Abstract
Background
To develop a prediction model predicting in-hospital mortality of elder patients with community-acquired pneumonia (CAP) admitted to the intensive care unit (ICU).
Methods
In this cohort study, data of 619 patients with CAP aged ≥ 65 years were obtained from the Medical Information Mart for Intensive Care III (MIMIC III) 2001–2012 database. To establish the robustness of predictor variables, the sample dataset was randomly partitioned into a training set group and a testing set group (ratio: 6.5:3.5). The predictive factors were evaluated using multivariable logistic regression, and then a prediction model was constructed. The prediction model was compared with the widely used assessments: Sequential Organ Failure Assessment (SOFA), Pneumonia Severity Index (PSI), systolic blood pressure, oxygenation, age and respiratory rate (SOAR), CURB-65 scores using positive predictive value (PPV), negative predictive value (NPV), accuracy (ACC), area under the curve (AUC) and 95% confidence interval (CI). The decision curve analysis (DCA) was used to assess the net benefit of the prediction model. Subgroup analysis based on the pathogen was developed.
Results
Among 402 patients in the training set, 90 (24.63%) elderly CAP patients suffered from 30-day in-hospital mortality, with the median follow-up being 8 days. Hemoglobin/platelets ratio, age, respiratory rate, international normalized ratio, ventilation use, vasopressor use, red cell distribution width/blood urea nitrogen ratio, and Glasgow coma scales were identified as the predictive factors that affect the 30-day in-hospital mortality. The AUC values of the prediction model, the SOFA, SOAR, PSI and CURB-65 scores, were 0.751 (95% CI 0.749–0.752), 0.672 (95% CI 0.670–0.674), 0.607 (95% CI 0.605–0.609), 0.538 (95% CI 0.536–0.540), and 0.645 (95% CI 0.643–0.646), respectively. DCA result demonstrated that the prediction model could provide greater clinical net benefits to CAP patients admitted to the ICU. Concerning the pathogen, the prediction model also reported better predictive performance.
Conclusion
Our prediction model could predict the 30-day hospital mortality in elder patients with CAP and guide clinicians to identify the high-risk population.
Similar content being viewed by others
Introduction
Community-acquired pneumonia (CAP), defined as pneumonia acquired outside the hospital, is one of the most common infectious diseases in clinical practice [1, 2]. The incidence of pneumonia increases with age, with a 10 times higher hospitalization rate in patients aged 65 years and older (about 2000 per 100,000 per year) than in the younger population [3, 4]. CAP remains a common cause of intensive care unit (ICU) admissions and in-hospital mortality in the elderly [5, 6]. Approximately 75% of CAP patients require hospitalization, up to 10% of them need to be admitted to the ICU, and the in-hospital mortality from 4 to 20.9% in these patients, which poses a huge burden on families and society [7, 8]. Therefore, early identification of elderly CAP patients with high in-hospital mortality is crucial to timely and effective intervention for prognosis improvement.
Several pneumonia severity scores include the Sequential Organ Failure Assessment (SOFA), Pneumonia Severity Index (PSI), CURB-65, and systolic blood pressure, oxygenation, age and respiratory rate (SOAR) have been developed and used to predict outcomes in patients with CAP [9,10,11]. These scores are useful in the management of patient risk stratification, but there is still a lack of accurate assessment with regard to patient mortality [12]. Moreover, a common limitation of the above score systems is that a lot of variables cannot be obtained within the first 24 h after admission [13]. In addition to the scoring methods, in recent years, many blood biomarkers have been shown to play crucial roles in the early diagnosis and prognosis of pneumonia, including CAP [14, 15]. Serum albumin (ALB) level was reported to be associated with in-hospital mortality in patients with CAP [12]. The value of the red cell distribution width (RDW) has also been found in predicting the prognosis in critically ill patients [15]. A study demonstrated that the ALB-RDW score is the independent factor of 90-day mortality in patients with severe CAP [16]. Another study indicated neutrophil to lymphocyte (NLR) ratio was a promising candidate predictor of unfavorable outcomes in CAP patients [17]. However, there is a lack of research establishing prediction models to predict in-hospital mortality in CAP patients based on these biomarkers. Therefore, it is necessary to incorporate these biomarkers and develop new prediction models to achieve early assessment of in-hospital mortality risk in elderly CAP patients and guide clinical decision-making.
