Abstract
Aim
To elucidate the association of serum irisin levels with bone mineral density (BMD) and calcium–phosphorus metabolism parameters in chronic kidney disease (CKD) patients and renal transplant recipients (RTRs).
Methods
This is a cross-sectional study involving CKD patients and RTRs. Healthy volunteers served as controls. Age, gender, and dialysis vintage were recorded. Serum irisin, creatinine, glucose, calcium, albumin, 25(OH) vitamin D, ferritin, C-reactive protein, A1C, and lipid profile were studied in all participants. Estimated glomerular filtration rate (eGFR), corrected calcium, and body mass index (BMI) were calculated.
Results
Overall, 49 patients (23 hemodialysis, 26 RTRs) and 25 control subjects were included. In hemodialysis (HD) group, 8 patients (34.8%) had osteoporosis, and 12 patients (52.2%) had osteopenia. In RTR group, 3 patients (11.5%) had osteoporosis, while 15 patients (57.7%) had osteopenia. Among controls, one had osteoporosis, and 7 had osteopenia. There was no significant difference between HD and RTRs; however, osteoporosis rate was significantly lower in control subjects. BMD measurements (femur and lumbar T- and Z-scores) were comparable between HD and RTR groups. Control group DEXA values were similar to RTRs; however, they were significantly higher compared to HD group. 25(OH) vitamin D levels were comparable between the HD and RTR groups, and these were significantly lower compared to values of the control group. Mean serum irisin level was 426.6 ± 191.2 pg/mL in hemodialysis group, 342.6 ± 174.8 in the RTR group, and 208.0 ± 186.1 in controls. Serum irisin levels were similar in RTR and HD groups, but their values were significantly higher compared to controls. When we compared serum irisin levels between patients with and without osteoporosis in the whole cohort and hemodialysis and RTR groups, there was no difference. Serum irisin was positively correlated with lumbar T-score both in hemodialysis and RTR groups.
Conclusion
Our study is the first in the literature revealing the positive correlation of serum irisin level with femur T-score in RTRs. Serum irisin level was also positively correlated with femur T-scores in hemodialysis patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Irisin is a member of the family known as myokines which are released from muscle in response to muscle contraction and allow muscle–bone and muscle–fat tissue cross-talk [1]. Irisin is produced by cleavage of the myocyte membrane protein FNDC5 and has a molecular weight between 10 and 32 kDa reported in various studies [2]. Irisin has a wide range of physiologic activities, including converting white fat to brown fat, improvement in insulin resistance and glucose tolerance, increasing nitric oxide release, and vasodilation, among others [3]. Serum irisin levels vary depending on many factors, including, but not limited to, sarcopenia, presence of diabetes mellitus, hypertension and chronic kidney disease, body mass index, and primary hyperparathyroidism [4,5,6,7].
The primary target of irisin is considered to be bone tissue. Osteocytes, osteoblasts and osteoclasts are all affected by irisin in some way. While osteocytes and osteoblasts are directly activated by irisin, osteoclasts interact in a dual way: direct activation by irisin and an indirect inhibition by irisin-induced osteoprotegerin [8, 9]. In the sum of these effects, irisin has been shown in experimental models to promote bone formation, prevent steroid-induced apoptosis, prevent disuse-induced loss of bone and muscle mass, and accelerates fracture healing [5]. Human data also confirmed the beneficial roles of irisin on bones. Several studies have demonstrated that serum irisin levels are positively correlated with bone mineral density in soccer players [10], older people [11], and postmenopausal women [12].
Chronic kidney disease (CKD) has detrimental effects on bones in the forms of osteoporosis, osteomalacia, and renal osteodystrophy [13]. Several studies to date have revealed decreased serum irisin levels in patients with chronic kidney disease [14]. Several factors were put forward to explain the positive correlation between glomerular filtration rate and serum irisin levels, including hyperparathyroidism, insulin resistance, sarcopenia, dialysis adequacy, and uremic toxins [15,16,17]. The association of serum irisin and bone mineral density has been studied poorly in patients with CKD [18]. Renal transplant recipients (RTRs) have a considerable burden of bone disease both related to renal osteodystrophy of the pretransplant dialysis phase and steroid-related osteoporosis of the transplantation phase [19]. As far as we know, no study to date has evaluated irisin and bone mineral density association in RTRs.
