Abstract
Purpose
The purpose of this study was to determine if objectively measured adherence to oral appliance (OA) treatment may affect dental changes and temporomandibular disorders (TMD) in patients with obstructive sleep apnea (OSA).
Methods
The original study group consisted of adults with OSA who were referred for OA therapy. Eight indicators of subjective side effects of using OA (temporomandibular joint (TMJ) and muscle pain, pain in teeth, jaw stiffness in the morning, clicking, dry mouth, hypersalivation, gingival irritation) were evaluated by a questionnaire. Three occlusal indicators (overjet, overbite, molar occlusion) and clinical TMD signs (TMJ pain, muscle pain, clicking, jaw deviation on opening) were evaluated at baseline and at the 3-, 6-, and 12-month follow-up. In addition, objective adherence monitoring for OA was registered. Statistical analyses included the chi-square test, Fisher’s exact test, paired sample t-test, and linear regression analyses.
Results
A total of 58 adults with OSA were referred for OA therapy. Mean (SD) age was 50.7 (11.7) and mean apnea-hypopnea index (AHI) was 19.5 (10.0). At 1-year follow-up, the study group consisted of 28 men and 12 women. Overjet but not overbite reduced significantly after 1-year OA therapy. The average nightly wear of OA was related to overjet and overbite reduction, and to TMD signs. Hypersalivation, dry mouth, and tooth discomfort were the most common subjective side effects of OA therapy.
Conclusion
There was a time-dependent relationship with the nightly wear of OA and reduction in overjet and overbite, and clinical TMD signs. With 60% of mandibular advancement, dental changes and TM-disorders were considered mild/minor in the 1‐year study period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral appliances (OA) for obstructive sleep apnea (OSA) are effective alternatives to continuous positive airway pressure (CPAP) therapy, especially for those who do not tolerate nor want to use CPAP [1, 2]. Considering the chronic nature of OSA, the use of an oral appliance is likely to be a lifelong treatment. Earlier studies have found that OAs have both short-term and long-term side effects such as dental/occlusal changes and signs and symptoms of temporomandibular disorders (TMD) [1,2,3,4,5]. It is suggested that the more one wears an OA, the more detrimental are the side-effects [6, 7]. Dental changes are visible early during the first year of OA use [8], and they are usually progressive with ongoing OA therapy [9]. Although dental changes do not usually disturb the subject, they are irreversible and thus may be clinically relevant [7]. Earlier review articles have found the following orofacial and dental changes with long-term OA use: retroclination of maxillary incisors, proclination of mandibular incisors, reduction in overjet (OJ) and overbite (OB), mandibular downward rotation, and increase in the lower facial height [10, 11]. Short-term temporomandibular disorders (TMD) during acclimatization to OA therapy are common, but they are usually temporary and disappear during the first few months of treatment [2, 4]. However, TM disorders may also be unchanged in long-term follow-up [12]. Altogether, moderate/severe side effects have a profound effect on adherence to OA therapy [13], and in addition to ineffectiveness of OA in decreasing OSA signs and symptoms, they are the major reasons for discontinuation of OA therapy [14]. The highest percentage of interruptions in OA use is likely to occur during the first year of appliance use [14].
The risk of side effects increases by augmentating the degree of protrusion of the mandible [15]. Therefore a moderate mandibular advancement is highly recommended. Regarding treatment outcomes among patients with OSA, our earlier results showed that more than half of patients attained a complete response (AHI < 5 events/h) to OA therapy. The prevalence of snoring also decreased significantly, and the upper airway space improved remarkably with 60% of mandibular advancement using the oral device [16]. The aim of this study was to determine if there were less subjective symptoms and TMD signs, as well as minor dental side effects with this treatment protocol. Another focus of this study was to determine if the objectively measured adherence to oral appliance therapy was related to the risk of dental and temporomandibular side effects.