Herein, this study aimed to conduct a prediction model to predict the in-hospital mortality in elderly CAP patients and to compare the predictive value of the prediction model with SOFA, PSI, SOAR, and CURB-65 scoring system. We developed a simpler prediction model that may be beneficial to the decrease of in-hospital mortality in elder patients with CAP.
Methods
Study design and population
This study was a retrospective cohort study, and all data were obtained from the Medical Information Mart for Intensive Care III (MIMIC-III) 2001–2012. The MIMIC-III is a large, single-center, freely available database, which contained the comprehensive and high-quality medical records of 50,000 patients admitted to ICU at the Beth Israel Deaconess Medical Center between 2001 and 2012 [18]. Study inclusion criteria were (1) aged ≥ 65 years old; (2) population diagnosed with CAP at the time of admission to ICU. The exclusion criteria of this study were as follows: (1) the number of predictive factors that were not recorded during the first 24 h of the ICU stay exceeds 30% of the total number of predictive factors. Since the clinical data in this study were collected from a publicly available database, there were no local or state ethical issues.
Data collection
All the patients were inquired the clinical data, including (1) baseline characteristics: age (years), gender, marital status, ethnicity; (2) vital signs: heart rate (times/min), respiratory rate (breaths/min), temperature (°C), systolic blood pressure (SBP, mmHg), diastolic blood pressure (DBP, mmHg), mean arterial pressure (MAP, mmHg); (3) comorbidities: liver cirrhosis, congestive heart-failure (CHF), renal failure, chronic obstructive pulmonary disease (COPD), septic shock, effusion, emphysema, lung cancer, heart disease, diabetes mellitus (DM), respiratory failure, atrial fibrillation (AF), hyperlipidemia, malignant cancer; (4) scoring systems: SOFA score, Simplified Acute Physiology Score (SAPSII), SOAR score, PSI, CURB-65 score, Glasgow coma scales (GCS), International normalized ratio (INR), Elixhauser comorbidity score; (5) laboratory parameters: red blood cell (RBC, m/uL), white blood cells (WBC, K/uL), mean corpuscular volume (MCV, μm3), blood urea nitrogen (BUN), sodium (mEq/L), haematocrit, potassium (mEq/L), phosphate (mg/dL), calcium (mg/dL), magnesium (mg/dL), lactate (mmol/L), creatine kinase (IU/L), arterial pH, oxygen saturation (SpO2, %), partial carbon dioxide pressure (PCO2), partial oxygen pressure (PO2), fraction of inspired oxygen (FiO2); (6) pathogen: Streptococcus pneumoniae, Klebsiella pneumoniae, Legionella pneumophila, other Streptococcus, Staphylococcus, Ecoli, Candida, Acinetobacter, Clostridium, Citrobacter, Enterococcus, Pneumocystis pneumonia (PCP), other bacteria, virus, fungus, yeast; (7) treatments: invasive ventilation, ventilation, vasopressor; (8) inflammatory biomarker: NLR, platelet–lymphocyte ratio (PLR), prognostic nutritional index (PNI), anion gap, hemoglobin/platelets ratio (HPR), RDW/BUN ratio, absolute neutrophil count/ (white blood cell count-neutrophil count) (dNLR), BUN/ALB ratio, platelet count*(lymphocytes/neutrophil) (SII). Blood tests, pathogen detections, and scoring systems were performed on the first day after admission.
Variable definitions and outcome
CAP was defined as evidence of a pulmonary infiltrate on the chest radiograph and symptoms of lower respiratory infection, including cough, dyspnea, fever, and/or pleuritic chest pain, which were not acquired in a hospital or a nursing home.
PNI referred to 10 × ALB (g/dL) + 0.005 × lymphocytes count. SOFA score uses SBP ≤ 100 mmHg, respiratory rate ≥ 22/min, and altered cognitive state to identify high risk patients. The SOAR score identifies severe CAP using the following criteria (definitions of variables for data extraction are also listed below): SBP < 90 mmHg, PaO2/FiO2 ratio < 250, age ≥ 65, and respiratory rate ≥ 30 breaths/min. The CURB-65 index identifies high risk patients using the following criteria (definitions of variables for data extraction are also listed below): confusion, BUN ≥ 20 mg/dl, respiratory rate ≥ 30 breaths/min, SBP < 90 mmHg or DBP ≤ 60 mmHg, and age ≥ 65.
