with myocarditis was reported in 1902 by McKenzie [26]. In endomyocardial biopsies of alcoholics up to 30 % of patients were found to exhibit sparse lymphocytic infiltrates with myocyte degeneration and focal necrosis and increased HLA (human leukocyte antigen) or ICAM (intercellular adhesion molecule) expression (Fig. 3; [16, 84]).
a Left ventricle (LV) biopsy of a 53-year-old individual with an alcohol consumption of >5 drinks/day for 32 years. Perivascular increase of leukocytes and fibrosis, myocytes in variable sizes with some myocytolysis. HE ×160. b LV biopsy of the 53-year-old alcoholic with increased ICAM (intercellular adhesion molecule) expression in capillaries and small vessels. ×320. c Circulating antimyosin antibodies in the 53-year-old patient with alcoholic abuse. Indirect immunofluorescent test. Titer 1:160 ×640
This may have to do with the susceptibility for infections due to a suppressed immune system in a compromised human host and also in experimental animal [85]. Ethanol can alter lymphocyte functions, inhibit neutrophil chemotaxis, and suppress the production of cytokines, which are involved in regulating acute inflammatory responses to infectious challenges [86–88]. Furthermore, autoimmunity and circulating autoantibodies seem to be associated in some patients with chronic alcohol consumption [16, 20, 84].
Coronary artery disease and atherosclerosis
The beneficial heart wine as universal remedy in medieval ages by Hildegard von Bingen [11] found its later correlates in many observations at the beginning of modern medicine when coronary artery disease (CAD) and its risk factors and symptoms received more attention. Heberden [89] described angina so elegantly in 1786 and also added that ”considerable relief“ through ”wine and spirituous liquors“ could be expected. This observation led to the erroneous belief that alcohol is an immediate coronary vasodilator. Alcohol is not a direct coronary vasodilator [90]. Symptomatic relief of angina could be through the anesthetic effect of ethanol or through peripheral vasodilation, which could transiently reduce oxygen demand of the heart.
In 1819 the Irish physician Dr. Samuel Black, who had a special interest in angina pectoris described what is probably the first commentary pertinent to the ”French Paradox“ [91]. This refers to the finding in the last century that moderate alcohol consumption could be the reason for the relatively low cardiovascular disease incidence in wine-drinking regions [92]. Renaud and de Lorgeril [93] suggested that the inhibition of platelet reactivity by wine may be one explanation for protection from CAD in France. However, there was further evidence on this and other dietary mechanisms with the observation that France and Finland have similar intakes of cholesterol and saturated fat, but consumption of vegetables and vegetable oil containing monounsaturated and polyunsaturated fatty acids is greater in France than in Finland.
This inverse relation on mortality resembles in most population based studies a U- or J-shaped curve: Total abstinence has a slightly increased mortality when compared to low or moderate alcohol consumption. It is present in individuals with and without overt CAD, with diabetes, and with hypertension and has been underlined by a large number of studies [94, 95]. The cardioprotective effect of alcohol can be attributed to the increase in total high-density lipoproteins (HDL), and especially by an increase in subfractions HDL2 and HDL3, whereas established cardiovascular risk factors like low-density lipoproteins (LDL) or lipoprotein(a) are thought to be moderately decreased [96]. Moderate alcohol intake also exerts beneficial effects on the blood coagulation system. It leads to an increase of endogenous plasminogen activators [97], or a decrease in fibrinogen concentrations [98].
In the Caerphilly prospective heart disease study, platelet aggregation induced by adenosine diphosphate was also inhibited in subjects who drank alcohol [99]. Assessing differences between various forms of alcoholic beverages it should be noted that resveratrol leads in vitro to platelet inhibition in a dose-dependent manner [100] and has shown effects on all-cause mortality in a community-based study [101]. Polyphenols of red barrique wines and flavonoids have been shown to inhibit endothelin-1 synthase [102] and PDGF-induced vasoproliferation thus also contributing to cardiovascular protection [103].
Signal transduction and beta-receptors
In alcoholic cardiomyopathy, similar to idiopathic dilated cardiomyopathy (DCM), beta 1‑adrenergic and muscarinic receptors are reduced in the myocardium itself and reduced responsiveness of the adenyl cyclase was shown, whereas catecholamine levels in the circulation may be elevated [104]. As a net effect, negative inotropism may result and contribute to heart failure.