Hence, we aimed to elucidate the association of serum irisin levels with bone mineral density and other factors in a mixed cohort of hemodialysis patients and RTRs.
Materials and methods
Patients, design, and setting
This is a cross-sectional study in which we evaluated serum irisin levels along with calcium and phosphorus metabolism parameters and bone mineral density in chronic kidney disease patients and renal transplant recipients (RTRs). We also included age- and sex-matched healthy volunteers as the control group. The study was conducted at the nephrology and transplantation unit of Medicana Hospital, Ankara, Turkey. Patient recruitment lasted from 1 January 2022 to 30 April 2022. Patients were selected among consecutive patients who were evaluated at an outpatient nephrology clinic and willing to participate in the study. Renal transplant recipients who were being followed at the transplantation unit and willing to take part in the study were also included. Subjects in the control group were selected among patients who presented to the check-up outpatient clinic who were not known to have kidney disease or osteoporosis. Patients with one or more of the following characteristics were excluded from the study: receiving osteoporosis treatment with medications such as bisphosphonates, teriparatide, or estrogen, history of lumbar vertebral fracture and/or instrumentation, history of malignancy with bone metastasis, and refusal to participate in the study. The Medicana Hospital's ethics committee approved the study protocol (BŞH.2022/12). Study aims and protocol were explained in detail to all prospective participants of the study, and written informed consent forms were signed by those who consented to participate. This study procedure was carried out in accordance with the Declaration of Helsinki.
Data collection
Age, gender, body height and weight, duration of chronic kidney disease, dialysis vintage, and duration of renal transplantation status were recorded for study participants. Drug uses related to calcium-phosphorus metabolism such as active vitamin D, cholecalciferol and/or phosphate binders were determined for each patient.
Irisin and other biochemical measurements
Fasting blood samples were taken from all study participants (30 min before starting hemodialysis in maintenance dialysis patients) and centrifuged at 3000 g for 10 min. Serum samples were used to make biochemical measurements, including creatinine, glucose, calcium, albumin, 25(OH) vitamin D, ferritin, C-reactive protein, hemoglobin A1C, low-density lipoprotein (LDL), and high-density lipoprotein (HDL) cholesterol, triglycerides by a clinical chemistry analyzer (Abbott ARCHITECT c8000). Complete blood counts were also studied in all participants. Serum intact parathyroid hormone level was measured by enzyme-linked immunosorbent assay (ELISA) (Abbott ARCHITECT i2000SR immunoassay analyzer). A commercial ELISA assay was used to measure serum irisin levels (Elabscience, Texas, US). Detection range is reported by the manufacturer as between 15.63 and 1000 pg/mL. The manufacturer claims that no significant cross-reactivity or interference between Human Irisin and analogs was observed. We found intra- and inter-assay coefficient variation of irisin to be < 10%.
The estimated glomerular filtration rate (eGFR) was calculated by the Modification of Diet in Renal Disease (MDRD) equation [20]. Corrected calcium was calculated by the following formula:
Corrected calcium (mg/dL) = measured total Ca (mg/dL) + 0.8 (4.0 − serum albumin [g/dL]).
Kt/V, URR (urea reduction ratio) and nPCR (Normalized Protein Catabolic Rate) were calculated via online calculators for each hemodialysis patient.
Body mass index (BMI) was calculated by dividing weight in kilograms by height in meters squared. Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) was calculated by the following equation: Score = (Fasting insulin) × (Fasting glucose)/405 [21].
