Abstract
Development of new topical drugs requires an animal onychomycosis model that can predict the drug efficacy against moderate to severe human onychomycosis because the severity of onychomycosis varies and affects the drug efficacy. This study established a non-immunosuppressive guinea pig tinea unguium model under 8-week infection condition in addition to a previously reported model under 4-week infection condition. In the tinea unguium model, most fungi were tightly present in the arthrospore form, like in human onychomycosis. The topical formulations of efinaconazole and luliconazole, two azole class anti-onychomycosis drugs, were evaluated for their efficacy in these models. In the untreated group, the nail fungal burden in the 8-week model was higher than that in the 4-week model and the stronger infection intensity affected the efficacy of the drugs, suggesting that the 8-week model was more severe. The 90% efficacy rate (42%) of luliconazole in the 8-week model was significantly lowered than that (83%) in the 4-week model, and its 99% efficacy rates were 0% in both models. Conversely, the 90% and 99% efficacy rates of efinaconazole (92% and 50% in the 4-week model, and 75% and 25% in the 8-week model, respectively) were not significantly different between the two infection durations. In addition, efinaconazole was more effective than luliconazole in reducing the nail fungal burden. Considering the relevance of clinical reports of the effectiveness of efinaconazole on severe onychomycosis, the new severe tinea unguium model would predict drug efficacy against moderate to severe onychomycosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Onychomycosis is an infectious disease primarily caused by Trichophyton rubrum and Trichophyton interdigitale and has an estimated prevalence of 10% in Japan and 13.8% in the USA [1, 2]. Generally, onychomycosis is difficult to cure completely and reduces the patient’s quality of life due to difficulty in walking and poor nail appearance [3] as well as causes secondary infections to other family members [4]. Distal lateral subungual onychomycosis (DLSO), among several types of onychomycosis, is reported to be the most common type [5, 6]. The infection involves the subungual space and nail matrix in DLSO, extending proximally in advanced cases. A couple of drugs, oral and topical antifungals, are used for treating onychomycosis [7].
Nevertheless, the severity of onychomycosis in humans varies and affects the drug efficacy. Furthermore, the complete cure rates of topical antifungals against severe onychomycosis are generally lower than those of oral drugs [7], and the development of new topical drugs with advanced efficacy is desired. Thus, an animal onychomycosis model with increased infection intensity is essential to predict the drug potency in severe human onychomycosis. However, there have been no reports on the influence of infection intensity on drug potency in the animal onychomycosis model.
Generally, the in vivo efficacy of anti-onychomycosis drugs is evaluated using guinea pig or rabbit models [8,9,10,11,12]. In the production of several onychomycosis models, animals were treated with immunosuppressants to establish infection [9, 10]. Other models have shown stable nail infection in animals without immunosuppression [8, 11, 12]. The morbidity risk of onychomycosis has been reported to be higher in patients receiving long-term administration of immunosuppressive drugs than in healthy people [13], indicating the involvement of the host defense ability in the fungal pathogenesis. Notwithstanding, onychomycosis is a common infection among healthy people [13], and hence a non-immunosuppressed animal model would be more appropriate for drug efficacy evaluation. It has been reported that the host immunity is concerned with the disease state formation, affecting the growth form of the fungus and localization in the nails [13, 14]. In addition, the most common pathogen of human onychomycosis is T. rubrum [1], but there have been no reports on establishing animal tinea unguium models using T. rubrum. Trichophyton rubrum is adapted to humans [5] and does not naturally infect animals [15]. Thus, zoophilic T. mentagrophytes is commonly used to produce experimental animal tinea unguium.
This study established a non-immunosuppressed tinea unguium model with a stronger infection intensity than the previously reported model (4-week infection) [11, 12] by extending the infection duration to 8 weeks. Furthermore, efinaconazole and luliconazole, two azole class topical anti-onychomycosis drugs with different nail permeabilities and keratin affinities [10, 16], were evaluated for their efficacy in the tinea unguium models to investigate the effect of the infection duration on therapeutic efficacy of the topical drugs. In addition, to consider the extractability of the animal model to human onychomycosis, in vitro antifungal activities of the drugs against the arthrospores (parasitic form) of T. mentagrophytes and T. rubrum, were evaluated.
