ABSTRACT
Purpose
To elucidate the role of metabolism in the pharmacokinetics and pharmacodynamics of intranasal loxapine in conscious animals.
Methods
At pre-determined time points after intranasal or oral loxapine administration, levels of loxapine, loxapine metabolites, and neurotransmitters in rat brain were quantified after catalepsy assessments (block test and paw test). Cataleptogenicity of loxapine was also compared with its metabolites.
Results
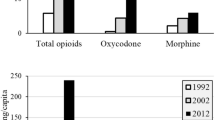
Intranasally administered loxapine was efficiently absorbed into systemic circulation followed by entering brain, with tmax ≤15 min in all brain regions. Oral route delivered minimal amounts of loxapine to plasma and brain. Brain AUC0–240min values of 7-hydroxy-loxapine were similar after intranasal and oral administration. Intranasal loxapine tended to induce less catalepsy than oral loxapine, although statistical significance was not reached. The catalepsy score was positively and significantly correlated with the striatal concentration of 7-hydroxy-loxapine, but not with loxapine. 7-hydroxy-loxapine was more cataleptogenic than loxapine, while the presence of loxapine tended to reduce rather than intensify 7-hydroxy-loxapine-induced catalepsy. The increases in striatal dopamine turnover were comparable after intranasal and oral loxapine administration.
Conclusions
The metabolite 7-hydroxy-loxapine, but not loxapine, was the main contributor to the catalepsy observed after intranasal and oral loxapine treatment. Intranasal route could effectively deliver loxapine to brain.









Similar content being viewed by others
Abbreviations
- 3-MT:
-
3-methoxytyramine
- 5-HIAA:
-
5-hydroxyindole-3-acetic acid
- 5-HT:
-
Serotonin
- 7-OH-amoxapine:
-
7-hydroxy-amoxapine
- 7-OH-loxapine:
-
7-hydroxy-loxapine
- 8-OH-amoxapine:
-
8-hydroxy-amoxapine
- 8-OH-loxapine:
-
8-hydroxy-loxapine
- AUC:
-
area under the curve
- Cmax :
-
maximum concentration
- CNS:
-
central nervous system
- CYP:
-
cytochrome P450
- DA:
-
dopamine
- DOPAC:
-
3,4-dihydroxyphenylacetic acid
- HVA:
-
homovanillic acid
- IM:
-
intramuscular
- IV:
-
intravenous
- PD:
-
pharmacodynamics
- PK:
-
pharmacokinetics
- t1/2 :
-
half life
- tmax :
-
time to maximum concentration
REFERENCES
Wong YC, Zuo Z. Intranasal delivery–modification of drug metabolism and brain disposition. Pharm Res. 2010;27(7):1208–23.
Wong YC, Qian S, Zuo Z. Regioselective biotransformation of CNS drugs and its clinical impact on adverse drug reactions. Expert Opin Drug Metab Toxicol. 2012;8(7):833–54.
Midha KK, Hubbard JW, McKay G, Hawes EM, Hsia D. The role of metabolites in a bioequivalence study 1: loxapine, 7-hydroxyloxapine and 8-hydroxyloxapine. Int J Clin Pharmacol Ther Toxicol. 1993;31(4):177–83.
Wong YC, Wo SK, Zuo Z. Investigation of the disposition of loxapine, amoxapine and their hydroxylated metabolites in different brain regions, CSF and plasma of rat by LC–MS/MS. J Pharm Biomed Anal. 2012;58(1):83–93.
Richelson E. Receptor pharmacology of neuroleptics: relation to clinical effects. J Clin Psychiatry. 1999;60 Suppl 10:5–14.
Pierre JM. Extrapyramidal symptoms with atypical antipsychotics: incidence, prevention and management. Drug Saf. 2005;28(3):191–208.
Porsolt RD, Moser PC, Castagné V. Behavioral indices in antipsychotic drug discovery. J Pharmacol Exp Ther. 2010;333(3):632–8.
Hoffman DC, Donovan H. Catalepsy as a rodent model for detecting antipsychotic drugs with extrapyramidal side effect liability. Psychopharmacology (Berl). 1995;120(2):128–33.
Wadenberg MLG, Kapur S, Soliman A, Jones C, Vaccarino F. Dopamine D2 receptor occupancy predicts catalepsy and the suppression of conditioned avoidance response behaviour in rats. Psychopharmacology (Berl). 2000;150(4):422–9.