Bone mineral density measurements
All patients and control subjects underwent lumbar and femur neck region bone mineral density measurements by dual-energy X-ray absorptiometry (DEXA) (Hologic QDR Explorer, Bedford, MA, USA). T- and Z-scores were calculated for all measurements. A T-score of -2.5 or below was accepted as osteoporosis. T-scores between -1 and -2.5 was considered osteopenia [22].
Statistical analysis
The Shapiro–Wilks test, histogram, and Q–Q plot were used to evaluate the normality. Normally distributed continuous variables were expressed as mean ± standard deviation, and non-normally distributed variables were specified as median (min–max). Categorical variables were given as numbers and percentages. Chi-square test or Fisher's exact test was used to compare categorical variables between the groups. In numerical variables, to compare two-group comparisons, the independent t-test or the Mann–Whitney U test were used, whereas, for three groups comparison, the one-way analysis of variance (ANOVA) or Kruskal–Wallis test was used. The Spearman correlation and point pairwise correlation test were performed to seek the correlation.
We performed univariate and multivariate linear regression analyses to determine the independent associates of the lumbar T-score. Based on the results of univariate linear regression, among those with a P value less than 0.05 and the variables with clinical significance were included in the multivariate linear regression analysis.
The SPSS 25.0 software package (IBM, Armonk, NY, USA) was used for analysis. A probability value of P < 0.05 was considered statistically significant, and two-tailed P values were used for all statistics.
Results
A total of 49 patients were included in this cross-sectional study. Of these, 23 patients were undergoing maintenance hemodialysis, while 26 patients were renal transplant recipients. Twenty-five healthy participants served as the control group. The median dialysis vintage was 4 years. The median duration since transplantation was 3 years among RTRs. All three groups were matched in terms of age and sex distribution. All hemodialysis patients except one had arteriovenous fistula, one patient had tunneled double lumen dialysis catheter. Table 1 summarizes clinicodemographic features, laboratory parameters and DEXA measurements of the hemodialysis, renal transplant recipient and the control groups.
Parameters of calcium and phosphorus metabolism and bone mineral density
In the hemodialysis group, 8 patients (34.8%) had osteoporosis, and 12 patients (52.2%) had osteopenia. In the RTR group, only 3 patients (11.5%) had osteoporosis, while 15 patients (57.7%) had osteopenia. Among control subjects, one participant (4%) had osteoporosis; whereas, 7 people (28%) had osteopenia. Although numerically, osteoporosis was more common among hemodialysis patients, there was no significant difference between the groups in this regard (P = 0.086). In the control group, only one subject had osteoporosis. Bone mineral density measurements were comparable between the hemodialysis patients and RTRs. All T and Z-scores in femoral and lumbar regions were significantly higher in control subjects compared to hemodialysis patients. There was no significant difference between RTRs and control subjects in this regard (Table 1).
Serum corrected calcium levels were significantly lower in hemodialysis patients compared to RTRs and control subjects, and the median values were similar in the latter two groups. Serum parathormone levels were highest in hemodialysis patients and lowest in control subjects. Median PTH values were significantly different in all three groups. Serum C-reactive protein, alkaline phosphatase, corrected calcium, fasting glucose, albumin, 25(OH) vitamin D, and irisin levels were comparable between the hemodialysis and RTR groups.
Serum irisin levels
The median serum irisin level was 426.6 ± 191.2 pg/mL in the hemodialysis group and 342.6 ± 174.8 ng/mL in the RTR group. There was no difference between the groups in this respect (Table 1). Control subjects had significantly lower serum irisin levels compared to hemodialysis patients and RTRs (Fig. 1). When we compared serum irisin levels between patients with and without osteoporosis in the whole cohort and hemodialysis and RTR groups, there was no difference in any of the comparisons. In all three comparisons, serum irisin levels were comparable between patients with and without osteoporosis (Table 2).