Materials and Methods
Test Substances
Efinaconazole (Sigma-Aldrich Co., LLC., St. Louis, MO, USA) and luliconazole (Toronto Research Chemicals, Toronto, ON, Canada) were used for the minimum effective concentration (MEC) test. Furthermore, to evaluate the therapeutic efficacy in guinea pig tinea unguium models, we used efinaconazole 10% solution (Kaken Pharmaceutical, Co., Ltd., Tokyo, Japan) prescribed clinically in Asia and North America, including Japan [10], and luliconazole 5% solution (Sato Pharmaceutical Co., Ltd., Tokyo, Japan) prescribed clinically in Japan for human onychomycosis treatment [10].
Strains
T. mentagrophytes SM-110 strain was provided by the Niigata University School of Medicine (Niigata, Japan). T. rubrum IFM 46157 strain was obtained from the Medical Mycology Research Center, Chiba University (Chiba, Japan).
Preparation of Arthrospores of T. mentagrophytes and T. rubrum
The arthrospores were prepared using a carbon dioxide culture medium according to the method of Fujita et al. [17]. Shortly, a membrane filter (pore size: 0.45 μm) was placed on a brain–heart infusion agar medium (Nissui Pharmaceutical Co., Ltd., Tokyo, Japan), onto which 100 μL of each strain’s microconidial suspension was added and plated. The agar plate was placed in an airtight container, generating carbon dioxide (theoretical concentration: 17%), and cultured at 30 °C for T. mentagrophytes and 35 °C for T. rubrum for 10 days. The arthrospores grown on the filter were collected and suspended in saline containing 0.05% Tween 80, giving fungal concentrations of 106 and 108 cells/mL for the MEC test and the production of the guinea pig tinea unguium models, respectively. For the MEC test, T. mentagrophytes and T. rubrum were used, and for the production of the animal models, T. mentagrophytes was used.
In vitro Antifungal Activity Against the Arthrospores
Antifungal activity was determined as follows: 200 mg of sterilized keratin powder (prepared by the method previously reported [11]) was added to the test tube as a condition for adding 20% keratin, and 500 μL of 3-(N-morpholino) propanesulfonic acid buffered RPMI 1640 medium (Nissui Pharmaceutical Co., Ltd., Tokyo, Japan) containing the test material (prepared by a two-fold stepwise dilution) and 500 μL of fungal suspension (final concentration: 104 cells/mL) were added after sterilizing the keratin powder. The mixture was statically incubated at 35 °C for 7 days. Generally, the antifungal activity is evaluated using the minimum inhibitory concentration (MIC), which is determined visually. However, in this study, the arthrospores were precipitated in a liquid medium, making it difficult to determine the MIC visually. Thus, the MEC was determined by microscopic examination of the fungi in the culture media and defined as the lowest drug concentration at which no obvious germination or hyphal elongation was observed compared with the growth control. The geometric mean MEC was calculated for each strain of the two independent experiments performed.
The Guinea Pig Tinea Unguium Model
The Production of the Guinea Pig Tinea Unguium Model and Histopathological Examination of Infected Nails
The arthrospore suspensions of T. mentagrophytes (inoculum size: 2 × 107 cells/foot) were inoculated into the plantar skin and between the toes (between the second and third toes and between the third and fourth toes) of the guinea pigs’ hind paws, as previously reported [11, 12]. The experiments were performed with a group of six animals (12 feet). The dermatophyte was transmitted from the skin to the nails by a 28-day (4-week) or 56-day (8-week) infection period, resulting in the production of the tinea unguium model (Fig. 1). A portion of the hind paw nails was collected in the 4-week infection model before the treatment. The morphology of the fungi in the nails was observed by light microscopy after the nail dissolution with 20% KOH. Before the 4-week infection treatment, the nail pieces of guinea pigs were collected, fixed in 10% neutral buffered formalin solution, and then demineralized with 10% formic acid–citric acid solution for 4 weeks (the fluid exchanges every 1 week). After demineralization, the nails were excised and neutralized with an aqueous sodium sulfate solution overnight. Eventually, paraffin embedding, slicing, and Grocott’s staining were performed using the conventional method. The nail specimens were then observed under a light microscope.
