Abstract
Background
There is increasing awareness of potential ergonomic challenges experienced by the laparoscopic surgeon. The purpose of this study is to quantify and compare the ergonomic stress experienced by a surgeon while performing open versus laparoscopic portions of a procedure. We hypothesize that a surgeon will experience greater ergonomic stress when performing laparoscopic surgery.
Methods
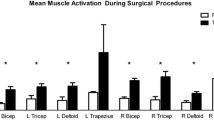
We designed a study to measure upper-body muscle activation during the laparoscopic and open portions of sigmoid colectomies in a single surgeon. A sample of five cases was recorded over a two-month time span. Each case contained significant portions of laparoscopic and open surgery. We obtained whole-case electromyography (EMG) tracings from bilateral biceps, triceps, deltoid, and trapezius muscles. After normalization to a maximum voltage of contraction (%MVC), these EMG tracings were used to calculate average muscle activation during the open and laparoscopic segments of each procedure. Paired Student’s t test was used to compare the average muscle activation between the two groups (*p < 0.05 considered statistically significant).
Results
Significant reductions in mean muscle activation in laparoscopic compared to open procedures were noted for the left triceps (4.07 ± 0.44% open vs. 2.65 ± 0.54% lap, 35% reduction), left deltoid (2.43 ± 0.45% open vs. 1.32 ± 0.16% lap, 46% reduction), left trapezius (9.93 ± 0.1.95% open vs. 4.61 ± 0.67% lap, 54% reduction), right triceps (2.94 ± 0.62% open vs. 1.85 ± 0.28% lap, 37% reduction), and right trapezius (10.20 ± 2.12% open vs. 4.69 ± 1.18% lap, 54% reduction).
Conclusions
Contrary to our hypothesis, the laparoscopic approach provided ergonomic benefit in several upper-body muscle groups compared to the open approach. This may be due to the greater reach of laparoscopic instruments and camera in the lower abdomen/pelvis. Patient body habitus may also have less of an effect in the laparoscopic compared to open approach. Future studies with multiple subjects and different types of procedures are planned to further investigate these findings.


Similar content being viewed by others
References
Lee J, Mabardy A, Kermani R, Lopez M, Pecquex N, McCluney A (2013) Laparoscopic vs open ventral hernia repair in the era of obesity. JAMA Surg 148:723–726. doi:10.1001/jamasurg.2013.1395
Lomanto D, Iyer SG, Shabbir A, Cheah W-K (2006) Laparoscopic versus open ventral hernia mesh repair: a prospective study. Surg Endosc Interv Tech 20:1030–1035. doi:10.1007/s00464-005-0554-2
Schauer PR, Ikramuddin S, McLaughlin RH, Graham TO, Slivka A, Lee KK, Schraut WH, Luketich JD (1998) Comparison of laparoscopic versus open repair of paraesophageal hernia. Am J Surg 176:659–665
Schauer PR, Ikramuddin S (2001) Laparoscopic surgery for morbid obesity. Surg Clin North Am 81:1145–1179. doi:10.1016/S0039-6109(05)70189-4
Bennett J, Boddy A, Rhodes M (2007) Choice of approach for appendicectomy: a meta-analysis of open versus laparoscopic appendicectomy. Surg Laparosc Endosc Percutan Tech 17:245–255. doi:10.1097/SLE.0b013e318058a117
Gollan JL, Bulkley GB, Diehl A et al (1993) Gallstones and laparoscopic cholecystectomy. JAMA 269:1018–1024. doi:10.1001/jama.1993.03500080066034
Tanphiphat C, Tanprayoon T, Sangsubhan C, Chatamra K (1998) Laparoscopic vs open inguinal hernia repair. Surg Endosc 12:846–851. doi:10.1007/s004649900727
Lannoo M, Dillemans B (2014) Laparoscopy for primary and secondary bariatric procedures. Best Pract Res Clin Gastroenterol 28:159–173. doi:10.1016/j.bpg.2013.11.013
Rashid AM, Nazir SM, Kakroo SMM, Chalkoo MAM, Razvi SAM, Wani AAM (2013) Laparoscopic interval appendectomy versus open interval appendectomy: a prospective randomized controlled trial. Surg Laparosc Endosc Percutaneous Tech Febr 23:93–96. doi:10.1097/SLE.0b013e318277df6a