The study outcome was the 30-day in-hospital mortality rate. When the patient died in the hospital, the follow-up period ended. The median follow-up was 8 days.
Statistics analysis
The t-test was used to evaluate the normally distributed data which was presented as mean ± standard deviation (Mean ± SD). Mann Whitney U test was used to evaluate the non-normally distributed variables and data were presented as median and quartile M (Q1, Q3). Fisher's exact test was used to analyze the enumeration data and data were described as the number of cases and constituent ratio N (%). Multiple imputation was performed by “mice” R package for missing values. Sensitivity analysis was performed by comparing the data before and after imputation.
To establish the robustness of predictor variables, the sample dataset was randomly partitioned into the training set group and the testing set group (ratio: 6.5:3.5). P < 0.05 was considered statistically significant. To determine the predictive factors, variables achieving a significance level were selected for multivariable Logistic analysis and other variables that are significant in other studies were included. Then stepwise regression was performed to construct the final prediction model. The performance of the prediction model was evaluated by the Hosmer–Lemeshow (H–L) goodness-of-fit test, using positive predictive value (PPV), negative predictive value (NPV), accuracy (ACC), area under the curve (AUC), and 95% confidence interval (CI). To compare the performance of our prediction model with the SOFA, PSI, SOAR, and CURB-65, the DeLong test was applied. In addition, the decision curve analysis (DCA) was used to assess the net benefit of the prediction model and SOFA, PSI, SOAR, CURB-65. The total population was divided into subgroups to verify our prediction model.
Multiple imputation, DCA curve, and Logistic regression were performed using R Software (version 4.0.3; The R Project for Statistical Computing, TX, USA). ROC curves and prediction results were completed using Python 3.8. All remaining analyses were performed using SAS software (version 9.4; SAS Institute Inc., Cary, NC, USA).
Results
Characteristics of the included patients
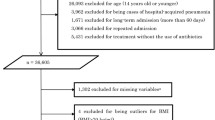
In total, 619 patients with CAP aged over 65 years were included in this study, with 217 patients in the testing set and 402 patients in the training set. The median follow-up was 8 days. The flow chart of the participants’ selection is shown in Fig. 1. The characteristics of the included patients between the testing set and the training set groups are described in Table 1. Among 402 patients in the training set, 90 (24.63%) elderly CAP patients suffered from 30-day in-hospital mortality; 41.41% (41 of 99) of the patients were male, while 58.59% (58 of 99) were women. The baseline and clinical characteristics between in-hospital mortality and non-in-hospital mortality are present in Table 2.
Identifications of the predictive factors for in-hospital mortality of elderly CAP patients
Factors achieving a significance level in the comparison of the in-hospital mortality and non-in-hospital mortality groups were septic shock (P = 0.003), respiratory failure (P = 0.009), respiratory rate (P = 0.027), SOFA score (P < 0.001), SAPSII score (P < 0.001), SOAR (P < 0.001), CURB-65 score (P < 0.001), GCS (P < 0.001), INR (P = 0.002), other bacteria (P = 0.001), yeast (P = 0.006), MCV (P = 0.038), RBC (P = 0.024), phosphate (P = 0.013), Ph (P = 0.009), invasive ventilation (P < 0.001), ventilation (P < 0.001), vasopressor (P < 0.001), PNI (P = 0.002), RDW/BUN ratio (P < 0.001), BUN/ALB ratio (P = 0.004) (Table 2). The above significant variables were included in multivariate logistic regression, and the significant variables in other studies were added to the multivariate model, including HPR, age, gender, ethnicity, anion gap, and Elixhauser comorbidity score. Finally, HPR [risk ratio (RR): 1.429, 95% CI 1.030–1.985, Pr > Chi-square: 0.033], age (RR: 1.017, 95% CI 0.984–1.05, Pr > Chi-square: 0.325), respiratory rate (RR: 1.049, 95% CI 1.012–1.087, Pr > Chi-square: 0.009), INR (RR: 1.363, 95% CI 1.077–1.724, Pr > Chi-square: 0.010), ventilation (RR: 1.974, 95% CI 1.084–3.592, Pr > Chi-square: 0.026), vesopressor (RR:4.201, 95% CI 1.643–10.743, Pr > Chi-square: 0.003), RDW/BUN (RR: 1.192, 95% CI 1.029–1.38, Pr > Chi-square: 0.019), GCS (RR: 0.919, 95% CI 0.861–0.982, Pr > Chi-square: 0.013) were the predictive factors for in-hospital mortality of elderly CAP patients. The predictive factors for in-hospital mortality of elderly CAP patients are shown in Table 3.
