Abstract
Developing drug delivery carriers for highly selective, controlled, and sustained release of the anti-cancer drugs is one of the crucial issues in the cancer strive. We herein report the synthesis of Fe3O4 (M) and SiO2 (S) nanoparticles and their nanocomposites with chitosan (CS) for high loading efficiency and subsequent release potentiality of Doxorubicin (DOX) anticancer drug. The as-synthesized nanostructures were characterized using Fourier transform infrared (FT-IR), X-ray diffraction (XRD), field emission scanning electron microscopy (FE-SEM), high-resolution transmission electron microscopy (HR-TEM), and thermal analysis techniques. The average crystallite sizes of the as-prepared M, S, CS/M, CS/S, and CS/M/S nanostructures were found to be 5, 15, 70, 22, and 29 nm, respectively. The loading and cumulative release of Doxorubicin for the produced nanostructures were examined, and the results exhibited loading efficacy of 71%, 95%, 96%, 79%, 17%, and 42% for M, S, CS, CS/M, CS/S, and CS/M/S nanostructures, respectively. The Doxorubicin releasing results revealed a promising cumulative release percentages at pH 4.2 and pH 5 compared with those at pH 7.4. At pH 4.2, the cumulative release percentages for DOX-M, DOX-S, DOX-CS, DOX/M, and DOX/CS/M/S were 94%, 96%, 92%, 95%, and 98%, respectively. While the corresponding percentages at pH 5 were 97%, 90%, 46%, 43%, and 70%. The percentage for DOX-CS/S was 60% at pH 5, though. The in-vitro cytotoxicity of M-DOX, CS-DOX, and M/CS-DOX was explored against two human cancer cell lines (MCF-7 and Hep-G2) using SRB (Sulforhodamine B) assay. The DOX-loaded M/CS exhibited the highest cytotoxicity and its IC50 values were 2.65 and 2.25 μg/mL against Hep-G2 and MCF-7 cell lines, respectively, compared to the corresponding values of 5.1 and 4.5 μg/mL for free DOX. The results indicated that M/CS nanocomposite is a good candidate as drug delivery nano-carrier for the Doxorubicin anti-cancer drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The incorporation of nanotechnological tools in medicine represents promising approaches to the diagnosis and treatment of many human health conditions, especially cancer therapy [1,2,3,4,5,6,7,8,9]. This is attributed to the unique physicochemical properties of nanomaterials such as easy surface functionalization, a large surface-to-mass ratio, and quantum characteristics [10,11,12,13]. The World Health Organization (WHO) reported that the mortality rate caused by cancer is ranked second after heart disease [14]. The most widely spreading cancer case among women is breast cancer; it is responsible for 16% of entire tumors [15]. Whereas, the human hepatic malignant is the third reason of cancer-correlated mortality, and the fifth most common tumor all-inclusive [16]. There are different types of treatment protocols for cancers, and the most commonly used protocol is chemotherapy. However, this protocol has some difficulties such as highly toxic side effects, lack of selectivity for malignant cells, the short lifetime of the drugs, and a large portion of the wasted drug [17]. Doxorubicin (DOX) is an anthracycline antibiotic considered one of the most successful drugs worldwide. It is mostly used as a chemotherapeutic drug for various cancers such as leukemia, breast cancer, ovarian, lung, solid tumors, bladder, and soft-tissue sarcomas [18,19,20]. Despite its efficacy and success in treating different kinds of tumors, there are several side effects associated with its use that limit its function such as nausea and vomiting, stomatitis, baldness, gastrointestinal disturbances, neurologic disturbances, bone marrow aplasia, and cumulative cardiotoxicity [21], as well as fast releasing due to resistance of cancer cells to drugs [22].
The application of nanomaterials as a drug carrier for Doxorubicin to target tumor cells is one of the most crucial methods to overcome Doxorubicin drawbacks and reduces the adverse side effects [23]. The effectiveness of nanomaterials as drug carriers is significantly influenced by biocompatibility, biodegradability, particle size, surface area, surface charge, particle charge, and hydrophilicity [24]. The mechanism of the drug delivery depends mainly upon targeting specific cells; therefore, many drugs are loaded on nanocarriers due to their easy penetration through different membranes and attaching to proteins of diseased cells [25]. In this light, silicon dioxide nanoparticles have been widely used in drug delivery applications due to its unique properties such as large surface area, minimal residual magnetism, lack of toxicity, biodegradability, biocompatibility, and its ease of production [26, 27]. In addition, magnetite nanoparticles (Fe3O4), which have an inverse spinel crystal structure [28], have recently attracted attention of several research groups due to their distinctive chemical and physical characteristics which make them appropriate for several applications [24, 29]. Magnetic resonance imaging (MRI), tissue engineering, hyperthermia, and drug delivery are among the most valuable biomedical applications of Fe3O4 nanoparticles [24, 30, 31]. Due to their high surface area, adjustable particle size, and promoted magnetic characteristics, magnetite nanoparticles are highly desirable for drug delivery applications because they are easily directed by an external magnetic field [32, 33]. The magnetic liquid in the body is produced by the particle-drug system and the drug consequently can be targeted directly to the specific area by applying an external magnetic field to control biodistribution and optimize the accumulation of the drug dose into the malignant interstitium [34, 35]. The primary drawback of employing magnetite NPs as drug nanocarriers is that they can interact with plasma proteins in the circulatory system, which causes them to be quickly eliminated via the reticuloendothelial system (RES) before reaching the target site [34, 35]. Therefore, magnetite nanoparticles should be protected via coating with biocompatible polymers such as polysaccharides or polyethylene glycol (PEG) to fabricate a core–shell modified system with the presence of magnetic characteristics of the core. The polymeric shell gives the nanoparticles a surface charge, prevents agglomeration, improves the stability of the nanoparticles during circulation, and controls the release of anticancer drugs at the targeted sites [36].
In recent years, polymers have been widely employed as drug conjugates to develop efficient drug carriers or drug delivery systems. Depending on the preparation process, the drug is either covalently attached to the polymer or physically trapped inside it [37]. Chitosan is a polysaccharide, the second naturally abundant biopolymer [38], and is the deacetylated derivative of chitin. Chitosan has high mechanical strength and has susceptibility to chemical modifications, and it has been widely used in the biomedical field such as drug delivery, due to its cationic character, adhesivity to mucous, its biocompatibility with living tissues, biodegradability, and non-toxicity [39]. It can be also easily degraded by a large number of enzymes and the products of degradation are nontoxic, and solubility in an acidic medium like tumor environment [40, 41]. To further improve delivery efficacy and malignancy selectivity, chitosan-based NPs with active tumor-targeting capability have undergone extensive development. Additionally, one method for overcoming Fe3O4’s aforementioned drawbacks and taking advantage of Fe3O4, SiO2, and chitosan, is to synthesize tunable particle-size nanocomposites made of these nanomaterials as drug delivery nano-carriers for Doxorubicin. Due to the existence of a magnetic moiety in the form of magnetite nanoparticles, the therapeutic and antibacterial capabilities of chitosan, and the porosity of SiO2, these nanocomposites can be a good candidate for treating cancer by using hyperthermia and an external magnetic field and having high efficiency as Doxorubicin nano-carriers. Therefore, in the present work, we synthesize various nanomaterials including Fe3O4, SiO2, and chitosan as well as their nanocomposites using low-cost, simple, time-saving, and eco-friendly procedures. The as-prepared nanomaterials were characterized using different techniques such as FT-IR, XRD, TGA, DTA, DSC, SEM, and TEM. We also investigated the in-vitro cumulative release profile of Doxorubicin-loaded nanomaterials at different pH values to mimic the normal physiological and tumoral environments and at the temperature of ~ 37 °C to determine the releasing behavior of the candidate DOX-nanocarriers. Sulforhodamine B (SRB) technique was employed in the in-vitro cytotoxicity evaluation of as-fabricated Doxorubicin nanocarriers against human breast (MCF7) and hepatic (Hep-G2) cancer cell lines were performed for comparison of cytotoxicity of Doxorubicin alone and its loaded nanocarrier formulations, and the morphological changes in hepatic and breast cancer cells after exposure to these nano-formulations were also observed.
