Abstract
In December 2022, the Chinese suffered widespread Omicron of SARS-CoV-2 with variable symptom severity and outcome. We wanted to develop a scoring model to predict the mortality risk of older Omicron pneumonia patients by analyzing admission data. We enrolled 227 Omicron pneumonia patients aged 60 years and older, admitted to our hospital from December 15, 2022, to January 16, 2023, and divided them randomly into a 70% training set and a 30% test set. The former were used to identify predictors and develop a model, the latter to verify the model, using the area under the receiver operating characteristic curve (AUC), the Hosmer–Lemeshow goodness-of-fit test, a calibration curve to test its performance and comparing it to the existing scores. The MLWAP score was calculated based on a multivariate logistic regression model to predict mortality with a weighted score that included immunosuppression, lactate ≥ 2.4, white blood cell count ≥ 6.70 × 109/L, age ≥ 77 years, and PaO2/FiO2 ≤ 211. The AUC for the model in the training and test sets was 0.852 (95% CI, 0.792–0.912) and 0.875 (95% CI, 0.789–0.961), respectively. The calibration curves showed a good fit. We grouped the risk scores into low (score 0–7 points), medium (8–10 points), and high (11–13 points). This model had a sensitivity of 0.849, specificity of 0.714, and better predictive ability than the CURB-65 and PSI scores (AUROC = 0.859 vs. 0.788 vs. 0.801, respectively). The MLWAP-mortality score may help clinicians to stratify hospitalized older Omicron pneumonia patients into relevant risk categories, rationally allocate medical resources, and reduce the mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
COVID-19 is an acute respiratory infectious disease caused by a new coronavirus type 2 (SARS-CoV-2) that is characterized by fever, fatigue, and a dry cough. In severe cases, it can develop rapidly into acute respiratory distress syndrome, septic shock, metabolic acidosis, and coagulation dysfunction [1]. SARS-CoV-2 is evolving, and new Alpha, Beta, Gamma, and Delta variants have emerged since the onset of COVID-19 [2]. Since January 2022, the Omicron variant has surpassed all previous mutants in its super transmissibility and immune escape and replaced Delta as the principal transmission strain in the world [3]. In December 2022, a large outbreak of the Omicron variant occurred in China. Despite indications that its clinical severity may be lower than that of Delta [4], the sudden surge of Omicron pneumonia patients placed unprecedented pressure on the Chinese healthcare system [5].
Additionally, there are many variations of the Omicron variant [6], with heterogeneity in the severity of the illness and the possibility of reinfection [7, 8]. By the end of June 2023, over 690 million people worldwide had been infected with COVID-19, causing nearly 6.9 million deaths. Reducing the mortality of critically ill patients requires early identification and medical intervention. Identifying the severity of the disease or patients at high-risk of death is a critical step in managing COVID-19. There are multiple tools for predicting the prognosis of pneumonia clinically, such as CRB-65, CURB-65, and PSI, which are widely used for evaluating community-acquired pneumonia (CAP) [9]. However, most are still not applicable for viral infections, such as COVID-19. Many scoring systems based on other diseases are used for assessing the adverse prognosis risk of COVID-19, including commonly used scores for CAP, viral pneumonia, and early sepsis recognition [10]. Age is positively associated with the severity and mortality of COVID-19 infection [11]. To our knowledge, there are no severity scoring methods for Omicron pneumonia in older adults.
Here, we assessed the clinical and laboratory characteristics of older Omicron pneumonia patients on admission and developed a new scoring system to predict their mortality risk.
Materials and methods
Study design and population
We retrospectively studied all hospitalized patients aged 60 years and older with a positive real-time polymerase chain reaction (RT-PCR; TIB respiratory kit, ROCHE, Switzerland) test for SARS-CoV-2 on nasopharyngeal swabs and no previous SARS-CoV-2 infections, who were admitted to the Second Affiliated Hospital of Soochow University, China, from December 15, 2022, to January 16, 2023 (during the rapid spread of the Omicron variant in China). The study was approved by the hospital ethics committee (no. JD-LK2023025-I01, approved in March 2023) and the need for informed consent was waived as it was a retrospective analysis. Our study enrolled patients diagnosed with pneumonia based on the 2009 Infectious Diseases Society of America (IDSA)/American Thoracic Society (ATS) criteria [12]. Following World Health Organization standards, Omicron pneumonia was divided into non-severe, severe, and critically ill [13]. The Omicron pneumonia patients included in this study had comorbid immunosuppression, including tumor patients undergoing radiation or chemotherapy, long-term use of steroids or immunosuppressive drugs for autoimmune diseases, and lymphocyte counts < 0.8 × 109/L. Exclusion criteria were age < 60 years, those ultimately diagnosed with other non-pneumonia diseases, and those hospitalized for more than 3 months before death.
