Abstract
Background
Visualization, analysis and characterization of the angioarchitecture of a brain arteriovenous malformation (bAVM) present crucial steps for understanding and management of these complex lesions. Three-dimensional (3D) segmentation and 3D visualization of bAVMs play hereby a significant role. We performed a systematic review regarding currently available 3D segmentation and visualization techniques for bAVMs.
Methods
PubMed, Embase and Google Scholar were searched to identify studies reporting 3D segmentation techniques applied to bAVM characterization. Category of input scan, segmentation (automatic, semiautomatic, manual), time needed for segmentation and 3D visualization techniques were noted.
Results
Thirty-three studies were included. Thirteen (39%) used MRI as baseline imaging modality, 9 used DSA (27%), and 7 used CT (21%). Segmentation through automatic algorithms was used in 20 (61%), semiautomatic segmentation in 6 (18%), and manual segmentation in 7 (21%) studies. Median automatic segmentation time was 10 min (IQR 33), semiautomatic 25 min (IQR 73). Manual segmentation time was reported in only one study, with the mean of 5–10 min. Thirty-two (97%) studies used screens to visualize the 3D segmentations outcomes and 1 (3%) study utilized a heads-up display (HUD). Integration with mixed reality was used in 4 studies (12%).
Conclusions
A golden standard for 3D visualization of bAVMs does not exist. This review describes a tendency over time to base segmentation on algorithms trained with machine learning. Unsupervised fuzzy-based algorithms thereby stand out as potential preferred strategy. Continued efforts will be necessary to improve algorithms, integrate complete hemodynamic assessment and find innovative tools for tridimensional visualization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain AVMs (bAVMs) are complex vascular lesions. Tailoring management for each patient is challenging and demands an accurate knowledge and understanding of the angioarchitecture of the malformation. bAVMs represent a relevant cause of secondary intracerebral hemorrhage, with a risk of rupture of approximately 1% yearly that on average increases fivefold after rupture [1,2,3].
Brain bAVMs are composed of feeding arteries and draining veins entangled in a nidus, without an intervening capillary bed [4]. Visualization of these structures is vital in the understanding of the angioarchitecture. Comprehension of flow direction and amount is necessary to grasp the hemodynamic effects. Determination of vessel positions in relationship to the nidus and brain structures is fundamental to optimize treatment strategies. The best imaging tools for the characterization of bAVMs are digital subtraction angiography (DSA) and magnetic resonance angiography (MRA)[5]. Both imaging modalities play a role in the diagnostic and perioperative management of these lesions, highlighting bAVMs’ features that drive their therapeutic management [6,7,8]. In neurosurgery, based on clinical and imaging findings, the severity of bAVMs, their predicted risk of rupture and necessity for intervention are mostly rated according to the classical Spetzler–Martin classification and its supplementation provided by Lawton et al. in 2010, demonstrating a stronger correlation with surgical outcomes [9,10,11].
Visualization of feeding arteries, nidus and venous drainage system is vital in the understanding of bAVM angioarchitecture and related hemodynamics: to tailor a therapeutic strategy, it is important to determine vessel positions and flow directions and to distinguish them depending on their nature and role. An accurate understanding of the angioarchitecture of bAVMs can be achieved by segmentation [3, 12,13,14,15,16]. Segmentation is intended as manual delineation of structures on a Digital Imaging and Communications in Medicine (DICOM) series to create its 3D shape. With segmentation, size and shape of cerebral structures can be measured to determine their spatial characterization and to plan a precise therapeutic intervention [16, 17]. Modern visualization techniques such as augmented reality (AR), 3D screens, as well as mixed reality (MR) and virtual reality (VR) have also been implemented to show segmentation results [18,19,20,21,22].