Subjects and methods
Subjects
This prospective study included consecutive patients diagnosed to have OSA by ambulatory polygraphic recording and who were referred for oral appliance therapy to the Oral and Maxillofacial Department, Kuopio University Hospital. Subjects were enrolled if they were 18 years or older, their AHI was at least ten events/h, their body mass index (BMI) was less than 35 kg/m2, and they had at least five teeth/jaw. The subjects were examined at baseline and 3, 6, and 12 months after OA therapy. The Research Ethics Committee of the Hospital District of Northern Savo in Kuopio, Finland, approved the study protocol on February 7, 2017 (80/2017). All patients supplied a written informed consent before participating in the study. The original study flowchart is elsewhere [16].
Methods
Nocturnal single-night ambulatory polygraphic recordings were conducted at home to diagnose OSA prior to this study and after 3 months with the oral appliance (OA) in situ. Apneas and hypopneas were automatically scored (Remlogic, version 3.2, and Somnologica, version 3.2 software, Embla Co., Broomfield, CO, USA) and manually verified and edited. Trained physicians evaluated the recordings. The present part of the study included the following data:
Descriptive data: age (years), gender, follow-up time of OA therapy (3, 6, and 12 months), mandibular protrusion with OA (mm), average nightly use of OA (hours) and regular use of OA (use of OA at least 4 h/night on at least 70% of all nights).
Clinical examination: Occlusal findings were assessed intraorally according to the modified method of Björk [17] including molar occlusion (anteroposterior upper and lower first molar relationship), overjet (OJ, the horizontal distance between the upper and lower front teeth), and overbite (OB, the vertical overlap between the upper and lower front teeth). Also, the number of missing teeth was recorded. Signs and symptoms of TMD and jaw movements were evaluated by the modified method of Helkimo [18] including palpatory tenderness of the masticatory muscles and the temporomandibular joints (TMJs), clicking, jaw deviation on maximal opening, and mandibular mobility (Table 1). The original study protocol did not include cephalometric measurements. The trained orthodontist (RP) examined all the patients.
Questionnaire of the treatment-related side effects (dichotomous scale): Pain in TMJ and in masticatory muscles, clicking, and jaw stiffness in the morning were assessed by the modified method of Helkimo [18]. In addition, patients were inquired (yes/no) about discomfort in teeth, gingival irritation, hypersalivation, and dry mouth (Table 2). The patients got the questionnaires at each follow-up visit, and they were asked to complete the questionnaires and return them by mail.
Mandibular advancement device therapy: Patients used SomnoDent Flex (SomnoMed Ltd, Sydney, Australia) custom-made acrylic duo block titratable oral device with a temperature-sensitive micro-recorder (DentiTrackR, Braebon, Ontario, Canada) to measure the objective adherence during OA therapy at 3, 6, and 12 months of follow-up. The recorder registers the wearing time of the device, and by using the base station, the data is uploaded into the Health Insurance Portability and Accountability Act of 1996 (HIPAA)-secure cloud. For each patient, the average OA wear in hours per night and in percentage of nights per week was recorded and was referred to as the objective mean wearing time. In the statistical analyses, frequent users were the ones whose objective wear of OA was at least 4 h/night over 70% of all the nights. In SomnoDent Flex, the adjustable interlocking acrylic buccal extensions connect the upper and lower splints. In this study, advancement of the mandible with OAs was determined as 60% of the voluntary maximal retrusion to maximal protrusion of the mandible. Advancement was assessed by SOMGauge bite registration device. In SomnoDent Flex, there is a screw mechanism to advance the jaw if any titration of the device is needed. No routine mandibular jaw exercises to cope with side effects were given to the patients.
Statistical analysis
For statistical analyses, the IBM SPSS statistics, version 22.0 (IBM Corp., Armonk, NY, USA) was used. The chi-square test was used to analyze the differences in categorical variables between males and females. Fisher’s exact test was used when the numbers of subjects in some cells were small. The differences in continuous variables were analyzed using paired samples t-test for normally distributed variables. Multivariate linear regression analysis was used to investigate the associations of age, gender, average nightly wear of OA, and mandibular protrusion with OA with a reduction of OJ and OB during 1 year of OA treatment. In addition, multivariate linear regression models were used to evaluate the associations between the sum of temporomandibular dysfunction signs (muscle tenderness, clicking, TMJ tenderness, deviation on opening) and those independent variables at the 3-month, 6-month, and 12-month follow-up. The independent variables were added simultaneously in regression analyses, and their choices except for age and gender were based on the outcomes in bivariate analyses. Associations with p values of < 0.05 were statistically significant.