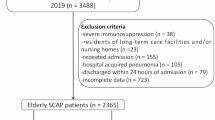
Initially, 329 hospitalized patients aged 60 years or older had positive RT-PCR tests for SARS-CoV-2 on nasopharyngeal swabs, and 242 of them with pneumonia were enrolled. From these, 15 cases diagnosed with other non-pneumonia diseases were excluded (n = 15), leaving 227 pneumonia patients with positive RT-PCR testing for SARS-CoV-2 on nasopharyngeal swabs in the analysis. This population was randomly divided on a 70:30 basis into training and test sets. The training set was used to identify predictors and develop a multivariate model. The test set was used to assess the discrimination and calibration of the model (Fig. 1).
Data collection
Infection caused by SARS-CoV-2 was confirmed by RT-PCR detection on nasopharyngeal swabs. We collected the patients’ admission data, including demographic information, comorbidities, symptoms, number of days before admission symptoms began, laboratory examinations, chest x-ray or CT images, respiratory tract secondary infection, treatment options, complications, intensive care unit (ICU) admission, and invasive mechanical ventilation. Myocardial injury was defined as a new elevation of the cardiac troponin (cTn) level exceeding the 99th percentile of the upper reference limit [14]; our reference range for cTn is 0–30 pg/mL. Acute renal injury refers to an increase in the serum creatinine (sCr) level by at least 26.5 μmol/L (0.3 mg/dL) within 48 h, an increase of 1.5 times the baseline sCr value within 7 days, or a decrease in urine output to 0.5 mL/kg/h for at least 6 h [15]. We calculated the CURB-65 [9] and PSI [16] scores of all patients and recorded their outcomes. Mortality was defined as the total mortality within 90 days.
Statistical methods
We randomly divided the 227 older adult Omicron pneumonia patients into a training set of 158 (70%) and a test set of 69 (30%), and classified the training set into survivor and 90-day death groups. The statistical analyses were done using SPSS ver. 26.0 (IBM, Armonk, NY, USA) and R4.2.3 (www.r-project.org). For continuous variables that conformed to a normal distribution, groups were compared using the t-test and reported as the mean ± standard deviation; otherwise, the non-parametric U-test was used and the results as the median (interquartile range). Enumeration data are expressed as n (%), and groups were compared using Pearson’s chi-square test. Taking the 90-day death as the dependent variable, variables with a p-value less than 0.05 in univariate analyses were used as independent variables, using a backward conditional method to obtain a multivariate logistic regression model in the training set, using the odds ratios (OR) as the risk assessment parameter. The performance of the score was evaluated by measuring the area under the ROC curve (AUROC), and the sensitivity and specificity were calculated. A calibration curve and the Hosmer–Lemeshow goodness-of-fit test were used to assess the calibration. The calibration of the model in both the training and test sets was validated using 1000 bootstrap resamplings. The points for each predictor were summed to calculate the total risk score for each patient. We grouped the risk scores into three categories (low-, medium-, and high-risk of 90-day mortality) and plotted the observed versus predicted proportion of 90-day mortality of the patients in each category in the test set. We used the ROC curve to assess the risk prediction ability of the score compared with the CURB-65 and PSI scores. All tests were two-sided and a p-value < 0.05 was considered a significant statistical difference.
Results
Demographics and clinical features
Our study included 227 older adult Omicron pneumonia patients of whom 32.2% (73/227) died. We randomly divided the entire sample into a training set with 158 patients and a test set with 69 patients (Fig. 1). Table S1 summarizes the clinical features of the two cohorts. Table 1 compares the demographics and baseline characteristics between the survivors and those who died within 90-days after admission in the training set. The survivor group comprised 105 (66.5%) patients, while the 90-day death group comprised 53 (33.5%) patients. The training sample comprised 102 (64.56%) males and 56 (35.44%) females for a gender ratio of 1.8. The median age of the 158 cases was 77 years, and the survival and 90-day death group was 74 years and 81 years, respectively. The two groups did not differ significantly in body mass index (BMI). The most common comorbidity was cardiovascular disease (70.25%), followed by immunosuppression, diabetes, malignant tumor, cerebrovascular disease, and chronic lung disease. The 90-day death group had more comorbid immunosuppression and cerebrovascular disease than the survivor group, and both differed statistically (p < 0.05). The most common symptoms were cough and fever, followed by chest tightness and pharyngalgia. The survivor group had more fever symptoms than the 90-day death group; while the opposite was true for chest tightness (p < 0.05). In the 90-day death group, 94.34% (50/53) of the cases had critical COVID-19 pneumonia, 56.60% (30/53) were admitted to the ICU, and 35.85% (19/53) received invasive mechanical ventilation, all significantly higher than in the survivor group, and were treated significantly more often with sivelestat than the survivor group (p < 0.05). There were no statistical differences in administering antiviral agents, anticoagulation, baricitinib, tocilizumab, human immunoglobulin, or glucocorticoid between the two groups. In terms of complications, the 90-day death group had significantly more respiratory tract secondary infection, myocardial injury, and acute kidney injury (AKI) than the survivor group (all p < 0.05).