Several publications have reviewed vessel extraction techniques [15, 23,24,25]. They have helped to classify segmentation and visualization strategies and show the diversity and limitations of the used methods. Nonetheless, a major lack in the current literature is the presence of a gold standard technique shared by multiple centers worldwide to address segmentation of bAVMs, as well as the integration of hemodynamic information to characterize not only the morphology, but also the physiology of these complex lesions. The aim of this systematic review is to provide an up-to-date collection of on 3D methods to study the angioarchitecture of bAVMs for pretreatment planning and during embolization, surgery or radiosurgical treatment, as well as their integration to hemodynamic information and augmented reality rendering.
Materials and methods
A systematic review was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [26]. Two reviewers (EC and TF) screened records independently, and disagreements at any stage were resolved by discussion and consensus. Two additional records were identified through reference search. Studies were excluded when considered beyond the scope for the aims of the present analysis, and/or when their outcomes were not of interest. The critical appraisal of the included studies was performed by means of risk of bias score as shown in Table 1.
Search strategy
The PubMed, Embase and Google Scholar databases were searched to identify eligible papers. The query was performed using the Boolean operators “AND” or “OR” and database-related filters to maximize the chance to identify articles focusing on segmentation strategies and their 3D visualization specific of bAVMs. The string ((‘cerebral arteriovenous malformations’) AND (‘brain arteriovenous malformations’) AND segmentation OR ‘tridimensional visualization’ OR ‘3D’ OR ‘skeletonization methods’ OR ‘augmented reality’) was entered. The most recent search was performed on February 18, 2022.
Selection criteria
Articles were included if all the following criteria were met. 1) Studies published after 1997; 2) studies analyzing specifically the angioarchitecture of brain arteriovenous malformations; 3) a 3D segmentation technique on top of source data as a mean to study angioarchitecture; 4) English, Italian, French or German language; 5) studies integrating the segmentation outcome with augmented reality technology.
Data extraction
The following information was extracted from all included publications: (1) study group and year of publication; (2) segmentation methods and their outcomes (volume model, surface model); (3) segmentation technique (purely manual strategies, semiautomatic techniques or automatic segmentations based on mathematical algorithms); (4) imaging data source (CT, MRI or DSA); (5) treatment modality; (6) duration of the segmentation; (7) blood flow incorporation; (8) 3D visualization methods (screens, virtual reality, mixed reality or augmented reality).
Statistical analysis
The descriptive statistical analyses were performed using IBM SPSS Statistics 25. Data were presented as numbers and percentages, and medians with IQR. Heterogeneity was tested by Chi-square test (significance level: p-value < 0.01).
Results
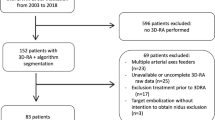
A PRISMA flowchart is displayed in Fig. 1. A total of 7212 publications were screened, 37 full-text articles were assessed for eligibility and 32 studies were included in this review.
Segmentation input (Table 1)
Thirteen out of 33 studies (39%) described high-resolution magnetic resonance imaging (MRI)-based segmentation [20, 27,28,29,30,31,32,33,34,35,36,37,38]. Within this group, tridimensional time of flight-MR-Angiography (TOF-MRA) was used in 11 studies (85%): 9 studies applied a protocol without gadolinium and 2 studies with gadolinium (28, 31). Nine studies (27%) described digital subtraction angiography (DSA)-based segmentations [39,40,41,42,43,44,45,46,47], and 7 (21%) described native CT and CT-Angiography (CTA)-based segmentations [25, 48,49,50,51,52,53] (Table 1).
Segmentation aim (Table 1)
Thirteen out the 33 studies (39%) aimed to render feeding arteries, the architecture of the nidus and draining veins [25, 28,29,30, 34, 37, 38, 43, 45, 47, 48, 50, 51]. Seven studies (21%) provided an analysis of feeders and veins, without specific focus on the nidus [18, 27, 31, 33, 49, 52, 54]. The exclusive focus on the nidus was documented in four studies (12%) [20, 21, 36, 54]. Information on the aim of the segmentation is provided in Table 1. Thirty studies (91%) implemented a segmentation strategy to achieve preoperative characterization of bAVMs; however, three studies (9%) segmented with the purpose to visualize on a navigation-linked intraoperative display [38, 55, 56].