Prediction model construction and evaluations
Based on the predictive factors, the prediction model for predicting in-hospital mortality of elderly CAP patients was constructed. Table 3 shows the detailed information of our prediction model. The final prediction model is.
y = − 4.83 + 0.36*HPR + 0.016age + 0.05*respiratory rate + 0.31*INR + 0.68*ventilation (yes = 1, no = 0) + 1.44*vasopressor (yes = 1, no = 0) + 0.176*RDW/BUN − 0.08GCS.
The chi-square and P values of the H–L goodness of fit of our model in the training set and testing set were χ2 = 3.502, P = 0.899, χ2 = 7.196, P = 0.516, respectively, indicating that our model showed good goodness-of-fit. In addition, In the training set, the PPV, NPV, AUC, and ACC of the prediction model were 0.529 (95% CI 0.433–0.626), 0.850 (95% CI 0.810–0.890), 0.751 (95% CI 0.749–0.752), 0.769 (95% CI 0.727–0.810), respectively. The results of the prediction model evaluation are described in Table 4. The DCA results indicated that the prediction model had a good ability for predicting in-hospital mortality of elderly CAP patients. DCA result of the prediction model is shown in Fig. 2.
For the external validation of the prediction model, the result showed that the AUC our prediction model was 0.703, higher than SOFA (AUC: 0.686), SOAR (0.564), PSI (0.613), and CURB-65 (0.570).
Comparison of the predictive performances between the prediction model and SOFA, SOAR, PSI, and CURB-65 scores
We calculated the AUC value of the prediction model and four other scoring systems as shown in Fig. 3. The AUC value of the prediction model was 0.751 (95% CI 0.749–0.752), while those of the SOFA, SOAR, PSI and CURB-65 scores were 0.672 (95% CI 0.670–0.674), 0.607 (95% CI 0.605–0.609), 0.538 (95% CI 0.536–0.540), and 0.645 (95% CI 0.643–0.646), respectively. PPV, NPV, and ACC were also calculated to compare the predictive performance of the prediction model and SOFA, SOAR, PSI, and CURB-65 scores. Details of the performance are shown in Table 4.
The predictive performances of the prediction model and SOFA, SOAR, PSI, and CURB-65 scores in the subgroup analysis based on the pathogen
Based on bacteria pathogen, the prediction model showed a higher AUC compared with SOFA, SOAR, PSI and CURB-65 scores, with AUC being 0.727 (95% CI 0.725–0.729), 0.632 (95% CI 0.630–0.634), 0.617(95% CI 0.616–0.619), 0.563(95% CI 0.561–0.565), 0.640 (95% CI 0.639–0.642), respectively. Concerning other pathogens, the prediction model also reported better predictive performance. The predictive performances of the prediction model and SOFA, SOAR, PSI, and CURB-65 scores based on the pathogen are shown in Table 5.
Discussion
CAP is a global infectious disease that causes high morbidity and mortality. Accurate and timely identification of patients at high risk of mortality is one of the most important works of physicians. In this study, patients with CAP 30-day mortality rate was 24.63%, slightly higher than the previous related literature reports, this may be because of the large cases included in the ICU, and the age, basic diseases, or a minority of the critically ill patient into the hospital later on. We identified HPR, RDW/BUN ratio, age, respiratory rate, INR, GCS, ventilation use, and vasopressor use were independent predictive factors that were related to the hospital mortality of elderly CAP patients. Based on the predictive factors, our prediction model showed a better predictive performance with an AUC being 0.751. Our model also showed good goodness-of-fit. The prediction model also demonstrated better predictive performances than the SOFA, PSI, SOAR, and CURB-65 scoring systems.