Veldkamp R, Kuhry E, Hop WCJ, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM, COlon cancer Laparoscopic or Open Resection Study Group (COLOR) (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484. doi:10.1016/S1470-2045(05)70221-7
Berguer R, Forkey DL, Smith WD (1999) Ergonomic problems associated with laparoscopic surgery. Surg Endosc 13:466–468. doi:10.1007/PL00009635
Berguer R, Rab GT, Abu-Ghaida H, Alarcon A, Chung J (1997) A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg Endosc 11:139–142
Hignett S, Carayon P, Buckle P, Catchpole K (2013) State of science: human factors and ergonomics in healthcare. Ergonomics 56:1491–1503. doi:10.1080/00140139.2013.822932
Berguer R, Chen J, Smith WD (2003) A comparison of the physical effort required for laparoscopic and open surgical techniques. Arch Surg 138:967–970. doi:10.1001/archsurg.138.9.967
Berguer R, Smith WD, Chung YH (2001) Performing laparoscopic surgery is significantly more stressful for the surgeon than open surgery. Surg Endosc 15:1204–1207. doi:10.1007/s004640080030
Franasiak J, Ko EM, Kidd J, Secord AA, Bell M, Boggess JF, Gehrig PA (2012) Physical strain and urgent need for ergonomic training among gynecologic oncologists who perform minimally invasive surgery. Gynecol Oncol 126:437–442. doi:10.1016/j.ygyno.2012.05.016
Miller K, Benden M, Pickens A, Shipp E, Zheng Q (2012) Ergonomics principles associated with laparoscopic surgeon injury/illness. Hum Fact J Hum Fact Ergon Soc 54:1087–1092. doi:10.1177/0018720812451046
Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D (2010) Patients Benefit While Surgeons Suffer: an Impending Epidemic. J Am Coll Surg 210:306–313. doi:10.1016/j.jamcollsurg.2009.10.017
Berguer R (1999) Surgery and ergonomics. Arch Surg 134:1011–1016. doi:10.1001/archsurg.134.9.1011
Zihni AM, Ohu I, Cavallo JA, Ousley J, Cho S, Awad MM (2014) FLS tasks can be used as an ergonomic discriminator between laparoscopic and robotic surgery. Surg Endosc 28:2459–2465. doi:10.1007/s00464-014-3497-7
Lee G, Lee T, Dexter D, Klein R, Park A (2007) Methodological infrastructure in surgical ergonomics: a review of tasks, models, and measurement systems. Surg Innov 14(3):153–167
Lee GI, Lee MR, Clanton T, Sutton E, Park AE, Marohn MR (2014) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28(2):456–465. doi:10.1007/s00464-013-3213-z Epub 2013 Oct 3
Lee G, Lee T, Dexter D, Godinez C, Meenaghan N, Catania R, Park A (2009) Ergonomic risk associated with assisting in minimally invasive surgery. Surg Endosc 23(1):182–188. doi:10.1007/s00464-008-0141-4
Acknowledgements
This study was supported by a research grant from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES). Dr. Zihni received research grant funding for unrelated studies from the National Institutes of Health. Dr. Awad has received research grant funding from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) and Intuitive, Surgical Inc. (Sunnyvale, CA).
Author contributions
RW, ZL, AMZ, SR, and MMA were involved in study conception and design; Wang, Liang, and Ray were involved in acquisition of data; RW, AMZ, ZL, and SR were involved in analysis and interpretation of data; RW, AMZ, and MMA drafted the manuscript; and RW, ZL, AMZ, SR, and MMA were involved in critical revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Robert Wang, Zhe Liang, Ahmed M. Zihni, Shuddhadeb Ray and Michael M. Awad have no conflicts of interest or financial ties to disclose.
Additional information
Disclaimers This study was supported by research grants from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES).
Rights and permissions
About this article
Cite this article
Wang, R., Liang, Z., Zihni, A.M. et al. Which causes more ergonomic stress: Laparoscopic or open surgery?. Surg Endosc 31, 3286–3290 (2017). https://doi.org/10.1007/s00464-016-5360-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5360-5