Results
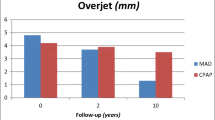
There were 28 men (mean age [SD] 49.2 [12.6]) and 12 women (mean age [SD] 58.3 [5.4]) who attended the 12-month follow-up. The results showed that during 1-year study interval OJ and OB reduced 0.36 mm and 0.25 mm, respectively (Table 3). Only in OJ, the reduction was statistically significant. Concerning molar occlusion, only four men and four women had occlusal changes after 1‐year of OA treatment (Table 4). The mean number of missing teeth per patient was 2.1, the range varying from 0 to 13 per subject. Multivariate linear regression analyses showed that the risk of OJ and OB reduction increased with nightly treatment time (Table 5). Furthermore, OJ reduction was positively related to female gender. The age- and gender-adjusted regression models explained 39% of the variation of OJ reduction and 37% of the variation of OB reduction. In the other multivariate regression analyses, the average nightly wear of OA was replaced by the frequent use of OA, but in this analysis, no significant associations were found.
Almost half of the patients had TMD symptoms and discomfort of using OA during the first week of OA therapy (Fig. 1a and b). Hypersalivation, dry mouth, and pain in teeth were the most common side effects reported by the patients. After the first visit at 3-month follow-up, the frequency of most symptoms almost halved except in clicking, which showed to be a persistent TM disorder. Pain in TMJ and in muscles, clicking, and dry mouth were significantly more common among females than in males, especially at 3-month follow-up. Concerning the clinical TMD signs (Table 6), the frequency of muscle pain temporarily tripled within 3 months after starting OA therapy compared to the baseline, while in TMJ pain and in clicking, the number of patients with those signs remained about the same during the study. In the linear regression analyses, predictive factors for clinical TMD signs were younger age at 3-month follow-up, female gender, and larger mandibular advancement with OAs at 6-month follow-up and greater nightly OA adherence at 12-month follow-up (Table 7). The age- and gender-adjusted regression models explained 21% of TMD at the 3-month, 30% of TMD at the 6-month, and 38% of TMD at 12-month follow-up. In bivariate analyses, there was a moderate correlation between overjet and overbite reduction and average nightly use of OA (r = 0.4 and r = 0.5, respectively). At 6-month follow-up, clicking correlated positively (r = 0.39) to the frequent use of OA, hypersalivation correlated also positively (r = 0.63) to the average nightly use of OA, but muscle pain correlated negatively (r = − 0.60 and r = − 0.40) to frequent and nightly use of OA. At 12-month follow-up, there was a negative correlation between gingival irritation and frequent and nightly use of OA (r = − 0.52 and r = − 0.59).
a Percentage of subjects who reported pain in TMJs (A), pain in muscles (B), and clicking (C) during OA therapy. The proportion of women n (%), and a significant difference in the prevalence between men and women (*) are announced in bar charts. b Percentage of subjects who reported pain in teeth (A), jaw stiffness (B), dry mouth (C), hypersalivation (D), and gingival irritation (E) during OA therapy. The proportion of women n (%) and a significant difference in the prevalence between men and women (*) are announced in bar charts
Discussion
This is the first study to evaluate if changes in occlusion in patients with OSA are related to objective adherence to OA use. Earlier review studies have found that the most reported OA side effects are dental, the risk of developing new TMD signs and symptoms with OA therapy is low, and pre-existing signs and symptoms of TMD do not seem to exacerbate with OA use [10, 19]. The OAs with 60% of mandibular advancement used in our study had a favorable effect on mild-to-moderate OSA [16], and there seemed to be only a minor effect on occlusion after 1‐year of OA therapy. The present study showed that reductions in OJ and OB, as well as clinical TMD, are significantly associated with a greater nightly adherence to OA but not with the frequent use of OA. To assess the wear time of OAs for clinical optimal treatment outcome without detrimental dental changes or exacerbation of TM-disorders in the future, objective measures of OA adherence together with investigating personal dental features influencing dental changes are needed.