Evaluation of Therapeutic Efficacy in the Guinea Pig Tinea Unguium Models
Efinaconazole 10% solution or luliconazole 5% solution was applied to the nails of the hind paw once daily for 28 consecutive days. Each treatment was initiated on the 29th or 57th day after the arthrospore suspension inoculation. All animals were euthanized one week after the previous treatment. For one group, six animals with 12 feet were used. Their nails were collected per foot and homogenized with a glass homogenizer in PBS (pH 7.4) containing 0.25% trypsin and digested at 37 °C for about 1 h. A portion of the homogenate was dropped onto modified glucose peptone agar with lecithin and polysorbate 80 containing 1% lecithin and antibiotics. Then, it was plated and cultured at 30 °C for 14 days. The number of fungal colonies on the agar was used to calculate the number of viable fungi in the nails. The percentage of nails showing 90% or more and 99% or more viability decrement compared to the average number of fungi in the foot nails of the infected control group was calculated in each group (total 12 nail samples from 12 feet) and was defined as 90% and 99% efficacy rates, respectively. The Student’s t-test (one-tailed) was carried out at a significance level of 95% to compare viable fungal counts in the nails of infected controls in 4- and 8-week infection models. The Fisher’s exact test (one-tailed) was performed at a significance level of 95% for the differences in the efficacy rates of drugs in infection periods. JMP® 16 (SAS Institute Inc., Cary, NC, USA) was used for the analyses.
Measurement of Drug Concentration in Nails
After the drug was extracted by adding methanol to the nail homogenate, the drug concentration in the homogenate extracts (total 12 nail samples from 12 feet) were measured using liquid chromatography-tandem mass spectrometry (LC–MS/MS). The drug concentrations in the nail were calculated (μg/g nail). Then, the Student’s t-test (two-tailed) was performed at a significance level of 95% for the differences in the drug concentrations between treatment groups. JMP® 16 (SAS Institute Inc., Cary, NC, USA) was used for the analysis.
Results
In vitro Antifungal Activity Against Arthrospores of T. mentagrophytes and T. rubrum
The geometric mean MECs of efinaconazole for arthrospores of T. mentagrophytes and T. rubrum in RPMI 1640 medium with 20% keratin were 0.13 and 0.25 μg/mL, respectively (Table 1). The geometric mean MECs of luliconazole for these arthrospores were 0.13 and 0.25 μg/mL, respectively. Thus, the antifungal activities of the two drugs against arthrospores of the species were almost identical under 20% keratin condition.
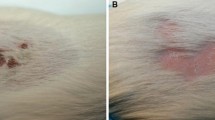
KOH Direct Microscopy and Histopathological Observation of the Infected Nails
Before treatment, many T. mentagrophytes were tightly present in the form of arthrospores in the nails in the 4-week infection model (Fig. 2a). Furthermore, at most sites of infection, many fungi (arthrospores and hyphae) infected the inside of the nail’s keratin layer (Fig. 2b).
