Abstract
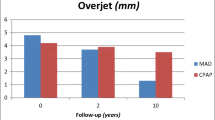
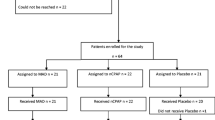
The objective of this study was to assess variations in the occurrence of temporomandibular disorders (TMDs) and the risk of developing pain and function impairment of the temporomandibular complex in obstructive sleep apnea syndrome (OSAS) patients treated with either an oral appliance (mandibular advancement device) or continuous positive airway pressure (CPAP) in a 2-year follow-up study. In addition, we assessed the relationship between the mean mandibular protrusion and the frequency of wearing the appliance during follow-up with the occurrence of pain and function impairment of the temporomandibular complex. Fifty-one patients were randomized to oral appliance therapy and 52 patients to CPAP therapy. TMDs (diagnosed according to the Axis I Research Diagnostic Criteria for TMD), pain intensity and disability and mandibular function impairment were recorded at baseline, after 2 months, 1 year and 2 years of therapy. Only in the initial period of treatment the occurrence of pain-related TMDs was considerably higher (24%) in the oral appliance group compared to CPAP (6%). Oral appliance therapy furthermore resulted in more temporomandibular pain compared to CPAP (odds ratio 2.33, 95% confidence interval (1.22–4.43)). However, there were no limitations in mandibular function in both groups during the (entire) follow-up period. Although generally not serious and of transient nature, oral appliance therapy results in more pain-related TMDs in the initial period of use compared with CPAP therapy. Oral appliance therapy is associated with increased pain in the temporomandibular complex in the initial period of use. Because of the transient nature, this pain is not a reason to contra-indicate an oral appliance in OSAS patients. Moreover, TMDs and the risk of developing pain and function impairment of the temporomandibular complex appear limited with long-term oral appliance use.

Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Malhotra A, White DP (2002) Obstructive sleep apnoea. Lancet 360:237–245
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353:2034–2041
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea–hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ (2006) Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 3:CD001106
Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, Mullins R, Jenkinson C, Stradling JR et al (2002) Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet 359:204–210
Barbe F, Mayoralas LR, Duran J, Masa JF, Maimo A, Montserrat JM et al (2001) Treatment with continuous positive airway pressure is not effective in patients with sleep apnea but no daytime sleepiness. A randomized, controlled trial. Ann Intern Med 134:1015–1023
Lim J, Lasserson TJ, Fleetham J, Wright J (2006) Oral appliances for obstructive sleep apnoea. Cochrane Database Syst Rev 1:CD004435
Marklund M (2006) Predictors of long-term orthodontic side effects from mandibular advancement devices in patients with snoring and obstructive sleep apnea. Am J Orthod Dentofacial Orthop 129:214–221
Fritsch KM, Iseli A, Russi EW, Bloch KE (2001) Side effects of mandibular advancement devices for sleep apnea treatment. Am J Respir Crit Care Med 164:813–818
Ferguson KA, Ono T, Lowe AA, al-Majed S, Love LL, Fleetham JA (1997) A short-term controlled trial of an adjustable oral appliance for the treatment of mild to moderate obstructive sleep apnoea. Thorax 52:362–368
Tegelberg A, Wilhelmsson B, Walker-Engstrom ML, Ringqvist M, Andersson L, Krekmanov L et al (1999) Effects and adverse events of a dental appliance for treatment of obstructive sleep apnoea. Swed Dent J 23:117–126
Walker-Engstrom ML, Ringqvist I, Vestling O, Wilhelmsson B, Tegelberg A (2003) A prospective randomized study comparing two different degrees of mandibular advancement with a dental appliance in treatment of severe obstructive sleep apnea. Sleep Breath 7:119–130
Rose E, Staats R, Virchow C, Jonas IE (2002) A comparative study of two mandibular advancement appliances for the treatment of obstructive sleep apnoea. Eur J Orthod 24:191–198
Almeida FR, Lowe AA, Sung JO, Tsuiki S, Otsuka R (2006) Long-term sequelae of oral appliance therapy in obstructive sleep apnea patients: part 1. Cephalometric analysis. Am J Orthod Dentofacial Orthop 129:195–204
Doff MH, Hoekema A, Pruim GJ, Huddleston Slater JJ, Stegenga B (2010) Long-term oral-appliance therapy in obstructive sleep apnea: a cephalometric study of craniofacial changes. J Dent 38:1010–1018