Manual and semiautomatic segmentation (Table 2)
Seven studies (21%) described manual bAVM segmentation [21, 34, 35, 38, 39, 48, 55], and 6 studies (18%) described semiautomatic algorithms [27, 40, 43, 54] In this subgroup, 3 studies (23%) aimed for delineation of all the bAVM components [34, 38, 48], while the other 10 studies (77%) focused on the segmentation on a single component of the bAVM or on the volume of the lesion. Four semiautomatic segmentation studies documented a median duration of 25 (IQR 73) minutes [27, 43, 51, 54].
Automatic segmentation (Table 2)
Twenty studies (61%) used an automatic mathematical algorithm to segment bAVMs [20, 25, 28,29,30,31,32,33, 36, 37, 42, 44,45,46,47, 49, 51,52,53, 56]. Eight of these studies (40%) aimed to segment all three bAVM components [25, 28,29,30, 37, 45, 47, 51]. Median segmentation time was 10 min (IQR 33), described in 6 out of the 20 studies. Eight automatic segmentation studies (40%) performed segmentation by an unsupervised fuzzy-based method, with a median processing time of 10 min (IQR 33) [20, 28,29,30,31,32, 36]. Only 1 research group further provided a hemodynamic characterization of the segmented bAVM components. Hemodynamics were provided by integrating temporal blood flow information of the vessels in proximity of the nidus [32, 33].
Other groups included in this cohort performed an automatic image segmentation based on supervised methods [37, 49, 53]. These strategies included supervised principal component analysis [49], supervised 3D V-Net with a compound loss function [53] and supervised convolutional neural network [37].
The most utilized imaging input in the automatic segmentation subgroup was MRI (10/20, 50%).
Segmentation variability
A Chi-square test of homogeneity was performed to examine the methodological variability of the collected studies. The homogeneity between the segmentation strategies and the reported outcomes, namely segmentation of all bAVM components, segmentation of the nidus only or other outcomes (e.g., volume), was not significant, with a Chi-squared = 0.13 (p-value 0.99).
3D visualization
Four studies (12%) described an integration of their segmentation strategies with mixed reality for intraoperative guidance under the microscope [37, 47, 55, 56]. While integration with AR was positively endorsed, the future necessity to integrate hemodynamic considerations to the AR rendering to provide more useful and precise intraoperative information was also suggested [18]. None of the included studies aimed to a rendering of the segmentation outcomes with VR.
Clinical value and blood flow analysis
In 19 studies (58%), the final goal of segmentation was an accurate and more precise planning and intraoperative management of bAVM [25, 27,28,29,30,31,32,33, 35, 38, 43, 45, 48, 50,51,52, 54,55,56]. Eleven studies (33%) aimed to a better delineation of bAVM components to achieve a more effective and safer radiosurgical treatment [20, 21, 34, 36, 37, 39,40,41,42, 49, 53]. Three (9%) of the included studies set embolization as the final goal of segmentation and better angioarchitecture visualization [44, 46, 47].Only one research group aimed and achieved the inclusion of hemodynamic considerations to 3D bAVM visualization. They could provide temporal information on blood flow of the vessels in the close proximity of the nidus by calculating a time-to-peak parameter map and registering it to TOF-MRA sequences [32, 33].
Discussion
The present study represents a systematic analysis on segmentation techniques of bAVMs for 3D visualization and accurate angioarchitectural study. This systematic review focusses on 3D bAVM segmentation and visualization strategies, which have been published from 1997 to 2022 on the characterization of the angioarchitecture of bAVMs. Although most studies use MRI as input and a tendency was shown in the direction of automatic machine learning trained algorithms, this review shows how significantly variable the possible methods of segmenting a bAVM are, and with this the absence of a gold standard.
