Abstract
Introduction Chromosome 10q allelic loss commonly occurs in glioblastoma. Disruption of PTEN, one of three known 10q tumor suppressor genes, affects the immune system by increasing tumor expression of immunosuppressive protein B7-H1 and by increasing tumor release of Th2-inducing cytokines. While the former might impair antitumor cellular immunity, a consideration for immunotherapy, the latter could cause 10q-maintaining tumor patients to experience comparatively higher rates of bacterial infections, a source of morbidity and mortality in glioblastoma patients. Methods We retrospectively reviewed 58 glioblastoma patients whose tumors were designated “normal-10q” (n = 16) or “LOH-10q” (n = 42) using loss of heterozygosity (LOH) assays of microsatellite markers in constitutional/tumor DNA pairs. Records were reviewed for symptomatic, microbiologically or radiographically confirmed infections in the first 2 years after diagnosis. Results Infection occurred more frequently in “normal-10q” than “LOH-10q” patients (56% vs. 14% of patients experiencing infection; P = 0.001). “Normal-10q” patients more commonly developed all four infection types studied (urinary tract = 38% vs. 13%, craniotomy wound = 19% vs. 0%, pneumonia = 19% vs. 5%, sepsis = 6% vs. 3%). “Normal-10q” and “LOH-10q” patients had similar survival, ages, chemotherapy treatment rates, and frequency of patients on dexamethasone 1 month after radiation therapy (P = 0.4–0.98), making these factors unlikely to explain the observed difference in infection rates. Conclusion While tumor mutations may inhibit antitumor immunity, the effects of these mutations on systemic immunity remain undetermined. We found higher infection rates after glioblastoma diagnosis in patients whose tumors maintained chromosome 10q than in patients whose tumors had allelic 10q loss. Differing effects of this genetic alteration on antitumor and systemic immunity may warrant further investigation, potentially providing insight into mechanisms of antitumor immunity and host defenses against local and systemic infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Three tumor suppressor genes residing on human chromosome 10q (ERCC 6, PTEN, and DMBT1) have been implicated in the development and progression of several types of neoplasms, including astrocytic tumors [1–5]. In particular, chromosome 10q allelic loss commonly occurs in glioblastoma, with over 80% of glioblastomas exhibiting loss of heterozygosity (LOH) for at least one locus on chromosome 10q [6].
Glioblastoma patients can exhibit impaired antitumor immunity and impaired systemic immunity leading to bacterial infections. The former relies on local cellular immunity mediated by the Th1 subset of helper T cells, while the latter relies on systemic humoral immunity mediated by the Th2 subset of helper T cells. These two types of impaired immunity may occur in different subsets of glioblastoma patients: two-thirds of glioblastoma patients have tumor-secreted cytokines that promote a circulating Th2 profile, while 1/3 favor a Th1 profile [7, 8].
Interestingly, disruption of two of the 3 tumor suppressor genes found on chromosome 10q may mediate a decrease in tumor cell immunogenicity, with their loss impairing an effective cellular host immune response to the tumor. First, DBMT1 may attract tumor-infiltrating macrophages: its loss may impair microglial infiltration into gliomas [9]. Second, disruption of PTEN (phosphatase and tensin homologue deleted in chromosome 10) may increase expression of immunosuppressive protein B7-H1 [10] and also increases Th2-inducing cytokine release [11, 12]. While the former might impair antitumor cellular immunity in patients with LOH on chromosome 10q, a consideration for immunotherapy, the latter could cause 10q-maintaining tumor patients to experience increased bacterial infections, a source of morbidity and mortality in glioblastoma patients.
We investigated the possibility that tumor-specific mutations in chromosome 10q could define two subsets of glioblastoma patients, one subset with impaired cellular antitumor immunity and another with less effective humoral immunity to systemic infection. Specifically, we sought to determine if tumor LOH of 10q, which has previously been shown to impair the cellular immune response to malignant gliomas [10], might be associated with increased systemic humoral immunity, as manifested by a reduced incidence of systemic infections.