Laboratory findings
The patients underwent laboratory testing on the day of admission (Table 1). In the training set, the CURB-65 and PSI scores and proportion of critical Omicron pneumonia were significantly higher in the 90-day death group than in the survivor group. In the 90-day death group, the PO2/FiO2 and lymphocyte counts were lower than in the survivor group (p < 0.001). Moreover, the lactate (Lac) content, white blood cell and neutrophil counts, C-reactive protein (CRP), procalcitonin (PCT), Interleukin 6 (IL-6), and d-dimer were all higher in the 90-day death group than in the survivor group (all p < 0.001).
Risk factors of mortality
Based on the above methods and analysis, the following categorical variables were analyzed by backward stepwise logistic regression: age, cerebrovascular disease, immunosuppression, fever, chest tightness, respiratory tract secondary infection, myocardial injury, AKI, sivelestat treatment, ICU admission, invasive mechanical ventilation, Omicron pneumonia, PO2/FiO2, Lac, white blood cell count, neutrophil count, lymphocyte count, CRP, PCT, IL-6, and d-dimer. To develop a simple clinical prediction tool, we allocated relative weights based on the regression coefficients of each categorical variable (β). Table 2 shows the coefficients with the OR and 95% CI, and calculation of the immunosuppression, Lac ≥ 2.4, white blood cell count ≥ 6.7 × 109/L, age ≥ 77, and PO2/FiO2 ≤ 211 (MLWAP) scores. The OR generated by the regression analysis model was rounded to the nearest integer, resulting in a total score of 13, with immunosuppression, Lac ≥ 2.4, white blood cell count ≥ 6.7 × 109/L, age ≥ 77 years, and PO2/FiO2 ≤ 211 given the respective scores of 5, 3, 2, 2, and 1 (Table 2). The points for each predictor were summed to calculate the total risk score for each patient. The AUC for the risk score model was 0.852 (95% CI, 0.792–0.912), similar to the AUC of the test set, 0.875 (95% CI, 0.789–0.961; Fig. 2a, b). The calibration curve showed a relatively good fit (Fig. 2c, d). We divided the risk score into low- (0–7 points; 90-day death risk < 30%), medium- (8–10 points; 90-day death risk 30–50%), and high- (11–13 points; 90-day death risk > 50%) risk groups (Figure S1). The incidence of predicted 90-day mortality with this model was similar to that observed in the test set (Fig. 3). This model had a sensitivity of 0.849, specificity of 0.714, and better predictive ability than the CURB-65 and PSI scores (AUROC = 0.859 vs. 0.788 vs. 0.801, respectively; Fig. 4).
The receiver operating characteristic curve and calibration curve. (a) AUC curve of the training set; (b) AUC curve of the test set; (c) Calibration plot for the training set with bootstrapping; (d) Calibration plot of the test set with bootstrapping. In (c) and (d), X-axis is the predicted probability of 90-day death risk; Y-axis is the actually observed probability. The dashed gray line indicates a perfect prediction by an ideal model. The blue solid line represents the calibration of prediction model, while black solid line is bias-corrected with bootstrapping technique. AUC area under the receiver operating characteristic curve
Discussion
The widespread transmission of COVID-19 is closely related to the continuous evolution of SARS-CoV-2 since its outbreak, which has raised enormous challenges for global epidemic prevention and control [17]. The Omicron variant has spread worldwide and has many mutations that affect its infectivity and immune escape [18]. The Chinese epidemic prevention and control policy was modified in December 2022, and the outbreak of the Omicron variant in China placed unprecedented pressure on the Chinese medical system. Few studies have examined the clinical characteristics and prognosis of Omicron pneumonia. In this context, we surveyed the clinical and epidemiological characteristics of older patients with Omicron pneumonia to develop a new score for predicting mortality risk. This score will facilitate early disease risk stratification and medical intervention to reduce mortality in critically ill patients.