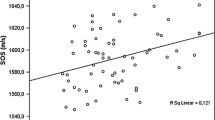
Among hemodialysis patients, serum irisin level showed a moderately strong positive correlation with femur neck T-score (r = 0.421, P = 0.046) and femur neck Z-score (r = 0.476, P = 0.022). İrisin was also significantly and positively correlated with BMI (r = 0.450, P = 0.031). In the RTR group, serum irisin level was significantly correlated with femur neck T-score (r = 0.410, P = 0.037). In the healthy controls group irisin level was not correlated with lumbar T-score (r = 0.224, P = 0.283). Similarly, lumbar T-score and serum irisin level had correlation neither in hemodialysis nor in RTRs groups (r = 0.375, P = 0.078 and r = 0.140, P = 0.497, respectively).
Independent associates of femur T-score
In the RTR group, irisin appeared as a significant associate with femur T-score. However, in the multivariate logistic regression model, only body mass index was an independent and significant associate of femoral T-score (Table 3) Multivariate analysis was not performed in hemodialysis patients since serum irisin did not appear as a significant determiner of femur neck or total T-score.
Discussion
The major findings of the present study were as follows: (1) Serum irisin levels were significantly lower in control subjects compared to hemodialysis patients and RTRs. (2) Although eGFR was significantly lower in hemodialysis patients compared to RTRs, serum irisin levels were comparable between the two groups. (3) Serum irisin level was not different between patients with and without osteoporosis in RTRs and hemodialysis patients. (3) Serum irisin level, similar to previous reports, was positively correlated with femur T-score in hemodialysis patients. (4) For the first time in the literature, our results showed a significant positive correlation between serum irisin level and femur T-score in renal transplant recipients. (5) Serum irisin level was an independent associate of femur T-score neither in hemodialysis nor in the RTR group.
Osteoporosis is a metabolic bone disorder characterized by reduced bone strength and architecture leading to increased fracture risk [23]. Osteoporosis seems like one of the inevitable consequences of advanced kidney disease. Several diverse factors contribute to the development of osteoporosis in patients with CKD, including hypocalcemia, hyperphosphatemia, active vitamin D deficiency, increased parathormone, increased fibroblast growth factor 23, among others [24]. Unfortunately, osteoporosis does not remain silent in CKD patients and, due to fractures, is associated with increased morbidity and mortality [25]. It was reported that between 9.5 and 23% of hemodialysis patients had osteoporosis [26].
The presence of renal osteodystrophy (ROD) complicates the diagnosis of osteoporosis in patients with advanced CKD: bone turnover markers, particularly parathormone, show considerable inconsistencies relative to the underlying bone pathology of the renal osteodystrophy. DEXA also has some shortcomings in patients with advanced CKD. It cannot determine a specific pathologic subtype of ROD and might be affected by increased skeletal and extraskeletal calcification commonly seen in CKD patients [27]. Thus, it is still an ongoing need to find a reliable marker to inform us regarding the presence of osteoporosis in patients with CKD. İrisin, in this respect, might be a candidate marker to detect and evaluate bone mineral abnormalities in CKD patients.
Several studies in the healthy population have shown that irisin is positively correlated with bone mineral density markers and T-scores [10, 11, 28, 29]. A meta-analysis including 1,018 middle-aged and older adults showed that the presence of osteoporosis was associated with lower serum irisin levels. Moreover, postmenopausal women and those with a fracture history had even lower levels of serum irisin. In patients with rheumatoid arthritis, reduced irisin levels could predict vertebral fractures independently [30]. Similar results were replicated in postmenopausal women as well [31]. Considering the major morbidity and mortality, it burdens on the CKD population; the osteoporosis–irisin association has not been adequately studied. Lu and colleagues evaluated serum irisin levels and bone mineral density in 80 maintenance hemodialysis patients [18]. The authors assessed bone density with DEXA at L2–L4 vertebrae. Of all patients, 12.5% had osteoporosis based on lumbar T-scores. T-score was found to be positively correlated with serum irisin level. Our results also confirmed the results of the latter study. Lumbar T-score was positively correlated with serum irisin level.