2 Materials and Methods
2.1 Chemicals and Reagents
All chemicals used were of analytical grade and used without further purification. Ferric nitrate and ammonium ferrous sulfate were obtained from ALFA CHEMIKA (India). Sodium hydroxide was supplied by LOBAL CHEMIE (India) for the synthesis of magnetite nanoparticles. Silica-gel 60/120 mesh [for cc] was purchased from ALFA CHEMIKA (India), and hydrochloric acid HCl from ADWIC (El-Nasr pharmaceutical chemicals company, (Egypt) for the synthesis of silicon dioxide nanoparticles. Chitosan of high molecular weight, white powder, 81.2% deacetylated, viscosity: 3600 cps, density: 0.15 g/mL, particle size: 95% purity was purchased form Sigma-Aldrich (Germany). Glutaraldehyde, acetic acid, and absolute ethanol from ADWIC-company (Egypt) for the synthesis of chitosan nanocomposites. Doxorubicin hydrochloride was purchased from HIKMA Specialized pharmaceuticals (Egypt). Hep-G2 (liver carcinoma cell line) and MCF-7 (breast carcinoma cell line) were obtained from VACSERA, Cairo, Egypt. The water used in all experiments was deionized H2O.
2.2 Experimental Procedures
2.2.1 Magnetite Nanoparticles (M)
Magnetite nanostructure synthesis was conducted by using a co-precipitation method. Two different iron salts; ferric nitrate (4 g, 9.9 mmol) and ammonium ferrous sulfate (2 g, 5 mmol) were dissolved in 30 mL of distilled water. The molar ratio of iron sources Fe3+:Fe2+ was 2:1. Sodium hydroxide (6 g, 150 mmol) was dissolved in 30 mL distilled H2O. The applied quantities so as the molar ratio of [Fe3+/Fe2+]:NaOH was 1:10. The prepared iron solution, after mixing and magnetic stirring, was then added dropwise to the prepared NaOH solution. The pH value of the reaction mixture was about 10, after the complete addition. The reaction blend was heated at 100 °C for 3 h with stirring. The formed black precipitate was separated by decantation with the help of a magnet and washed with distilled water several times to remove unwanted products, and dried in an oven at 80 °C overnight.
2.2.2 Silicon Dioxide Nanoparticles (S)
Silicon dioxide (SiO2) nanoparticles were prepared by the sol–gel method. NaOH sodium hydroxide (3.2 g, 80 mmol) was dissolved in 40 mL distilled H2O, then (2.4 g, 40 mmol) SiO2 silica gel, 60:120 mesh (for cc) was added. The mixture was magnetically stirred at 70 °C to obtain a homogeneous solution. The solution was allowed to get the room temperature and to which an aqueous solution of hydrochloric acid (1 M HCl) was dropwise added. A colorless gel-like precipitate was formed at pH ca. 9 but the addition of the hydrochloric acid solution was continued to pH ~ 6. Then the precipitate was washed five times with distilled water, then dried in an electric oven at 80 °C overnight. The produced white precipitate was transferred to a porcelain crucible and calcined in a muffle furnace at 850 °C for 3 h.
2.2.3 Preparation of Magnetite, Silicon Dioxide, and Chitosan Nanocomposites
The magnetite/chitosan (M/CS) nanocomposite was synthesized as follows: 0.5 g chitosan was dissolved in 100 mL (5%, v/v) acetic acid solution. To this solution, the as-prepared magnetite nanoparticles (0.25 g) were added and stirred for 30 min and ultra-sonicated, using Hielscher ultrasonic processor-up 400 s at amplitude 70%, for 15 min. Afterward, the cross-linking method was carried out in situ by dropwise addition of 1 mL glutaraldehyde (GL) as a cross-linker to the previously stirring blend. The blend was dried at 60 °C for 6 h, then washed with distilled water five times and with ethanol twice. Then, the precipitate was dried at 60 °C overnight to obtain a dried powder of magnetite/chitosan (M/CS) nanocomposite. Similar procedure was applied using chitosan, as-prepared magnetite (0.25 and 0.125 g for M/CS and CS/M/S, nanocomposites, respectively), and as-prepared silicon dioxide (0.25 and 0.125 g for S/CS and CS/M/S, nanocomposites, respectively) to synthesize silicon dioxide/chitosan (S/CS) and chitosan/magnetite/silicon dioxide (CS/M/S) nanocomposites. Scheme 1 presents the outlines of the preparations methods and applications of the nanomaterials of interest.
2.2.4 Doxorubicin Loading on the Synthesized Nanomaterials
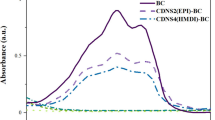
Loading of Doxorubicin (DOX) on the as-synthesized nanomaterials was carried out using the same initial DOX concentration to compare their loading capacities and efficiencies. As such 1 mg/mL of Doxorubicin in distilled water was prepared and its concentration was measured by using a UV–Vis spectrophotometer. The anticancer drug (Doxorubicin) with a fixed concentration was mixed individually with a fixed weight of the synthesized nanostrucutres (0.1 g of each) at room temperature in a light-protected, brown vial to avoid the drug decomposition. The suspension was stirred for 24 h at 300 rpm in the dark. After that, the suspension was centrifuged and the absorbance of the supernatant was measured by the UV–Vis spectrophotometer at wavelength 480 nm (λmax of Doxorubicin) to calculate the drug loading efficiency (LE) percentage using Eq. (1).
2.2.5 Doxorubicin In-Vitro Release Studies
The in-vitro cumulative release of Doxorubicin from Doxorubicin-loaded nanomaterials was determined in phosphate buffer solution (PBS) at different pH values of 4.2, 5, and 7.4 in light-protected tubes at 37 °C. The drug released from nanomaterials was calculated by measuring the absorbance of Doxorubicin in the supernatant at 480 nm by using the UV–Vis spectrophotometer. Quantification of Doxorubicin was performed by generating a calibration curve by known amounts of DOX drug concentrations.
2.2.6 In-Vitro Cytotoxicity Evaluation
The in-vitro cytotoxicity was evaluated for three selected DOX-load nanocomposites: magnetite-DOX, chitosan-DOX, and magnetite/chitosan-DOX, separately in synchronization with the in-vitro cytotoxicity evaluation of DOX alone. The in-vitro cytotoxicity was evaluated against two human cell lines; Hep-G2 (liver carcinoma cell line) and MCF-7 (breast carcinoma cell line). These cells were maintained in RPMI-1640 medium supplemented with 100 µg/mL penicillin, 100 µg/mL streptomycin, and 10% heat-inactivated fetal bovine serum (FBS). These cells were grown at 37 °C in a 5% CO2 humidified atmosphere [42]. Cell viability has been assessed by SRB assay (Sulforhodamine B assay). Aliquots of 100 μL cell suspension ~ (5 × 103 cells) were seeded in 96-well plates and incubated in complete media for 24 h. Cells were treated with another aliquot of 100 μL media containing drug (M-Dox, CS-Dox, M/CS-Dox, and free DOX) at various concentrations ranging from (0.01, 0.1, 1, 10, and 100 μg/mL) after 72 h of drug exposure, cells were fixed by replacing media with 150 μL of 10% TCA and incubated at 4 °C for 1 h. The TCA solution was removed, and the cells were washed five times with distilled water. An aliquot of 70 μL SRB solution (0.4% w/v) was added and incubated in a dark place at room temperature for 10 min. Plates were washed three times with 1% acetic acid and allowed to air-dry overnight. Then, 150 μL of TRIS (10 mM) was added to dissolve the protein-bound SRB stain; the absorbance was measured at 540 nm using a BMG LABTECH-FLUO star OMEGA microplate reader (Ortenberg, Germany).