T. mentagrophytes infected guinea pig nails. a KOH direct microscopic image: before the treatment, in the 4-week infection model, a part of the nails was lysed with 20% KOH, and the morphology of fungi in the nails was observed by light microscopy. Arrowheads indicate the observed fungi. b Histopathological observation: nail pieces were collected before the treatment in the 4-week infection model. Thin sections and Grocott’s staining were performed after fixation and demineralization and observed under a light microscope
Nail Fungal Burden of Infected Control Groups in 4-week and 8-week Infection Models
The viable fungal counts in the nails of the infected control group in 4- and 8-week infection models after the treatment period were 4.60 ± 0.26 and 4.94 ± 0.30 Log colony-forming unit in the nails/foot (mean ± SD), respectively. The number of viable fungi in the nails in the 8-week infection model was 2.3 times higher than that in the 4-week infection model, with a statistically significant difference (p = 0.0062).
Therapeutic Efficacy of Drugs in Both Infection Models
The 90% efficacy rates of the efinaconazole 10% solution groups in the 4- and 8-week infection models were 92% (11/12) and 75% (9/12), respectively (Fig. 3a). There was no statistically significant difference between the two infection models (p = 0.2950). The 99% efficacy rates of the efinaconazole 10% solution groups in the 4- and 8-week infection models were 50% (6/12) and 25% (3/12), respectively. There was no statistically significant difference between the two infection models (p = 0.2002). In contrast, the 90% efficacy rates of the luliconazole 5% solution groups in the 4- and 8-week infection models were 83% (10/12) and 42% (5/12), respectively (Fig. 3b), with a statistically significant difference between the two infection models (p = 0.0447). The 99% efficacy rates of the luliconazole 5% solution groups in 4- and 8-week infection models were both 0% (0/12), and the statistical analysis was not performed.
Efficacy rates of efinaconazole 10% solution and luliconazole 5% solution in guinea pig tinea unguium models. Nails were collected 1 week after the last treatment and homogenized using a glass homogenizer. The viable fungal count in the nails was calculated from the counts of colony-forming units present in the nail homogenates. The rates of nails showing 90% and 99% efficacy in each group (90% and 99% efficacy rates, respectively) were calculated. Ninety percent and 99% efficacy were defined as 90% or more and 99% or more reduction, respectively, in the viable fungal count compared to the average viable fungal count in the infected control group (12 nails per group). White bars indicate 90% efficacy rate, and gray bars indicate 99% efficacy rate. The numbers above the bars indicate the number of validated cases/total number of cases. *: p < 0.05 vs. the 4-week infection model (Fisher’s exact test). †: p < 0.05 vs. the luliconazole 5% solution (Fisher’s exact test)
In the 4-week infection model, there was no statistically significant difference between the 90% efficacy rates of efinaconazole 10% solution and luliconazole 5% solution groups (p = 0.5000), whereas the 99% efficacy rate of efinaconazole 10% solution was significantly higher than that of luliconazole 5% solution (p = 0.0069). In the 8-week infection model, the 90% and 99% efficacy rates of efinaconazole 10% solution were higher than those of luliconazole 5% solution (p = 0.1069 and p = 0.1087, respectively).
Drug Concentration in the Nails
In the 4-week infection model, the drug concentrations (mean ± SD) in the nails of efinaconazole 10% solution and luliconazole 5% solution groups were 1720 ± 1400 and 3290 ± 1040 μg/g nail, respectively (Table 2), with a statistically significant difference between the two drugs (p = 0.0049). In the 8-week infection model, the drug concentrations in the nails of efinaconazole 10% solution and luliconazole 5% solution groups were 3080 ± 1360 and 4160 ± 3160 μg/g nail, respectively (Table 2), with no statistically significant difference between the two drugs (p = 0.2878). There was a statistically significant difference between the concentrations of efinaconazole in the infection periods (p = 0.0242). In contrast, there was no statistically significant difference between luliconazole groups (p = 0.3738).