This study investigated the clinical features of 227 older Omicron pneumonia patients who were treated in a tertiary hospital after the Chinese epidemic prevention and control policies were changed. The dominant variants in China at the time were Omicron BA 5.2 and BF.7. In our series, 32.2% (73/227) of the patients with Omicron pneumonia died, which is much greater than the 4.2% (10/238) that Xu et al. reported during the same period [19]. That study enrolled immunocompetent Omicron pneumonia patients with an average age of 71.84 ± 14.11 years, with comorbid cerebrovascular disease in 57.56% (137/238) and cardiovascular disease in 11.76% (28/238). Our study population comprised patients aged 60 years and older; the median age of the entire training set and its 90-day death group was 77 years and 81 years, respectively. Their leading comorbidity was cardiovascular disease (70.25%; 111/158), followed by immunosuppression (58.23%; 92/158). A previous study showed that older COVID-19 patients and patients with pre-existing disease develop more severe disease and have higher mortality rates [20]. Male gender, advanced age, and concomitant hypertension are associated with prolonged viral RNA shedding [21]. Moreover, age is positively associated with the severity and mortality of COVID-19 infection [11]. In addition, the large number of cases in a short period led to insufficient medical resources and ICU beds, delaying treatment in some severe and critical high-risk patients. Based on the 10th Chinese Novel Coronavirus infection diagnosis and treatment protocol, severe and critically ill high-risk patients are people (1) over 65 years old, especially those who have not been vaccinated with the COVID-19 vaccine; (2) with cardiovascular and cerebrovascular diseases, chronic lung diseases, diabetes, chronic liver and kidney diseases, tumors, and other comorbidities and maintenance dialysis; (3) immunodeficiency (such as AIDS, immunodeficiency caused by long-term use of corticosteroids or other immunosuppressive drugs); (4) BMI > 30 kg/m2; (5) late pregnancy and perinatal women; and (6) heavy smokers. Since our study population had many high-risk factors for developing severe and critical COVID-19, this may be the most crucial reason for the high mortality.
In our training set, the main symptoms were cough (113, 71.52%), fever (110, 69.62%), chest tightness (81, 51.27%), and pharyngalgia (17, 10.76%), which was similar to the study population in Miao et al. [22]. The CURB-65 and PSI scores in the 90-day death group were higher than in the survivor group (p < 0.001). As the scores most commonly used to evaluate disease severity and determine the appropriate nursing site for CAP, the CURB-65 and PSI scores are used in emergency departments and clinics for deciding the best setting for continuing patient management. Armiñanzas reported that the CURB-65 was an alternative score for predicting severity in patients with COVID-19 [23]. Another study showed that the mortality of COVID‐19 patients with PSI grades IV–V was significantly higher than that of patients with PSI grades I–III, reaching 32.1% (9/28) [24]. In addition, the PSI score of older COVID‐19 patients is higher than that of young and middle-aged patients, reflecting a higher risk of severe illness [25]. While the two scores may be unsuitable for predicting progress. In another prospective cohort study, 26.3% (CURB-65 score 0–2 points) and 37.7% (PSI grade I–III), with the development of ARDS, and both scores suggest low risk [26].
In the 90-day death group, the PO2/FiO2 and lymphocyte count were lower than in the survivor group (p < 0.001). PO2/FiO2 can be used as an index of the severity of respiratory insufficiency and the therapeutic effect. Franchini et al. found that PO2/FiO2 was the strongest determinant of survival in COVID-19 patients [27]. As an essential part of the adaptive immune system, lymphocytes play a vital role in eliminating invasive viruses and protecting human health from the threat of viruses. One study found that lymphopenia is a common characteristic of COVID-19 patients [28]. Moreover, Chen et al. found that natural killer (NK), CD4 + T, and CD8 + T cells in severely ill patients secreted less IFN-γ, suggesting that severe COVID-19 patients were immunosuppressed [29]. In the 90-day death group, the Lac content, white blood cell and neutrophil counts, CRP, PCT, IL-6, and d-dimer were all higher in the 90-day death group than in the survivor group (all p < 0.001), which was consistent with previous studies [19, 23] As a product of anaerobic metabolism, lactate is considered a powerful indicator for assessing the severity of sepsis [30]. Gupta et al. indicated that lactate is a key factor involved in the death of COVID-19 patients [31]. Neutrophilia is associated with a high inflammatory state and cytokine storm, a crucial part of the pathogenic mechanism of COVID-19 [32]. Soraya et al. found that the white blood cell and neutrophil counts were significantly higher in patients with severe COVID-19 than in non-severe cases, and increased with COVID-19 disease progression [33]. As an inflammatory biomarker, CRP is related to the development of COVID-19 and is an early predictor of severe disease [34]. IL-6, a vital inflammatory cytokine in the development of COVID-19, leads to acute lung injury, acute respiratory distress syndrome (ARDS), and further tissue damage [35]. One study showed that IL-6 ≥ 74.98 pg/mL, CRP ≥ 81 mg/L, PCT ≥ 0.56 ng/mL, and d-dimer ≥ 760 ng/mL effectively predicted the in-hospital mortality in COVID-19 patients [36].