Fransson AM, Svenson BA, Isacsson G (2002) The effect of posture and a mandibular protruding device on pharyngeal dimensions: a cephalometric study. Sleep Breath 6:55–68
Ringqvist M, Walker-Engstrom ML, Tegelberg A, Ringqvist I (2003) Dental and skeletal changes after 4 years of obstructive sleep apnea treatment with a mandibular advancement device: a prospective, randomized study. Am J Orthod Dentofacial Orthop 124:53–60
de Leeuw R (ed) (2008) Orofacial pain: guidelines for assessment, diagnosis and management. Quintessence, Chicago
Bondemark L, Lindman R (2000) Craniomandibular status and function in patients with habitual snoring and obstructive sleep apnoea after nocturnal treatment with a mandibular advancement splint: a 2-year follow-up. Eur J Orthod 22:53–60
de Almeida FR, Bittencourt LR, de Almeida CI, Tsuiki S, Lowe AA, Tufik S (2002) Effects of mandibular posture on obstructive sleep apnea severity and the temporomandibular joint in patients fitted with an oral appliance. Sleep 25:507–513
Fransson AM, Tegelberg A, Johansson A, Wenneberg B (2004) Influence on the masticatory system in treatment of obstructive sleep apnea and snoring with a mandibular protruding device: a 2-year follow-up. Am J Orthod Dentofacial Orthop 126:687–693
Martinez-Gomis J, Willaert E, Nogues L, Pascual M, Somoza M, Monasterio C (2010) Five years of sleep apnea treatment with a mandibular advancement device. Side effects and technical complications. Angle Orthod 80:30–36
Cunali PA, Almeida FR, Santos CD, Valdrighi NY, Nascimento LS, Dal’Fabbro C et al (2009) Prevalence of temporomandibular disorders in obstructive sleep apnea patients referred for oral appliance therapy. J Orofac Pain 23:339–344
Giannasi LC, Almeida FR, Magini M, Costa MS, de Oliveira CS, de Oliveira JC et al (2009) Systematic assessment of the impact of oral appliance therapy on the temporomandibular joint during treatment of obstructive sleep apnea: long-term evaluation. Sleep Breath 13:375–381
Hoekema A, Stegenga B, Wijkstra PJ, van der Hoeven JH, Meinesz AF, de Bont LG (2008) Obstructive sleep apnea therapy. J Dent Res 87:882–887
AASM (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22:667–689
Dworkin SF, LeResche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 6:301–355
Wiese M, Svensson P, Bakke M, List T, Hintze H, Petersson A et al (2008) Association between temporomandibular joint symptoms, signs, and clinical diagnosis using the RDC/TMD and radiographic findings in temporomandibular joint tomograms. J Orofac Pain 22:239–251
Stegenga B, de Bont LG, de Leeuw R, Boering G (1993) Assessment of mandibular function impairment associated with temporomandibular joint osteoarthrosis and internal derangement. J Orofac Pain 7:183–195
Hoekema A, Stegenga B, van der Aa JG, Meinesz AF, van der Hoeven JH, Wijkstra PJ (2006) Nap-titration: an effective alternative for continuous positive airway pressure titration. Respir Med 100:705–713
Le Bell Y, Niemi PM, Jamsa T, Kylmala M, Alanen P (2006) Subjective reactions to intervention with artificial interferences in subjects with and without a history of temporomandibular disorders. Acta Odontol Scand 64:59–63
Lundh H, Westesson PL, Kopp S, Tillstrom B (1985) Anterior repositioning splint in the treatment of temporomandibular joints with reciprocal clicking: comparison with a flat occlusal splint and an untreated control group. Oral Surg Oral Med Oral Pathol 60:131–136
Al-Ani MZ, Davies SJ, Gray RJ, Sloan P, Glenny AM (2004) Stabilisation splint therapy for temporomandibular pain dysfunction syndrome. Cochrane Database Syst Rev 1:CD002778
Kurita K, Westesson PL, Yuasa H, Toyama M, Machida J, Ogi N (1998) Natural course of untreated symptomatic temporomandibular joint disc displacement without reduction. J Dent Res 77:361–365
Cunali PA, Almeida FR, Santos CD, Valdrichi NY, Nascimento LS, Dal-Fabbro C et al (2010) Mandibular exercises improve mandibular advancement device therapy for obstructive sleep apnea. Sleep Breath (in press)
Kato J, Isono S, Tanaka A, Watanabe T, Araki D, Tanzawa H et al (2000) Dose-dependent effects of mandibular advancement on pharyngeal mechanics and nocturnal oxygenation in patients with sleep-disordered breathing. Chest 117:1065–1072
Bush FM, Harkins SW, Harrington WG, Price DD (1993) Analysis of gender effects on pain perception and symptom presentation in temporomandibular pain. Pain 53:73–80
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Doff, M.H.J., Veldhuis, S.K.B., Hoekema, A. et al. Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on temporomandibular side effects. Clin Oral Invest 16, 689–697 (2012). https://doi.org/10.1007/s00784-011-0555-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-011-0555-6