Due to methodological variety of manual, semiautomatic and automatic segmentation techniques and their outcomes, the results should be interpreted with caution. Intrinsic biases of included publications cannot be ruled out. The average segmentation duration was evaluated using very limited data from only a few studies. Because of the great variability of the data collected in the present systematic review, a descriptive statistical analysis was performed. Given the technical and preclinical nature of most of the included studies, very few of them documented sensitivity and specificity of the segmentation method. Therefore, the scarcity of statistical data made the performance of a pooled analysis impossible.
This review describes a tendency over time to base bAVM segmentation on algorithms trained with machine learning, especially deep learning, because manual segmentations are prone to human error and interindividual assessment and are labor intensive [28]. Algorithms trained with machine learning stem from two principles: supervised and unsupervised learning. Supervised learning algorithms, such as support vector machine, have the disadvantage of relying on manual segmentations. In addition, the variability of scans should be large, because algorithms trained on scans from 1 center are rarely easily extrapolated. Unsupervised learning does not require initial information, and algorithms based on this technology are generally fast. In the present analysis, fully automated segmentation via unsupervised learning has good results using fuzzy-based methods. This approach is based on the computation of vesselness filter and maximum parameter images on MRI-TOF sequences, providing a highly precise delineation of large as well as fine vessels [32, 36].
The deep-learning algorithm developed by Forkert et al. describes the extra advantage of producing surface models of the vascular system, which can be not only visualized but also manipulated in 3D [28, 32]. In the settings of 3D segmentation, operability of surface models differentiates them from outcomes of computational heavier volumetric models, that in general are more detailed and look sharper than surface models but do not allow any interaction and are mostly too heavy to visualize in a head-up display without streaming [57]. In view of extensive integration of medical imaging with mixed reality or virtual reality in the future, the use of surface models versus volume models as a possible output of algorithms in highly complex 3D lesions as bAVMs should be further investigated.
In a medical world moving toward personalized medicine, segmentation strategies and 3D imaging visualization techniques are increasingly gaining popularity. Pre- and intraoperative delineation of complex anatomical entities like bAVMs with these technologies provides important clinical advances [58]. First is a more precise understanding of bAVM angioarchitecture and anatomical relationships with the surrounding structures [37, 38]. Therefore, a more accurate and individualized therapy planning and the possibility to achieve more efficient patient management and potentially better clinical outcomes [56]. Only one research group incorporated flow in 3D bAVM segmentation. However, flow is extremely important in assessing brain AVM (re-)rupture risk analysis [59]. Transcranial Doppler (TD), DSA and quantitative MR-Angiography (QMRA) [60, 61] have been described as useful techniques to analyze flow in bAVM [22, 62,63,64]. The integration of these techniques in 3D bAVM segmentation should be a future goal.
Conclusion
A golden standard for 3D visualization of bAVMs does not exist. This review describes a tendency over time to base segmentation on algorithms trained with machine learning. Unsupervised fuzzy-based algorithms thereby stand out as potential preferred strategy. Continued efforts will be necessary to further improve algorithms, integrate complete hemodynamic assessment and find new innovative tools for tridimensional visualization.