Effect of OA adherence on side effects
In OA therapy, there is no consensus describing adequate adherence. Based on self-reports, patients with OSA usually wear OAs at least 5 h a day and at least 4 days per week [11]. Although currently debated for CPAP-therapy, the treatment threshold of less than 4 h a day on less than 5 days a week is defined as non-adherence [20]. Our previous results showed that the objective wear time of OA (percentage use, mean (SD)) during the 1-year follow-up was 64% (37) [21]. The wear time of OA (hours/night, mean (SD)) in women was 6.2 (2.6) h, and among men 7.6 (1.1) h. The parameter that was positively related to higher objective adherence was more pronounced disturbance of snoring, while in mandibular retrusion, bruxism, and daily smoking, the relationship was negative. Surprisingly, excessive daytime sleepiness, side effects, or patients’ sociodemographic parameters were not associated with OA adherence [21].
The most common dental changes related to the use of OAs are the reduction in OJ and OB. When a subject wears an OA with dental arch coverage, the mandible tends to return to its natural position, which applies palatal force to maxillary incisors and labial force to mandibular incisors. Thus, dental changes are due to altered inclination of the incisors rather than skeletal changes or mandibular rotation [6]. This OA mechanism of action on the dentition is like that of functional orthodontic appliance used in growing subjects with Class II malocclusion. To achieve occlusal change, the target wearing time for the device is 12–14 h a day, and for minor dental effect, the wear of any device is 4 to 6 h per day [22]. As Cohen-Levy and co-workers found, a small force of 1.18 N per millimeter of advancement in OAs can induce dental movements [23]. Our earlier results showed that in the present sample, the objective nightly adherence of OA increased from 6.7 h at 3-month follow-up to 7.1 h at a 1-year study interval [21], which exceed the treatment duration threshold for dental changes. Earlier studies agree that there are progressive dental changes with prolonged OAs use [1, 6, 7]. The present results are parallel to earlier reports that especially the risk of OJ reduction is associated with OA treatment time but disagree the finding that dental changes are related to the frequent use of OA [1, 24]. This disagreement may be due to the finding that in this study, only half of the patients were frequent OA users after 12 months of therapy [21].
Like in other studies [2, 4] in the present report, the frequency of short-term TM disorders during acclimatization to OA therapy was high. In our study, the most common symptoms were hypersalivation and pain in teeth, which prevalence halved by the 3-month study interval; meanwhile, the prevalence of clicking and dry mouth remained almost unchanged during the 1-year study period. Interestingly, there was a clear difference in the prevalence of subjective and clinical TMJ pain, which most likely reflects difficulties in patients to differ TMJ pain from muscle pain. In the present report, subjects were not inquired about the subjective TMD symptoms at the baseline, but the initial signs of TMD were clinically evaluated. Despite a temporary increase in the frequency of muscle pain after OA therapy, the risk of developing new TMD signs with the use of OA proved to be low. Nevertheless, the results showed that the better the nightly adherence the higher the risk for clinical TMD signs. More specifically, a study on TM disorders in OSA patients suggests that TM dysfunction following OA wearing is related to altered muscle dynamics rather than changes due to increased stress in the temporomandibular joint itself [25]. Since early adherence to OSA treatment is a strong predictor of long-term adherence [26], an early check-up for identification and resolution of problems using OA is important.
To summarize, adherence to OA therapy is of utmost importance to ensure successful treatment for OSA. Generally, subjects who are less adherent are less susceptible to dental changes, but if the wear of OA is minor, OSA symptoms are likely to continue. At present, it is impossible to assess the target wearing time of OA to ensure the success of OA therapy and to avoid side effects.
