Abstract
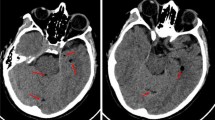
Midodrine, a prodrug, is converted after oral administration into its active drug, desglymidodrine, which acts as an α1-adrenoceptor stimulant. Midodrine is prescribed for the treatment of neurogenic orthostatic hypotension in patients with spinal cord injury. By virtue of its α1-adrenergic effects, midodrine causes an increase in the tone of the vesical sphincter, which may silently lead to progressive retention of urine, particularly in patients with spinal cord injury who void urine spontaneously. Further, midodrine may aggravate detrusor-sphincter dyssynergia, which can lead to hydroureteronephrosis. A 68-year-old man with C-4 tetraplegia was voiding urine satisfactorily through reflex detrusor contractions. He was prescribed midodrine (5 mg at 8:00am, 5 mg at 1:00pm, and 2.5 mg at 10:00pm) for postural hypotension. During the next 7 wk, this patient experienced severe leg spasms while passing urine, and the flow of urine became very slow. Intravenous urography showed bilateral hydroureteronephrosis, although an earlier study had revealed normal kidneys. Midodrine therapy was stopped, and intermittent catheterization 4 times a day, along with oral oxybutynin, was started. After midodrine was discontinued, the leg spasms during passage of urine and slowing of the urine stream coincident with the spasms disappeared completely. The patient was able to pursue activities of daily living without taking midodrine. A 40-year-old man with C-7 tetraplegia was passing urine spontaneously with no problem. For postural hypotension, he was prescribed midodrine (5 mg in the morning and 2.5 mg at lunchtime), fludrocortisone (100 μg daily), and ephedrine (15 mg by mouth, taken 10 min before getting up in the morning). Three months later, the patient presented with sweating. During the day, he would pass only small amounts of urine, but from evening onward, he would void large volumes of urine, and the sweating would diminish. Intravenous urography showed vesical diverticula; a postmicturition film revealed moderate residual urine. This patient was able to stop taking the second dose of midodrine, but he required midodrine and ephedrine in the morning to enable him to get up without feeling dizzy. After the noon midodrine dose was stopped, the patient’s sweating diminished by late afternoon. During the morning hours, however, he continued to sweat and had difficulty passing urine. Intermittent catheterization was not possible in the community setting, and the patient remains under close follow-up. These cases illustrate that patients with cervical spinal cord injury who void spontaneously may develop insidious urologic adverse effects after taking midodrine for postural hypotension. When patients with spinal cord injury develop urologic adverse effects while taking midodrine, the drug should be stopped, and other pharmacologic agents (eg, fludrocortisone) and nonpharmacologic methods should be prescribed for management of orthostatic hypotension. If a patient continues to require midodrine to control postural hypotension, intermittent catheterization combined with antimuscarinic therapy (eg, oxybutynin) should be recommended instead of spontaneous voiding.
Similar content being viewed by others
References
Cruz DN. Midodrine: a selective alpha-adrenergic agonist for orthostatic hypotension and dialysis hypotension.Expert Opin Pharmacother. 2000;1:835–840.
Wright RA, Kauffmann HC, Perera R, et al. A double-blind, dose-response study of midodrine in neurogenic orthostatic hypotension.Neurology. 1998;51:120–124.
Mukand J, Karlin L, Barrs K, Lublin P. Midodrine for the management of orthostatic hypotension in patients with spinal cord injury: a case report.Arch Phys Med Rehabil. 2001;82:694–696.
Barber DB, Rogers SJ, Fredrickson MD, Able AC. Midodrine hydrochloride and the treatment of orthostatic hypotension in tetraplegia: two cases and a review of the literature.Spinal Cord. 2000;38:109–111.
Prakash S, Garg AX, Heidenheim AP, House AA. Midodrine appears to be safe and effective for dialysis-induced hypotension: a systematic review.Nephrol Dial Transplant. 2004;19:2553–2558.
Gnad H, Burmucic R, Petritsch P, Steindorfer P. Conservative therapy of female stress incontinence: double-blind study with the alpha-sympathomimetic midodrin. [in German].Fortschr Med. 1984;102:578–580.
Tai C, Roppolo JR, de Groat WC. Spinal reflex control of micturition after spinal cord injury.Restor Neurol Neurosci. 2006;24:69–78.
Angeli P, Volpin R, Gerunda G, et al. Reversal of type 1 hepatorenal syndrome with the administration of midodrine and octreotide.Hepatology. 1999;29:1690–1697.
Diskin CJ, Stokes TJ, Dansby LM, Radcliff L, Carter TB. Massive increase in proteinuria after the introduction of midodrine in an elderly patient—a case report.Nephrol Dial Transplant. 2006; 21:1988.
Piddle TJ, Little JW. Hydronephrosis due to improper condom catheter use.J Am Paraplegia Soc. 1994;17:168–170.
Lahrmann H, Cortelli P, Hilz M, Mathias CJ, Struhal W, Tassinari M. EFNS guidelines on the diagnosis and management of orthostatic hypotension.Eur J Neurol. 2006;13:930–936.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vaidyanathan, S., Soni, B.M. & Hughes, P.L. Midodrine: Insidious development of urologic adverse effects in patients with spinal cord injury: A report of 2 cases. Adv Therapy 24, 712–720 (2007). https://doi.org/10.1007/BF02849965
Issue Date:
DOI: https://doi.org/10.1007/BF02849965