In the training set, 26.58% (42/158) of the patients were admitted to the ICU, and 13.29% (21/158) received invasive mechanical ventilation. In the 90-day death group, 56.60% (30/53) were admitted to the ICU and 35.85% (19/53) received invasive mechanical ventilation, both more than in the survivor group (p < 0.05). This suggests that those Omicron pneumonia patients who died became critically ill quickly, needed ICU admission and invasive mechanical ventilation, and had a poor prognosis. A recent meta-analysis of 26 original studies and two systematic reviews including 83,619 COVID-19 patients reported an average ICU admission rate of 20.1% (range 4.6–32%); in the studies reporting ventilator support rates, an average of 48.8% needed invasive mechanical ventilation; moreover, the average mortality rate in the ICU was 34.9% (range 0–72%) [37]. Our findings were similar to those of Aziz et al., except that 13.66% of our entire sample required invasive mechanical ventilation versus 48.80% in Aziz et al. [37]. Possible reasons were that the number of Omicron pneumonia patients increased sharply, causing a shortage of medical resources; and some patients refused invasive mechanical ventilation for their own reasons.
In terms of complications, the complications in the 90-day death group included myocardial injury in 71.70% (38/53), AKI in 60.3% (32/53), and respiratory tract secondary infection in 45.28% (24/53), all significantly more frequent than in the survivor group (all p < 0.05). Zhou et al. reported that secondary infection decreases the survival of COVID-19 patients, especially those admitted to the ICU, and found that 15% (29/191) of COVID-19 patients had a secondary infection with 31% of these patients requiring mechanical ventilation in the ICU, and that 50% of the non-survivors had secondary infections versus only 1% of the survivors [38]. In another study, myocardial injury related to COVID-19 occurred in 15.0–27.8%, and was directly related to the risk of disease severity and death, increasing the risk of fatal events by 8–21 times [39]. A recent review revealed that about 31.5% of hospitalized COVID-19 patients developed AKI, and the death risk of COVID-19 patients with chronic kidney disease (CKD) stage 4–5 was 2.5 times than that of patients with normal renal function or CKD stage 1–2 [40]. Our results were consistent with the previous studies.
In the 90-day death group, 30.19% (16/53) of the patients were treated with sivelestat, which was significantly higher than the percentage in the survivor group (p < 0.05). However, there were no statistical differences in the use of antiviral agents, anticoagulation, baricitinib, tocilizumab, human immunoglobulin, or glucocorticoid between the two groups. ARDS is one of the most common fatal complications of COVID-19, and its occurrence and progression to death is critically dependent on neutrophil elastase. Sivelestat is a neutrophil elastase inhibitor (NEI) used to treat ALI/ARDS [41]. Clinical trials have shown that sivelestat can significantly reduce the non-mechanical ventilation time and improve the survival rate of ALI/ARDS patients with lung injury score (LIS) < 2.5, and improve the adverse prognosis of ALI/ARDS patients. However, the STRIVE study found that sivelestat cannot be used as an early intervention for patients with LIS > 2.5 [42, 43]. There is no evidence supporting the use of NEIs in ARDS induced by COVID-19. Although we did not use the Murray score [44] to evaluate lung injury, based on the data for the 90-day death group, 83.02% (44/53) of the patients had multi-lobar infiltration, for a value of 3, with a mean PO2/FiO2 of 96.00 (68.00–153.00) for a value of 4; the final value is obtained by dividing the aggregate value (= 7) by the number of components (= 2), strongly suggesting that the lung injury scores exceeded 2.5. Treatment with sivelestat did not provide benefits, although our sample was small. We expect future clinical trials to evaluate the efficacy of sivelestat in COVID-19 patients with a high risk of respiratory failure.
The CURB-65 score, which evaluates confusion, urea levels, respiratory rate, blood pressure, and age ≥ 65 years, was proposed by the British Thoracic Association in 2003 and is mainly used to evaluate the 30-day mortality risk of CAP [9]. PSI is a five-grade comprehensive score proposed in 1997 by Fine [16], covering 20 variables such as age, gender, complications, vital signs, and laboratory tests, that is mainly used to predict the death risk of community pneumonia within 6 weeks. Genc Yavuz reported that a CURB-65 ≥ 3 points and PSI ≥ grade IV show considerable predictive performance for the 30-day death risk of COVID-19 patients over 60 years old (AUC = 0.832 vs. 0.846) [45]. When there is a heavy emergency department burden, CURB-65 can be considered when following patients over 60 years old. Some scholars found that the CURB-65 had a poorer predictive ability in influenza A virus for older patients than for younger ones [46, 47]. In older adults, the mortality rate of viral diseases was more than twice that of young patients [48]. Our entire sample consisted of patients aged 60 years and older; in the training set, the median age of the 90-day death group was 81 years, which was higher than that of the survivor group (74 years). This suggests that if we used the CURB-65 to predict the death risk of this sample, its efficiency might be reduced. In addition, when there is a heavy emergency department burden, the PSI score is complicated to use as it involves many variables.