Effect of mandibular advancement on side effects
Earlier studies disagree of the proportional improvement of apnea–hypopnea index (AHI) by an increase of mandibular advancement [15, 27]. Our earlier results showed that AHI normalized in 51% of the patients with moderate mandibular advancement (60%), indicating effective treatment. The risk of OJ [22, 28], and OB reduction [5] is associated with the amount of mandibular advancement in the device, and side effects appear with over 50% of mandibular protrusion [15]. The present results showed that with 60% of mandibular advancement, OJ reduced about 0.4 mm in 1‐year study period, and the reduction in OB was even less (0.25 mm). In the earlier studies, the mean reductions of OJ and OB after 6 months of OA therapy was 0.87 mm and 0.61 mm [8], while the reductions in OJ and OB after several years of OA therapy varied from 0.7 to 1.22 mm and from 0.60 to 1.25 mm, respectively [6]. Regarding dental changes by OA therapy, also the number of occlusal contacts in (pre)molar region is likely to reduce, and the molar/cuspid occlusion tends to shift towards a more mesial occlusion [5]. In the present sample, the molar occlusion changed in only eight subjects, partly due to molar extraction, and in the regression analyses, mandibular protrusion with OA was not related to dental changes. To conclude, the present results show that by using SomnoDent Flex device with 60% of mandibular advancement, dental side effects are minor in 1‐year study period.
Device design may also influence the risk of occlusal changes. A flexible device without incisor coverage is likely to increase the irregularity of the lower incisors compared with a rigid OA with incisor coverage [29]. Marklund recommends a soft elastomeric device with a small vertical opening of the mandible to prevent large reductions in OJ and OB [1]. In the present study, all the patients used the SomnoDent Flex device, which is an acrylic device with soft inner liner, which is comfortable to teeth. This device allows free jaw opening but no lateral movements, a quality that appeals patients who are likely to be distressed of fixed appliances (i.e., monoblocks), but may be inconvenient for patients with bruxism. Regarding the degree of mandibular vertical opening in OAs, it has been found that larger (14 mm) incisal opening increases patients´ inconvenience and decreases device acceptance compared to 4 mm incisal opening [30]. In SomnoDent Flex, the vertical incisal opening is about 4 mm. Initially, all the patients had 60% of mandibular advancement of the OAs. After the second ambulatory polygraphic recodings with OAs in situ (after 3-month follow-up), the advancement was increased 1 mm in four patients and 2 mm in one patient, but no new TM disorders developed in these patients after the titration. As recently concluded, there is not one superior custom-made OA design in OSA treatment regarding AHI reduction, improvement in daytime sleepiness, adherence, patient preference, or side effects [31]. However, custom-made OA designs proved to be superior to thermoplastic OA designs because of higher rates of objective improvement and cure of OSA [32] and higher hours per night adherence [33].
Regarding signs and symptoms of TM disorders, the earlier Finnish study [12] showed that the subject’s TMD symptoms remained unchanged during 2-year follow-up with the mandibular advancement of 50% of maximum (mean protrusion was 5.4 mm). The present results are in line with those findings since the prevalence of subjective symptoms remained almost unchanged between 6- and 12-month follow-up with the mandibular advancement of 60% (mean protrusion was 5.8 mm). At 6-month follow-up, the larger mandibular protrusion increased the risk of clinical TMD signs.
Effects of gender and age on side effects
The linear regression model showed that the risk of OJ reduction with OA treatment increased in women, which refers to significantly (p = 0.041) larger baseline OJ in women (3.5 mm) compared to that of men (2.5 mm). Although dental changes during OA therapy are more likely among elderly people due to age changes in their periodontal health [28], in the present study, age was not a risk factor of dental changes. In adult population, the prevalence of orofacial pain varies from 10 to 15% being twice as high in women compared to men [34, 35]. Gender difference in TMD prevalence may be due to genetic factors affecting pain vulnerability as well as hormonal and psychosocial determinants [35]. Since female patients tend to have more often TM disorders, they are also more prone to interrupt OA treatment than males [36]. In the present study at 3-month check-up, women had more often TMJ pain, muscle pain, and clicking than men, and in the linear regression analysis, they were more likely to have clinical TMD signs. During this study, four patients dropped out because of TM disorders; three of them were women. In our original study group, the age range varied from 26 to 73 years. The present finding that younger age (model 1) predisposes to TMD signs is parallel to the finding of Häggman-Henrikson and co-workers [35] that TM disorders are most prevalent among 35‐ to 50-year-olds.