Discussion
Dermatophytes form arthrospores in the human nails and the stratum corneum of the human skin [18]. Arthrospore formation is believed to be primarily responsible for dermatophyte infection and transmission in humans [19]. In this study, animal tinea unguium models without immunosuppression were produced because the host immunity is concerned with the disease state formation, affecting the growth form of the fungus and localization in the nails [13, 14]. The fungal form and localization in the model have not been clarified in detail, and those were histopathologically examined in this study. The histopathological observation showed that most fungi in the nails of the guinea pig model were present in an arthrospore form, as reported in human nails [18]. Moreover, several fungi infected the nail plate rather than the nail’s surface. The pathological results of the nail were close to the finding, “sandwich sign” [20]; the fungus was confirmed between two zones of the cell layers in the stratum corneum of the patients with skin dermatophytosis. Therefore, this tinea unguium model was considered to be similar to a clinical-pathological condition in the infection form and dermatophyte localization. In addition, the arthrospores of T. mentagrophytes and T. rubrum were susceptible to efinaconazole and luliconazole at almost the same level, as reported in their susceptibilities to several other antifungals [21]. From these findings, the efficacy of drugs in this animal model using T. mentagrophytes was considered relevant to the clinical efficacy against human onychomycosis, primarily caused by T. rubrum.
Furthermore, since the efficacy of drugs on onychomycosis is affected by its severity, an animal onychomycosis model that can predict their clinical efficiency against moderate to severe human onychomycosis is deemed valuable. Therefore, a predictive guinea pig tinea unguium model was newly produced under the conditions discussed above with a stronger infection intensity than a previously reported model (4-week infection) [11, 12] by extending the infection duration to 8 weeks. As a result, in the infected control group, the viable fungal count in the nails of the 8-week infection model was significantly higher than that of the 4-week infection model, which implied that the fungi would have spread in the nails after 8 weeks of infection. Efinaconazole and luliconazole, which have the same mechanisms of action but different nail permeabilities and keratin affinities [10, 16], were evaluated in the models with different infection duration to investigate the effects of infection duration on the therapeutic efficacy of the drugs. The mean drug concentration in the nail of the 8-week infection model was slightly higher for luliconazole and siginificantly higher for efinaconazole than that in the nail of the 4-week infection model. The nail infection progression in the 8-week infection model compared to the 4-week infection model was speculated to reduce the drug penetration barrier function in the nail, resulting in an increase in the drug concentration in the nail. However, their efficacy against the tinea unguium model was lower in the 8-week infection model than in the 4-week infection model. These results suggested that the 8-week infection model is more resistant to topical antifungal therapy than the 4-week infection model because of its higher fungal burden.
Efinaconazole 10% solution showed therapeutic effects on the 4- and 8-week infection models (90% efficacy rates: 92% and 75%, 99% efficacy rates: 50% and 25%, respectively). Its efficacy rates in the 8-week infection model were slightly reduced compared with those in the 4-week infection model, but there was no statistically significant difference. On the other hand, luliconazole 5% solution showed therapeutic effects on the 4- and 8-week infection models with 90% efficacy rates of 83% and 42%, respectively. Its efficacy rate in the 8-week infection model was significantly lower than that in the 4-week infection model. The 99% efficacy rates of luliconazole 5% solution in the 4- and 8-week infection models were both 0%. In a phase III study, efinaconazole 10% solution was reported to have a 28.8% complete cure rate in a subpopulation analysis of Japanese patients with moderate DLSO (infected area: 20–50%) [22]. In a postmarketing clinical study of Japanese patients, the complete cure rate of efinaconazole 10% solution was 25.0% for patients with including severe DLSO (infected area > 50%) [23]. Also, there are reports that efinaconazole 10% solution exerted clinical efficacy against refractory onychomycosis [24, 25]. Alternatively, luliconazole 5% solution was reported to have a 14.9% complete cure rate in a phase III study of Japanese patients with moderate DLSO (infected area: 20%–50%) [26]. However, there are no clinical studies on the use of luliconazole 5% solution in patients with more severe onychomycosis. Considering the above reports, efinaconazole 10% solution’s high efficacy in clinical studies reflects its efficacy even in more refractory 8-week model in this study.