Arrhythmias and stroke
Acute effects of alcohol can result in rhythm disturbances. Since this happens often on weekends and holidays, Ettinger and Regan coined the term ”holiday heart syndrome“, when they described 32 habitual drinkers with an additional ingestion of ethanol prior to the arrhythmia [59, 105]. Atrial fibrillation was the commonest manifestation, which resolved with abstinence. In the Kaiser Permanente Study, atrial arrhythmias in 1322 persons reporting >6 drinks per day were compared to arrhythmias in 2644 matched light drinkers, showing a doubled relative risk for heavy drinkers [106]. Apart from direct cardiotoxicity, hypertension causing atrial stretch the arrhythmogenic potential of alcohol may come from the lowering the resting membrane potential [107] and the prolongation of conduction [108].
Studies of alcohol and stroke are complicated by the various contributing factors to stroke. Heavier drinkers are apparently at a higher risk of hemorrhagic stroke, whereas moderate drinking might be neutral or even result in a reduced risk of ischemic stroke.
Clinical work-up for alcoholic cardiomyopathy
Habitual drinkers often hide their alcohol dependence fairly effectively. They may admit drinking at social events but not the abuse in the first contact. Patients with alcoholic cardiomyopathy, therefore, usually present with symptoms of heart failure, i. e., dyspnea, orthopnea, edema, nocturia, and tachycardia. Echocardiography may reveal a mild or severe depression of cardiac function and ejection fraction or even show hypertrophy in the beginning [109]. Heart failure symptoms may be due to early diastolic or to later systolic dysfunction. At later stages, due to atrial fibrillation, thrombi are not uncommon in the dilated atria. Mitral regurgitation is found in up to two thirds of cases [110]. Atrial fibrillation and supraventricular tachyarrhythmias are common findings in 15–20 % of patients [111], whereas ventricular tachycardias are rare [112]. On ECG, unspecific abnormalities like complete or incomplete left bundle branch block, atrioventricular conduction disturbances, alterations in the ST segment, and P wave changes can be found comparable to those in idiopathic DCM [113].
On endomyocardial biopsy, a discrimination between idiopathic, chronic inflammatory and alcoholic cardiomyopathy is virtually impossible since common features such as fibrosis, hypertrophy of cardiac myocytes, and alterations of nuclei are present at light microscopy in the alcoholic cardiomyopathy [114] as well as in chronic myocarditis according to the Dallas criteria [115] or the World Heart Federation/International Society and Federation of Cardiomyopathy (WHF/ISFC) definition of myocarditis [116]. Although the severity of histological alterations on endomyocardial biopsy correlates with the degree of heart failure in one of our studies, biopsy is not in common use for prognostic purposes [117]. Even the recovery after abstinence of alcohol is hard to predict based on morphometric evaluation of endomyocardial biopsies [118].
Cardiac MRI may be helpful in the differential diagnosis to hypertrophic cardiomyopathy, storage diseases, and inflammatory cardiomyopathy. For a comprehensive overview see Table 1 (combined data from [6, 8, 24, 28]).
Laboratory findings
Measuring blood alcohol concentration in an acute intoxication gives baseline information but does not permit deductions to chronic misuse. Markers for chronic alcohol consumption rely on liver enzymes such as gamma-glutamyltransferase (GGT) [119], glutamic oxalacetic transaminase (GOT), and glutamic pyruvic transaminase (GPT). Elevations of the transaminases (GOT, GPT), especially a ratio of GOT/GPT higher than 2 might be indicative of alcoholic liver disease instead of liver disease from other etiologies [120, 121]. An excellent marker is carbohydrate deficient transferrin (CDT), which best detects chronic alcohol consumption alone [122, 123] or in combination with the other markers such as GGT [8, 124]. Markers such as ethyl sulphate, phosphatidyl ethanol, and fatty acid ethyl esters are not routinely done. For a comprehensive overview see Table 2 with combined data from [6, 8, 24, 28].
Biomarkers of heart failure such as NT-proBNP and of myocardial necrosis such as the troponins and CKMB indicate heart failure or myocytolysis.
Is there an immediate risk of alcohol intake?