Effects of dentofacial features on side effects
The extent of dental movements with OA therapy is somehow related to the dentofacial features [1, 3, 9]. Marklund [1] found that patients with favorable occlusal bites are likely to develop OJ reduction with OA use. Therefore, she recommends for patients with normal occlusion a soft elastomeric device with an advancement less than 6 mm and low-to-moderate vertical displacement to diminish the risks of dental side effects. The present finding of larger baseline OJ in women increases the risk of OJ reduction partly agrees with the finding of Marklund, but in this study, the correlation between baseline OB and OJ/OB reduction was weak. Furthermore, it is suggested that in patients with fewer teeth and reduced periodontal health, dental changes are larger [9, 22], but in bivariate analyses of this study, the correlations between OJ and OB reduction and the number of missing teeth were weak (r = − 0.06 and r = − 0.07, respectively). The evaluation of the periodontal health was not included in the present study protocol.
Conclusion
The present results showed that although OJ reduced significantly during the study period, the dental changes were minor with SomnoDent Flex device set at 60% of mandibular advancement. Further, OJ and OB reductions and clinical TMD signs were associated with a greater nightly adherence to OA therapy but not with the frequent use of OAs. To assess the wear time of OAs for clinical optimal treatment outcome without detrimental dental changes or exacerbation of TM disorders in the future, objective measures of OA adherence together with investigating personal dental features influencing dental changes are needed.
Limitations of the study
This study has limitations. The power analyses of the original study showed that in the main outcomes (AHI reduction at least 50% and OA adherence at least 60%), with standard parameters of 80% power and α 0.05, 31 patients were needed. Considering the expected dropouts, the required sample size was estimated to be 40 patients. Concerning patients with available adherence data, attrition was larger than expected; therefore, the sample is small for this part of the study. Thus, the risk of bias of the results could not be eliminated. The follow-up time was short to conduct an investigation of the long-term dental side effects in patients using OAs. Unfortunately, not all the patients returned the questionnaires regarding subjective symptoms of TMD.
Data availability
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data are not available.
References
Marklund M (2006) Predictors of long-term orthodontic side effects from mandibular advancement devices in patients with snoring and obstructive sleep apnea. Am J Orthod Dentofacial Orthop 129:214–221. https://doi.org/10.1016/j.ajodo.2005.10.004
Sutherland K, Vsanderveken OM, Tsuda H et al (2014) Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med 10:215–227. https://doi.org/10.5664/jcsm.3460
Chen H, Lowe AA, de Almeida FR et al (2008) Three-dimensional computer-assisted study model analysis of long-term oral-appliance wear. Part 2. Side effects of oral appliances in obstructive sleep apnea patients. Am J Orthod Dentofacial Orthop 134:408–417. https://doi.org/10.1016/j.ajodo.2006.10.031
Doff MH, Veldhuis SK, Hoekema A et al (2012) Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on temporomandibular side effects. Clin Oral Investig 16(3):689–697. https://doi.org/10.1007/s00784-011-0555-6
Doff MH, Finnema KJ, Hoekema A et al (2013) Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on dental side effects. Clin Oral Investig 17:475–482. https://doi.org/10.1007/s00784-012-0737-x
Araie T, Okuno K, Ono Minagi H, Sakai T (2018) Dental and skeletal changes associated with long-term oral appliance use for obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev 41:161–172. https://doi.org/10.1016/j.smrv.2018.02.006
