Abstract
Introduction
Robotic surgery may result in ergonomic benefits to surgeons. In this pilot study, we utilize surface electromyography (sEMG) to describe a method for identifying ergonomic differences between laparoscopic and robotic platforms using validated Fundamentals of Laparoscopic Surgery (FLS) tasks. We hypothesize that FLS task performance on laparoscopic and robotic surgical platforms will produce significant differences in mean muscle activation, as quantified by sEMG.
Methods
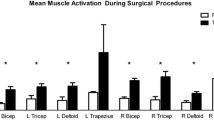
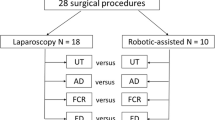
Six right-hand-dominant subjects with varying experience performed FLS peg transfer (PT), pattern cutting (PC), and intracorporeal suturing (IS) tasks on laparoscopic and robotic platforms. sEMG measurements were obtained from each subject’s bilateral bicep, tricep, deltoid, and trapezius muscles. EMG measurements were normalized to the maximum voluntary contraction (MVC) of each muscle of each subject. Subjects repeated each task three times per platform, and mean values used for pooled analysis. Average normalized muscle activation (%MVC) was calculated for each muscle group in all subjects for each FLS task. We compared mean %MVC values with paired t tests and considered differences with a p value less than 0.05 to be statistically significant.
Results
Mean activation of right bicep (2.7 %MVC lap, 1.3 %MVC robotic, p = 0.019) and right deltoid muscles (2.4 %MVC lap, 1.0 %MVC robotic, p = 0.019) were significantly elevated during the laparoscopic compared to the robotic IS task. The mean activation of the right trapezius muscle was significantly elevated during robotic compared to the laparoscopic PT (1.6 %MVC lap, 3.5 %MVC robotic, p = 0.040) and PC (1.3 %MVC lap, 3.6 %MVC robotic, p = 0.0018) tasks.
Conclusions
FLS tasks are validated, readily available instruments that are feasible for use in demonstrating ergonomic differences between surgical platforms. In this study, we used FLS tasks to compare mean muscle activation of four muscle groups during laparoscopic and robotic task performance. FLS tasks can serve as the basis for larger studies to further describe ergonomic differences between laparoscopic and robotic surgery.


Similar content being viewed by others
References
Bhogal RH, Athwal R, Durkin D, Deakin M, Cheruvu CN (2008) Comparison between open and laparoscopic repair of perforated peptic ulcer disease. World J Surg 32:2371–2374
Wilson CH, Sanni A, Rix DA, Soomro NA (2011) Laparoscopic versus open nephrectomy for live kidney donors. Cochrane Database Syst Rev. doi:10.1002/14651858.CD006124
Li MZ, Lian L, Xiao LB, Wu WH, He YL, Song XM (2012) Laparoscopic versus open adhesiolysis in patients with adhesive small bowel obstruction: a systematic review and meta-analysis. Am J Surg 204:779–786
Sari V, Nieboer TE, Vierhout ME, Stegeman DF, Kluivers KB (2010) The operation room as a hostile environment for surgeons: physical complaints during and after laparoscopy. Minim Invasive Ther Allied Technol 19:105–109
Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D (2010) Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg 210:306–313
Berguer R, Smith WD, Chung YH (2001) Performing laparoscopic surgery is significantly more stressful for the surgeon than open surgery. Surg Endosc 15:1204–1207
Berguer R, Chen J, Smith WD (2003) A comparison of the physical effort required for laparoscopic and open surgical techniques. Arch Surg 138:967–970
Lee G, Lee T, Dexter D, Godinez C, Meenaghan N, Catania R, Park A (2009) Ergonomic risk associated with assisting in minimally invasive surgery. Surg Endosc 23:182–188
Berguer R (1998) Surgical technology and the ergonomics of laparoscopic instruments. Surg Endosc 12:458–462
O’Sullivan OE, O’Reilly BA (2012) Robot-assisted surgery: impact on gynaecological and pelvic floor reconstructive surgery. Int Urogynecol J 23:1163–1173