2.2.7 Characterization of Nanoparticles and Chitosan Nanocomposites
The structure of the synthesized products was characterized using x-ray diffraction (XRD), collected by an 18 kW diffractometer (Bruker; model D8 advance) with monochromator Cu-Ka radiation (1.54178 Å). Fourier transform infrared (FT-IR) spectra were obtained by using an FT-IR spectrometer (Thermo Fisher-Nicolet IS10) from 4000 to 400 cm−1 at room temperature. Scanning electron microscopy (SEM) images were captured by using a field emission electron microscope (FE-SEM) with a microscope (JEOL JSM-6500F). Transmission electron microscopy (TEM) images were taken by electron microscope (JEM 2100) at an accelerating voltage of 200 kV; where the sample was dispersed in ethanol on a copper grid. UV–Vis spectra of Doxorubicin drug were collected by using a Jasco UV–Vis spectrophotometer (Jasco; model v670), SRB assay (Sulforhodamine B assay) for the cytotoxicity evaluation study. The stained cells were examined using an inverted microscope (Olympus opticals, Japan). The thermal analysis (TGA and DSC) measurements were performed on a thermal analyzer instrument (Shimadzu; model TA-60WS) with 10 °C/min heating rate under airflow.
3 Results and Discussion
3.1 X-Ray Diffraction
The X-ray diffraction patterns of the as-prepared nanomaterials were depicted in Fig. 1. The characteristic peaks of the as-prepared magnetite were observed at 2θ values of 30°, 35°, 43°, 54°, 57°, and 62° for crystalline planes of (220), (311), (400), (422), (511), and (440) with lattice spacing d and lattice parameters a°, as shown in Table 1. The position and relative intensity of the peaks of the XRD pattern matched well with the standard magnetite samples [43], and according to space group Fd-3m, ICSD file No. 01-089-0688, this data demonstrated that the as-prepared magnetite (M) sample has an inverse spinel structure with a face-centered cubic phase (Fig. 1a).
The average crystallite of the as-prepared magnetite nanoparticles was estimated to be 5 nm using the Debye–Sherrer equation (Eq. (2)) [44]. The crystallite size of the as-prepared Fe3O4 nanoparticles is lower than those published elsewhere [45].
where D is the crystallite size (nm), k is a constant = 0.9, λ is the wavelength of radiation = 1.54060 Å (in the case of Cu Kα), β is the full width of half maximum of the strongest peak (FWHM) in the radian, and θ is the diffraction angle in radian. It is worth mentioning that the mechanism of the formation of the magnetite can be explained as follows: at high pH values, ferrous hydroxide precipitates, and then this precipitate may undergo dissolution, forming FeOH+. This species may undergo slow oxidation in air, and then in alkaline aqueous media, it may be converted into magnetite. The reaction mechanism for the formation of Fe3O4 can probably be expressed as follows:
In addition, the XRD pattern of the as-prepared silica nanoparticles (S) is depicted in Fig. 1b. This XRD pattern revealed reflection peaks at 2θ of 21.8°, 28.2°, 31.2°, 35.9°, 55.2°, and 58.3°, indexed to (101), (111), (102), (316), (130), and (222) crystal planes, respectively, due to pure silica nanoparticles with tetragonal crystal structure cristobalite with space group P41212 and ICSD card no 01-082-0512 [46]. The XRD pattern also exhibited reflection peaks at 2θ of 20.5° and 23.2°, which could be indexed to (112) and (006) crystal planes, respectively, of monoclinic crystal structure tridymite with space group Cc and ICSD card no 01-071-0032 [47]. The determined average crystallite size of silica nanoparticles was 15 nm. The reaction mechanism for the formation of SiO2 nanoparticles can be proposed as follows:
On the other hand, the XRD patterns of the as-prepared CS/M and CS/M/S nanocomposites (Fig. 1c, e), revealed no certain diffraction peaks due to the presence of chitosan polymer coating the nanoparticles, and then these nanocomposites have mainly an amorphous nature. However, the XRD pattern of the CS/S nanocomposite Fig. 1d revealed diverse silica characteristic peaks at 2θ of 20.8°, 26°, and 50° corresponding to quartz crystal form, as well as reflection peaks at 2θ of 21.5° and 25.5° attributing to cristobalite crystal. However, the average crystallite size of CS/S composite nanoparticles was found to be ca. 22 nm.
3.2 Thermal Analysis of the As-Prepared Silica Nanoparticles
Thermal analysis is an important technique to confirm the composition of as-prepared silica nanoparticles and their thermal stability. The thermal behavior of silica nanoparticles was elucidated using TGA, DTA, DSC, and DTG analysis (Fig. 2). The obtained results revealed that the silica nanoparticles have three mass loss steps in the temperature ranges: ≤ 200 °C, 200–400, and 400–1000 °C, respectively. According to the TGA curve, the first step (mass loss of 4.23%) is attributed to the removal of hygroscopic water molecules [48]. The second and third decomposition steps are overlapped. The second step (mass loss of 0.82%) is mostly related to the condensation of silanol groups (S–OH) into siloxane bridges (Si–O–Si) and evaporation of H2O molecules. As the temperature increases, the loss of weight was continued despite the evaporation of water, so the mass loss of 2.39% in the range of 400–1000 °C can be attributed to further formation of Si–O–Si bonds via self-condensation, and dehydration of water molecules evaporation [49].
The investigation of the DTG curve showed three peaks. The first peak at about 60 °C, which accounted for physically adsorbed water elimination. The second and third broad peaks at ca. 400 and 800 °C, respectively, which accounted for the elimination of hydrogen-bonded hydroxyl groups from silica surface and from evaporation of H2O molecules due to the condensation of silanol groups (S–OH) into siloxane bridges (Si–O–Si). Inspection of DTA thermogram revealed the presence of three peaks at 60, 700, and 900 °C. The first peak is probably due to the elimination of physically surface adsorbed water molecules. The second and third peaks are attributed to evaporation of water molecules due to the condensation of silanol groups (S–OH) into siloxane bridges (Si–O–Si). These data are in consistent with the obtained DTG data. On the other hand, the DSC curve showed also three peaks due to the aforementioned reasons. These results are in good agreement with those of DTA curve. It could be concluded from the TGA, DTA, and DSC analysis that the optimum decomposition temperature of the precursor of SiO2 is ≥ 800 °C. These data are consistent with our published data elsewhere [49].
3.3 Fourier Transforms Infrared (FT-IR) Analysis
FT-IR spectra of the as-prepared nanostructures before and after Doxorubicin loading are displayed in Figs. 3 and 4. Magnetite nanoparticles (Fig. 3a) exhibited vibrational bands at 434, 570, and 630 cm−1, which were characteristic of magnetite nanoparticles [24, 45]. The band that appeared at 570 cm−1 could be assigned to the stretching vibration of the Fe‒O functional group [50, 51]. The band at 630 cm−1 is probably due to the octahedral vibrational matrix [52]. While the SiO2 spectrum (Fig. 3b) revealed all bands characteristic of SiO2 nanoparticles. The absorption bands at 470 and 797 cm−1 are related to the stretching vibrations of Si‒O‒Si [49]. The band at 1101 cm−1 is related to Si‒O‒Si asymmetric fluctuation [53, 54]. The absorption band at 2000 cm−1 corresponds to the silica matrix skeletal vibrations [55]. The FT-IR spectrum of bare chitosan is shown in (Fig. 3c), where strong broadband appeared at 3433 cm−1 corresponding to N‒H and O‒H stretching vibrations, as well as the intramolecular hydrogen bond [24]. The bands at 2923 and 2855 cm−1 were attributed to the C‒H stretching of chitosan. The bands at 1647 and 1425 cm−1were corresponding to N–H bending vibration, and C‒N stretching vibration, respectively. While, the bands at 1157, 1080, and 1035 cm−1 were due to C‒O‒C and C‒O stretching vibrations [24].