References
Lawton MT, Rutledge WC, Kim H et al (2015) Brain arteriovenous malformations. Nat Rev Dis Primers 1:15008. https://doi.org/10.1038/nrdp.2015.8
Mohr JP, Parides MK, Stapf C et al (2014) Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet 383(9917):614–621. https://doi.org/10.1016/S0140-6736(13)62302-8
Chen C-J, Ding D, Derdeyn CP et al (2020) Brain arteriovenous malformations: A review of natural history, pathobiology, and interventions. Neurology 95(20):917–927. https://doi.org/10.1212/WNL.0000000000010968
Yasargil MG (1987) AVM of the brain, history, embryology, pathological considerations, hemodynamics, diagnostic studies, diagnostic studies, microsurgical anatomy, Microneurosurgery, 4 Vols, Vol.3A. 1st ed. Thieme
Raman A, Uprety M, Calero MJ et al (2022) A systematic review comparing digital subtraction angiogram with magnetic resonance angiogram studies in demonstrating the angioarchitecture of cerebral arteriovenous malformations. Cureus 14(6):e25803. https://doi.org/10.7759/cureus.25803
Cenzato M, Boccardi E, Beghi E et al (2017) European consensus conference on unruptured brain AVMs treatment (Supported by EANS, ESMINT, EGKS, and SINCH). Acta Neurochir (Wien) 159(6):1059–1064. https://doi.org/10.1007/s00701-017-3154-8
Kato Y, Dong VH, Chaddad F et al (2019) Expert consensus on the management of brain arteriovenous malformations. Asian J Neurosurg 14(4):1074–1081. https://doi.org/10.4103/ajns.AJNS_234_19
De Leacy R, Ansari SA, Schirmer CM et al (2022) Endovascular treatment in the multimodality management of brain arteriovenous malformations: report of the Society of NeuroInterventional Surgery Standards and Guidelines Committee. J Neurointerv Surgneurintsurg-2021-018632. https://doi.org/10.1136/neurintsurg-2021-018632
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg. 65(4):476–483. https://doi.org/10.3171/jns.1986.65.4.0476
Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL (2010) A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery 66(4):702–713. https://doi.org/10.1227/01.NEU.0000367555.16733.E1
Hafez A, Koroknay-Pál P, Oulasvirta E et al (2019) The application of the novel grading scale (Lawton-Young grading system) to predict the outcome of brain arteriovenous malformation. Neurosurgery 84(2):529–536. https://doi.org/10.1093/neuros/nyy153
Li H, Yezzi A (2007) Vessels as 4-D curves: global minimal 4-D paths to extract 3-D tubular surfaces and centerlines. IEEE Trans Med Imaging 26(9):1213–1223. https://doi.org/10.1109/tmi.2007.903696
Lorigo LM, Faugeras OD, Grimson WE et al (2001) CURVES: curve evolution for vessel segmentation. Med Image Anal 5(3):195–206. https://doi.org/10.1016/s1361-8415(01)00040-8
Yan P, Kassim AA (2005) MRA image segmentation with capillary active contour. Med Image Comput Comput Assist Interv 8(Pt 1):51–58. https://doi.org/10.1007/11566465_7
Qian X, Brennan MP, Dione DP et al (2009) A non-parametric vessel detection method for complex vascular structures. Med Image Anal 13(1):49–61. https://doi.org/10.1016/j.media.2008.05.005
Kirbas C, Quek F (2004) A review of vessel extraction techniques and algorithms. ACM Comput Surv 36(2):81–121. https://doi.org/10.1145/1031120.1031121
Yushkevich PA, Piven J, Hazlett HC et al (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31(3):1116–1128. https://doi.org/10.1016/j.neuroimage.2006.01.015
Cabrilo I, Bijlenga P, Schaller K (2014) Augmented reality in the surgery of cerebral aneurysms: a technical report. Neurosurgery. 10(Suppl 2):252–260. https://doi.org/10.1227/NEU.0000000000000328
Kersten-Oertel M, Chen SSJ, Drouin S, Sinclair DS, Collins DL (2012) Augmented reality visualization for guidance in neurovascular surgery. Stud Health Technol Inform 173:225–229. https://doi.org/10.3233/978-1-61499-022-2-225