Several studies conducted in patients with CKD showed that eGFR is associated with serum irisin levels such that as eGFR decreases, serum irisin level decreases as well. Rodríguez-Carmona et al. evaluated 95 dialysis (hemodialysis and peritoneal dialysis) and predialysis patients. The authors found reduced serum irisin levels in CKD patients. However, levels of irisin were higher compared to those receiving hemodialysis or conservatively managed predialysis patients [32]. In a cross-sectional case–control study, Wen and colleagues found that serum irisin levels were lower in stage-5 CKD patients compared to normal subjects. Serum irisin levels showed an inverse correlation with serum creatinine values [33]. Our results did not demonstrate a significant difference in serum irisin levels between hemodialysis patients and RTRs. This result seems surprising, given the mean eGFR values were significantly different between the groups. We predicted that serum irisin levels would be lower in hemodialysis patients who had much lower eGFR values compared to healthy controls and RTRs. Since serum irisin levels are affected by numerous factors, the lack of difference in our results might be attributed to not controlling all relevant factors. However, serum irisin levels in healthy control subjects was significantly lower compared to values observed in hemodialysis patients and RTRs. Our results seem counterintuitive at first sight with regards to the results of the irisin studies published till now. One of the possible explanations might be the relatively small number of subjects in each subgroup of the patients in the present study. Another possible confounder is that serum irisin levels are affected by many variables. Some of these factors are diabetes mellitus, nonalcoholic fatty liver disease, cardiovascular disease and obesity, among others [34]. We could not control all these factors in our study. Another possibility explaining the divergent results is the inherent problems with ELISA assay of irisin. Albrecht and colleagues in their elaborate study examined different antibodies used in commercial irisin ELISA kits and questioned the reliability and validity of serum measurements performed with these kits. Thus, differing irisin kits might be responsible for contradicting results in the literature.
Some clinical studies revealed that serum irisin levels are also significantly and independently related to insulin resistance in patients with advanced kidney disease [15, 35]. In contrast to these studies, our results did not show any association of serum irisin levels with serum glucose or HOMA-IR values.
Renal transplant patients have higher rates of osteoporosis. In a recent study by Yavuz et al., it was shown that the prevalence of osteoporosis was 20% among RTRs. In contrast to the reversal of metabolic abnormalities related to uremia, bone changes usually remain stable and do not improve after renal transplantation [36]. Thus, osteoporosis related fractures are a common cause of morbidity among RTRs [37]. As far as we know, no study in the literature evaluated serum irisin levels in RTRs in the context of osteoporosis. Our results showed a significant and positive correlation between femur T-score and serum irisin level. However, serum irisin levels were not different from those of hemodialysis patients.
Some limitations of the present study deserve mention. First, our sample size was relatively small to reveal subtle differences between the hemodialysis and renal transplant group. Second, we could not determine and control all factors that can potentially affect serum irisin levels, such as underlying cardiovascular disease, sarcopenia, blood pressure, and daily activity level. Hence, these uncontrolled factors might have had an impact on our results.
In conclusion, despite the aforementioned limitations, our study is the first in the literature revealing the positive correlation of serum irisin level with femur T-score in renal transplant recipients. We also confirmed the results of a previous study in that serum irisin level was also positively correlated with femur T-scores in hemodialysis patients. Serum irisin level was found to be increased both in hemodialysis patients and RTRs relative to healthy control subjects. Since a number of factors can potentially affect serum irisin levels, to elucidate its precise role in osteoporosis in patients with CKD and renal transplantation, studies with large sample sizes and taking confounding factors into account are necessary.
Data availability
The data that support the findings of current study are available from the corresponding author, upon reasonable request.