The spectrum of chitosan-coated magnetite nanocomposite (Fig. 3d) showed a significant shift in the vibrational frequencies of pure chitosan after mixing with magnetite nanoparticles. The band corresponding to N‒H bending vibration at 1647 cm−1 disappeared upon the formation of chitosan-coated magnetite nanocomposite and a new band appeared at 1633 cm−1 attributed to imine C=N stretching, which confirmed the reaction between glutaraldehyde (crosslinker) and chitosan [24]. C‒N stretching vibration was shifted from 1425 to 1411 cm−1. In addition, the spectrum showed also the presence of magnetite characteristic bands at 563 and 450 cm−1. While the FT-IR spectrum of the synthesized chitosan-silica nanocomposite (Fig. 3e) showed bands at 1635 and 1411 cm−1 corresponding to C=N and C–N stretching vibration, respectively. Besides, the spectrum exhibited an intensive absorption band at 1107 cm−1 due to the Si–O stretching vibration [49]. The FT-IR spectrum of chitosan/magnetite/silica nanocomposite is shown in (Fig. 3f). The bands assigned to C=N bending and C‒N stretching appeared at 1628 and 1422 cm−1, respectively. While the characteristic strong band at 1101 cm−1 in bare silica related to the asymmetric fluctuation of Si‒O‒Si appeared as a medium band at 1110 cm−1 for CS/M/S nanocomposite. The band at 570 cm−1 corresponding to Fe‒O vibration in bare magnetite appeared as a shoulder at 580 cm−1 in the spectrum of CS/M/S nanocomposite. Moreover, the octahedral vibrational matrix band of magnetite was shifted to 618 cm−1 compared with pure magnetite. It is worth mentioning that the driving force governing the formation of CS/M is the electrostatic attraction, while in the acidic medium, the positive charges generated by protonation of the amino groups of chitosan on the surface of magnetite nanoparticles enable chitosan to adsorb easily onto Fe3O4 as a shell [56]. But the driving force governing the formation of CS/S is the tendency of chitosan which bearing functional groups to form hydrogen bonds with silica as interfacial interaction [24].
The IR spectrum of Doxorubicin has multiple bands at 3331 (N–H stretch); 3525 (O–H stretch); 2935 and 2897 (C‒H stretch); 1729 (C=O stretch); 1617, 1582, and 1414 (C=C ring stretch); 1115 and 1073 (C‒O–C stretch); and 805, 688 cm−1 (C=H bend) and (C=C ring bend) [57]. These bands are also found in the FT-IR spectrum of the loaded Doxorubicin on the as-prepared nanomaterials. For the FT-IR spectrum of Doxorubicin-loaded magnetite (Fig. 4a), the bands at 2935 cm−1 of C‒H stretching and 1730 cm−1 of C‒O stretching disappeared, but the other bands were shifted to 1635 and 1561 cm−1 (N–H); 1412 cm−1 (C‒C); and 1021 cm−1 (C‒O). And the spectrum showed the presence of magnetite by observing its characteristic bands at 633, 587, and 440 cm−1. While the FT-IR spectrum of Doxorubicin-loaded silica nanoparticles (Fig. 4b) showed bands at 1577 (N‒H) and 1070 cm−1 (C‒O), which were shifted to 1561 cm−1 and 1099 cm−1, respectively. The vibrational bands of Si‒O‒Si of bare silica appeared at 797 and 470 cm−1 were slightly shifted to lower frequencies at 790 and 478 cm−1, respectively. The FT-IR spectrum of Doxorubicin-loaded chitosan (Fig. 4c) showed Doxorubicin multiple characteristic bands at 2926 cm−1 (C‒H); 1638 and 1563 cm−1 (N‒H); 1414 cm−1 (C‒C); and 1022 cm−1 (C‒O). Notably, this loaded chitosan showed the characteristic bands of the bare chitosan at 3428, 1346, and 772 cm−1 with slight shifts. On the other hand, the FT-IR spectrum of Doxorubicin-loaded nanocomposites: Dox-CS/M, Dox-CS/S, and Dox-CS/M/S (Fig. 4d–f), revealed the same characteristic bands of free nanocomposites with a slight shift in the vibrational frequencies. Additionally, the broadness of the band that appeared around 3400 cm−1 might be attributed to hydrogen bonding between the OH group of chitosan and the Doxorubicin drug [58]. These results indicate that Doxorubicin was successfully loaded onto the as-prepared nanomaterials. It is worth mentioning that the vibrational frequencies of the physically surface adsorbed water molecules on the as-prepared nanoparticles also contributed to the broadness of the bands that appeared at ca. 3400 cm−1 [59, 60].
Regarding glutaraldehyde, the FT-IR spectrum of the as-fabricated chitosan nanocomposites revealed that the glutaraldehyde characteristic bands [24] at 2850 and 2750 cm−1 of C‒H stretching are related to aldehydes. Besides, the strong bands from the carbonyl group at 1720–1740 cm−1 disappeared, which means no excess of glutaraldehyde present in the as-prepared chitosan nanocomposites.
3.4 Morphological Studies
The morphologies of the as-prepared nanostructures were investigated by using TEM and SEM techniques. TEM images (Fig. 5a) of the synthesized magnetite nanoparticles exhibited that the product is composed of uncompleted hexagonal-shaped, irregular-shaped, and spherical particles with an average particle size of ca. 5 nm, which is in good agreement with the calculated size from XRD data. The image also revealed little agglomerations of the particles. The TEM image of as-prepared silica nanoparticles (S) (Fig. 5b) exhibited that the SiO2 product consists of spherical and irregular morphology with an average particle size of ca. 15 nm which is consistent with XRD results. While the TEM image of chitosan/magnetite/silica nanocomposite (Fig. 4c), revealed that the nanocomposite is composed of semi-spherical and irregular particles with an average size of 29 nm. A deep inspection of the TEM image of as-prepared CS/M/S nanocomposite showed distinctive differences between the distribution of silica and magnetite nanoparticles inside and on the surface of chitosan sheets.
On the other hand, the SEM technique of the products shed more light on their surface morphology. The FE-SEM (Fig. 6a) of the as-prepared magnetite showed the product consists of uniform spherical particles with an average grain size of ca. 50 nm. The FE-SEM image (Fig. 6b( of the synthesized silica nanoparticles exhibited that the product was composed of spherical and peanut-shaped particles with grain size in the range of 0.5 µm. The FE-SEM image of the as-prepared CS/M nanocomposite (Fig. 6c) exhibited the full encapsulation of the spherical magnetite nanoparticles with chitosan. The average grain size of the coated magnetite nanoparticles was ca. 70 nm, which was greater than that of pure magnetite (50 nm). Figure 6d displays the FE-SEM image of the synthesized (CS/S) nanocomposite. This image revealed the agglomeration of silica nanoparticles on the chitosan sheets' surfaces. However, the FE-SEM image (Fig. 6e) of the CS/M/S nanocomposite showed that the magnetite nanoparticles were embedded inside the chitosan sheets, but silica nanoparticles were concentrated more on the chitosan sheet surfaces.
3.5 Doxorubicin Loading Study
The purpose of this investigation was to eliminate or decrease the adverse side effects of the Doxorubicin anticancer drug and increase its efficiency. Therefore, for this purpose, we prepared various nanomaterials. The Doxorubicin loading efficiency and releasing profile for the synthesized nanostructures and their chitosan nanocomposites are one of the main issues for this study. The drug loading process of the as-prepared nanomaterials was carried out overnight using Doxorubicin solutions of fixed concentration (100 μg/mL) at pH 7 and room temperature. The Doxorubicin loading efficiency percentages for (M), (S), (CS), (CS/M), (CS/S), and (CS/M/S) were 71%, 95%, 96%, 79%, 17%, and 42%, respectively, as presented in Fig. 7. According to the above results, CS/S nanocomposite showed poor loading efficiency, which might be attributed to an agglomeration of silicon dioxide on the surface of chitosan as deduced from its SEM, and TEM morphological analysis.
3.6 Doxorubicin In-Vitro Cumulative Release Study
The in-vitro cumulative drug release was estimated for the prepared drug-loaded nanostructures. The withdrawn sample for measuring after intervals of time was replaced with the same volume of fresh buffer (phosphate buffer solution (PBS) at different pH values of 4.2, 5, or 7.4 at ~ 37 °C). The concentration of the released drug was determined at a wavelength of 500 nm using a UV–Vis spectrophotometer in this study. The calibration curve was constructed to calculate the released drug concentrations, and the following linear equation was obtained.
where y is the obtained absorbance, and x is the concentration. Besides, m and b are the slope and intercept, respectively. Therefore, the drug concentration and amount of released drug were calculated using Eqs. (9) and (10), respectively.