Lee K-Y, Han SW, Kim SH et al (2007) Early recanalization after intravenous administration of recombinant tissue plasminogen activator as assessed by pre- and post-thrombolytic angiography in acute ischemic stroke patients. Stroke 38(1):192–193. https://doi.org/10.1161/01.STR.0000251788.03914.00
Zhang X-Q, Shirato H, Aoyama H et al (2003) Clinical significance of 3D reconstruction of arteriovenous malformation using digital subtraction angiography and its modification with CT information in stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 57(5):1392–1399. https://doi.org/10.1016/s0360-3016(03)00780-6
Alaraj A, Luciano CJ, Bailey DP et al (2015) Virtual reality cerebral aneurysm clipping simulation with real-time haptic feedback. Neurosurgery. 11(Suppl 2):52–58. https://doi.org/10.1227/NEU.0000000000000583
Lesage D, Angelini ED, Bloch I, Funka-Lea G (2009) A review of 3D vessel lumen segmentation techniques: models, features and extraction schemes. Med Image Anal 13(6):819–845. https://doi.org/10.1016/j.media.2009.07.011
Yaniv Z, Cleary K (2006) Image guided procedures: a review computer aided interventions and medical robotics. Technical Report
Babin D, Pižurica A, De Vylder J, Vansteenkiste E, Philips W (2013) Brain blood vessel segmentation using line-shaped profiles. Phys Med Biol 58(22):8041–8061. https://doi.org/10.1088/0031-9155/58/22/8041
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ339:b2535. https://doi.org/10.1136/bmj.b2535
Bullitt E, Aylward S, Bernard EJ, Gerig G (2001) Computer-assisted visualization of arteriovenous malformations on the home personal computer. Neurosurgery. 48(3):576–582. https://doi.org/10.1097/00006123-200103000-00024
Forkert ND, Säring D, Fiehler J, Illies T, Handels H (2009) AnToNIa: A software tool for the hemodynamic analysis of cerebral vascular malformations using 3D and 4D MRA image sequences. Informatik. pp 1249–1256
Forkert ND, Säring D, Wenzel K, et al (2009) Automatische segmentierung der zerebralen Gefäße aus 3D-TOF-MRA-bildsequenzen mittels Fuzzy-Methoden. Informatik. pp 46–51. https://doi.org/10.1007/978-3-540-93860-6_10
Forkert ND, Säring D, Wenzel K, Illies T, Fiehler J, Handels H (2009) Fuzzy-based extraction of vascular structures from time-of-flight MR images. Stud Health Technol Inform 150:816–820 (PMID: 19745426)
Forkert ND, Säring D, Handels H (2010) Automatic analysis of the anatomy of arteriovenous malformations using 3D and 4D MRA image sequences. Stud Health Technol Inform 160(Pt 2):1268–1272 (PMID: 20841888)
Forkert ND, Fiehler J, Illies T, Möller DPF, Handels H, Säring D (2012) 4D blood flow visualization fusing 3D and 4D MRA image sequences. J Magn Reson Imaging 36(2):443–453. https://doi.org/10.1002/jmri.23652
Forkert ND, Illies T, Goebell E, Fiehler J, Säring D, Handels H (2013) Computer-aided nidus segmentation and angiographic characterization of arteriovenous malformations. Int J Comput Assist Radiol Surg 8(5):775–786. https://doi.org/10.1007/s11548-013-0823-9
Di Ieva A, Boukadoum M, Lahmiri S, Cusimano MD (2015) Computational analyses of arteriovenous malformations in neuroimaging. J Neuroimaging 25(3):354–360. https://doi.org/10.1111/jon.12200
Phellan R, Forkert ND (2017) Comparison of vessel enhancement algorithms applied to time-of-flight MRA images for cerebrovascular segmentation. Med Phys 44(11):5901–5915. https://doi.org/10.1002/mp.12560
Peng S-J, Lee C-C, Wu H-M et al (2019) Fully automated tissue segmentation of the prescription isodose region delineated through the Gamma knife plan for cerebral arteriovenous malformation (AVM) using fuzzy C-means (FCM) clustering. Neuroimage Clin 21:101608. https://doi.org/10.1016/j.nicl.2018.11.018