The drug’s therapeutic efficacy is determined by its permeability and antifungal activity in the nails [16, 27]. In this study, luliconazole showed equal or higher nail concentrations than efinaconazole, presumably because of its higher keratin affinity. Still, both drugs were detected in the nails at significantly higher concentrations than the MECs in a keratin-added medium. Conversely, efinaconazole 10% solution was highly effective in reducing the nail fungal burden, whereas luliconazole 5% solution showed no 99% efficacy rate. Therefore, the effectiveness of efinaconazole was thought to be due to their different characteristics because efinaconazole has a lower keratin affinity and higher human nail permeability than luliconazole [16, 27]. In addition, our recent study showed that there was a drug concentration gradient from the superficial to the internal part of the treated nails, and in the deeper nail layer, the antifungal activity and the amount of permeated efinaconazole were higher than those of permeated luliconazole [27]. Considering these, it was believed that efinaconazole 10% solution was more effective than luliconazole 5% solution in reducing the nail fungal burden and its therapeutic efficacy was less influenced by the duration of infection, which is unlikely with that of luliconazole 5% solution, presumably because efinaconazole reached the nail’s deep layer and killed the infecting fungi.
In conclusion, an tinea unguium model close to a clinical infection condition was newly developed with fungal burden increased by extending the infection duration. Considering the increased infection intensity and intractableness to drugs and the relevance of clinical studies, the new tinea unguium model would predict the drug’s efficacy against moderate to severe onychomycosis, leading to the development of new topical anti-onychomycosis drugs.
References
Gupta AK, Jain HC, Lynde CW, Macdonald P, Cooper EA, Summerbell RC. Prevalence and epidemiology of onychomycosis in patients visiting physicians’ offices: a multicenter Canadian survey of 15,000 patients. J Am Acad Dermatol. 2000;43:244–8. https://doi.org/10.1067/mjd.2000.104794.
Watanabe S, Harada T, Hiruma M, Iozumi K, Katoh T, Mochizuki T, Naka W. Japan Foot Week Group Epidemiological survey of foot diseases in Japan: Results of 30,000 foot checks by dermatologists. J Dermatol. 2010;37:397–406. https://doi.org/10.1111/j.1346-8138.2009.00741.x.
Drake LA, Scher RK, Smith EB, Faich GA, Smith SL, Hong JJ, Stiller MJ. Effect of onychomycosis on quality of life. J Am Acad Dermatol. 1998;38(5 Pt 1):702–4. https://doi.org/10.1016/S0190-9622(98)70199-9.
Tosti A, Elewski BE. Onychomycosis: Practical Approaches to Minimize Relapse and Recurrence. Skin Appendage Disord. 2016;2(1–2):83–7. https://doi.org/10.1159/000448056.
Gupta AK, MacLeod MA, Tosti A. Onychomycosis: clinical aspects. In: Rubin AI, Jellinek NJ, Daniel CR, Scher RK, editors. Scher and Daniel’s nails. Berlin, Germany: Springer; 2018. p. 153–9. https://doi.org/10.1007/978-3-319-65649-6_9.
Bang CH, Lee YB, Park HJ, Cho BK. Comparison of therapeutic efficacy between lateral type of distal and lateral subungual onychomycosis (DLSO) and non-lateral types of DLSO. Korean J Med Mycol. 2011;16(4):186–95.
Aggarwal R, Targhotra M, Kumar B, Sahoo PK, Chauhan MK. Treatment and management strategies of onychomycosis. J Mycol Med. 2020;30(2):100949. https://doi.org/10.1016/j.mycmed.2020.100949.
Tatsumi Y, Yokoo M, Senda H, Kakehi K. Therapeutic efficacy of topically applied KP-103 against experimental tinea unguium in guinea pigs in comparison with amorolfine and terbinafine. Antimicrob Agents Chemother. 2002;46(12):3797–801. https://doi.org/10.1128/AAC.00399-11.
