Abstract
Background
Minimally invasive surgery may introduce new ergonomic challenges for surgeons. Increased patient body mass index (BMI) may further add to this ergonomic stress.
Objectives
The objective of this study was to quantify the ergonomic impact of patient BMI on surgeons during laparoscopic surgery.
Setting
University Hospital, USA.
Methods
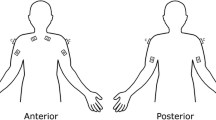
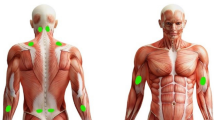
This prospective cohort study analyzed five minimally invasive surgeons during 24 laparoscopic procedures. Each subject’s muscle stress was assessed by recording surface electromyography (EMG) data from eight upper body muscle groups during laparoscopic procedures. EMG data was normalized against the maximal voluntary contraction (MVC) of each muscle measured before the start of surgery to create a percentage of the MVC value (%MVC). Subject workload was assessed through the NASA Task Load Index (NTLX). Statistical analysis was used to determine significance between surgeons operating on patients with or without obesity for %MVC and NTLX scores.
Results
There was no significant difference (p > 0.05) in both the average muscle activation of all eight muscle groups and NTLX scores during laparoscopic surgery in surgeons operating on patients with BMI > = 30 compared with patients with a BMI < 30.
Conclusions
We detected no differences in ergonomic stress or workload for surgeons operating on patients with or without obesity. For surgeons, the laparoscopic approach may offer an additional advantage over open surgery in patients with obesity. This advantage may be due to an “equalizing effect” of laparoscopy—that surgical ergonomics are less affected by the BMI of the patient when using laparoscopic tools.


Similar content being viewed by others
References
Park A, Lee G, Seagull FJ, et al. Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg. 2010;210:306–13.
Lee J, Mabardy A, Kermani R, et al. Laparoscopic vs open ventral hernia repair in the era of obesity. JAMA Surg. 2013;148:723–6.
Lomanto D, Iyer SG, Shabbir A, et al. Laparoscopic versus open ventral hernia mesh repair: a prospective study. Surg Endosc. 2006;20:1030–5.
Schauer PR, Ikramuddin S, McLaughlin RH, et al. Comparison of laparoscopic versus open repair of paraesophageal hernia. Am J Surg. 1998;176:659–65.
Tanphiphat C, Tanprayoon T, Sangsubhan C, et al. Laparoscopic vs open inguinal hernia repair. A randomized, controlled trial. Surg Endosc. 1998;12:846–51.
Schauer PR, Ikramuddin S. Laparoscopic surgery for morbid obesity. Surg Clin North Am. 2001;81:1145–79.
NIH Consensus conference. Gallstones and laparoscopic cholecystectomy. JAMA. 1993;269:1018–24.
Berguer R, Chen J, Smith WD. A comparison of the physical effort required for laparoscopic and open surgical techniques. Arch Surg. 2003;138:967–70.
Zihni AM, Ohu I, Cavallo JA, et al. Ergonomic analysis of robot-assisted and traditional laparoscopic procedures. Surg Endosc. 2014;28:3379–84.
Wang R, Liang Z, Zihni AM, et al. Which causes more ergonomic stress: laparoscopic or open surgery? Surg Endosc. 2017;8:3286–90.
Zihni AM, Cavallo JA, Ray S, et al. Ergonomic analysis of primary and assistant surgical roles. J Surg Res. 2016;203:301–5.
Lee GI, Lee MR, Clanton T, et al. Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc. 2014;28:456–65.
Zihni AM, Ohu I, Cavallo JA, et al. FLS tasks can be used as an ergonomic discriminator between laparoscopic and robotic surgery. Surg Endosc. 2014;28:2459–65.
Lee G, Lee T, Dexter D, et al. Methodological infrastructure in surgical ergonomics: a review of tasks, models, and measurement systems. Surg Innov. 2007;14:153–67.
Lee G, Lee T, Dexter D, et al. Ergonomic risk associated with assisting in minimally invasive surgery. Surg Endosc. 2009;23:182–8.
Zihni A, Ge T, Ray S, et al. Transfer and priming of surgical skills across minimally invasive surgical platforms. J Surg Res. 2016;206:48–52.
Sundbom M. Laparoscopic revolution in bariatric surgery. World J Gastroenterol. 2014;20:15135–43.
Pasam RT, Esemuede IO, Lee-Kong SA, et al. The minimally invasive approach is associated with reduced surgical site infections in obese patients undergoing proctectomy. Tech Coloproctol. 2015;19:733–43.
Hardiman K, Chang ET, Diggs BS, et al. Laparoscopic colectomy reduces morbidity and mortality in obese patients. Surg Endosc. 2013;27:2907–10.
Scheib SA, Tanner E, Green IC, et al. Laparoscopy in the morbidly obese: physiologic considerations and surgical techniques to optimize success. J Minim Invasive Gynecol. 2014;21:182–95.
Acknowledgements
This work was supported by the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) [2012] and Intuitive, Surgical Inc. [2013].
Funding
This work was supported by the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) [2012] and Intuitive, Surgical Inc. [2013].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liang, Z., Gerull, W.D., Wang, R. et al. Effect of Patient Body Mass Index on Laparoscopic Surgical Ergonomics. OBES SURG 29, 1709–1713 (2019). https://doi.org/10.1007/s11695-019-03748-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03748-0