The widespread application of scoring systems in clinical practice has brought great benefits to the management of CAP. However, these assessment scales do have limitations. PSI contains 20 variables and is very complex for prediction, these variables are usually not available at the initial visit, which may affect its promotion and implementation in daily practice. The CURB-65 score may not perform a suitable outcome in patients over the age of 70 due to its low sensitivity [19]. The SOFA score is unduly dependent on clinical therapeutic interventions which fail to be mastered easily [13]. SOAR might be more suitable for assessing disease severity, particularly in the elderly [19]. However, SOAR for in-hospital mortality needs further confirmation. Furthermore, our study showed that these scoring systems have only moderate AUC. Zhang et al. conducted a new prediction model for assessing the clinical outcomes of ICU patients with CAP [20]. However, the AUC of this model was 0.661. Another study with age, congestive heart failure, dementia, respiratory rate and BUN level being predictive factors to develop a prediction model to predict 1-year mortality after hospitalization for CAP. Nevertheless, the C-index was only. 0.76. In addition, the model only focuses on out-of-hospital mortality and only focuses on single biomarkers. The variables considered in our prediction model are more complete. Based on the predictive factors including HPR, RDW/BUN ratio, age, respiratory rate, INR, GCS, ventilation use, and vasopressor use, our prediction model was conducted. our prediction model demonstrated a higher AUC than the scoring systems, with an AUC being 0.751. Moreover, our prediction model was constructed based on the predictive factor that has the benefit of being easily calculated and not dependent on operator capacity to correctly gauge the level of confusion in a patient.
Our study demonstrated that RDW/BUN ratio and HPR were associated with in-hospital mortality of elderly CAP patients. The predictive value of the RDW/BUN ratio on the in-hospital mortality of elderly CAP patients may be due to the prognostic value of RDW and BUN. The RDW can be obtained immediately from blood routine reports, which has been found to be associated with mortality in patients with CAP [21, 22]. Ge et al. also confirmed that elevated RDW and WBC increased mortality in adult CAP patients [23]. Inflammation and oxidative stress caused by infection were thought to be the mechanisms of RDW and infectious diseases. Erythropoietin regulates myelogenesis, red cell maturation, and survival and was previously considered to be one of the major determinants of RDW [24]. Abnormal production of erythropoietin or the body's low response to erythropoietin will lead to a gradual increase in RDW value [25]. CAP is a typical infectious disease, during which Inflammation stimulates the release of inflammatory factors, damages the activity of erythropoietin, prevents the maturation of RBCs, leads to the production of ineffective RBCs, increases the heterogeneity of RBC size, and RDW value [26]. Increased RDW values have been reported to be correlated with inflammatory markers, indicating that C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are high when RDW is high [27]. BUN is produced by the metabolism of protein and amino acids in the body, then hydrolyzed by the liver and excreted by the kidney with urine [28]. Due to this complex interplay of modulatory factors, BUN is generally used as a surrogate marker of systemic illness rather than a specific marker of renal dysfunction [29]. BUN ≥ 7 mmol was one of the CURB-65 scoring criteria for CAP [30]. In a retrospective study by Kang et al. in China that evaluated 4880 patients aged ≥ 65 with CAP, BUN was a prognostic factor for in-hospital mortality [31]. Uematsu et al. reported that elevated BUN had a significantly higher risk of 30-day mortality in CAP patients [32]. RDW/BUN ratio may be a simple and potentially useful prognostic factor of in-hospital mortality in elderly CAP patients. The HPR was calculated based on the hemoglobin and platelet counts. Patients with CAP often exhibit a declining hemoglobin concentration [33]. A study of patients with CAP found that hemoglobin levels < 10 g/dL were independently associated with 90-day mortality [34]. Abnormal platelet count has previously been related to different complications in patients with CAP admitted to ICU [35]. Rising platelet count throughout hospitalization has been found to be a powerful predictor of better survival, while declining platelet count predicts poor outcomes [36]. Tang et al. found that preoperative HPR can be taken into account as a factor predictive of oncological outcomes for stage 1 and grade 3 bladder cancer, particularly disease progression and mortality outcomes [37]. The HPR can be used as a veritable blood biomarker to predict the in-hospital mortality of elder patients with CAP.
Age, respiratory rate, ventilation use, vesopressor use, GCS could also predict the in-hospital mortality of elderly CAP patients in this study. A study evaluating the prognostic factors in hospitalized CAP identified age, respiratory rate, and mechanical ventilation as prognostic factors of in-hospitalized CAP patients [30]. Braunet al. found that variables associated with an increased risk of 90-day mortality included age ≥ 51 years [38]. A study by Baek et al. found that mechanical ventilation was associated with in-hospital mortality of pneumonia [39]. GCS is the most widely accepted tool for evaluating consciousness [40]. Wang et al. identified GCS as an independent predictor that was closely related to the hospital mortality of severe CAP [13].