All the parameters in the MLWAP score are easy to obtain and all the tests can be performed in a hospital. The AUC for the model in the training and test sets was 0.852 (95% CI, 0.792–0.912) and 0.875 (95% CI, 0.789–0.961), respectively. Hosmer–Lemeshow goodness-of-fit test in the two sets showed that the p-values were 0.948 and 0.975 respectively (both p > 0.05), suggesting the calibration curves with good fit, and it showed good consistency in predicting the death risk and actual risk of older patients with Omicron pneumonia. This model had a sensitivity of 0.849, specificity of 0.714, and better predictive ability than the CURB-65 and PSI scores (AUROC = 0.859 vs. 0.788 vs. 0.801, respectively). In summary, the MLWAP score shows promise for predicting 90-day death in older Omicron pneumonia patients.
There are some limitations to our study. First, as a retrospective study, uncertain bias and confounding factors cannot be addressed, and patients with a high risk of death may reduce the maximum intervention measures or even refuse ICU treatment; the mortality prediction was retrospective by introducing biased data. Second, establishing a mortality risk score for predicting disease prognosis may be evaluated better in a larger multi-center sample, and our sample size was relatively small. Finally, the score should be verified using larger international datasets to improve its universality and robustness.
Conclusion
In summary, the MLWAP score, based on five conventional indexes available in hospitals, was a good predictor of 90-day mortality in older Omicron pneumonia patients. This tool may help clinicians predict these patients’ admission prognoses, thus assisting in the allocation of medical resources and contributing to a reduction in their mortality.
Funding source
This work was supported by the Medical, Health Science and Technology Innovation Project of Suzhou, China (grant no. SKY2021006); this work was also supported by the Competitive discipline lift project of the Second Affiliated Hospital of Soochow University (grant no. XKTJ-XK202007); this work was also supported by the science and technology project of Suzhou Hospital of Integrated Traditional Chineseand Western Medicine (grant no. YJ2022026).
Data availability
Data are available on request due to privacy/ethical restrictions.
References
Berlin DA, Gulick RM, Martinez FJ (2020) Severe Covid-19. N Engl J Med 383(25):2451–2460. https://doi.org/10.1056/NEJMcp2009575
Sanches PRS, Charlie-Silva I, Braz HLB et al (2021) Recent advances in SARS-CoV-2 Spike protein and RBD mutations comparison between new variants Alpha (B.1.1.7, United Kingdom), Beta (B.1.351, South Africa), Gamma (P.1, Brazil) and Delta (B.1.617.2, India). J Virus Erad 7(3):100054. https://doi.org/10.1016/j.jve.2021.100054
Markov PV, Katzourakis A, Stilianakis NI (2022) Antigenic evolution will lead to new SARS-CoV-2 variants with unpredictable severity. Nat Rev Microbiol 20(5):251–252. https://doi.org/10.1038/s41579-022-00722-z
Maslo C, Friedland R, Toubkin M et al (2022) Characteristics and outcomes of hospitalized patients in South Africa during the COVID-19 Omicron wave compared with previous waves. JAMA 327(6):583–584. https://doi.org/10.1001/jama.2021.24868
Cai J, Deng X, Yang J et al (2022) Modeling transmission of SARS-CoV-2 Omicron in China. Nat Med 28(7):1468–1475. https://doi.org/10.1038/s41591-022-01855-7
Harvey WT, Carabelli AM, Jackson B et al (2021) SARS-CoV-2 variants, spike mutations and immune escape. Nat Rev Microbiol 19(7):409–424. https://doi.org/10.1038/s41579-021-00573-0
Pulliam JRC, van Schalkwyk C, Govender N et al (2022) Increased risk of SARS-CoV-2 reinfection associated with emergence of Omicron in South Africa. Science 376(6593):eabn4947. https://doi.org/10.1126/science.abn4947
Zhang X, Wu S, Wu B et al (2021) SARS-CoV-2 Omicron strain exhibits potent capabilities for immune evasion and viral entrance. Signal Transduct Target Ther 6(1):430. https://doi.org/10.1038/s41392-021-00852-5
Barlow G, Nathwani D, Davey P (2007) The CURB-65 pneumonia severity score outperforms generic sepsis and early warning scores in predicting mortality in community-acquired pneumonia. Thorax 62:253–259. https://doi.org/10.1136/thx.2006.067371
Cai YQ, Zeng HQ, Li YP et al (2022) Advances in clinical prediction scores for prognosis of coronavirus disease-2019. Zhonghua Jie He He Hu Xi Za Zhi 45(7):706–711. https://doi.org/10.3760/cma.j.cn112147-20211125-00837