In a recent meta-analysis, Mostofsky et al. [125] analyzed if independent from habitual moderate or heavy alcohol consumption an immediate risks exists following alcohol intake. Data from 23 studies with 20,457 participants showed that even with moderate consumption an immediately higher cardiovascular risk was attenuated after 24 h. It then became protective for myocardial infarction and hemorrhagic stroke with a 30 % lower risk and protective against ischemic stroke within one week. In contrast, heavy alcohol drinking continued to be associated with higher cardiovascular risk in the following day (RR =1.3–2.3) and week (RR =2.25–6.2).
Prognosis and treatment
Prognosis in individuals with low or moderate consumption up to one or two drinks per day in men and one drink in women is not different from people who do not drink at all. In CAD, diabetes, and stroke prevention the J‑type mortality curves even indicate some benefit apart from the social ”well-being“. In patients with chronic alcohol use disorders and severe heart failure prognosis is poor, since continued alcohol abuse results in refractory congestive heart failure. Death might also be sudden due to arrhythmias, heart conduction block, and systemic or pulmonary embolism. In these patients, only early and absolute abstinence of alcohol can reverse myocardial dysfunction [56, 57, 126] which in a historic study by McDonald and Burch was achieved with prolonged bedrest for several months without further access to alcoholic beverages. This was an excellent result long before ACE inhibitors or betablockers were available for heart failure treatment [57]. Mortality can otherwise reach 40–50 % within a 4–5 year period in the nonabstinent patients [127], whereas after withdrawal from alcohol hemodynamic and clinical improvement or at least a slower progression of disease compared to the idiopathic form of dilated cardiomyopathy was shown [128, 129].
To maintain abstinence, recent investigations suggest the benefits of adjuvant medications, e. g., naltrexone, which is an opiate receptor antagonist that blocks endogenous opioid reward and reduces alcohol-cue-conditioned reinforcement signals; acamprosate, an agent that exerts action through excitatory amino acids; by disulfiram, an aldehyde dehydrogenase inhibitor, which causes in alcohol use acetaldehyde accumulation and symptoms such as nausea, flushing, sweating, and tachycardia or by selective serotonin re-uptake inhibitors (SSRI) [8, 130, 131]. To treat the alcohol problem, a combined approach comprising pharmacologic and psychosocial therapy involving self-help groups or Alcoholics Anonymous is essential.
Treatment of alcoholic cardiomyopathy follows the usual regimen for therapy of heart failure, including ACE inhibitors, betablockers, diuretics including spironolactone or eplerinone, and digitalis in atrial fibrillation for rate control together with anticoagulation, whenever appropriate (Table 3). Caution for anticoagulation is warranted due to the problems of noncompliance, trauma, and overdosage especially in hepatic dysfunction.
Conclusion
The individual amount of alcohol consumption decides on harm or benefit. The preponderance of data suggests that drinking one to two drinks in men and one drink in women will benefit the cardiovascular system over time. More than this amount can lead to alcoholic cardiomyopathy. Moderate drinking below that threshold might even reduce the incidence of coronary artery disease, diabetes, and heart failure.
References
Madden JS (1993) The definition of alcoholism. Alcohol 28:617–620
Schuckit MA, Hesselbrock V, Tipp J et al (1994) A comparison of DSM-III-R, DSM-IV and ICD-10 substance use disorders diagnoses in 1922 men and women subjects in the COGA study. Addiction 89:1629–1638