Methods
Patients
We retrospectively reviewed 58 glioblastoma patients whose tumors were classified on the basis of loss of heterozygosity of 10q (n = 42) or maintained heterozygosity of 10q (n = 16). Tumor DNA was extracted from microdissected, formalin-fixed, paraffin-embedded sections; constitutional DNA was extracted from blood lymphocytes or from formalin-fixed, paraffin-embedded sections of adjacent, uninvolved brain or other tissues [13]. Allelic chromosomal loss was assessed by loss of heterozygosity assays in constitutional DNA/tumor DNA pairs using microsatellite markers on 10q23-24 (D10S185 and D10S2491, near PTEN) and 10q25-26 (D10S587) [13]. The tumors reported here are those among a consecutive series of 140 consecutive newly diagnosed glioblastomas resected at our institution 1995–2001 and molecularly analyzed in a previous report [14] for which sufficient tissue was available to assess for loss of heterozygosity of 10q. Karnofsky performance score (KPS) was determined by the neuro-oncologist at the first clinic visit. We reviewed medical records for the following types of infections occurring within 2 years of patients’ glioblastoma diagnosis: (1) symptomatic pneumonia confirmed by chest X-ray and treated with antibiotics; (2) urinary tract infection confirmed by suspicious urinalysis or positive urine culture and treated with antibiotics; (3) craniotomy wound infection requiring reoperation and/or antibiotics; and (4) blood-borne infection confirmed by two bottles of blood cultures that grew an organism and led to antibiotic treatment. This study was approved by the Institutional Review Board (IRB) at our institution.
Statistical analysis
Student’s t-test was used for parametric comparisons between variables. A Mantel–Haenszel analysis was used to analyze infections in patients with and without LOH 10q stratified by infection type. A multivariate Cox proportional hazards model was used to analyze infections as a function of LOH 10q status, age, postoperative chemotherapy, and whether a patient was still on dexamethasone 1 month after radiation. Kaplan Meier survival analysis and the logrank test were used to compare time to infection in the glioblastoma subgroups. Patients who died without known infections were censored in this analysis at the time of death. P values are two-tailed.
Results
Patient characteristics
Patients whose tumors had maintenance versus LOH 10q had similar profiles when analyzed for parameters that might influence their rate of systemic infections, including survival, age at diagnosis, KPS, tumor diameter at diagnosis, white blood cell (WBC) count prior to chemotherapy and radiation, percentage of patients whose tumors were biopsied versus surgically resected, percentage of patients receiving postoperative chemotherapy, and percentage of patients on dexamethasone 1 month after finishing radiation therapy (P = 0.4–0.98) (Table 1).
Infections
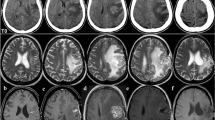
Infections of all kinds were more frequent in patients whose glioblastomas did not have LOH 10q (56%) compared to patients whose glioblastomas had LOH 10q (14%) (Fig. 1) (P = 0.001). In terms of specific types of infections, urinary tract infections (38% vs. 13%, P = 0.03), craniotomy wound infections (19% vs. 0%, P = 0.004), pneumonia (19% vs. 5%, P = 0.09), and positive blood cultures (6% vs. 3%, P = 0.5) were more common in patients whose glioblastomas did not have LOH 10q (Fig. 2). A Mantel–Haenszel analysis stratified by infection type yielded an odds ratio of 4.2 (95% CI = 1.4–12.4) for infection in patients whose tumors did not have LOH 10q compared to those whose tumors did (P = 0.0002). A Cox proportional hazards model revealed that infection of any type was significantly predicted by lack of LOH 10q (Hazard Ratio = 4.6; P = 0.002) and by dexamethasone use 1 month after radiation therapy (Hazard Ratio = 1.9; P = 0.003); age, postoperative chemotherapy, KPS, tumor diameter, WBC count prior to chemotherapy and radiation, and use of resection rather than biopsy were not significantly predictive of infection of any type (Table 2).