Borgoni S, Kudryashova KS, Burka K et al (2021) Targeting immune dysfunction in aging. Ageing Res Rev 70:101410. https://doi.org/10.1016/j.arr.2021.101410
Charles PG, Davis JS, Grayson ML (2009) Rocket science and the Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) guidelines for severe community-acquired pneumonia. Clin Infect Dis 48(12):1796–1797. https://doi.org/10.1086/599227
Lamontagne F, Agarwal A, Rochwerg B et al (2020) A living WHO guideline on drugs for covid-19. BMJ 370:m3379. https://doi.org/10.1136/bmj.m3379
Chew MS, Saugel B, Lurati-Buse G (2023) Perioperative troponin surveillance in major noncardiac surgery: a narrative review. Br J Anaesth 130(1):21–28. https://doi.org/10.1016/j.bja.2022.08.041
Ostermann M, Bellomo R, Burdmann EA et al (2020) Controversies in acute kidney injury: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) conference. Kidney Int 98(2):294–309. https://doi.org/10.1016/j.kint.2020.04.020
Fine MJ, Auble TE, Yealy DM et al (1997) A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 336(4):243–250. https://doi.org/10.1056/NEJM199701233360402
Zaidi A, Harris R, Hall J et al (2023) Effects of second dose of SARS-CoV-2 vaccination on household transmission. Engl Emerg Infect Dis 29(1):127–132. https://doi.org/10.3201/eid2901.220996
Tan ST, Kwan AT, Rodriguez-Barraquer I et al (2023) Infectiousness of SARS-CoV-2 breakthrough infections and reinfections during the Omicron wave. Nat Med 29(2):358–365. https://doi.org/10.1038/s41591-022-02138-x
Xu J, Cao Z, Miao C et al (2023) Predicting omicron pneumonia severity and outcome: a single-center study in Hangzhou, China. Front Med 10:1192376. https://doi.org/10.3389/fmed.2023.1192376
Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 395(10223):497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
Xu K, Chen Y, Yuan J et al (2020) Factors associated with prolonged viral RNA shedding in patients with coronavirus disease 2019 (COVID-19). Clin Infect Dis 71(15):799–806. https://doi.org/10.1093/cid/ciaa351
Miao Y, Ren Y, Ren T (2023) Clinical characteristics profile of COVID-19 patients with Omicron variant admitted in a Tertiary Hospital, Central China. Int J Gen Med 16:2365–2371. https://doi.org/10.2147/IJGM.S409478
Armiñanzas C, de Las A, Revillas F, Gutiérrez Cuadra M et al (2021) Usefulness of the COVID-GRAM and CURB-65 scores for predicting severity in patients with COVID-19. Int J Infect Dis 108:282–288. https://doi.org/10.1016/j.ijid.2021.05.048
Han R, Su H, Guo G et al (2021) Prognostic value of immune-inflammatory index in PSI IV-V patients with COVID-19. BioMed Res Int 9987931:1–6. https://doi.org/10.1155/2021/9987931
Liu K, Chen Y, Lin R et al (2020) Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Infect 80(6):e14–e18. https://doi.org/10.1016/j.jinf.2020.03.005
García Clemente MM, Herrero Huertas J, Fernández Fernández A et al (2021) Assessment of risk scores in Covid-19. Int J Clin Pract 75(12):e13705. https://doi.org/10.1111/ijcp.13705
Franchini S, Mette F, Landoni G et al (2022) Gas-exchange deficit and systemic hypoperfusion in COVID-19 and non-COVID-19 young adult patients with pneumonia. Panminerva Med. https://doi.org/10.23736/S0031-0808.22.04562-1
Diao B, Wang C, Tan Y et al (2020) Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19). Front Immunol 11:827. https://doi.org/10.3389/fimmu.2020.00827
Chen G, Wu D, Guo W et al (2020) Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Investig 130(5):2620–2629. https://doi.org/10.1172/JCI137244
Gattinoni L, Vasques F, Camporota L et al (2019) Understanding lactatemia in human sepsis. Potential impact for early management. Am J Respir Crit Care Med 200(5):582–589. https://doi.org/10.1164/rccm.201812-2342OC
Gupta GS (2022) The lactate and the lactate dehydrogenase in inflammatory diseases and major risk factors in COVID-19 patients. Inflammation 45(6):2091–2123. https://doi.org/10.1007/s10753-022-01680-7
Zhang L, Huang B, Xia H et al (2020) Retrospective analysis of clinical features in 134 coronavirus disease 2019 cases. Epidemiol Infect 148:e199. https://doi.org/10.1017/S0950268820002010
Soraya GV, Ulhaq ZS (2020) Crucial laboratory parameters in COVID-19 diagnosis and prognosis: an updated meta-analysis. Med Clin 155(4):143–151. https://doi.org/10.1016/j.medcle.2020.05.004
Tan C, Huang Y, Shi F et al (2020) C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J Med Virol 92(7):856–862. https://doi.org/10.1002/jmv.25871