Hasin D, McCloud S, Li Q, Endicott J (1996) Cross-system agreement among demographic subgroups: DSM-III, DSM-III-R, DSM-IV and ICD-10 diagnoses of alcohol use disorders. Drug Alcohol Depend 41:127–135
Preedy VR, Atkinson LM, Richardson PJ, Peters TJ (1993) Mechanisms of ethanol-induced cardiac damage. Br Heart J 69:197–200
Batra A, Müller CA, Mann K, Heinz A (2016) Abhängigkeit und schädlicher Gebrauch von Alkohol. Dtsch Arztebl 113:301–310
Mann K, Hoch E, Batra A (2015) S3-Leitlinie Screening, Diagnose und Behandlung alkoholbezogener Störungen. Springer, Heidelberg
Wodarz N, Mann K, Hoch E et al (2016) S3 Leitlinie: Alkoholbezogene Störungen, Screening, Diagnose und Behandlung. Bayerisches Ärztebl 2016(4):144–149
Connor JP, Huber PS, Hall WD (2016) Alcohol use disorders. Lancet 387:988–998
Rocco A, Compare D, Angrisani D et al (2014) Alcoholic disease: Liver and beyond. World J Gastroenterol 20:14652–14659
Solfrizzi V, D‘Introno A, Colacicco AM et al (2007) Alcohol consumption, mild cognitive impairment, and progression to dementia. Neurology 68(21):1790–1799
Panza F, Capurso C, D’Introno A et al (2009) Alcohol drinking, cognitive functions in older age, predementia, and dementia syndromes. J Alzheimers Dis 17(1):7–31
Gonçalves A, Claggett B, Jhund PS, Rosamond W (2015) Alcohol consumption and risk of heart failure: The Atherosclerosis Risk in Communities study. Eur Heart J 36:939–945
Goncalves A, Jhund PS, Glaggett B et al (2015) Relationship between alcohol consumption and cardiac structure and function in the elderly. The atherosclerosis risk in communities study. Circ Cardiovasc Imaging 8:e002846. doi:10.1161/CIRCIMAGING.114.002846
George A, Figueredo VM (2011) Alcoholic cardiomyopathy: A review. J Cardiac Fail 17:844–849
Maisch B (1996) Alcohol and the heart. Herz 21:207–212
Wilke A, Kaiser A, Ferency I, Maisch B (1996) Alcohol and myocarditis. Herz 21:248–257
Menz V, Grimm W, Hoffmann J, Maisch B (1996) Alcohol and rhythm disturbance: The Holiday Heart syndrome. Herz 21:227–231
Rupp H, Brilla CG, Maisch B (1996) Hypertension and alcohol: Central and peripheral mechanisms. Herz 21:258–264
Schoppet M, Maisch B (2001) Alcohol and the heart. Herz 26:345–352
Maisch B, Gelbrich G, Pankuweit S et al (2008) Alcohol and heart failure. Eur Heart J 29(Abstr Suppl):553
Münzinger (1877) Das Tübinger Herz. Ein Beitrag zur Lehre von der Überanstrengung des Herzens. Dtsch Arch Klin Med 19:449
Frenzel H, Schwartzkopff B (2000) Toxische Schäden des Herzens durch Alkohol, Anthrazykline und Kokain. In: Hort W (ed) Pathologie des Endokard, der Kranzarterien und des Myokard, 1st edn. vol 22/2. Springer, Berlin, pp 1175–1228
von Bollinger O (1884) Über die Häufigkeit und Ursachen der idiopathischen Herzhypertrophie in München. Dtsch Med Wochenschr 10:180
https://www.hdbg.eu. Accessed 8 Aug 2016
Steell G (1893) Heart failure as a result of chronic alcoholism. Med Chron Manchester 18:1–22
MacKenzie J (1902) The Study of the Pulse. Y. J. Pentland, Edinburgh, p 237
Brigden W, Robinson J (1964) Alcoholic heart disease. Brit Med J 2:1283–1289
Aalsmeer WC, Wenckebach KF (1929) Herz und Kreislauf bei der Beri Beri Krankheit. Wien Arch Inn Med 16:193–272
Akbarian M, Yankopoulos NA, Abelmann WH (1966) Hemodynamic studies in Beriberi heart disease. Am J Med 414(2):197–212
Djoenaidi W, Notermans SL, Dunda G (1992) Beriberi cardiomyopathy. Eur J Clin Nutr 46:227–234
Mehta PA, Dubrey SW (2009) High output failure. Q J Med 102:235–241
Hunt SA, Abraham WT, Chin MH et al (2005) ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult-summary article a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (writing committee to update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 46:1116–1143
Kelynack TN, Kirkby W (1901) Arsenical poisoning in beer drinkers. Baillière, Tyndall & Cox, London