Admission with infection
Patients whose tumors maintained 10q were admitted to the hospital with infection more frequently (38%) than those whose tumors had LOH 10q (5%) (P = 0.001) (Fig. 3). Total hospital days for these admissions were 43 days for patients whose glioblastomas maintained 10q compared to 23 days for patients whose glioblastomas had LOH 10q, with a mean of 6 days per admission.
Time to infection
Patients with glioblastomas that maintained 10q developed infection sooner after glioblastoma diagnosis than patients whose glioblastomas exhibited LOH 10q (Fig. 4; logrank P = 0.0002).
Discussion
While tumor mutations may inhibit the host antitumor cellular immune response, the effects of these mutations on host immunity to systemic infections remain undetermined. We found that loss of heterozygosity of 10q, a glioblastoma mutation that may reduce antitumor cellular immunity, is also associated with less frequent systemic infections, suggesting a nonspecifically enhanced humoral immunity relative to patients who harbor glioblastomas maintaining 10q.
The rates of systemic infections in our glioblastoma patients are comparable to those reported elsewhere. We reported a 13% overall rate of hospitalization with infection during the 2 years after glioblastoma diagnosis, while another report described a 9% rate of hospitalization for glioblastoma patients during the 6 weeks of radiotherapy [15]. Another study reported a 4% wound infection rate with craniotomies in general [16]. Thus, our overall wound infection rate of 5% is not unreasonable considering the immunosuppressed state of glioblastoma patients.
Three tumor suppressor genes residing on human chromosome 10q (ERCC 6, PTEN, and DMBT1) have been implicated in the development and progression of several types of neoplasms, including astrocytic tumors. Chromosome 10q allelic loss commonly occurs in glioblastoma, with over 80% of glioblastomas exhibiting loss of heterozygosity (LOH) for at least one locus on chromosome 10q [6], a far more common alteration than alterations in any of the three individual oncogenes residing on 10q. For example, PTEN alterations are seen in 30–44% of glioblastomas [17]. Thus, our findings suggest that there is a reduced rate of systemic infections in patients whose glioblastomas exhibit alterations of one or more of these three oncogene(s) on chromosome 10q.
Interestingly, two of the three known tumor suppressor genes found on chromosome 10q may mediate a cellular antitumor immune response, with their loss impairing this response. First, DMBT1 is a candidate tumor suppressor for brain, gastrointestinal, and lung cancer, although one study found that DMBT1 homozygous deletions in 10 glioblastomas with 10q LOH reflected unmasking of constitutional deletion polymorphisms by the 10q loss [18]. DMBT1 belongs to the superfamily of scavenger receptor cysteine-rich proteins, is produced by both tumor-associated macrophages and tumor cells, and appears to attract tumor-infiltrating macrophages, allowing its loss to potentially impair microglial infiltration into gliomas [9]. Second, disruption of PTEN, an inhibitor of the PI3 kinase signaling pathway, may increase expression of immunosuppressive protein B7-H1 [10] and increases Th2-inducing cytokine release [11, 12].