Simon AB, Hurt B, Karunamuni R et al (2022) Automated segmentation of multiparametric magnetic resonance images for cerebral AVM radiosurgery planning: a deep learning approach. Sci Rep 12(1):786. https://doi.org/10.1038/s41598-021-04466-3
Mandel M, Li Y, Figueiredo EG, Teixeira MJ, Steinberg GK (2022) Presurgical Planning with Open-Source Horos Software for Superficial Brain Arteriovenous Malformations. World Neurosurgery 157:3–12. https://doi.org/10.1016/j.wneu.2021.09.081
Söderman M, Karlsson B, Launnay L, Thuresson B, Ericson K (2000) Volume measurement of cerebral arteriovenous malformations from angiography. Neuroradiology 42(9):697–702. https://doi.org/10.1007/s002340000374
Coste E, Gibon D, Leclercq X, Verdonck B, Vasseur C, Rousseau J (2001) 3D reconstruction of the encapsulating contour of arteriovenous malformations for radiosurgery using digital subtraction angiography. Int J Radiat Oncol Biol Phys 50(1):247–255. https://doi.org/10.1016/s0360-3016(01)01441-9
Berger M-O, Anxionnat R, Kerrien E, Picard L, Söderman M (2008) A methodology for validating a 3D imaging modality for brain AVM delineation: application to 3DRA. Comput Med Imaging Graph 32(7):544–553. https://doi.org/10.1016/j.compmedimag.2008.06.003
Hristov D, Liu L, Adler JR et al (2011) Technique for targeting arteriovenous malformations using frameless image-guided robotic radiosurgery. Int J Radiat Oncol Biol Phys 79(4):1232–1240. https://doi.org/10.1016/j.ijrobp.2010.05.015
Clarençon F, Maizeroi-Eugène F, Bresson D et al (2015) Elaboration of a semi-automated algorithm for brain arteriovenous malformation segmentation: initial results. Eur Radiol 25(2):436–443. https://doi.org/10.1007/s00330-014-3421-5
Li Null Fan, Tankyevych O, Chenoune Y, Blanc R, Petit E (2015) Symbolic representation of brain vascular network with Arteriovenous Malformations from 3DRA images. Annu Int Conf IEEE Eng Med Biol Soc. 2015:662–665. https://doi.org/10.1109/EMBC.2015.7318449
Li F, Chenoune Y, Ouenniche M, Blanc R, Petit E (2014) Segmentation and reconstruction of cerebral vessels from 3D rotational angiography for AVM embolization planning. Annu Int Conf IEEE Eng Med Biol Soc 2014:5522–5525. https://doi.org/10.1109/EMBC.2014.6944877
Babin D, Pižurica A, Velicki L et al (2018) Skeletonization method for vessel delineation of arteriovenous malformation. Comput Biol Med 93:93–105. https://doi.org/10.1016/j.compbiomed.2017.12.011
Chenoune Y, Tankyevych O, Li F, Piotin M, Blanc R, Petit E (2019) Three-dimensional segmentation and symbolic representation of cerebral vessels on 3DRA images of arteriovenous malformations. Comput Biol Med 115:103489. https://doi.org/10.1016/j.compbiomed.2019.103489
Muacevic A, Steiger HJ (1999) Computer-assisted resection of cerebral arteriovenous malformations. Neurosurgery. 45(5):1164–1170. https://doi.org/10.1097/00006123-199911000-00030
Nyui Y, Ogawa K, Kunieda E, Kawaguchi O (2003) Visualization of intracranial arteriovenous malformation using multivariate analysis. Nippon Igaku Hoshasen Gakkai Zasshi 63(6):322–328
Coenen VA, Dammert S, Reinges MHT, Mull M, Gilsbach JM, Rohde V (2005) Image-guided microneurosurgical management of small cerebral arteriovenous malformations: the value of navigated computed tomographic angiography. Neuroradiology 47(1):66–72. https://doi.org/10.1007/s00234-004-1307-y
Babin D, Pižurica A, Bellens R et al (2012) Generalized pixel profiling and comparative segmentation with application to arteriovenous malformation segmentation. Med Image Anal 16(5):991–1002. https://doi.org/10.1016/j.media.2012.02.006
