Abstract
Background and Objective
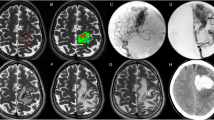
A compact nidus is a well-known feature of good outcome after treatment in brain arteriovenous malformations (bAVM). This item, included in the “Supplementary AVM grading system” by Lawton, is subjectively evaluated on DSA. The present study aimed to assess whether quantitative nidus compacity along with other angio-architectural bAVM features were predictive of angiographic cure or the occurrence of procedure-related complications.
Materials and Methods
Retrospective analysis of 83 patients prospectively collected data base between 2003 to 2018 having underwent digital subtraction 3D rotation angiography (3D-RA) for pre-therapeutic assessment of bAVM. Angio-architectural features were analyzed. Nidus compacity was measured with a dedicated segmentation tool. Univariate and multivariate analyses were performed to test the association between these factors and complete obliteration or complication.
Results
Compacity was the only significant factor associated with complete obliteration in our predictive model using logistic multivariate regression; the area under the curve for compacity predicting complete obliteration was excellent (0.82; 95% CI 0.71–0.90; p < 0.0001). The threshold value maximizing the Youden index was a compacity > 23% (sensitivity 97%; specificity 52%; 95% CI 85.1–99.9; p = 0.055). No angio-architectural factor was associated with the occurrence of a complication.
Conclusion
Nidus high compacity quantitatively measured on 3D-RA, using a dedicated segmentation tool is predictive of bAVM cure. Further investigation and prospective studies are warranted to confirm these preliminary results.


Similar content being viewed by others
Abbreviations
- 3D-RA:
-
3D Rotational angiography
- ADC:
-
Apparent diffusion coefficient
- AUC:
-
Area under the curve
- bAVM:
-
Brain arterio-venous malformation
- DSA:
-
Digital subtraction angiography
- EVOH:
-
Ethylene vinyl alcohol
- ICH:
-
Intra-cerebral hemorrhage
- ICP:
-
Intra-cranial pressure
- mRS:
-
Modified Rankin scale
- n‑BCA:
-
n‑butyl cyanoacrylate
- ROC:
-
Receiver operating characteristics
- SM:
-
Spetzler-Martin
- SRS:
-
Stereotaxic radiosurgery
References
Kim H, Su H, Weinsheimer S, Pawlikowska L, Young WL. Brain arteriovenous malformation pathogenesis: a response-to-injury paradigm. Acta Neurochir Suppl. 2011;111:83–92.
Shotar E, Debarre M, Sourour NA, Di Maria F, Gabrieli J, Nouet A, Chiras J, Degos V, Clarençon F. Retrospective study of long-term outcome after brain arteriovenous malformation rupture: the RAP score. J Neurosurg. 2018;128(1):78–85.
Imbesi SG, Knox K, Kerber CW. Reproducibility analysis of a new objective method for measuring arteriovenous malformation nidus size at angiography. AJNR Am J Neuroradiol. 2002;23(3):412–5.
Anxionnat R, Bracard S, Macho J, Da Costa E, Vaillant R, Launay L, Trousset Y, Romeas R, Picard L. 3D angiography. Clinical interest. First applications in interventional neuroradiology. J Neuroradiol. 1998;25(4):251–62.
Combaz X, Levrier O, Moritz J, Mancini J, Regis JM, Bartoli JM, Girard N. Three-dimensional rotational angiography in the assessment of the angioarchitecture of brain arteriovenous malformations. J Neuroradiol. 2011;38(3):167–74.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8.
Joint Writing Group of the Technology Assessment Committee American Society of Interventional and Therapeutic Neuroradiology; Joint Section on Cerebrovascular Neurosurgery a Section of the American Association of Neurological Surgeons and Congress of Neurological Surgeons; Section of Stroke and the Section of Interventional Neurology of the American Academy of Neurology, Atkinson RP, Awad IA, Batjer HH, Dowd CF, Furlan A, Giannotta SL, Gomez CR, Gress D, Hademenos G, Halbach V, Hemphill JC, Higashida RT, Hopkins LN, Horowitz MB, Johnston SC, Lawton MW, McDermott MW, Malek AM, Mohr JP, Qureshi AI, Riina H, Smith WS, Pile-Spellman J, Spetzler RF, Tomsick TA, Young WL. Reporting terminology for brain arteriovenous malformation clinical and radiographic features for use in clinical trials. Stroke. 2001;32(6):1430–42.