The amount of drug encapsulated in nanomaterials immersed in buffer solution must be known to calculate the release and cumulative release precentages at sampling time t, using Eqs. (11) and (12), respectively.
where pt = percentage release at time t and p(t − 1) = percentage release previous to t.
Doxorubicin drug cumulative release profile was investigated at 37 °C and performed in a phosphate buffer solution at different pH values: 7.4, 5, and 4.2, which mimic physiological fluid of tumor environment and endosomal conditions, respectively [61], within 96 h. The acidic medium in tumor cells was generated by the anaerobic glucose metabolism and lactic acid was produced due to glycolysis from the cytosol in malignant cells because of the inadequacy of the oxygen/nutrient stream [37]. From releasing profile study, it can be seen that Doxorubicin release was the highest at pH 4.2 and 5 compared with that at pH 7.4. Hence, at low pH values, pH-responsive chitosan nanocomposites and nanoparticles release their Doxorubicin cargo in the acidic microenvironment of tumor tissues higher than neutral or normal cells. The Doxorubicin cumulative release percentages were summarized in Table 2. The cumulative release profiles were depicted in Fig. 8. It is worth mentioning that the drug releasing might take place in two stages: (1) the burst release by diffusion of the drug, which is precipitated on the surface of the as-prepared nanomaterials for the first time, and (2) the sustained release, which is the second step as the time increases. In the case of release of Doxorubicin from the as-prepared magnetite nanoparticles, the DOX was bound covalently to the surface of magnetite, via chelation with Fe2+ in the Fe3O4 molecule. The weak acidic medium might then induce the cleavage of the chemical bond between DOX and magnetite molecule, leading to the liberation of DOX into the dissolution media, so that, the burst release was acquired [62]. But the DOX loaded onto silica nanoparticles released under acidic conditions might be attributed to the increased solubility of Doxorubicin and diffusion as a consequence from the carrier pores to the acidic environment [63]. This discussion illustrates the burst release of DOX from magnetite and silica nanoparticles for the first time in addition to the precipitated DOX on the surfaces of M and S nanoparticles. On the other hand, DOX was loaded on CS due to the interaction between the functional carbonyl group of DOX and the amino group of CS. Hence, an imine bond was formed, and the DOX was diffused due to the increased pore sizes as a consequence of the enhanced swelling characteristics and protonation of its functional amine groups under acidic conditions. However, in the case of CS/M, CS/S, and CS/M/S nanocomposites, the cross-linked bonds have high chemical stability at pH 7.4, but these bonds can be degraded in acidic pH values in a sustained manner [64]. This is consistent with the obtained results which revealed that the chitosan nanocomposites have greater stability than those of bare magnetite and silicon dioxide nanoparticles (which exhibited some burst release) over 72 h. The results also revealed that CS/M nanocomposite did not exhibit any release at pH 7.4, but CS/S nanocomposite did not exhibit release at pH 4.2 values. By removing a sample and replacing it with fresh PBS, we were discarding the drug in each sample, so that at the end time of the study the partial release may be lowered, which is pretty normal.
The Doxorubicin-loaded nanostructures prepared in this study were compared with some other reported Doxorubicin-loaded nano-carriers as presented in Table 3. The results showed that the synthesized nano-formulations exhibited high loading and release characteristics except for CS/S nanocomposite. It has poor DOX loading compared with tabulated nanocarriers (illustrated in the loading section), and it has a good releasing profile in acidic conditions. The compared Doxorubicin carrier systems such as Gold nanorods coated with Dopamine HCl (GNRs @ DA) showed relatively high loading and release properties but the release process could be thermally induced to alter the desorption of DOX. Liposome/gold nanorods/gelatin/polyglutamic acid (lipo/AuNR/Gel/PGA) carrier system exhibited lower loading and release percentages compared with the as-fabricated systems and the released drug was temperature stimulated using NIR-laser radiation. The other systems such as liposome/gold nanorods/gelatin/polyglutamic acid (lipo/AuNR/Gel/PGA) and methacrylo hydrazide hydrobromide (EKCEK/MAH.HBr functionalized Glu-Lys-Cys-Glu-Lys oligopeptides) have lower loading and release efficiencies than those of the as-prepared nanostructures in the current study.
The remaining system; Glucose oxidase@ hollow mesoporous silica nanoparticles-poly electrolyte multilayer (GOX@HMSN-PEM), has lower Doxorubicin loading efficiency and offers a higher releasing profile in the lower pH values. On the other hand, the as-synthesized DOX nanocarriers in this study; especially, chitosan nanocomposites were prepared using a facile method compared with other tabulated DOX carriers, and they showed better loading and releasing characteristics in an acidic condition. Furthermore, they can be magnetically directed to target sites, and the drug release can be induced via temperature, and they can be good candidates in thermal ablation therapy (hyperthermia).
3.7 Cytotoxicity Effect of the As-Prepared Nanostructures on Cancer Cells
The cytotoxicity test was performed on two well-known malignant cell lines (MCF-7 & HepG2) to determine the (adverse or no) effect of the as-prepared nanomaterials on DOX potency. Three nanostructures M-DOX, CS-DOX, and M/CS-DOX were selected and in-vitro tested, separately, for their cytotoxic activity against two human cancer cell lines (MCF-7, and Hep-G2) using SRB assay. This is due to the SRB assay provides better linearity with cell number and higher sensitivity, and its staining is not cell-line dependent. In contrast to the MTT assay, the SRB assay stained recently lysed cells. Cell debris, however, was not stained by SRB and therefore the drug sensitivity data were not affected [70]. Their activities were compared with the cytotoxicity of DOX as a positive control, which is a potent anticancer agent. Results showed that the tested nanomaterials gave potent and obvious cytotoxic activity against the two tested cancer human cell lines, compared to DOX (positive control) (Figs. 9, 10). Interestingly, the gained results revealed that some drug-loaded nanostructures have higher activity than that of Doxorubicin alone. Furthermore, the estimated half-maximal inhibitory concentration, or in other words; the concentration of drug mandatory to inhibit cell growth by 50% compared to untreated control cells (IC50) values for the examined products: M-DOX, CS-DOX, and CS/M–DOX, were as follows: 3.95 μg/mL, 4.20 μg/mL, and 2.65 μg/mL, respectively, against Hep-G2 after 48 h. While the IC50 value for the positive control Doxorubicin was estimated to be 4.5 μg/mL, against the Hep-G2 cell line. On the other hand, IC50 values for M-DOX, CS-DOX, and CS/M–DOX against the MCF-7 cell line were determined to be 3.40, 3.85, and 2.25 μg/mL, respectively. While the determined IC50 value for the positive control Doxorubicin was 5.1 μg/mL against the MCF-7 cell line. Furthermore, DOX activity in cancer therapy via intercalation into DNA hence inhibits the synthesis of DNA, and it can interact with fast-associated protein with the death domain. Thus, apoptosis was started due to the generation of reactive oxygen species. The previous studies reported that magnetic nanoparticles and the anti-cancer drug can sensitize human breast (MCF-7) and human hepatic (Hep-G2) cancer cells to DOX-induced apoptosis [71,72,73,74]. Therefore, this study benefited from these advantages along with the issue that chitosan, which is a natural, biocompatible, and biodegradable polymer, exhibited antimicrobial and anticancer properties, and it is considered a smart carrier for drugs that could be used for cancer therapy [75]. The cellular transport of these nano-carriers is also significantly different from that of chemical compounds or drugs because they can move across cells, reach nuclear membranes, and target specific nuclear structures such as proteins or gene sequences [11].