Glioblastoma patients can exhibit impaired antitumor immunity and impaired systemic immunity leading to bacterial infections. The former relies on local cellular immunity mediated by the Th1 subset of helper T cells, while the latter relies on systemic humoral immunity mediated by the Th2 subset of helper T cells. These two types of impaired immunity may occur in different subsets of glioblastoma patients. Of note, two-thirds of glioblastoma patients have tumor-secreted cytokines that favor a circulating Th2 profile, while 1/3 of glioblastomas secrete cytokines favoring a Th1 profile [7, 8]. One study found that most glioblastoma patients have both elevated circulating levels of interleukin 10, a Th2 promoting cytokine, and reduced circulating interleukin 12, a Th1 promoting cytokine, and that the changes were independent of corticosteroid usage [19]. A similar report found that the Th1-promoting cytokines tumor necrosis factor (TNF) α and interferon (IFN) gamma were reduced in peripheral lymphocytes and glioma cell cultures compared to controls, and that the Th2 promoting cytokines interleukin 4 and interleukin 10 were elevated in peripheral lymphocytes and glioma cell cultures compared to controls [20]. In addition to the roles of these cytokines in maintaining the Th2 profile in the majority of glioma patients, others have found that an increased regulatory T cell fraction causes this Th2 profile [21]. In some tumor types, Th1 cells are tumoricidal via a FasL-Fas interaction, while Th2 cells promote tumor growth [22], underscoring the ability of the two helper T cell types to exert opposite effects on tumors. The observations that glioblastoma patients who experience postoperative cranial wound infections exhibit longer survival [23, 24] and that postoperative empyema prolongs survival in bronchogenic carcinoma patients [25, 26] have been attributed to bacterial lipopolysaccharide (LPS) eliciting a nonspecific immune response a portion of which targets the tumor [27, 28] or to these infections causing an immune cell infiltrate at the tumor resection site which promotes a specific cross-reactive immunological attack against the tumor. However, our findings also raise the possibility that tumor mutations might stratify patients into two groups with different circulating helper T cell profiles—those with more potent antitumor Th1-mediated cellular immunity capable of limiting tumor growth may also have weaker Th2-mediated humoral immunity rendering them more prone to infections, while patients whose tumor mutations lead to a circulating Th2 profile might ward off infection effectively but be unable to mount a cellular immune response against the tumor.
We hypothesize that our finding that patients whose glioblastomas exhibited LOH 10q exhibited a reduced frequency of systemic infections reflected a circulating Th2 versus Th1 profile. Our study was an initial study designed to address a different hypothesis, that patients whose glioblastomas exhibiting LOH 10q would exhibit a reduced frequency of systemic infections. Future studies will need to overcome limitations of our study, which include its retrospective nature and somewhat smaller sample size. The hypothesis that we verified in our retrospective series will first require verification by prospective analysis in larger series. Such studies could also address other questions by investigating the circulating helper T cell profile in a large number of glioblastoma patients and correlating it with, not just tumoral 10q status, the parameter analyzed in our report, but with mutations in each of the three specific 10q oncogenes, and with the subsequent development of clinical infections. If our data is elaborated upon in this manner, the fact that the majority of glioblastomas exhibit LOH 10q could explain why the majority of glioblastoma patients exhibit a circulating Th2 rather than Th1 profile, one that promotes humoral immunity against systemic infection but weakens cellular antitumor immunity [19]. Further investigation of the different effects of an oncogene mutation on antitumor cellular versus systemic humoral immunity could provide insight into both antitumor immunity and host defenses against local and systemic infection. Such insight may help identify glioblastoma patients who might benefit most from immunotherapy or patients who might need greater antibiotic prophylaxis, and might eventually lead to ways of stimulating antitumor immunity while protecting glioblastoma patients from infection-induced morbidity and mortality.