Meduri GU, Headley S, Kohler G et al (1995) Persistent elevation of inflammatory cytokines predicts a poor outcome in ARDS. Plasma IL-1 beta and IL-6 levels are consistent and efficient predictors of outcome over time. Chest 107(4):1062–1073. https://doi.org/10.1378/chest.107.4.1062
Milenkovic M, Hadzibegovic A, Kovac M et al (2022) D-dimer, CRP, PCT, and IL-6 Levels at admission to ICU can predict in-hospital mortality in patients with COVID-19 pneumonia. Oxid Med Cell Longev 2022:8997709. https://doi.org/10.1155/2022/8997709
Aziz S, Arabi YM, Alhazzani W et al (2020) Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med 46(7):1303–1325. https://doi.org/10.1007/s00134-020-06092-5
Zhou F, Yu T, Du R et al (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (London, England) 395(10229):1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3
Abate SM, Mantefardo B, Nega S et al (2012) (2021) Global burden of acute myocardial injury associated with COVID-19: a systematic review, meta-analysis, and meta-regression. Ann Med Surg 68:102594. https://doi.org/10.1016/j.amsu.2021.102594
Mahalingasivam V, Su G, Iwagami M et al (2022) COVID-19 and kidney disease: insights from epidemiology to inform clinical practice. Nat Rev Nephrol 18(8):485–498. https://doi.org/10.1038/s41581-022-00570-3
Miyoshi S, Hamada H, Ito R et al (2013) Usefulness of a selective neutrophil elastase inhibitor, sivelestat, in acute lung injury patients with sepsis. Drug Des Dev Ther 7:305–316. https://doi.org/10.2147/DDDT.S42004
Hashimoto S, Okayama Y, Shime N et al (2021) Nanomedicine for acute respiratory distress syndrome: the latest application, targeting strategy, and rational design. Acta pharmaceutica Sinica B 11(10):3060–3091. https://doi.org/10.1016/j.apsb.2021.04.023
Murray JF, Matthay MA, Luce JM et al (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138(3):720–723. https://doi.org/10.1164/ajrccm/138.3.720
Lim WS, van der Eerden MM, Laing R et al (2003) Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 58(5):377–382. https://doi.org/10.1136/thorax.58.5.377
Genc Yavuz B, Colak S, Guven R et al (2021) Clinical features of the 60 years and older patients infected with 2019 novel coronavirus: can we predict mortality earlier? Gerontology 67(4):433–440. https://doi.org/10.1159/000514481
Riquelme R, Jiménez P, Videla AJ et al (2011) Predicting mortality in hospitalized patients with 2009 H1N1 influenza pneumonia. Int J Tuberc Lung Dis 15(4):542–546. https://doi.org/10.5588/ijtld.10.0539
Bjarnason A, Thorleifsdottir G, Löve A et al (2012) Severity of influenza A 2009 (H1N1) pneumonia is underestimated by routine prediction rules. Results from a prospective, population-based study. PloS one 7(10):e46816. https://doi.org/10.1371/journal.pone.0046816
Pawelec G, Barnett Y, Forsey R et al (2002) T cells and aging, January 2002 update. Front Biosci 7:d1056–d1183. https://doi.org/10.2741/a831
Acknowledgements
We gratefully acknowledge the role of all our colleagues, nurses, and others involved in the care of patients.
Author information
Authors and Affiliations
Contributions
Yongjian Pei and Ting Li conceptualized, managed, and coordinated the project, assisted with the design of the methodology, analyzed the data, and prepared the initial and final drafts of the manuscript. Chen Chen, Yongkang Huang, and Yun Yang took responsibility for the data and their analysis. Tong Zhou and Minhua Shi conceptualized the project and helped to review and comment on the initial and final drafts of the manuscript. All authors performed a critical review and approval of the final manuscript for interpretation of the data and important intellectual input.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
As stated in the methods section the study was performed in line with the principles of the Declaration of Helsinki, the approval was granted by the the Ethics Committee of the Second Affiliated Hospital of Suzhou University (internal code JD-LK2023025-I01).
Informed consent
Informed consent was obtained from the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pei, Y., Li, T., Chen, C. et al. Clinical features that predict the mortality risk in older patients with Omicron pneumonia: the MLWAP score. Intern Emerg Med 19, 465–475 (2024). https://doi.org/10.1007/s11739-023-03506-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03506-2