From these results, we could conclude that the DOX-loaded CS/M nanocomposite has the highest cytotoxicity for both cell lines; HepG2, and MCF-7. Therefore, we studied the morphologies of the human liver carcinoma cell line (Hep-G2) and human breast carcinoma cell line (MCF-7) before (control group) and after treatment with the DOX-loaded CS/M nanocomposite (M/CS-DOX) of 100 µg/mL concentration as depicted in Fig. 11. Notably that these pictures are the better we have, and the used inverted microscope was an old version. The images (Fig. 11b, d) of the treated HepG2 cells and MCF-7 cells, respectively, with M/CS-DOX nanocomposite, exhibited the loss of characteristic cell structure and the decrease in the cell population, compared to the untreated cells (Fig. 11a, c). Besides, for both cell types, the cells lost their form, detached from the substrate, and diminished in size. These changes were characteristics of the dead cells. However, the sensitivity of the M/CS-DOX nanocomposite towards the MCF-7 cell line was found to be higher leading to more cell death in comparison to its sensitivity towards the HepG2 cell line. These results are consistent with the cytotoxicity results.
4 Conclusions
In summing up, we have reported a facile and controlled approach for preparation of drug delivery nano-carriers based on modified chitosan, magnetite, and silicon dioxide nanostructures along with their nanocomposites for the Doxorubicin anticancer drug. The products were characterized by employing XRD, FT-IR, thermal analysis, HR-TEM, and FE-SEM techniques. The as-synthesized magnetite and silica were prepared, with a crystallite size of ca. 5 and 15 nm, respectively, using co-precipitation and sol–gel methods, respectively. The nanocomposites: CS/M, CS/S, and CS/M/S, were simply prepared using ultra-sonication method and the obtained average particle sizes were 70, 22, and 29 nm, respectively. The DOX drug loading and releasing efficiencies were determined for the as-prepared nanostructures. M, S, CS, CS/M, CS/S, and CS/M/S nanostructures exhibited loading efficacy of 71%, 95%, 96%, 79%, 17%, and 42%, respectively. The Doxorubicin releasing results revealed a promising cumulative release percentages at pH 4.2 and pH 5 compared with those at pH 7.4. The cumulative release percentages were 94%, 96%, 92%, 95%, and 98% for DOX-M, DOX-S, DOX-CS, DOX-CS/M, and DOX-CS/M/S, respectively, at pH 4.2. While the percentages at pH 5 were 97%, 90%, 46%, 43%, and 70%, respectively. However, at pH 5, the percentage for DOX-CS/S was 60%. These data indicated that the fabricated nanomaterials reduced the systemic toxicity of DOX and increased effectively its potent activity. Besides, the DOX-CS/M nano-carrier showed the highest in-vitro cytotoxicity, and its IC50 values were 2.65 and 2.25 μg/mL against Hep-G2 and MCF-7 cell lines respectively, compared to the other DOX-loaded nanostructures and free DOX. The obtained results indicated that CS/M nanocomposite is a good candidate as a drug delivery nano-carrier for the Doxorubicin anti-cancer drug.
References
Z. Bakhtiary, A.A. Saei, M.J. Hajipour, M. Raoufi, O. Vermesh, M. Mahmoudi, Targeted superparamagnetic iron oxide nanoparticles for early detection of cancer: possibilities and challenges. Nanomed.: Nanotechnol. Biol. Med. 12, 287–307 (2016)
K.M.L. Taylor-Pashow, J. Della Rocca, R.C. Huxford, W. Lin, Hybrid nanomaterials for biomedical applications. Chem. Commun. 46, 5832–5849 (2010)
G. Ibáñez-Redín, N. Joshi, G.F. do Nascimento, D. Wilson, M.E. Melendez, A.L. Carvalho, R.M. Reis, D. Gonçalves, O.N. Oliveira, Determination of p53 biomarker using an electrochemical immunoassay based on layer-by-layer films with NiFe2O4 nanoparticles. Microchim. Acta 187, 619 (2020)
E.M. Materon, A. Wong, L.M. Gomes, G. Ibáñez-Redín, N. Joshi, O.N. Oliveira, R.C. Faria, Combining 3D printing and screen-printing in miniaturized, disposable sensors with carbon paste electrodes. J. Mater. Chem. C 9, 5633–5642 (2021)
X. Liang, M. Liu, M. Komiyama, Recognition of target site in various forms of DNA and RNA by peptide nucleic acid (PNA): from fundamentals to practical applications. Bull. Chem. Soc. Jpn. 94, 1737–1756 (2021)
A.A. Halwani, Development of pharmaceutical nanomedicines: from the bench to the market. Pharmaceutics 14, 106 (2022)
J.L. Paris, M. Vallet-Regí, Ultrasound-activated nanomaterials for therapeutics. Bull. Chem. Soc. Jpn. 93, 220–229 (2020)
M. Moharramnejad, A. Ehsani, S. Salmani, M. Shahi, R.E. Malekshah, Z.S. Robatjazi, H. Parsimehr, Zinc-based metal-organic frameworks: synthesis and recent progress in biomedical application. J. Inorg. Organomet. Polym. Mater. (2022). https://doi.org/10.1007/s10904-022-02385-y
G. Kermani, E. Karimi, M.H. Tabrizi, Hybrid nanoarchitectonics of chitosan-cerium oxide nanoparticles for anticancer potentials. J. Inorg. Organomet. Polym. Mater. 32, 2591–2599 (2022)
M. Kutwin, E. Sawosz, S. Jaworski, M. Wierzbicki, B. Strojny, M. Grodzik, M. Ewa Sosnowska, M. Trzaskowski, A. Chwalibog, Nanocomplexes of graphene oxide and platinum nanoparticles against colorectal cancer colo205, HT-29, HTC-116, SW480, liver cancer HepG2, human breast cancer MCF-7, and adenocarcinoma LNCaP and human cervical Hela B cell lines. Materials 12, 909 (2019)
D.M. Jaya Seema, B. Saifullah, M. Selvanayagam, S. Gothai, M.Z. Hussein, S.K. Subbiah, N. Mohd Esa, P. Arulselvan, Designing of the anticancer nanocomposite with sustained release properties by using graphene oxide nanocarrier with phenethyl isothiocyanate as anticancer agent. Pharmaceutics 10, 109 (2018)
C. Xu, K. Pu, Second near-infrared photothermal materials for combinational nanotheranostics. Chem. Soc. Rev. 50, 1111–1137 (2021)
B. Divband, N. Gharehaghaji, S. Hassani, Fe3O4/graphene-based nanotheranostics for bimodal magnetic resonance/fluorescence imaging and cancer therapy. J. Inorg. Organomet. Polym. (2022). https://doi.org/10.1007/s10904-022-02457-z
H. Thakkar, N. Patel, S. Amodwala, Formulation development of controlled release mucoadhesive beads of capecitabine. J. Drug Deliv. Ther. 6, 42–50 (2016)
M.S. Jabir, U.M. Nayef, W.K. Abdulkadhim, Z.J. Taqi, G.M. Sulaiman, U.I. Sahib, A.M. Al-Shammari, Y.-J. Wu, M. El-Shazly, C.-C. Su, Fe3O4 nanoparticles capped with PEG induce apoptosis in breast cancer AMJ13 cells via mitochondrial damage and reduction of NF-κB translocation. J. Inorg. Organomet. Polym. Mater. 31, 1241–1259 (2021)
F. Pepe, S. Pagotto, S. Soliman, C. Rossi, P. Lanuti, C. Braconi, R. Mariani-Costantini, R. Visone, A. Veronese, Regulation of miR-483-3p by the O-linked N-acetylglucosamine transferase links chemosensitivity to glucose metabolism in liver cancer cells. Oncogenesis 6, e328 (2017)