References
Dabholkar MD, Berger MS, Vionnet JA, Overton L, Thompson C, Bostick-Bruton F, Yu JJ, Silber JR, Reed E (1996) Comparative analyses of relative ERCC3 and ERCC6 mRNA levels in gliomas and adjacent non-neoplastic brain. Mol Carcinog 17:1–7. doi:10.1002/(SICI)1098-2744(199609)17:1<1::AID-MC1>3.0.CO;2-M
Suzuki T, Maruno M, Wada K, Kagawa N, Fujimoto Y, Hashimoto N, Izumoto S, Yoshimine T (2004) Genetic analysis of human glioblastomas using a genomic microarray system. Brain Tumor Pathol 21:27–34. doi:10.1007/BF02482174
Choe G, Horvath S, Cloughesy TF, Crosby K, Seligson D, Palotie A, Inge L, Smith BL, Sawyers CL, Mischel PS (2003) Analysis of the phosphatidylinositol 3′-kinase signaling pathway in glioblastoma patients in vivo. Cancer Res 63:2742–2746
Ermoian RP, Furniss CS, Lamborn KR, Basila D, Berger MS, Gottschalk AR, Nicholas MK, Stokoe D, Haas-Kogan DA (2002) Dysregulation of PTEN and protein kinase B is associated with glioma histology and patient survival. Clin Cancer Res 8:1100–1106
Smith JS, Tachibana I, Passe SM, Huntley BK, Borell TJ, Iturria N, O’Fallon JR, Schaefer PL, Scheithauer BW, James CD, Buckner JC, Jenkins RB (2001) PTEN mutation, EGFR amplification, and outcome in patients with anaplastic astrocytoma and glioblastoma multiforme. J Natl Cancer Inst 93:1246–1256. doi:10.1093/jnci/93.16.1246
Daido S, Takao S, Tamiya T, Ono Y, Terada K, Ito S, Ouchida M, Date I, Ohmoto T, Shimizu K (2004) Loss of heterozygosity on chromosome 10q associated with malignancy and prognosis in astrocytic tumors, and discovery of novel loss regions. Oncol Rep 12:789–795
Hao C, Parney IF, Roa WH, Turner J, Petruk KC, Ramsay DA (2002) Cytokine and cytokine receptor mRNA expression in human glioblastomas: evidence of Th1, Th2 and Th3 cytokine dysregulation. Acta Neuropathol 103:171–178. doi:10.1007/s004010100448
Morford LA, Dix AR, Brooks WH, Roszman TL (1999) Apoptotic elimination of peripheral T lymphocytes in patients with primary intracranial tumors. J Neurosurg 91:935–946
Mollenhauer J, Herbertz S, Holmskov U, Tolnay M, Krebs I, Merlo A, Schroder HD, Maier D, Breitling F, Wiemann S, Grone HJ, Poustka A (2000) DMBT1 encodes a protein involved in the immune defense and in epithelial differentiation and is highly unstable in cancer. Cancer Res 60:1704–1710
Parsa AT, Waldron JS, Panner A, Crane CA, Parney IF, Barry JJ, Cachola KE, Murray JC, Tihan T, Jensen MC, Mischel PS, Stokoe D, Pieper RO (2007) Loss of tumor suppressor PTEN function increases B7-H1 expression and immunoresistance in glioma. Nat Med 13:84–88. doi:10.1038/nm1517
Moody JL, Jirik FR (2004) Compound heterozygosity for Pten and SHIP augments T-dependent humoral immune responses and cytokine production by CD(4 +) T cells. Immunology 112:404–412. doi:10.1111/j.1365-2567.2004.01901.x
Suzuki A, Yamaguchi MT, Ohteki T, Sasaki T, Kaisho T, Kimura Y, Yoshida R, Wakeham A, Higuchi T, Fukumoto M, Tsubata T, Ohashi PS, Koyasu S, Penninger JM, Nakano T, Mak TW (2001) T cell-specific loss of Pten leads to defects in central and peripheral tolerance. Immunity 14:523–534. doi:10.1016/S1074-7613(01)00134-0
Louis DN, von Deimling A, Seizinger BR (1992) A (CA)n dinucleotide repeat assay for evaluating loss of allelic heterozygosity in small and archival human brain tumor specimens. Am J Pathol 141:777–782
Batchelor TT, Betensky RA, Esposito JM, Pham LD, Dorfman MV, Piscatelli N, Jhung S, Rhee D, Louis DN (2004) Age-dependent prognostic effects of genetic alterations in glioblastoma. Clin Cancer Res 10:228–233. doi:10.1158/1078-0432.CCR-0841-3