Royal Commission Appointed to Inquire into Arsenical Poisoning from the Consumption of Beer and other Articles of Food or Drink (1903) ”Final Report“ Part I. Wyman and Sons, London
Reynolds ES (1901) An account of the epidemic outbreak of arsenical poisoning occurring in beer drinkers in the north of England and the midland counties in 1900. Lancet 157(4038):166–170
http://www.npr.org/sections/thesalt/2013/04/08/176587506/arsenic-in-beer-may-come-from-widely-used-filtering-process. Accessed 8 Aug 2016
McDermott PH, Delaney RL, Egan JD, Sullivan JF (1966) Myocardosis and cardiac failure in men. JAMA 198(3):253–256
Kesteloot H, Terryn R, Bosmans P, Joossens JV (1966) Alcoholic perimyocardiopathy. Acta Cardiol 21(3):341–357
Morin Y, Daniel P (1967) Quebec beer-drinkers‘ cardiomyopathy: Etiologic considerations. Can Med Assoc J 97:926–928
Bonenfant JL, Miller G, Roy PE (1967) Quebec beer-drinkers’ cardiomyopathy: pathologic studies. Can Med Assoc J 97:910–916
Sandusky GE, Henk WG, Roberts ED (1981) Histochemistry and ultrastructure of the heart in experimental cobalt cardiomyopathy in the dog. Toxicol Appl Pharmacol 61:89–95
Van Vleet JF, Rebar AH, Ferrans VJ (1977) Acute cobalt and isoproterenol cardiotoxicity in swine: Protection by selenium-vitamin E supplementation and potentiation by stress-susceptible phenotype. Am J Vet Res 38:991–1002
Dahms K, Sharkowva Y, Heitland P et al (2014) Cobalt intoxication diagnosed with the help of Dr House. Lancet 383:574
Møller S, Henriksen JH (2010) Cirrhotic cardiomyopathy. J Hepatol 53:179–190
Lian C (1915) L‘alcoholisme cause d’hypertension arterielle. Bull Acad Med 74:525–528
Abe H, Kawano Y, Kojima S et al (1994) Biphasic effects of repeated alcohol intake on 24-hour blood pressure in hypertensive patients. Circulation 89:2626–2633
Wigle DA, Pang SC, Sarda IR, a (1993) Acute ethanol ingestion modifies the circulating plasma levels of atrial natriuretic peptide. Alcohol 10:275–280
Guillaume P, Jankowski M, Gianoulakis C, Gutkowska J (1996) Effect of chronic ethanol consumption on the atrial natriuretic system of spontaneously hypertensive rats. Alcohol Clin Exp Res 20:1653–1661
Potter JF, Beevers DG (1984) Pressor effect of alcohol in hypertension. Lancet 1:119–122
MacMahon S (1987) Alcohol consumption and hypertension. Hypertension 9:111–121
Klatsky AL (1996) Alcohol and hypertension. Clin Chim Acta 246:91–105
Klatsky AL (2000) Alcohol and hypertension. In: Operil S, Weber M (eds) Hypertension, 2nd edn. WB. Saunders Co, Philadelphia, pp 211–220
Urbano-Marquez A, Estrich R, Navarro-Lopez F et al (1989) The effects of alcoholism on skeletal and cardiac muscle. N Engl J Med 320:409–415
Wendt VE, Ajluni R, Bruce TA et al (1966) Acute effects of alcohol on the human myocardium. Am J Cardiol 17:804–812
Regan TJ, Levinson GE, Oldewurtel HA (1969) Ventricular function in noncardiacs with alcoholic fatty liver: Role of ethanol in the production of cardiomyopathy. J Clin Invest 48:397–407
Burch GE, Giles TD (1971) Alcoholic cardiomyopathy. Concept of the disease and its treatment. Am J Med 50:141–145
McDonald CD, Burch GE, Walsh JJ (1971) Alcoholic cardiomyopathy managed with prolonged bed rest. Ann Intern Med 74:681–691
Richardson P, McKenna W, Bristow M et al (1996) Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the definition and classification of cardiomyopathies. Circulation 93:841–842
Regan TJ (1990) Alcohol and the cardiovascular system. JAMA 264:377–381
Rubin E, Urbano-Marquez A (1994) Alcoholic cardiomyopathy. Alcohol Clin Exp Res 18:111–114
Piano MR, Schwertz DW (1994) Alcoholic heart disease: A review. Heart Lung 23:3–17
Henry WL, Gardin JM, Ware JH (1980) Echocardiographic measurements in normal subjects from infancy to old age. Circulation 62:1054–1061