Bartolucci ML, Bortolotti F, Martina S et al (2019) Dental and skeletal long-term side effects of mandibular advancement devices in obstructive sleep apnea patients: a systematic review with meta-regression analysis. Eur J Orthod 41:89–100. https://doi.org/10.1093/ejo/cjy036
Robertson C, Herbison P, Harkness M (2003) Dental and occlusal changes during mandibular advancement splint therapy in sleep disordered patients. Eur J Orthod 25:371–376. https://doi.org/10.1093/ejo/25.4.371
Uniken Venema JAM, Doff MHJ, Joffe-Sokolova DS et al (2020) Dental side effects of long-term obstructive sleep apnea therapy: a 10-year follow-up study. Clin Oral Investig 24:3069–3076. https://doi.org/10.1007/s00784-019-03175-6
Martins OFM, Chaves Junior CM, Rossi RRP et al (2018) Side effects of mandibular advancement splints for the treatment of snoring and obstructive sleep apnea: a systematic review. Dental Press J Orthod 23:45–54. https://doi.org/10.1590/2177-6709.23.4.045-054.oar
Tsolakis IA, Palomo JM, Matthaios S, Tsolakis AI (2022) Dental and skeletal side effects of oral appliances used for the treatment of obstructive sleep apnea and snoring in adult patients-a systematic review and meta-analysis. J Pers Med 12(3):483. https://doi.org/10.3390/jpm12030483
Näpänkangas R, Raunio A, Sipilä K, Raustia A (2012) Effect of mandibular advancement device therapy on the signs and symptoms of temporomandibular disorders. J Oral Maxillofac Res 3:e1–e8. https://doi.org/10.5037/jomr.2012.3405
Mullane S, Loke W (2019) Influence of short-term side effects on oral sleep appliance compliance among CPAP-intolerant patients: An objective monitoring of compliance. J Oral Rehabil 46:715–722. https://doi.org/10.1111/joor.12802
Saglam-Aydinatay B, Taner T (2018) Oral appliance therapy in obstructive sleep apnea: Long-term adherence and patients experiences. Med Oral Patol Oral Cir Bucal 23:e72–e77. https://doi.org/10.4317/medoral.22158
Aarab G, Lobbezoo F, Hamburger HL, Naeije M (2010) Effects of an oral appliance with different mandibular protrusion positions at a constant vertical dimension on obstructive sleep apnea. Clin Oral Investig 14:339–345. https://doi.org/10.1007/s00784-009-0298-9
Pahkala R, Seppä J, Myllykangas R et al (2020) The impact of oral appliance therapy with moderate mandibular advancement on obstructive sleep apnea and upper airway volume. Sleep Breath 24:865–873. https://doi.org/10.1007/s11325-019-01914-3
Björk A, Krebs B, Solow B (1964) A method for epidemiological registration of malocclusion. Acta Odontol Scand 22:27–41
Helkimo M (1974) Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state. Sven Tandlak Tidskr 67:101–121
Alessandri-Bonetti A, Bortolotti F, Moreno-Hay I et al (2019) Effects of mandibular advancement device for obstructive sleep apnea on temporomandibular disorders: a systematic review and meta-analysis. Sleep Med Rev 48:101211. https://doi.org/10.1016/j.smrv.2019.101211
Kribbs NB, Pack AI, Kline LR et al (1993) Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir 147:887–895
Pahkala R, Suominen AL (2021) Adherence to oral appliance treatment and its determinants in obstructive sleep apnoea patients. Eur J Orthod 43:408–414. https://doi.org/10.1093/ejo/cjaa084
Proffit WR (2001) Contemporary Orthodontics. Mosby, St. Louis, MO
Cohen-Levy J, Pételle B, Pinguet J et al (2013) Forces created by mandibular advancement devices in OSAS patients: a pilot study during sleep. Sleep Breath 17:781–789. https://doi.org/10.1007/s11325-012-0765-4
Minagi HO, Okuno K, Nohara K, Sakai T (2018) Predictors of side effects with long-term oral appliance therapy for obstructive sleep apnea. J Clin Sleep Med 14:119–125. https://doi.org/10.5664/jcsm.6896
Heidsieck DSP, Koolstra JH, de Ruiter MHT et al (2018) Biomechanical effects of a mandibular advancement device on the temporomandibular joint. J Craniomaxillofac Surg 46:288–292. https://doi.org/10.1016/j.jcms.2017.11.015