Kumar P, Kommu SS, Challacombe BJ, Dasgup-Ta P (2010) Laparoendoscopic single-site surgery (LESS) prostatectomy–robotic and conventional approach. Minerva Urol Nefrol 62:425–430
Lunca S, Bouras G, Stanescu AC (2005) Gastrointestinal robot-assisted surgery. A current perspective. Rom J Gastroenterol 14:385–391
Xia T, Baird C, Jallo G, Hayes K, Nakajima N, Hata N, Kazanzides P (2008) An integrated system for planning, navigation and robotic assistance for skull base surgery. Int J Med Robot 4:321–330
Frick AC, Falcone T (2009) Robotics in gynecologic surgery. Minerva Ginecol 61:187–199
Wright AS, Gould JC, Melvin WS (2004) Computer-assisted robotic antireflux surgery. Minerva Gastroenterol Dietol 50:253–260
Anton D, Gerr F, Meyers A, Cook TM, Rosecrance JC, Reynolds J (2007) Effect of aviation snip design and task height on upper extremity muscular activity and wrist posture. J Occup Environ Hyg 4:99–113
Jones T, Kumar S (2008) Comparison of ergonomic risk assessment output in a repetitive sawmill occupation: trim-saw operator. Work 31:367–376
Lee G, Lee T, Dexter D, Klein R, Park A (2007) Methodological infrastructure in surgical ergonomics: a review of tasks, models, and measurement systems. Surg Innov 14:153–167
Lofland KR, Mumby PB, Cassisi JE, Palumbo NL, Camic PM (1995) Assessment of lumbar EMG during static and dynamic activity in pain-free normals: implications for muscle scanning protocols. Biofeedback Self Regul 20:3–18
Edelman DA, Mattos MA, Bouwman DL (2012) Value of fundamentals of laparoscopic surgery training in a fourth-year medical school advanced surgical skills elective. J Surg Res 177:207–210
Antosh DD, Auguste T, George EA, Sokol AI, Gutman RE, Iglesia CB, Desale SY, Park AJ (2013) Blinded assessment of operative performance after fundamentals of laparoscopic surgery in gynecology training. J Minim Invasive Gynecol 20:353–359
Sweet RM, Beach R, Sainfort F, Gupta P, Reihsen T, Poniatowski LH, McDougall EM (2011) Introduction and validation of the American Urological Association Basic Laparoscopic Urologic Surgery skills curriculum. J Endourol 26:190–196
Berguer R, Smith W (2006) An ergonomic comparison of robotic and laparoscopic technique: the influence of surgeon experience and task complexity. J Surg Res 134:87–92
Lee GI, Lee MR, Clanton T, Sutton E, Park AE, Marohn MR (2013) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28:456–465
Vassiliou MC, Dunkin BJ, Marks JM, Fried GM (2010) FLS and FES: comprehensive models of training and assessment. Surg Clin N Am 90:535–558
Acknowledgments
The authors thank Gyusung Lee, PhD of the Department of Surgery at Johns Hopkins University (Baltimore, MD) for his valuable advice. This study was supported by a research grant from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES), and also by a research grant from Intuitive Surgical, Inc. (Sunnyvale, CA).
Disclosures
Dr. Zihni has received research grant funding for unrelated studies from the National Institutes of Health. Dr. Cavallo has received research grant funding for unrelated studies from the National Institutes of Health, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), and the American Hernia Society in collaboration with Davol® Incorporated; and has served as a one-time consultant for Guidepoint Global® Incorporated. Dr. Cho has received research grant funding from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) and Intuitive, Surgical Inc. (Sunnyvale, CA). Dr. Awad has received research grant funding from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) and Intuitive, Surgical Inc. (Sunnyvale, CA). Mr. Ohu and Ms. Ousley have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zihni, A.M., Ohu, I., Cavallo, J.A. et al. FLS tasks can be used as an ergonomic discriminator between laparoscopic and robotic surgery. Surg Endosc 28, 2459–2465 (2014). https://doi.org/10.1007/s00464-014-3497-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3497-7