Kupari M, Koskinen P, Suokas A (1991) Left ventricular size, mass and function in relation to the duration and quantity of heavy drinking in alcoholics. Am J Cardiol 67:274–279
Fabrizio L, Regan TF (1994) Alcoholic cardiomyopathy. Cardiovasc Drugs Ther 8:89–94
Steinberg JD, Hayden MT (1981) Prevalence of clinically occult cardiomyopathy in chronic alcoholism. Am Heart J 101:461–464
Fernandez-Sola J, Estruch R, Grau JM et al (1994) The relation of alcoholic myopathy to cardiomyopathy. Ann Intern Med 120:529–536
Guarnieri T, Lakatta EG (1990) Mechanism of myocardial contractile depression by clinical concentrations of ethanol. A study in ferret papillary muscles. J Clin Invest 85:1462–1467
Danziger RS, Sakai M, Capogrossi MC et al (1991) Ethanol acutely and reversibly suppresses excitationcontraction coupling in cardiac myocytes. Circ Res 68:1660–1668
Thomas AP, Rozanski DJ, Renard DC, Rubin E (1994) Effects of ethanol on the contractile function of the heart: A review. Alcohol Clin Exp Res 18:121–131
Kojima S, Wu ST, Wikman-Coffelt J, Parmley WW (1993) Acute effects of ethanol on cardiac function and intracellular calcium in perfused rat heart. Cardiovasc Res 27:811–816
Tepper D, Capasso JM, Sonnenblick EH (1986) Excitation-contraction coupling in rat myocardium: Alterations with long term ethanol consumption. Cardiovasc Res 20:369–374
Das AM, Harris DA (1993) Regulation of the mitochondrial ATP-synthase is defective in rat heart during alcohol-induced cardiomyopathy. Biochim Biophys Acta 1181:295–299
Capasso JM, Li P, Guideri G et al (1992) Myocardial mechanical, biochemical, and structural alterations induced by chronic ethanol ingestion in rats. Circ Res 71:346–356
Segel LD, Rendig SV, Choquet Y et al (1975) Effects of chronic graded ethanol consumption on the metabolism, ultrastructure, and mechanical function of the rat heart. Cardiovasc Res 9:649–663
Siddiq T, Richardson PJ, Mitchell WD et al (1993) Ethanolinduced inhibition of ventricular protein synthesis in vivo and the possible role of acetaldehyde. Cell Biochem Funct 11:45–54
Preedy VR, Peters PJ (1990) Changes in protein, RNA, and DNA and rates of protein synthesis in muscle-containing tissues of the mature rat in response to ethanol feeding: A comparative study of heart, small intestine and gastrocnemius muscle. Alcohol Alcohol 25:489–498
Lang CH, Frost RA, Kumar V, Vary T (2000) Impaired myocardial protein synthesis induced by acute alcohol intoxication is associated with changes in eIF4F. Am J Physiol Endocrinol Metab 279:1029–1038
Preedy VR, Patel VB, Why HJ et al (1996) Alcohol and the heart: Biochemical alterations. Cardiovasc Res 31:139–147
Patel VB, Sandhu G, Corbett JM et al (2000) A comparative investigation into the effect of chronic alcohol feeding on the myocardium of normotensive and hypertensive rats: An electrophoretic and biochemical study. Electrophoresis 21:2454–2462
Chen DB, Wang L, Wang PH (2000) Insulin-like growth factor I retards apoptotic signaling induced by ethanol in cardiomyocytes. Life Sci 67:1683–1693
Fernández-Solà J, Fatjó F, Sacanella E et al (2006) Evidence of apoptosis in alcoholic cardiomyopathy. Hum Pathol 37(8):1100–1110
Hajnoczky G, Buzas CJ, Pacher P et al (2005) Alcohol and mitochondria in cardiac apoptosis: Mechanisms and visualization. Alcohol Clin Exp Res 29:693–701
Rodriguez A, Chawla K, Umoh NA et al (2015) Alcohol and apoptosis: Friends or foes? Biomolecules 5:3193–3203
Vasiljevic JD, Kanjuh V, Seferovic P et al (1990) The incidence of myocarditis in endomyocardial biopsy samples from patients with congestive heart failure. Am Heart J 120:1370–1377
Morin Y, Roy PE, Mohiuddin SM, Taskar PK (1969) The influence of alcohol on viral and isoproterenol cardiomyopathy. Cardiovasc Res 3(3):363–368
Bernstein IM, Webster KH, Williams RC, Strickland RG (1974) Reduction in circulating T lymphocytes in alcoholic liver disease. Lancet 2:488–490