Kumar M, Misra A, Babbar AK, Mishra AK, Mishra P, Pathak K. Intranasal nanoemulsion based brain targeting drug delivery system of risperidone. Int J Pharm. 2008;358(1–2):285–91.
Kumar M, Misra A, Mishra AK, Mishra P, Pathak K. Mucoadhesive nanoemulsion-based intranasal drug delivery system of olanzapine for brain targeting. J Drug Target. 2008;16(10):806–14.
Patel S, Chavhan S, Soni H, Babbar AK, Mathur R, Mishra AK, et al. Brain targeting of risperidone-loaded solid lipid nanoparticles by intranasal route. J Drug Target. 2011;19(6):468–74.
Illum L. Nasal delivery. The use of animal models to predict performance in man. J Drug Target. 1996;3(6):427–42.
Hirai S, Yashiki T, Matsuzawa T, Mima H. Absorption of drugs from the nasal mucosa of rat. Int J Pharm. 1981;7(4):317–25.
Mayor SH, Illum L. Investigation of the effect of anaesthesia on nasal absorption of insulin in rats. Int J Pharm. 1997;149(1):123–9.
Yang Z, Huang Y, Gan G, Sawchuk RJ. Microdialysis evaluation of the brain distribution of stavudine following intranasal and intravenous administration to rats. J Pharm Sci. 2005;94(7):1577–88.
Sanberg PR, Martinez R, Shytle RD, Cahill DW. The catalepsy test: is a standardized method possible? In: Sanberg PR, Ossenkopp KP, Kavaliers M, editors. Motor activity and movement disorders Totowa. NJ: Humana Press; 1996. p. 197–211.
Sanberg PR, Bunsey MD, Giordano M, Norman AB. The catalepsy test: its ups and downs. Behav Neurosci. 1988;102(5):748–59.
Vrijmoed-De Vries MC, Tonissen H, Cools AR. The relationship between hindlimb disturbances, forelimb disturbances and catelepsy after increasing doses of muscimol injected into the striatal-pallidal complex. Psychopharmacology (Berl). 1987;92(1):73–7.
Ellenbroek BA, Peeters BW, Honig WM, Cools AR. The paw test: a behavioral paradigm for differentiating between classical and atypical neuroleptic drugs. Psychopharmacology (Berl). 1987;93(3):343–8.
Costall B, Naylor RJ. Neuroleptic and non neuroleptic catalepsy. Arzneimittelforschung. 1973;23:674–83.
Stille G, Lauener H. Pharmacology of catatonigenic substances. 1. Correlation between neuroleptic catalepsy and the homovanillic acid level in rat corpus striatum. Arzneimittelforschung. 1971;21(2):252–5.
Tareke E, Bowyer JF, Doerge DR. Quantification of rat brain neurotransmitters and metabolites using liquid chromatography/electrospray tandem mass spectrometry and comparison with liquid chromatography/electrochemical detection. Rapid Commun Mass Spectrom. 2007;21(23):3898–904.
Diop L, Gottberg E, Briere R, Grondin L, Reader TA. Distribution of dopamine D1 receptors in rat cortical areas, neostriatum, olfactory bulb and hippocampus in relation to endogenous dopamine contents. Synapse. 1988;2(4):395–405.
Ereshefsky L. Pharmacologic and pharmacokinetic considerations in choosing an antipsychotic. J Clin Psychiatry. 1999;60 Suppl 10:20–30.
Narige T, Mizumura M, Okuizumi N, Matsumoto K, Furukawa Y, Hondo T. Study of the absorption, distribution, metabolism, and excretion of amoxapine in rats. Yakuri to Chiryo. 1981;9(5):1885–92.
Furubayashi T, Kamaguchi A, Kawaharada K, Masaoka Y, Kataoka M, Yamashita S, et al. Evaluation of the contribution of the nasal cavity and gastrointestinal tract to drug absorption following nasal application to rats. Biol Pharm Bull. 2007;30(3):608–11.
Tuk B, Van Oostenbruggen MF, Herben VMM, Mandema JW, Danhof M. Characterization of the pharmacodynamic interaction between parent drug and active metabolite in vivo: midazolam and alpha-OH-midazolam. J Pharmacol Exp Ther. 1999;289(2):1067–74.
Burstein S, Hunter SA, Latham V, Renzulli L. A major metabolite of Δ1-tetrahydrocannabinol reduces its cataleptic effect in mice. Experientia. 1987;43(4):402–3.