Van Ryswyk E, Anderson CS, Antic NA et al (2019) Predictors of long-term adherence to continuous positive airway pressure in patients with obstructive sleep apnea and cardiovascular disease. SLEEPJ 1–9. https://doi.org/10.1093/sleep/zsz152
Tegelberg A, Walker-Engström ML, Vestling O, Wilhelmsson B (2003) Two different degrees of mandibular advancement with a dental appliance in treatment of patients with mild to moderate obstructive sleep apnea. Acta Odontol Scand 61:356–362. https://doi.org/10.1080/00016350310007130
Marklund M, Franklin KA, Persson M (2001) Orthodontic side-effects of mandibular advancement devices during treatment of snoring and sleep apnoea. Eur J Orthod 23:135–144. https://doi.org/10.1093/ejo/23.2.135
Norrhem N, Nemeczek H, Marklund M (2017) Changes in lower incisor irregularity during treatment with oral sleep apnea appliances. Sleep Breath 21:607–613. https://doi.org/10.1007/s11325-016-1456-3
Pitsis AJ, Darendeliler MA, Gotsopoulos H et al (2002) Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J Respir Crit Care Med 166:860–864. https://doi.org/10.1164/rccm.200204-342OC
Uniken Venema JAM, Rosenmöller BRAM, de Vries N (2021) Mandibular advancement device design: a systematic review on outcomes in obstructive sleep apnea treatment. Sleep Med Rev 60:101557. https://doi.org/10.1016/j.smrv.2021.10155732
Friedman M, Hamilton C, Samuelson CG et al (2012) Compliance and efficacy of titratable thermoplastic versus custom mandibular advancement devices. Otolaryngol Head Neck Surg 147:379–386. https://doi.org/10.1177/0194599812439683
Bortolotti F, Corazza G, Bartolucci ML et al (2022) Dropout and adherence of obstructive sleep apnoea patients to mandibular advancement device therapy: a systematic review of randomised controlled trials with meta-analysis and meta-regression. J Oral Rehabil 49:553–572. https://doi.org/10.1111/joor.13290
Bueno CH, Pereira DD, Pattussi MP et al (2018) Gender differences in temporomandibular disorders in adult populational studies: a systematic review and meta-analysis. J Oral Rehabil 45:720–729. https://doi.org/10.1111/joor.12661
Häggman-Henrikson B, Liv P, Ilgunas A, Visscher CM et al (2020) Increasing gender differences in the prevalence and chronification of orofacial pain in the population. Pain 161:1768–1775. https://doi.org/10.1097/j.pain.0000000000001872
Vecchierini MF, Attali V, Collet JM et al (2019) Sex differences in mandibular repositioning device therapy effectiveness in patients with obstructive sleep apnea syndrome. Sleep Breath 23:837–848. https://doi.org/10.1007/s11325-018-1766-8
Acknowledgements
SomnoMed Ltd placed the components of the DentiTrack System and software at our disposal during the survey.
Funding
Open access funding provided by University of Eastern Finland (including Kuopio University Hospital). This study was supported by the Finnish Dental Society Apollonia (Research Grant 2018 to R.P.) and the North Savo Regional Fund of the Finnish Cultural Foundation (Research Grant 2020 to R.P.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study were in accordance with the international and national ethical standards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study received ethics committee approval on February 7, 2017.
Informed consent
Informed consent was obtained from all the participants included in the study.
Conflict of interest
The author declare no competing interests.
Disclaimer
The funding sources had no role in the study design or in the collection, analysis, or interpretation of the data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pahkala, R. Objectively measured adherence may affect side effects of mandibular advancement therapy in subjects with obstructive sleep apnea. Sleep Breath 28, 813–821 (2024). https://doi.org/10.1007/s11325-023-02959-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02959-1