Arbabi S, Garcia I, Bauer GJ, Maier RV (1999) Alcohol (ethanol) inhibits IL-8 and TNF: role of the p38 pathway. J Immunol 162:7441–7445
Cook RT (1998) Alcohol abuse, alcoholism, and damage to the immune system – a review. Alcohol Clin Exp Res 22:1927–1942
Heberden W (1786) Some account of a disorder of the breast. Med Trans R Coll Physicians (london) 2:59–67
Klatsky AL, Friedman GD, Siegelaub AB (1974) Alcohol consumption before myocardial infarction. Results from the Kaiser-Permanente epidemiologic study of myocardial infarction. Ann Intern Med 81:294–301
Black S (1819) Clinical and pathological reports. Alex Wilkinson, Newry, pp 1–47
Renaud S, de Lorgeril M (1992) Alcohol, platelets, and the French paradox for coronary heart disease. Lancet 339:1523–1526
Artaud-Wild SM, Connor SL, Sexton G et al (1993) Differences in coronary mortality can be explained by differences in cholesterol and saturated fat intakes in 40 countries but not in France and Finland. A paradox. Circulation 88:2771–2779
Pearson TA, Terry P (1994) What to advise patients about drinking alcohol: The clinician‘s conundrum. JAMA 272:967–968
Friedman GD, Klatsky AL (1993) Is alcohol good for your health? N Engl J Med 329:1882–1883
Gaziano JM, Buring JE, Breslow JL et al (1993) Moderate alcohol intake, increased levels of high-density lipoprotein and its subfractions, and decreased risk of myocardial infarction. N Engl J Med 329:1829–1834
Ridker PM, Vaughan DE, Stampfer MJ et al (1994) Association of moderate alcohol consumption and plasma concentration of endogenous tissue-type plasminogen activator. JAMA 272:929–933
Mennen LI, Balkau B, Vol S et al (1999) Fibrinogen: A possible link between alcohol consumption and cardiovascular disease? Arterioscler Thromb Vasc Biol 19:887–892
Renaud SC, Beswick AD, Fehily AM et al (1992) Alcohol and platelet aggregation: The Caerphilly Prospective Heart Disease study. Am J Clin Nutr 55(5):1012–1017
Pace-Asciak CR, Hahn S, Diamandis EP et al (1995) The red wine phenolics trans-resveratrol and quercetin block human platelet aggregation and eicosanoid synthesis: Implications for protection against coronary heart disease. Clin Chim Acta 235(2):207–219
Semba RD, Ferrucci L, Bartali B et al (2014) Resveratrol levels and all-cause mortality in older community-dwelling adults. JAMA Intern Med 174(7):1077–1084
Corder R, Douthwaite JA, Lees DM et al (2001) Entothelin-1 synthesis reduced by red wine. Nature 414(6866):863–864
Rosenkranz S, Knirel D, Dietrich H et al (2002) Inhibition of the PDGF receptor by red wine flavonoids provides a molecular explanation for the ”French paradox“. FASEB J 16(14):1958–1960
Strasser RH, Nuchter I, Rauch B et al (1996) Changes in cardiac sinal transduction systems in chronic ethanol treatment preceding the development of alcoholic cardiomyopathy. Herz 21:232–240
Ettinger PO, Wu CF, De La Cruz C, Weisse AB, Ahmed SS, Regan TJ (1978) Arryhthmias and the ”Holiday Heart“: Alcohol-associated cardiac rhythm disorders. Am Heart J 1978(95):555–562
Klatsky AL (2005) Alcohol and cardiovascular diseases: A historical review and 2005 update. http://www.aim-digest.com/gateway/pages/heart/articles/CVD/klatsky1105.htm. Accessed 8 Aug 2016
Patterson E, Dormer KJ, Scherlag BJ et al (1987) Long-term intracoronary ethanol administration electrophysiologic and morphologic effects. Alcohol 4:375–384
Greenspon AJ, Schaal SF (1983) The ”Holiday Heart“: Electrophysiologic studies of alcohol effects in alcoholics. Ann Intern Med 98:135–139
Kasper EK, Agema WR, Hutchins GM et al (1994) The causes of dilated cardiomyopathy: A clinicopathologic review of 673 consecutive patients. J Am Coll Cardiol 23:586–590
Johnson RA, Palacios I (1982) Dilated cardiomyopathies of the adult. N Engl J Med 307:1051–1058