H. Lin, Y. Chen, J. Shi, Nanoparticle-triggered in situ catalytic chemical reactions for tumour-specific therapy. Chem. Soc. Rev. 47, 1938–1958 (2018)
M. Songbo, H. Lang, C. Xinyong, X. Bin, Z. Ping, S. Liang, Oxidative stress injury in doxorubicin-induced cardiotoxicity. Toxicol. Lett. 307, 41–48 (2019)
R.M. Damiani, D.J. Moura, C.M. Viau, R.A. Caceres, J.A.P. Henriques, J. Saffi, Pathways of cardiac toxicity: comparison between chemotherapeutic drugs doxorubicin and mitoxantrone. Arch. Toxicol. 90, 2063–2076 (2016)
A. Fraix, C. Conte, E. Gazzano, C. Riganti, F. Quaglia, S. Sortino, Overcoming doxorubicin resistance with lipid–polymer hybrid nanoparticles photoreleasing nitric oxide. Mol. Pharm. 17, 2135–2144 (2020)
C. Carvalho, R.X. Santos, S. Cardoso, S. Correia, P.J. Oliveira, M.S. Santos, P.I. Moreira, Doxorubicin: the good, the bad and the ugly effect. Curr. Med. Chem. 16, 3267–3285 (2009)
K. Chegaev, C. Riganti, L. Lazzarato, B. Rolando, S. Guglielmo, I. Campia, R. Fruttero, A. Bosia, A. Gasco, Nitric oxide donor doxorubicins accumulate into doxorubicin-resistant human colon cancer cells inducing cytotoxicity. ACS Med. Chem. Lett. 2, 494–497 (2011)
T.D. Schladt, K. Schneider, H. Schild, W. Tremel, Synthesis and bio-functionalization of magnetic nanoparticles for medical diagnosis and treatment. Dalton Trans. 40, 6315–6343 (2011)
A.S. Abdel-Bary, D.A. Tolan, M.Y. Nassar, T. Taketsugu, A.M. El-Nahas, Chitosan, magnetite, silicon dioxide, and graphene oxide nanocomposites: synthesis, characterization, efficiency as cisplatin drug delivery, and DFT calculations. Int. J. Biol. Macromol. 154, 621–633 (2020)
B. Yameen, W.I. Choi, C. Vilos, A. Swami, J. Shi, O.C. Farokhzad, Insight into nanoparticle cellular uptake and intracellular targeting. J. Control. Release 190, 485–499 (2014)
J. Lewandowska-Łańcucka, M. Staszewska, M. Szuwarzyński, M. Kępczyński, M. Romek, W. Tokarz, A. Szpak, G. Kania, M. Nowakowska, Synthesis and characterization of the superparamagnetic iron oxide nanoparticles modified with cationic chitosan and coated with silica shell. J. Alloys Compd. 586, 45–51 (2014)
D. Mai, L. Danh, H. Dang, H. Nguyen, H. Ta, T. Doan, T. Le, T. Phan, Study on adenosine loading capacity of porous nanosilica for application in drug delivery. Sci. Technol. Dev. J. Nat. Sci. (2020). https://doi.org/10.32508/stdjns.v5i1.933
P.J. Vikesland, R.L. Rebodos, J.Y. Bottero, J. Rose, A. Masion, Aggregation and sedimentation of magnetite nanoparticle clusters. Environ. Sci. Nano 3, 567–577 (2016)
M.Y. Nassar, E.A. El-Moety, M. El-Shahat, Synthesis and characterization of a ZnMn2O4 nanostructure as a chemical nanosensor: a facile and new approach for colorimetric determination of omeprazole and lansoprazole drugs. RSC Adv. 7, 43798–43811 (2017)
X. Wei, L. Jing, C. Liu, Y. Hou, M. Jiao, M. Gao, Molecular mechanisms for delicately tuning the morphology and properties of Fe3O4 nanoparticle clusters. CrystEngComm 20, 2421–2429 (2018)
J. Wan, W. Cai, X. Meng, E. Liu, Monodisperse water-soluble magnetite nanoparticles prepared by polyol process for high-performance magnetic resonance imaging. Chem. Commun. (2007). https://doi.org/10.1039/b712795b
K. Yan, P. Li, H. Zhu, Y. Zhou, J. Ding, J. Shen, Z. Li, Z. Xu, P.K. Chu, Recent advances in multifunctional magnetic nanoparticles and applications to biomedical diagnosis and treatment. RSC Adv. 3, 10598 (2013)
E.M. Materón, C.M. Miyazaki, O. Carr, N. Joshi, P.H.S. Picciani, C.J. Dalmaschio, F. Davis, F.M. Shimizu, Magnetic nanoparticles in biomedical applications: a review. Appl. Surf. Sci. Adv. 6, 100163 (2021)
H. Shagholani, S.M. Ghoreishi, M. Mousazadeh, Improvement of interaction between PVA and chitosan via magnetite nanoparticles for drug delivery application. Int. J. Biol. Macromol. 78, 130–136 (2015)
X.N. Pham, T.P. Nguyen, T.N. Pham, T.T.N. Tran, T.V.T. Tran, Synthesis and characterization of chitosan-coated magnetite nanoparticles and their application in curcumin drug delivery. Adv. Nat. Sci.: Nanosci. Nanotechnol. 7, 045010 (2016)
J.L. Arias, L.H. Reddy, P. Couvreur, Fe3O4/chitosan nanocomposite for magnetic drug targeting to cancer. J. Mater. Chem. 22, 7622–7632 (2012)
K. Cho, X. Wang, S. Nie, D.M. Shin, Therapeutic nanoparticles for drug delivery in cancer. Clin. Cancer Res. 14, 1310–1316 (2008)
Y. Xu, Y. Du, Effect of molecular structure of chitosan on protein delivery properties of chitosan nanoparticles. Int. J. Pharm. 250, 215–226 (2003)
G.Z. Kyzas, M. Kostoglou, N.K. Lazaridis, D.A. Lambropoulou, D.N. Bikiaris, Environmental friendly technology for the removal of pharmaceutical contaminants from wastewaters using modified chitosan adsorbents. Chem. Eng. J. 222, 248–258 (2013)
G. Unsoy, R. Khodadust, S. Yalcin, P. Mutlu, U. Gunduz, Synthesis of Doxorubicin loaded magnetic chitosan nanoparticles for pH responsive targeted drug delivery. Eur. J. Pharm. Sci. 62, 243–250 (2014)
C. Cao, L. Xiao, C. Chen, X. Shi, Q. Cao, L. Gao, In situ preparation of magnetic Fe3O4/chitosan nanoparticles via a novel reduction–precipitation method and their application in adsorption of reactive azo dye. Powder Technol. 260, 90–97 (2014)
G. Abdelaziz, H.A. Shamsel-Din, M.O. Sarhan, M.A. Gizawy, Tau protein targeting via radioiodinated azure A for brain theranostics: radiolabeling, molecular docking, in vitro and in vivo biological evaluation. J. Label. Compd. Radiopharm. 63, 33–42 (2020)
U.S. Khan, Amanullah, A. Manan, N. Khan, A. Mahmood, A. Rahim, Transformation mechanism of magnetite nanoparticles. Mater. Sci.-Pol. 33, 278–285 (2015)
R. Jenkins, R.L. Snyder, Introduction to X-Ray Powder Diffractometry (Wiley, New York, 1996)
I. Ramadan, M.M. Moustafa, M.Y. Nassar, Facile controllable synthesis of magnetite nanoparticles via a co-precipitation approach. Egypt. J. Chem. (2022). https://doi.org/10.21608/ejchem.2022.116869.5284
D.J. Lacks, R.G. Gordon, Crystal-structure calculations with distorted ions. Phys. Rev. B 48, 2889 (1993)
W.H. Baur, Silicon–oxygen bond lengths, bridging angles Si–O–Si and synthetic low tridymite. Acta Crystallogr. B 33, 2615–2619 (1977)
H. Zhang, C. Li, G. Jinshan, L. Zang, J. Luo, In situ synthesis of poly(methyl methacrylate)/SiO2 hybrid nanocomposites via “Grafting Onto” strategy based on UV irradiation in the presence of iron aqueous solution. J. Nanomater. (2012). https://doi.org/10.1155/2012/217412
M.Y. Nassar, I.S. Ahmed, M.A. Raya, A facile and tunable approach for synthesis of pure silica nanostructures from rice husk for the removal of ciprofloxacin drug from polluted aqueous solutions. J. Mol. Liq. 282, 251–263 (2019)