References
Pedersen BK, Akerstrom TC, Nielsen AR, Fischer CP (2007) Role of myokines in exercise and metabolism. J Appl Physiol (1985) 103(3):1093–1098. https://doi.org/10.1152/japplphysiol.00080.2007
Ugur K, Aydin S (2019) What is the actual molecular weight of irisin hormone according to western blot analysis? Biochem Mod Appl 2:40–41
Fu J, Han Y, Wang J, Liu Y, Zheng S, Zhou L, Jose PA, Zeng C (2016) Irisin lowers blood pressure by improvement of endothelial dysfunction via AMPK-Akt-eNOS-NO pathway in the spontaneously hypertensive rat. J Am Heart Assoc. https://doi.org/10.1161/JAHA.116.003433
Fu J, Li F, Tang Y, Cai L, Zeng C, Yang Y, Yang J (2021) The emerging role of irisin in cardiovascular diseases. J Am Heart Assoc 10(20):e022453. https://doi.org/10.1161/JAHA.121.022453
Zerlotin R, Oranger A, Pignataro P, Dicarlo M, Maselli F, Mori G, Colucci SC, Grano M, Colaianni G (2022) Irisin and secondary osteoporosis in humans. Int J Mol Sci. https://doi.org/10.3390/ijms23020690
Zhao M, Zhou X, Yuan C, Li R, Ma Y, Tang X (2020) Association between serum irisin concentrations and sarcopenia in patients with liver cirrhosis: a cross-sectional study. Sci Rep 10(1):16093. https://doi.org/10.1038/s41598-020-73176-z
Wang R, Liu H (2021) Association between serum irisin and diabetic nephropathy in patients with type 2 diabetes mellitus: a meta-analysis. Horm Metab Res 53(5):293–300. https://doi.org/10.1055/a-1475-4444
Colucci S, Colaianni G, Brunetti G, Ferranti F, Mascetti G, Mori G, Grano M (2020) Irisin prevents microgravity-induced impairment of osteoblast differentiation in vitro during the space flight CRS-14 mission. FASEB J 34(8):10096–10106. https://doi.org/10.1096/fj.202000216R
Colaianni G, Mongelli T, Cuscito C, Pignataro P, Lippo L, Spiro G, Notarnicola A, Severi I, Passeri G, Mori G, Brunetti G, Moretti B, Tarantino U, Colucci SC, Reseland JE, Vettor R, Cinti S, Grano M (2017) Irisin prevents and restores bone loss and muscle atrophy in hind-limb suspended mice. Sci Rep 7(1):2811. https://doi.org/10.1038/s41598-017-02557-8
Colaianni G, Notarnicola A, Sanesi L, Brunetti G, Lippo L, Celi M, Moretti L, Pesce V, Vicenti G, Moretti B, Colucci S, Grano M (2017) Irisin levels correlate with bone mineral density in soccer players. J Biol Regul Homeost Agents 31(4 suppl 1):21–28
Zhang J, Huang X, Yu R, Wang Y, Gao C (2020) Circulating irisin is linked to bone mineral density in geriatric Chinese men. Open Med (Wars) 15(1):763–768. https://doi.org/10.1515/med-2020-0215
Badr Roomi A, Nori W, Mokram Hamed R (2021) Lower serum irisin levels are associated with increased osteoporosis and oxidative stress in postmenopausal. Rep Biochem Mol Biol 10(1):13–19. https://doi.org/10.52547/rbmb.10.1.13
Asadipooya K, Abdalbary M, Ahmad Y, Kakani E, Monier-Faugere MC, El-Husseini A (2021) Bone quality in CKD patients: current concepts and future directions - part I. Kidney Dis (Basel) 7(4):268–277. https://doi.org/10.1159/000515534
Gan W, Chen W, Li T, Shao D, Xu F, Huo S, Li C, Yang Z, Zeng X (2022) Circulating irisin level in chronic kidney disease patients: a systematic review and meta-analysis. Int Urol Nephrol 54(6):1295–1302. https://doi.org/10.1007/s11255-021-03000-8