Shimamura T, Kubota N, Nagasaka S, Suzuki T, Mukai H, Shibuya K. Establishment of a novel model of onychomycosis in rabbits for evaluation of antifungal agents. Antimicrob Agents Chemother. 2011;55(7):3150–5. https://doi.org/10.1128/AAC.00399-11.
Nakamura A, Hirakawa S, Nagai H, Inagaki K. A comparative study between two antifungal agents, Luliconazole and Efinaconazole, of their preventive effects in a Trichophyton-infected guinea pig onychomycosis model. Med Mycol. 2021;59(3):289–95. https://doi.org/10.1093/mmy/myaa111.
Tachibana H, Kumagai N, Tatsumi Y. Fungicidal activity in the presence of keratin as an important factor contributing to In vivo efficacy: a comparison of Efinaconazole, Tavaborole, and Ciclopirox. J Fungi. 2017;3(4):58. https://doi.org/10.3390/jof3040058.
Sugiura K, Sugimoto N, Hosaka S, Katafuchi-Nagashima M, Arakawa Y, Tatsumi Y, Jo SW, Pillai R. The low keratin affinity of efinaconazole contributes to its nail penetration and fungicidal activity in topical onychomycosis treatment. Antimicrob Agents Chemother. 2014;58(7):3837–42. https://doi.org/10.1128/AAC.00111-14.
Celestrino GA, Verrinder VJ, Benard G, Sousa MGT. Host immune responses in dermatophytes infection. Mycoses. 2021;64(5):477–83. https://doi.org/10.1111/myc.13246.
Burstein VL, Beccacece I, Guasconi L, Mena CJ, Cervi L, Chiapello LS. Skin immunity to dermatophytes: from experimental infection models to human disease. Front Immunol. 2020;11:605644. https://doi.org/10.3389/fimmu.2020.605644.
Cambier L, Heinen MP, Mignon B. Relevant animal models in dermatophyte research. Mycopathologia. 2017;182(1–2):229–40. https://doi.org/10.1007/s11046-016-0079-3.
Matsuda Y, Sugiura K, Hashimoto T, Ueda A, Konno Y, Tatsumi Y. Efficacy coefficients determined using nail permeability and antifungal activity in keratin-containing media are useful for predicting clinical efficacies of topical drugs for onychomycosis. PLoS ONE. 2016;11(7):e0159661. https://doi.org/10.1371/journal.pone.0159661.
Fujita S, Matsuyama T, Sato Y. A simple and reliable culturing method for production of arthrospores by dermatophytes. Jpn J Med Mycol. 1986;27(3):175–81. https://doi.org/10.3314/jjmm1960.27.175.
Brasch J, Hipler UC. Clinical aspects of dermatophyte infections. In: Brakhage AA, Zipfel PF, editors. Human and Animal Relationships. Berlin, Germany: Springer; 2008. p. 263–86. https://doi.org/10.1007/978-3-540-79307-6_13.
Hashimoto T, Blumenthal HJ. Factors affecting germination of Trichophyton mentagrophytes arthrospores. Infect Immun. 1977;18(2):479–86. https://doi.org/10.1128/iai.18.2.479-486.1977.
Gottlieb GJ, Ackerman AB. The “sandwich sign” of dermatophytosis. Am J Dermatopathol. 1986;8(4):347–50. https://doi.org/10.1097/00000372-198608000-00013.
Coelho LM, Aquino-Ferreira R, Leite CM, Martinez-Rossi NM. In vitro antifungal drug susceptibilities of dermatophytes microconidia and arthroconidia. J Antimicrob Chemother. 2008;62(4):758–61. https://doi.org/10.1093/jac/dkn245.
Elewski BE, Rich P, Pollak R, Pariser DM, Watanabe S, Senda H, Ieda C, Smith K, Pillai R, Ramakrishna T, Olin JT. Efinaconazole 10% solution in the treatment of toenail onychomycosis: two phase III multicenter, randomized, double-blind studies. J Am Acad Dermatol. 2013;68(4):600–8. https://doi.org/10.1016/j.jaad.2012.10.013.