M.Y. Nassar, M. Khatab, Cobalt ferrite nanoparticles via a template-free hydrothermal route as an efficient nano-adsorbent for potential textile dye removal. RSC Adv. 6, 79688–79705 (2016)
M.Y. Nassar, I.S. Ahmed, T.Y. Mohamed, M. Khatab, A controlled, template-free, and hydrothermal synthesis route to sphere-like [small alpha]-Fe2O3 nanostructures for textile dye removal. RSC Adv. 6, 20001–20013 (2016)
R.M. Cornell, U. Schwertmann, The Iron Oxides: Structure, Properties, Reactions, Occurrences and Uses (Wiley, Hoboken, 2003)
H.H. El-Feky, M.S. Behiry, A.S. Amin, M.Y. Nassar, Facile fabrication of nano-sized SiO2 by an improved sol–gel route: as an adsorbent for enhanced removal of Cd(II) and Pb(II) ions. J. Inorg. Organomet. Polym. Mater. 32, 1129 (2022)
M.M. Baz, N.M. El-Barkey, A.S. Kamel, A.H. El-Khawaga, M.Y. Nassar, Efficacy of porous silica nanostructure as an insecticide against filarial vector Culex pipiens (Diptera: Culicidae). Int. J. Trop. Insect Sci. 42, 2113 (2022)
D.L. Sonin, D.V. Korolev, V.N. Postnov, E.B. Naumysheva, E.I. Pochkaeva, M.L. Vasyutina, M.M. Galagudza, Silicon-containing nanocarriers for targeted drug delivery: synthesis, physicochemical properties and acute toxicity. Drug Deliv. 23, 1747–1756 (2016)
A. Zhu, L. Yuan, T. Liao, Suspension of Fe3O4 nanoparticles stabilized by chitosan and o-carboxymethylchitosan. Int. J. Pharm. 350, 361–368 (2008)
R. Bansal, R. Singh, K. Kaur, Quantitative analysis of doxorubicin hydrochloride and arterolane maleate by mid IR spectroscopy using transmission and reflectance modes. BMC Chem. 15, 1–11 (2021)
N. Mallick, M. Anwar, M. Asfer, S.H. Mehdi, M.M.A. Rizvi, A.K. Panda, S. Talegaonkar, F.J. Ahmad, Chondroitin sulfate-capped super-paramagnetic iron oxide nanoparticles as potential carriers of doxorubicin hydrochloride. Carbohydr. Polym. 151, 546–556 (2016)
M.Y. Nassar, M.M. Moustafa, M.M. Taha, Hydrothermal tuning of the morphology and particle size of hydrozincite nanoparticles using different counterions to produce nanosized ZnO as an efficient adsorbent for textile dye removal. RSC Adv. 6, 42180–42195 (2016)
M.Y. Nassar, S. Abdallah, Facile controllable hydrothermal route for a porous CoMn2O4 nanostructure: synthesis, characterization, and textile dye removal from aqueous media. RSC Adv. 6, 84050–84067 (2016)
M. Ko, A. Quiñones-Hinojosa, R. Rao, Emerging links between endosomal pH and cancer. Cancer Metastasis Rev. 39, 519–534 (2020)
S. Sadighian, K. Rostamizadeh, H. Hosseini-Monfared, M. Hamidi, Doxorubicin-conjugated core–shell magnetite nanoparticles as dual-targeting carriers for anticancer drug delivery. Colloids Surf. B 117, 406–413 (2014)
F. Ji, H. Sun, Z. Qin, E. Zhang, J. Cui, J. Wang, S. Li, F. Yao, Engineering polyzwitterion and polydopamine decorated doxorubicin-loaded mesoporous silica nanoparticles as a pH-sensitive drug delivery. Polymers 10, 326 (2018)
S. Sadighian, H. Hosseini-Monfared, K. Rostamizadeh, M. Hamidi, pH-Triggered magnetic-chitosan nanogels (MCNs) for doxorubicin delivery: physically vs. chemically cross linking approach. Adv. Pharm. Bull. 5, 115 (2015)
H. Chen, R. Sun, J. Zheng, N. Kawazoe, Y. Yang, G. Chen, Doxorubicin-encapsulated thermosensitive liposome-functionalized photothermal composite scaffolds for synergistic photothermal therapy and chemotherapy. J. Mater. Chem. B 10, 4771–4782 (2022)
K. Cheng, Y. Zhang, Y. Li, Z. Gao, F. Chen, K. Sun, P. An, C. Sun, Y. Jiang, B. Sun, A novel pH-responsive hollow mesoporous silica nanoparticle (HMSN) system encapsulating doxorubicin (DOX) and glucose oxidase (GOX) for potential cancer treatment. J. Mater. Chem. B 7, 3291–3302 (2019)
P. Patel, D. Umapathy, S. Manivannan, V.M. Nadar, R. Venkatesan, V.A. Joseph Arokiyam, S. Pappu, K. Ponnuchamy, A doxorubicin–platinum conjugate system: impacts on PI3K/AKT actuation and apoptosis in breast cancer cells. RSC Adv. 11, 4818–4828 (2021)
W. Xue, A. Trital, S. Liu, L. Xu, Doxorubicin-loaded micelles with high drug-loading capacity and stability based on zwitterionic oligopeptides. New J. Chem. 44, 12633 (2020)
M. Qamar, G. Abbas, M. Afzaal, M.Y. Naz, A. Ghuffar, M. Irfan, S. Legutko, J. Jozwik, M. Zawada-Michalowska, A.A.J. Ghanim, S. Rahman, U.M. Niazi, M. Jalalah, F.S. Alkahtani, M.K.A. Khan, E. Kosicka, Gold nanorods for doxorubicin delivery: numerical analysis of electric field enhancement, optical properties and drug loading/releasing efficiency. Materials 15, 1764 (2022)
Y.P. Keepers, P.E. Pizao, G.J. Peters, J. van Ark-Otte, B. Winograd, H.M. Pinedo, Comparison of the sulforhodamine B protein and tetrazolium (MTT) assays for in vitro chemosensitivity testing. Eur. J. Cancer Clin. Oncol. 27, 897–900 (1991)
K. Aljarrah, N.M. Mhaidat, M.-A.H. Al-Akhras, A.N. Aldaher, B. Albiss, K. Aledealat, F.M. Alsheyab, Magnetic nanoparticles sensitize MCF-7 breast cancer cells to doxorubicin-induced apoptosis. World J. Surg. Oncol. 10, 1–5 (2012)
M.K. Yu, Y.Y. Jeong, J. Park, S. Park, J.W. Kim, J.J. Min, K. Kim, S. Jon, Drug-loaded superparamagnetic iron oxide nanoparticles for combined cancer imaging and therapy in vivo. Angew. Chem. Int. Ed. 47, 5362–5365 (2008)
M. Norouzi, V. Yathindranath, J.A. Thliveris, B.M. Kopec, T.J. Siahaan, D.W. Miller, Doxorubicin-loaded iron oxide nanoparticles for glioblastoma therapy: a combinational approach for enhanced delivery of nanoparticles. Sci. Rep. 10, 1–18 (2020)
H.R. Al Refaey, A.-S.A. Newairy, M.M. Wahby, C. Albanese, M. Elkewedi, M.U. Choudhry, A.S. Sultan, Manuka honey enhanced sensitivity of HepG2, hepatocellular carcinoma cells, for Doxorubicin and induced apoptosis through inhibition of Wnt/β-catenin and ERK1/2. Biol. Res. 54, 16 (2021)
M.S. Shakil, K.M. Mahmud, M. Sayem, M.S. Niloy, S.K. Halder, M.S. Hossen, M.F. Uddin, M.A. Hasan, Using chitosan or chitosan derivatives in cancer therapy. Polysaccharides 2, 795–816 (2021)
Acknowledgements
Authors have no competing acknowledgements.
Funding
Open access funding is provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). Besides, owing to the support received by the present study from Benha University, the first author is also grateful to Benha University (http://bu.edu.eg), Egypt.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nassar, M.Y., El-Salhy, H.I., El-Shiwiny, W.H. et al. Composite Nanoarchitectonics of Magnetic Silicon Dioxide-Modified Chitosan for Doxorubicin Delivery and In Vitro Cytotoxicity Assay. J Inorg Organomet Polym 33, 237–253 (2023). https://doi.org/10.1007/s10904-022-02498-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10904-022-02498-4