Ebert T, Focke D, Petroff D, Wurst U, Richter J, Bachmann A, Lossner U, Kralisch S, Kratzsch J, Beige J, Bast I, Anders M, Bluher M, Stumvoll M, Fasshauer M (2014) Serum levels of the myokine irisin in relation to metabolic and renal function. Eur J Endocrinol 170(4):501–506. https://doi.org/10.1530/EJE-13-1053
Gouveia MC, Vella JP, Cafeo FR, Affonso Fonseca FL, Bacci MR (2016) Association between irisin and major chronic diseases: a review. Eur Rev Med Pharmacol Sci 20(19):4072–4077
Tan Z, Ye Z, Zhang J, Chen Y, Cheng C, Wang C, Liu X, Lou T, Peng H (2017) Serum irisin levels correlated to peritoneal dialysis adequacy in nondiabetic peritoneal dialysis patients. PLoS One 12(4):e0176137. https://doi.org/10.1371/journal.pone.0176137
Lu CW, Wang CH, Lin YL, Kuo CH, Lai YH, Hsu BG, Tsai JP (2021) Serum irisin level is positively associated with bone mineral density in patients on maintenance hemodialysis. Int J Endocrinol 2021:8890042. https://doi.org/10.1155/2021/8890042
Molinari P, Alfieri CM, Mattinzoli D, Campise M, Cervesato A, Malvica S, Favi E, Messa P, Castellano G (2022) Bone and mineral disorder in renal transplant patients: overview of pathology, clinical, and therapeutic aspects. Front Med (Lausanne) 9:821884. https://doi.org/10.3389/fmed.2022.821884
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, Ckd EPI (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Cacho J, Sevillano J, de Castro J, Herrera E, Ramos MP (2008) Validation of simple indexes to assess insulin sensitivity during pregnancy in Wistar and Sprague-Dawley rats. Am J Physiol Endocrinol Metab 295(5):E1269-1276. https://doi.org/10.1152/ajpendo.90207.2008
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9(8):1137–1141. https://doi.org/10.1002/jbmr.5650090802
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285(6):785–795. https://doi.org/10.1001/jama.285.6.785
Tasnim N, Dutta P, Nayeem J, Masud P, Ferdousi A, Ghosh AS, Hossain M, Rajia S, Kubra KT, Sakibuzzaman M, Khan AT (2021) Osteoporosis, an inevitable circumstance of chronic kidney disease: a systematic review. Cureus 13(10):e18488. https://doi.org/10.7759/cureus.18488
Hall RK, Sloane R, Pieper C, Van Houtven C, LaFleur J, Adler R, Colon-Emeric C (2018) Competing risks of fracture and death in older adults with chronic kidney disease. J Am Geriatr Soc 66(3):532–538. https://doi.org/10.1111/jgs.15256
Slouma M, Sahli H, Bahlous A, Laadhar L, Smaoui W, Rekik S, Gharsallah I, Sallami M, Moussa FB, Elleuch M, Cheour E (2020) Mineral bone disorder and osteoporosis in hemodialysis patients. Adv Rheumatol 60(1):15. https://doi.org/10.1186/s42358-020-0118-0
Fusaro M, Re Sarto GV, Gallieni M, Cosmai L, Messa P, Rossini M, Chiodini I, Plebani M, Evenepoel P, Harvey N, Ferrari S, Cannata-Andia J, Trombetti A, Brandi ML, Ketteler M, Nickolas TL, Cunningham J, Salam S, Della Rocca C, Scarpa A, Minisola S, Malberti F, Cetani F, Cozzolino M, Mazzaferro S, Morrone L, Tripepi G, Zaninotto M, Mereu MC, Ravera M, Cianciolo G, La Manna G, Aghi A, Giannini S, Dalle Carbonare L, On Behalf Of The Sin-Siommms Bone Biopsy Promoting Group (2022) Time for revival of bone biopsy with histomorphometric analysis in chronic kidney disease (CKD): moving from skepticism to pragmatism. Nutrients. https://doi.org/10.3390/nu14091742