Engler R, Ray R, Higgins CB (1982) Clinical assessment and follow-up of functional capacity in patients with chronic congestive cardiomyopathy. Am J Cardiol 1982(49):1832–1837
Follansbee WP, Michelson EL, Morganroth J (1980) Nonsustained ventricular tachycardia in ambulatory patients: Characteristics and association with sudden cardiac death. Ann Intern Med 92:741–747
Marriott HJL (1964) Electrocardiographic abnormalities, conduction disorders and arrhythmias in primary myocardial disease. Prog Cardiovasc Dis 7:99–114
Teragaki M, Takeuchi K, Takeda T (1993) Clinical and histologic features of alcohol drinkers with congestive heart failure. Am Heart J 125:808–817
Aretz HT, Billingham ME, Edwards WD et al (1987) Myocarditis. A histopathologic definition and classification. Am J Cardiovasc Pathol 1:3–14
Maisch B, Portic I, Ristic AD et al (2000) Definition of inflammatory cardiomyopathy (myocarditis): On the way to consensus. Herz 25(3):200–209
Maisch B, Bauer E, Hufnagel G (1988) The use of endomyocardial biopsies in heart failure. Eur Heart J 9(Suppl H):59–71
La Vecchia LL, Bedogni F, Bozzola L et al (1996) Prediction of recovery after abstinence in alcoholic cardiomyopathy: Role of hemodynamic and morphometric parameters. Clin Cardiol 19:45–50
Leggett BA, Powell LW, Halliday JW (1989) Laboratory markers of alcoholism. Dig Dis 7:125–134
Cohen JA, Kaplan MM (1979) The SGOT/SGPT ratio – an indicator of alcoholic liver disease. Dig Dis Sci 24:835–838
Williams AL, Hoofnagle JH (1988) Ratio of serum aspartate to alanine aminotransferase in chronic hepatitis. Relationship to cirrhosis. Gastroenterology 95:734–739
Salaspuro M (1999) Carbohydrate-deficient transferrin as compared to other markers of alcoholism: A systemic review. Alcohol 19:261–271
Arndt T (2001) Carbohydrate-deficient transferrin as a marker of chronic alcohol abuse: A critical review of preanalysis, analysis, and interpretation. Clin Chem 47:13–27
Reynaud M, Schellenberg F, Loisequx-Meunier NN et al (2000) Objective diagnosis of alcohol abuse: Compared values of Carbohydrate-Deficient Transferrin (CDT), Gamma-Glutamyl Transferase (GGT), and Mean Corpuscular Volume (MCV). Alcohol Clin Exp Res 24:1414–1419
Mostofsky E, Chalhal HS, Mukamal KJ et al (2016) Alcohol and immediate risk of cardiovascular events: A systematic review and dose-response meta-analysis. Circulation 133(10):979–987
Nethala V, Brown EJ, Timson CR, Patcha R (1993) Reversal of alcoholic cardiomyopathy in a patient with severe coronary artery disease. Chest 104:626–632
Pathak SK, Kukreja RC, Hess M (1996) Molecular pathology of dilated cardiomyopathies. Curr Probl Cardiol 21:99–144
Guillo P, Mansourati J, Maheu B et al (1997) Long-term prognosis in patients with alcoholic cardiomyopathy and severe heart failure after total abstinence. Am J Cardiol 79:1276–1278
Prazak P, Pfisterer M, Osswald S et al (1996) Differences of disease progression in congestive heart failure due to alcoholic as compared to idiopathic dilated cardiomyopathy. Eur Heart J 17:251–257
Litten RZ, Allen JP (1998) Advances in development of medications for alcoholism treatment. Psychopharmacology (Berl) 139:20–33
Garbutt JC, West SL, Carey TS et al (1999) Pharmacological treatment of alcohol dependence: a review of the evidence. JAMA 281:1318–1325
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. Maisch states that he has no competing interest.
This article quotes studies with human participants or animals. See references with the contributing author on human studies.
Rights and permissions
Open Access . This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Maisch, B. Alcoholic cardiomyopathy. Herz 41, 484–493 (2016). https://doi.org/10.1007/s00059-016-4469-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-016-4469-6