Our predictive factors are routinely and rapidly measured in patients in a hospital setting; our prediction model therefore may be a useful early tool in predicting elderly CAP patients with a high risk of in-hospital mortality, who require rapid and timely decision making. There are several limitations to this study. First, considering the retrospective design, and the limitation of the sampling analysis, selection and sampling bias cannot be excluded. Second, this study only included hospitalized patients; therefore, it is difficult to generalize these findings to all CAP patients. Third, as no external validation was conducted in this study, the applicability of the prediction model in clinical practice requires further study. Therefore, the results should be interpreted cautiously when applied in other clinical settings. Further multicenter studies with populations of different geographic areas, a larger number of subjects, and above all, a prospective design are needed to corroborate the additive value of these markers to clinical prediction models to provide a safer and more effective assessment tool for clinicians.
Conclusion
HPR, age, respiratory rate, INR, ventilation use, vasopressor use, RDW/BUN ratio, and GCS can be used as the factors to predict the in-hospital mortality of elderly CAP patients. The prediction model based on these predictive factors can help clinicians to make clinical decisions timely and early, and decrease the in-hospital mortality of elder patients with CAP admitted to the ICU.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the MIMIC-III database, https://mimic.mit.edu/docs/gettingstarted/.
Abbreviations
- CAP:
-
Community-acquired pneumonia
- ICU:
-
Intensive care unit
- SOFA:
-
Sequential Organ Failure Assessment
- PSI:
-
Pneumonia Severity Index
- ALB:
-
Serum albumin
- MIMIC-III:
-
Medical Information Mart for Intensive Care III
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- MAP:
-
Mean arterial pressure
- CHF:
-
Congestive heart-failure
- COPD:
-
Chronic obstructive pulmonary disease
- DM:
-
Diabetes mellitus; atrial fibrillation
- SAPSII:
-
Simplified Acute Physiology Score
- GCS:
-
Glasgow coma scales
- INR:
-
International normalized ratio
- RBC:
-
Red blood cell
- WBC:
-
White blood cell
- MCV:
-
Mean corpuscular volume
- BUN:
-
Blood urea nitrogen
- SpO2 :
-
Oxygen saturation
- PCO2 :
-
Partial carbon dioxide pressure
- PO2 :
-
Partial oxygen pressure
- FiO2 :
-
Fraction of inspired oxygen
- PCP:
-
Pneumocystis pneumonia
- PLR:
-
Platelet–lymphocyte ratio
- PNI:
-
Prognostic nutritional index
References
Cuypers F, Schäfer A, Skorka SB, Surabhi S, Tölken LA, Paulikat AD, et al. Innate immune responses at the asymptomatic stage of influenza A viral infections of Streptococcus pneumoniae colonized and non-colonized mice. Sci Rep. 2021;11(1):20609.
Ghia CJ, Rambhad GS. Systematic review and meta-analysis of comorbidities and associated risk factors in Indian patients of community-acquired pneumonia. SAGE Open Med. 2022;10:20503121221095484.
Divino V, Schranz J, Early M, Shah H, Jiang M, DeKoven M. The annual economic burden among patients hospitalized for community-acquired pneumonia (CAP): a retrospective US cohort study. Curr Med Res Opin. 2020;36(1):151–60.
McLaughlin JM, Khan FL, Thoburn EA, Isturiz RE, Swerdlow DL. Rates of hospitalization for community-acquired pneumonia among US adults: a systematic review. Vaccine. 2020;38(4):741–51.
Huang HR, Cho SJ, Harris RM, Yang J, Bermejo S, Sharma L, et al. RIPK3 activates MLKL-mediated necroptosis and inflammasome signaling during Streptococcus infection. Am J Respir Cell Mol Biol. 2021;64(5):579–91.
Brown JD, Harnett J, Chambers R, Sato R. The relative burden of community-acquired pneumonia hospitalizations in older adults: a retrospective observational study in the United States. BMC Geriatr. 2018;18(1):92.
Ma HM, Tang WH, Woo J. Predictors of in-hospital mortality of older patients admitted for community-acquired pneumonia. Age Ageing. 2011;40(6):736–41.