Bun SS, Voeurng V, Bun H. Interspecies variability and drug interactions of loxapine metabolism in liver microsomes. Eur J Drug Metab Pharmacokinet. 2003;28(4):295–300.
Burki HR, Fischer R, Hunziker F. Dibenzo-epines: effect of the basic side-chain on neuroleptic activity. Eur J Med Chem. 1978;13(5):479–85.
Seeman P. Targeting the dopamine D2 receptor in schizophrenia. Expert Opin Ther Targets. 2006;10(4):515–31.
Midha KK, Rawson MJ, Hubbard JW. The role of metabolites in bioequivalence. Pharm Res. 2004;21(8):1331–44.
Paprocki J, Versiani M. A double-blind comparison between loxapine and haloperidol by parenteral route in acute schizophrenia. Curr Ther Res Clin Exp. 1977;21(1):80–100.
Simpson GM, Cooper TB, Lee JH, Young MA. Clinical and plasma level characteristics of intramuscular and oral loxapine. Psychopharmacology (Berl). 1978;56(2):225–32.
Al-Suwayeh SA, Tebbett IR, Wielbo D, Brazeau GA. In vitro-in vivo myotoxicity of intramuscular liposomal formulations. Pharm Res. 1996;13(9):1384–8.
Chakrabarti A, Bagnall A, Chue P, Fenton M, Palaniswamy V, Wong W, et al. Loxapine for schizophrenia. Cochrane Database Syst Rev. 2007;4, CD001943.
Sztrymf B, Chevrel G, Bertrand F, Margetis D, Hurel D, Ricard J, et al. Beneficial effects of loxapine on agitation and breathing patterns during weaning from mechanical ventilation. Crit Care. 2010;14(3).
Krieger D, Hansen K, McDermott C, Matthews R, Mitchell R, Bollegala N, et al. Loxapine versus olanzapine in the treatment of delirium following traumatic brain injury. NeuroRehabilitation. 2003;18(3):205–8.
Reinblatt SP, Abanilla PK, Jummani R, Coffey B. Loxapine treatment in an autistic child with aggressive behavior: therapeutic challenges. J Child Adolesc Psychopharmacol. 2006;16(5):639–43.
Carlyle W, Ancill RJ, Sheldon L. Aggression in the demented patient: a double-blind study of loxapine versus haloperidol. Int Clin Psychopharmacol. 1993;8(2):103–8.
Hale RL, Munzar P, Rabinowitz JD, inventors. Alexza Molecular Delivery Corporation, USA, assignee. Method for treating pain with loxapine and amoxapine. Patent Application Country: Application: US; Patent Country: US; Priority Application Country: US patent 2004102434. 2004 0527; Patent Application Date: 20031120.; Priority Application Date: 20021126.
Kimishima K, Sakamoto T, Yamasaki M, Tanabe K, Amano Y. Central nervous actions of new neuroleptics, dibenzoazepine derivatives. Yonago Igaku Zasshi. 1969;20(6):525–36.
Stefanova D. Cloxazepine—neuropharmacological studies. Eksp Med Morfol. 1981;20(4):208–13.
Chen YW, Huang KL, Liu SY, Tzeng JI, Chu KS, Lin MT, et al. Intrathecal tri-cyclic antidepressants produce spinal anesthesia. Pain. 2004;112(1–2):106–12.
Matsudaira K, Seichi A, Yamazaki T, Kishimoto J, Takeshita K, Nakamura K. Efficacy of tricyclic antidepressant for somatoform pain disorders with chronic lower back and leg pain. J Lumbar Spine Disord. 2004;10(1):155–62.
Lochhead JJ, Thorne RG. Intranasal delivery of biologics to the central nervous system. Adv Drug Deliv Rev. 2012;64(7):614–28.
Akerman S, Holland PR, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci. 2011;12(10):570–84.
Johnson NJ, Hanson LR, Frey II WH. Trigeminal pathways deliver a low molecular weight drug from the nose to the brain and orofacial structures. Mol Pharm. 2010;7(3):884–93.
ACKNOWLEDGMENTS AND DISCLOSURES
CUHK Direct Grant 4450272 and General Research Fund CUHK 480809.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 379 kb)
Rights and permissions
About this article
Cite this article
Wong, Y.C., Zuo, Z. Brain Disposition and Catalepsy After Intranasal Delivery of Loxapine: Role of Metabolism in PK/PD of Intranasal CNS Drugs. Pharm Res 30, 2368–2384 (2013). https://doi.org/10.1007/s11095-013-1080-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-013-1080-x