Iozumi K, Abe M, Ito Y, Uesugi T, Onoduka T, Kato I, Kato F, Kodama K, Takahashi H, Takeda O, Tomizawa K, Nomiyama T, Fujii M, Mayama J, Muramoto F, Yasuda H, Yamanaka K, Sato T, Oh-I T, Kasai H, Tsuboi R, Hattori N, Maruyama R, Omi T, Shimoyama H, Sei Y, Nakasu I, Nishimoto S, Hata Y, Mochizuki T, Fukuzawa M, Seishima M, Sugiura K, Katayama I, Yamamoto O, Shindo M, Kiryu H, Kusuhara M, Takenaka M, Watanabe S. Efficacy of long-term treatment with efinaconazole 10% solution in patients with onychomycosis, including severe cases: a multicenter, single-arm study. J Dermatol. 2019;46(8):641–51. https://doi.org/10.1111/1346-8138.14935.
Noguchi H, Matsumoto T, Hiruma M, Asao K, Hirose M, Fukushima S, Ihn H. Topical efinaconazole: a promising therapeutic medication for tinea unguium. J Dermatol. 2018;45:1225–8. https://doi.org/10.1111/1346-8138.14575.
Kubota Y, Tatsukawa R, Inoue Y, Terawaki S, Shimizu H, Adachi M, Murao R. Efficacy of long-term treatment with efinaconazole 10% solution in patients with severe onychomycosis, including the examination by clinical type. Jpn J Dermatol. 2021;131(1):63–73. https://doi.org/10.14924/dermatol.131.63.
Watanabe S, Kishida H, Okubo A. Efficacy and safety of luliconazole 5% nail solution for the treatment of onychomycosis: A multicenter, double-blind, randomized phase III study. J Dermatol. 2017;44(7):753–9. https://doi.org/10.1111/1346-8138.13816.
Masumoto A, Takagi M, Sugiura K, Matsuda Y, Nakamura S, Tatsumi Y. A novel method for predicting the efficacy of topical drugs on onychomycosis: a comparison of efinaconazole and luliconazole. J Med Mycol. 2022;32(3):101259. https://doi.org/10.1016/j.mycmed.2022.101259.
Acknowledgements
The authors would like to thank Masahiro Satsukawa, Sadayoshi Furuta and Hisato Senda for discussion and review of the manuscript, and Toshiaki Okuda for supporting experiment.
Funding
Funding for this study was provided by Kaken Pharmaceutical Co., Ltd., Tokyo, Japan.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Akane Masumoto, Keita Sugiura, Yoshiki Matsuda and Haruki Tachibana. The first draft of the manuscript was written by Akane Masumoto and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors has the following conflict of interest: The authors are the employees and stockholders of Kaken Pharmaceutical Co., Ltd. Kaken Pharmaceutical Co., Ltd. discovered Clenafin/Jublia, a topical onychomycosis treatment product that contains efinaconazole. Clenafin and Jublia is commercialized in Japan by Kaken Pharmaceutical Co., Ltd and the United States/Canada by Bausch Health Companies Inc., respectively.
Ethical approval
The animal experiments were approved by the Animal Experiments Committee of Kaken Pharmaceutical Co., Ltd. and were conducted following the ethical rules for the conduct of animal experiments in Kaken Pharmaceutical, Co., Ltd (Approval No. K16-236 and K17-071).
Additional information
Handling Editor: Koichi Makimura.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Masumoto, A., Sugiura, K., Matsuda, Y. et al. Evaluation of Topical Antifungals Using a New Predictive Animal Model for Efficacy against Severe Tinea Unguium: A Comparison of Efinaconazole and Luliconazole. Mycopathologia 187, 481–489 (2022). https://doi.org/10.1007/s11046-022-00664-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-022-00664-3