Colaianni G, Faienza MF, Sanesi L, Brunetti G, Pignataro P, Lippo L, Bortolotti S, Storlino G, Piacente L, D’Amato G, Colucci S, Grano M (2019) Irisin serum levels are positively correlated with bone mineral status in a population of healthy children. Pediatr Res 85(4):484–488. https://doi.org/10.1038/s41390-019-0278-y
Wu LF, Zhu DC, Tang CH, Ge B, Shi J, Wang BH, Lu YH, He P, Wang WY, Lu SQ, Zhong J, Zhou X, Zhu K, Ji W, Gao HQ, Gu HB, Mo XB, Lu X, Zhang L, Zhang YH, Deng FY, Lei SF (2018) Association of plasma irisin with bone mineral density in a large chinese population using an extreme sampling design. Calcif Tissue Int 103(3):246–251. https://doi.org/10.1007/s00223-018-0415-3
Gamez-Nava JI, Ramirez-Villafana M, Cons-Molina F, Gomez-Ramirez EE, Esparza-Guerrero Y, Saldana-Cruz AM, Sanchez-Rodriguez EN, Jacobo-Cuevas H, Totsuka-Sutto SE, Perez-Guerrero EE, Huerta M, Trujillo X, Vasquez-Jimenez JC, Nava-Zavala AH, Cardona-Munoz EG, Alcaraz-Lopez MF, Gonzalez-Lopez L (2022) Serum irisin concentrations and osteoporotic vertebral fractures in women with rheumatoid arthritis: a cross-sectional study. Medicine (Baltimore) 101(6):e28799. https://doi.org/10.1097/MD.0000000000028799
Liu K, Jing P, Liu Z, Wang Y, Han Z, Wang Y, Zheng Z, Wu Y, Wang T, Li Y, Zhang H, Wang L (2021) Serum levels of irisin in postmenopausal women with osteoporotic hip fractures. Cytokine 148:155708. https://doi.org/10.1016/j.cyto.2021.155708
Rodriguez-Carmona A, Perez Fontan M, Sangiao Alvarellos S, Garcia Falcon T, Pena Bello ML, Lopez Muniz A, Cordido F (2016) Serum levels of the adipomyokine irisin in patients with chronic kidney disease. Nefrologia 36(5):496–502. https://doi.org/10.1016/j.nefro.2016.05.019
Wen MS, Wang CY, Lin SL, Hung KC (2013) Decrease in irisin in patients with chronic kidney disease. PLoS One 8(5):e64025. https://doi.org/10.1371/journal.pone.0064025
Polyzos SA, Anastasilakis AD, Efstathiadou ZA, Makras P, Perakakis N, Kountouras J, Mantzoros CS (2018) Irisin in metabolic diseases. Endocrine 59(2):260–274. https://doi.org/10.1007/s12020-017-1476-1
Kaluzna M, Hoppe K, Schwermer K, Ibrahim AY, Pawlaczyk K, Ziemnicka K (2016) Adropin and irisin levels in relation to nutrition, body composition, and insulin resistance in patients with end-stage renal disease on chronic hemodialysis and peritoneal dialysis. Pol Arch Med Wewn 126(7–8):474–482. https://doi.org/10.20452/pamw.3466
Meng C, Jorgensen HS, Verlinden L, Bravenboer N, de Loor H, D’Haese PC, Carmeliet G, Evenepoel P (2022) Contemporary kidney transplantation has a limited impact on bone microarchitecture. Bone Rep 16:101172. https://doi.org/10.1016/j.bonr.2022.101172
Hori M, Yasuda K, Takahashi H, Matsuoka Y, Tsujita M, Nishihira M, Uchida K, Morozumi K, Maruyama S (2022) Lateral spine dual-energy X-ray absorptiometry and the risk of fragility fractures in long-term kidney graft recipients. Clin Exp Nephrol. https://doi.org/10.1007/s10157-022-02210-3
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Demir, C., Dursun, A.D., Sarıyıldız, G.T. et al. Serum irisin levels and osteoporosis in patients with advanced chronic kidney disease and renal transplant recipients. Int Urol Nephrol 55, 1821–1828 (2023). https://doi.org/10.1007/s11255-023-03475-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03475-7