Guo S, Mao X, Liang M. The moderate predictive value of serial serum CRP and PCT levels for the prognosis of hospitalized community-acquired pneumonia. Respir Res. 2018;19(1):193.
Kolditz M, Ewig S, Höffken G. Management-based risk prediction in community-acquired pneumonia by scores and biomarkers. Eur Respir J. 2013;41(4):974–84.
Zhang X, Liu B, Liu Y, Ma L, Zeng H. Efficacy of the quick sequential organ failure assessment for predicting clinical outcomes among community-acquired pneumonia patients presenting in the emergency department. BMC Infect Dis. 2020;20(1):316.
Bradley J, Sbaih N, Chandler TR, Furmanek S, Ramirez JA, Cavallazzi R. Pneumonia severity index and CURB-65 score are good predictors of mortality in hospitalized patients with SARS-CoV-2 community-acquired pneumonia. Chest. 2022;161(4):927–36.
Zhao L, Bao J, Shang Y, Zhang Y, Yin L, Yu Y, et al. The prognostic value of serum albumin levels and respiratory rate for community-acquired pneumonia: a prospective, multi-center study. PLoS ONE. 2021;16(3):e0248002.
Wang X, Jiao J, Wei R, Feng Y, Ma X, Li Y, et al. A new method to predict hospital mortality in severe community acquired pneumonia. Eur J Intern Med. 2017;40:56–63.
Menéndez R, Méndez R, Aldás I, Reyes S, Gonzalez-Jimenez P, España PP, et al. Community-acquired pneumonia patients at risk for early and long-term cardiovascular events are identified by cardiac biomarkers. Chest. 2019;156(6):1080–91.
Jeong JH, Heo M, Lee SJ, Jeong YY, Lee JD, Yoo JW. Clinical usefulness of red cell distribution width/albumin ratio to discriminate 28-day mortality in critically ill patients with pneumonia receiving invasive mechanical ventilation, compared with lacate/albumin ratio: a retrospective cohort study. Diagnostics (Basel, Switzerland). 2021;11(12):2344.
Chen L, Lu XY, Zhu CQ. Prognostic value of albumin-red cell distribution width score in patients with severe community-acquired pneumonia. Ann Palliat Med. 2020;9(3):759–65.
Lv C, Chen Y, Shi W, Pan T, Deng J, Xu J. Comparison of different scoring systems for prediction of mortality and ICU admission in elderly CAP population. Clin Interv Aging. 2021;16:1917–29.
Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, et al. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035.
Subramanian DN, Musonda P, Sankaran P, Tariq SM, Kamath AV, Myint PK. Performance of SOAR (systolic blood pressure, oxygenation, age and respiratory rate) scoring criteria in community-acquired pneumonia: a prospective multi-centre study. Age Ageing. 2013;42(1):94–7.
Zhang S, Zhang K, Yu Y, Tian B, Cui W, Zhang G. A new prediction model for assessing the clinical outcomes of ICU patients with community-acquired pneumonia: a decision tree analysis. Ann Med. 2019;51(1):41–50.
Lee SM, Lee JH, Kim K, Jo YH, Lee J, Kim J, et al. The clinical significance of changes in red blood cell distribution width in patients with community-acquired pneumonia. Clin Exp Emerg Med. 2016;3(3):139–47.
Ren Q, Liu H, Wang Y, Dai D, Tian Z, Jiao G, et al. The role of red blood cell distribution width in the severity and prognosis of community-acquired pneumonia. Can Respir J. 2021;2021:8024024.
Ge YL, Liu CH, Rana MA, Zhu XY, Wang N, Xu J, et al. Elevated red blood cell distribution width combined white blood cell in peripheral blood routine have a better sensitivity than CURB-65 scores in predicting ICU admission and mortality in adult community-acquired pneumonia patients. Clin Lab. 2019; 65(3).
Lippi G, Franchini M, Salvagno GL, Guidi GC. Biochemistry, physiology, and complications of blood doping: facts and speculation. Crit Rev Clin Lab Sci. 2006;43(4):349–91.
Afsar B, Saglam M, Yuceturk C, Agca E. The relationship between red cell distribution width with erythropoietin resistance in iron replete hemodialysis patients. Eur J Intern Med. 2013;24(3):e25–9.
Förhécz Z, Gombos T, Borgulya G, Pozsonyi Z, Prohászka Z, Jánoskuti L. Red cell distribution width in heart failure: prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. Am Heart J. 2009;158(4):659–66.