Clarençon F, Maizeroi-Eugène F, Bresson D, Maingreaud F, Sourour N, Couquet C, Ayoub D, Chiras J, Yardin C, Mounayer C. Elaboration of a semi-automated algorithm for brain arteriovenous malformation segmentation: initial results. Eur Radiol. 2015;25(2):436–43.
Potts MB, Zumofen DW, Raz E, Nelson PK, Riina HA. Curing arteriovenous malformations using embolization. Neurosurg Focus. 2014;37(3):E19.
Starke RM, Komotar RJ, Otten ML, Hahn DK, Fischer LE, Hwang BY, Garrett MC, Sciacca RR, Sisti MB, Solomon RA, Lavine SD, Connolly ES, Meyers PM. Adjuvant embolization with N‑butyl cyanoacrylate in the treatment of cerebral arteriovenous malformations: outcomes, complications, and predictors of neurologic deficits. Stroke. 2009;40(8):2783–90.
Sandoval-Garcia C, Yang P, Schubert T, Schafer S, Hetzel S, Ahmed A, Strother C. Comparison of the diagnostic utility of 4D-DSA with conventional 2D- and 3D-DSA in the diagnosis of cerebrovascular abnormalities. AJNR Am J Neuroradiol. 2017;38(4):729–34.
Conti A, Pontoriero A, Faragò G, Midili F, Siragusa C, Granata F, Pitrone A, De Renzis C, Longo M, Tomasello F. Integration of three-dimensional rotational angiography in radiosurgical treatment planning of cerebral arteriovenous malformations. Int J Radiat Oncol Biol Phys. 2011;81(3):e29–37.
Anderson JL, Khattab MH, Sherry AD, Luo G, Chitale RV, Froehler MT, Fusco MR, Cmelak AJ, Attia A. Improved cerebral arteriovenous malformation obliteration with 3‑dimensional rotational digital subtraction angiography for radiosurgical planning: a retrospective cohort study. Neurosurgery. 2020;88(1):122–30.
Buis DR, Lagerwaard FJ, Barkhof F, Dirven CM, Lycklama GJ, Meijer OW, van den Berg R, Langendijk HA, Slotman BJ, Vandertop WP. Stereotactic radiosurgery for brain AVMs: role of interobserver variation in target definition on digital subtraction angiography. Int J Radiat Oncol Biol Phys. 2005;62(1):246–52.
Al-Shahi R, Pal N, Lewis SC, Bhattacharya JJ, Sellar RJ, Warlow CP, AVM Observer Agreement Study Group. Observer agreement in the angiographic assessment of arteriovenous malformations of the brain. Stroke. 2002;33(6):1501–8.
Lawton MT, Kim H, McCulloch CE, Mikhak B, Young WL. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery. 2010;66(4):702–13. discussion 713.
Jin H, Lenck S, Krings T, Agid R, Fang Y, Li Y, Kostynskyy A, Tymianski M, Pereira VM, Radovanovic I. Interval angioarchitectural evolution of brain arteriovenous malformations following rupture. J Neurosurg. 2018;131(1):96–103.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N.-A. Sourour is consultant for Medtronic, Balt Extrusion, Microvention, Stock/Stock Options: Medina. F. Clarençon reports conflict of interest with Medtronic, Guerbet, Balt Extrusion, Penumbra (payment for readings; non-related to the study), Codman Neurovascular and Microvention (core lab; non-related to the study). A. Pacini, E. Shotar, B. Granger, F. Maizeroi-Eugène, M. Delaitre, A. Talbi, A.-L. Boch, C.-A. Valéry, K. Premat, M. Drir, S. Lenck and C. Mounayer report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. The manuscript is not supported by industry.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pacini, A., Shotar, E., Granger, B. et al. Nidus Compacity Determined by Semi-Automated Segmentation is a Strong Quantitative Predictor of Brain Arterio-Venous Malformation Cure. Clin Neuroradiol 33, 1095–1104 (2023). https://doi.org/10.1007/s00062-023-01313-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-023-01313-y