Hughes MA, Parisi M, Grossman S, Kleinberg L (2005) Primary brain tumors treated with steroids and radiotherapy: low CD4 counts and risk of infection. Int J Radiat Oncol Biol Phys 62:1423–1426. doi:10.1016/j.ijrobp.2004.12.085
Zentner J, Gilsbach J, Daschner F (1987) Incidence of wound infection in patients undergoing craniotomy: influence of type of shaving. Acta Neurochir (Wien) 86:79–82. doi:10.1007/BF01402288
Teng DH, Hu R, Lin H, Davis T, Iliev D, Frye C, Swedlund B, Hansen KL, Vinson VL, Gumpper KL, Ellis L, El-Naggar A, Frazier M, Jasser S, Langford LA, Lee J, Mills GB, Pershouse MA, Pollack RE, Tornos C, Troncoso P, Yung WK, Fujii G, Berson A, Steck PA et al (1997) MMAC1/PTEN mutations in primary tumor specimens and tumor cell lines. Cancer Res 57:5221–5225
Sasaki H, Betensky RA, Cairncross JG, Louis DN (2002) DMBT1 polymorphisms: relationship to malignant glioma tumorigenesis. Cancer Res 62:1790–1796
Kumar R, Kamdar D, Madden L, Hills C, Crooks D, O’Brien D, Greenman J (2006) Th1/Th2 cytokine imbalance in meningioma, anaplastic astrocytoma and glioblastoma multiforme patients. Oncol Rep 15:1513–1516
Zisakis A, Piperi C, Themistocleous MS, Korkolopoulou P, Boviatsis EI, Sakas DE, Patsouris E, Lea RW, Kalofoutis A (2007) Comparative analysis of peripheral and localised cytokine secretion in glioblastoma patients. Cytokine 39:99–105. doi:10.1016/j.cyto.2007.05.012
Fecci PE, Mitchell DA, Whitesides JF, Xie W, Friedman AH, Archer GE, Herndon JE II, Bigner DD, Dranoff G, Sampson JH (2006) Increased regulatory T-cell fraction amidst a diminished CD4 compartment explains cellular immune defects in patients with malignant glioma. Cancer Res 66:3294–3302. doi:10.1158/0008-5472.CAN-05-3773
Hong S, Qian J, Yang J, Li H, Kwak LW, Yi Q (2008) Roles of idiotype-specific t cells in myeloma cell growth and survival: Th1 and CTL cells are tumoricidal while Th2 cells promote tumor growth. Cancer Res 68:8456–8464. doi:10.1158/0008-5472.CAN-08-2213
Bowles AP Jr, Perkins E (1999) Long-term remission of malignant brain tumors after intracranial infection: a report of four cases. Neurosurgery 44:636–642. doi:10.1097/00006123-199903000-00110
Borrello I, Sotomayor E, Grossman SA (1997) Postoperative infections may impart a survival advantage in high-grade astrocytomas. American Society of Clinical Oncology (ASCO) 33rd Annual Meeting, Denver, CO
Ruckdeschel JC, Codish SD, Stranahan A, McKneally MF (1972) Postoperative empyema improves survival in lung cancer. Documentation and analysis of a natural experiment. N Engl J Med 287:1013–1017
Cady B, Cliffton EE (1967) Empyema and survival following surgery for bronchogenic carcinoma. J Thorac Cardiovasc Surg 53:102–108
Mariani CL, Rajon D, Bova FJ, Streit WJ (2007) Nonspecific immunotherapy with intratumoral lipopolysaccharide and zymosan A but not GM-CSF leads to an effective anti-tumor response in subcutaneous RG-2 gliomas. J Neurooncol 85:231–240. doi:10.1007/s11060-007-9415-2
Chicoine MR, Won EK, Zahner MC (2001) Intratumoral injection of lipopolysaccharide causes regression of subcutaneously implanted mouse glioblastoma multiforme. Neurosurgery 48:607–614. doi:10.1097/00006123-200103000-00032
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Aghi, M.K., Batchelor, T.T., Louis, D.N. et al. Decreased rate of infection in glioblastoma patients with allelic loss of chromosome 10q. J Neurooncol 93, 115–120 (2009). https://doi.org/10.1007/s11060-009-9826-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-009-9826-3