Miyamoto K, Inai K, Takeuchi D, Shinohara T, Nakanishi T. Relationships among red cell distribution width, anemia, and interleukin-6 in adult congenital heart disease. Circ J. 2015;79(5):1100–6.
van Veldhuisen DJ, Ruilope LM, Maisel AS, Damman K. Biomarkers of renal injury and function: diagnostic, prognostic and therapeutic implications in heart failure. Eur Heart J. 2016;37(33):2577–85.
Agarwal M, Joshi M, Gupta M, Bharti N, Chakraborti A, Sonigra M. Role of blood urea nitrogen and serum albumin ratio in predicting severity of community acquired pneumonia (CAP). Monaldi Arch Chest Dis Archivio Monaldi per le malattie del torace. 2021; 92(3).
Ito A, Ishida T, Tokumasu H, Washio Y, Yamazaki A, Ito Y, et al. Prognostic factors in hospitalized community-acquired pneumonia: a retrospective study of a prospective observational cohort. BMC Pulm Med. 2017;17(1):78.
Kang Y, Fang XY, Wang D, Wang XJ. Activity of daily living upon admission is an independent predictor of in-hospital mortality in older patients with community-acquired pneumonia. BMC Infect Dis. 2021;21(1):314.
Uematsu H, Kunisawa S, Sasaki N, Ikai H, Imanaka Y. Development of a risk-adjusted in-hospital mortality prediction model for community-acquired pneumonia: a retrospective analysis using a Japanese administrative database. BMC Pulm Med. 2014;14:203.
Schoorl M, Snijders D, Schoorl M, Boersma WG, Bartels PC. Transient impairment of reticulocyte hemoglobin content and hepcidin-25 induction in patients with community-acquired pneumonia. Scand J Clin Lab Investig. 2013;73(1):54–60.
Reade MC, Weissfeld L, Angus DC, Kellum JA, Milbrandt EB. The prevalence of anemia and its association with 90-day mortality in hospitalized community-acquired pneumonia. BMC Pulm Med. 2010;10:15.
Wool GD, Miller JL. The impact of COVID-19 disease on platelets and coagulation. Pathobiol J Immunopathol Mol Cell Biol. 2021;88(1):15–27.
Gorelik O, Izhakian S, Barchel D, Almoznino-Sarafian D, Tzur I, Swarka M, et al. Prognostic significance of platelet count changes during hospitalization for community-acquired pneumonia. Platelets. 2017;28(4):380–6.
Tang G, Zhen Y, Xie W, Wang Y, Chen F, Qin C, et al. Preoperative hemoglobin-platelet ratio can significantly predict progression and mortality outcomes in patients with T1G3 bladder cancer undergoing transurethral resection of bladder tumor. Oncotarget. 2018;9(26):18627–36.
Braun E, Domany E, Kenig Y, Mazor Y, Makhoul BF, Azzam ZS. Elevated red cell distribution width predicts poor outcome in young patients with community acquired pneumonia. Crit Care (Lond, Engl). 2011;15(4):R194.
Baek MS, Park S, Choi JH, Kim CH, Hyun IG. Mortality and prognostic prediction in very elderly patients with severe pneumonia. J Intensive Care Med. 2020;35(12):1405–10.
Suresh V, Yaddanapudi LN, Podder S. Full outline of unresponsiveness score versus glasgow coma scale in critically ill patients with altered sensorium: a comparison of inter-observer variability and outcomes. Indian J Anaesth. 2019;63(8):640–7.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
NL and WC designed the study. NL wrote the manuscript. NL and WC collected, analyzed and interpreted the data. WC critically reviewed, edited and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The project was approved by the Institutional Review Boards of Beth Israel Deaconess Medical Center (Boston, MA) and the Massachusetts Institute of Technology (Cambridge, MA). Since the clinical data in this study were collected from a publicly available database, there were no local or state ethical issues. All individuals provided written informed consent before participating in the study. All methods were carried out in accordance with relevant guidelines and regulations (declaration of Helsinki).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, N., Chu, W. Development and validation of a survival prediction model in elder patients with community-acquired pneumonia: a MIMIC-population-based study. BMC Pulm Med 23, 23 (2023). https://doi.org/10.1186/s12890-023-02314-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02314-w