Babin D, Vansteenkiste E, Pizurica A, Philips W (2011) Segmentation of brain blood vessels using projections in 3-D CT angiography images. Annu Int Conf IEEE Eng Med Biol Soc 2011:8475–8478. https://doi.org/10.1109/IEMBS.2011.6092091
Wang T, Lei Y, Tian S et al (2019) Learning-based automatic segmentation of arteriovenous malformations on contrast CT images in brain stereotactic radiosurgery. Med Phys 46(7):3133–3141. https://doi.org/10.1002/mp.13560
Bullitt E, Aylward S (2002) Patient-specific vascular models for endovascular and open operative procedures. Int Congr Ser 1247:129–138. https://doi.org/10.1016/S0531-5131(02)01084-1
Mascitelli JR, Schlachter L, Chartrain AG et al (2018) Navigation-linked heads-up display in intracranial surgery: early experience. Oper Neurosurg (Hagerstown) 15(2):184–193. https://doi.org/10.1093/ons/opx205
Cabrilo I, Bijlenga P, Schaller K (2014) Augmented reality in the surgery of cerebral arteriovenous malformations: technique assessment and considerations. Acta Neurochir (Wien) 156(9):1769–1774. https://doi.org/10.1007/s00701-014-2183-9
Shah A, Abrámoff MD, Wu X (2019) Optimal surface segmentation with convex priors in irregularly sampled space. Med Image Anal 54:63–75. https://doi.org/10.1016/j.media.2019.02.004
Zhang C, Gao H, Liu Z, Huang H (2021) The potential value of mixed reality in neurosurgery. J Craniofacial Surg 32(3):940–943. https://doi.org/10.1097/SCS.0000000000007317
Hernesniemi JA, Dashti R, Juvela S, Väärt K, Niemelä M, Laakso A (2008) Natural history of brain arteriovenous malformations: a long-term follow-up study of risk of hemorrhage in 238 patients. Neurosurgery 63(5):823–831. https://doi.org/10.1227/01.NEU.0000330401.82582.5E
Shakur SF, Amin-Hanjani S, Mostafa H, Charbel FT, Alaraj A (2015) Hemodynamic characteristics of cerebral arteriovenous malformation feeder vessels with and without aneurysms. Stroke 46(7):1997–1999. https://doi.org/10.1161/STROKEAHA.115.009545
Shakur SF, Brunozzi D, Hussein AE et al (2018) Validation of cerebral arteriovenous malformation hemodynamics assessed by DSA using quantitative magnetic resonance angiography: preliminary study. J Neurointerv Surg 10(2):156–161. https://doi.org/10.1136/neurintsurg-2017-012991
Lindegaard KF, Grolimund P, Aaslid R, Nornes H (1986) Evaluation of cerebral AVM’s using transcranial Doppler ultrasound. J Neurosurg 65(3):335–344. https://doi.org/10.3171/jns.1986.65.3.0335
Kaspera W, Ładziński P, Larysz P et al (2014) Transcranial color-coded Doppler assessment of cerebral arteriovenous malformation hemodynamics in patients treated surgically or with staged embolization. Clin Neurol Neurosurg 116:46–53. https://doi.org/10.1016/j.clineuro.2013.11.001
Ansari SA, Schnell S, Carroll T et al (2013) Intracranial 4D flow MRI: toward individualized assessment of arteriovenous malformation hemodynamics and treatment-induced changes. AJNR Am J Neuroradiol 34(10):1922–1928. https://doi.org/10.3174/ajnr.A3537
Funding
Open access funding provided by University of Zurich. This work is part of “SURGENT” under the auspices of University Medicine Zurich/Hochschulmedizin Zürich.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tristan van Doormaal is Co-founder and CMO of Augmedit bv, an augmented reality company.
Ethical approval
Ethical approval will not be required because this study will retrieve and synthesize data from already published studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Colombo, E., Fick, T., Esposito, G. et al. Segmentation techniques of brain arteriovenous malformations for 3D visualization: a systematic review. Radiol med 127, 1333–1341 (2022). https://doi.org/10.1007/s11547-022-01567-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01567-5