Abstract
The aim of this in vitro study was to evaluate the effects of erbium-doped yttrium aluminum garnet (Er:YAG) laser irradiation on titanium surface topography and the proliferation and differentiation of osteoblasts using standard clinical treatment settings. Er:YAG laser irradiation at two levels ((1): 160 mJ, pulse at 20 Hz; (2): 80 mJ, pulse at 20 Hz) was applied to moderately rough and smooth titanium disks before MG-63 osteoblast-like cells were cultured on these surfaces. Titanium surface and cell morphology were observed by scanning electron microscopy. Cell proliferation/viability was measured by CCK-8 test. Gene expression of alkaline phosphatase (ALP), osteocalcin (OC), osteoprotegerin (OPG), receptor activator of nuclear factor kappa-B ligand (RANKL), and collagen type 1 was measured by qPCR, and OPG and OC protein production was determined by enzyme-linked immunosorbent assay. Treatment with Er:YAG laser at 160 mJ/20 Hz markedly caused heat-induced fusion of titanium and cell condensation on moderately rough surfaces, but not in smooth surfaces. MG-63 proliferation/viability decreased after 5 days in moderately rough surfaces. The expression of ALP, OC, OPG, and collagen type 1 was unaffected by laser treatment at 160 mJ/20. Laser irradiation at 80 mJ/20 Hz enhanced RANKL gene expression after 5 days in moderately rough surfaces. Study results suggest that Er:YAG laser irradiation at clinically relevant setting has no essential effect on osteogenic gene and protein expression of osteoblasts. However, surface structure, cell attachment, and proliferation are influenced by both treatment protocols, which implies that caution should be taken in the clinical treatment of peri-implant diseases when Er:YAG laser is used.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Endosseous implants nowadays represent a standard treatment procedure in clinical practice, demonstrating high long-term success rates [1, 2]. Titanium has shown long-term evidence as a safe material for dental implants and still is considered gold standard. In terms of tissue biocompatibility, surface topography is considered as a critical factor influencing the osseointegration process following implant insertion [3]. Preclinical studies have demonstrated that titanium implants with moderately rough surfaces exhibit both higher bone-to-implant contact and removal torque compared to smooth surface implants [4]. Profile roughness average (Sa) of 1–2 µm is suggested to provide optimal conditions for osseointegration, and the majority of commercially available implants nowadays match this roughness level [5]. In vitro, moderately rough surfaces promote osteoblast migration and the expression of osteogenic differentiation markers, whereas these functional parameters might be inhibited by extremely rough surfaces [6]. Despite positive effects on osseointegration, moderately rough surfaces also promote bacterial adherence and facilitate plaque accumulation, which is considered the primary etiologic agent for peri-implant diseases [7, 8].
Peri-implantitis is a site-specific inflammatory disease affecting peri-implant soft and hard tissues and might lead to implant loss. With a subject-based weighted mean prevalence of 19.83%, peri-implantitis represents a growing problem in dentistry, as numbers of dental implants placed are increasing [9]. Accumulation of plaque and the formation of biofilm on the implant surface promote the development of mucositis, which can progress to peri-implantitis without proper treatment [10]. Peri-implantitis treatment strategies, either surgical or nonsurgical, aim primarily to achieve sufficient surface decontamination [11, 12]. Although literature describes several approaches to treat peri-implantitis, there is no gold standard method defined clinically, as the treatment success often remains unpredictable [13,14,15,16].
Application of effects of erbium-doped yttrium aluminum garnet (Er:YAG) laser represents a promising tool for surface decontamination, which is a prerequisite in the treatment of peri-implant diseases [17]. This laser can be used for both nonsurgical and surgical approaches [18] and demonstrates superior effects with regard to bactericidal efficacy compared to conventional mechanical debridement using curettes [19]. Such decontamination strategy is especially useful on rough surfaces and/or between contaminated implant threads. An essential requirement for laser treatment protocols is the minimal collateral damaging effect on the implant surface, which could impair the re-osseointegration process.
To date, evidence on the impact of Er:YAG laser treatment of titanium surfaces on osseointegration generally and osteoblast response, in particular, is scarce. On the one hand, Er:YAG laser irradiation was shown to cause less temperature increases and profound alterations of titanium surfaces compared to the neodymium-doped: yttrium, aluminum, and garnet or CO2 lasers [20]. Few studies investigating the effect of Er:YAG laser irradiation suggest beneficial effects on osteoblast adhesion and proliferation [21, 22]. On the other hand, Er:YAG laser irradiation might cause adverse events, such as distinct alterations of titanium surfaces, when applied at high energy settings [23]. Findings by Galli et al. [24] suggest that Er:YAG laser irradiation of machined as well as on sandblasted and acid-etched titanium disks at 150 mJ/10 Hz pulse decreases proliferation of osteoblast-like Saos-2 cells. The same study further shows that titanium surface irradiation with Er:YAG laser at higher settings impairs the production of osteoprotegerin (OPG) [24]. Recent studies suggest that Er:YAG laser irradiation is also capable of debriding contaminated implant surfaces even at a low-energy level of 50, 60, or 120 mJ/pulse [25,26,27]. However, the effect of clinically relevant low-energy Er:YAG laser settings on osteoblast response, representing a crucial element for implant re-osseointegration, has not been investigated to date.
Therefore, the present study aimed to evaluate how the treatment of smooth and moderately rough titanium surfaces with Er:YAG laser at clinically relevant irradiation settings influences the response of osteoblast-like MG-63 cells cultivated on these surfaces.
2 Materials and methods
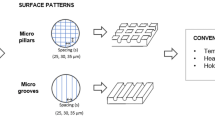
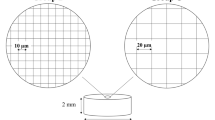
Test titanium disks of 1 mm thickness and 15 mm in diameter were prepared from grade 2 unalloyed commercially pure titanium sheets. Pickled (PT) disks were degreased by washing in acetone and processed through a 2% ammonium fluoride, 2% hydrofluoric acid, 10% nitric acid solution at 55 °C for 30 s. The coarse-grit acid-etched surfaces (SLA) were prepared, as described previously [28, 29].
2.1 Sample preparation and Er:YAG laser treatment
The laser used for experiments was a solid state Er:YAG (Fotona; 2940 nm, Ljubljana, Slovenia) with a wavelength of 2940 nm and a flexible arm. The titanium samples of both PT and SLA surfaces were irradiated at a distance of 2 mm with a conical fiber (Fotona Conical 8. 1,3–0,8, Ljubljana, Slovenia) held at 90 degrees, with a feed speed set at 1 mm per second and continuous water cooling. The application was moved in a standardized meander pattern to cover the entire surface, using a programmable mechanical device. Irradiation parameters were as follows:
-
Group I (PT I, SLA I): 160 mJ, pulse at 20 Hz.
-
Group II (PT II, SLA II): 80 mJ, pulse at 20 Hz.
Untreated PT and SLA surfaces served as controls.
Following laser treatment, each side of the titanium disks was exposed to UV light for 20 min for sterilization before cell cultivation.
2.2 Cell culture
Osteoblast-like MG-63 cells (American Type Culture Collection, Rockville, USA) were used in the present study. Cells were cultured in modified Eagle’s minimum essential medium (MEM, Gibco, Carlsbad, USA) supplemented with 10% fetal bovine serum, penicillin (100 U/ml), and streptomycin (50 µg/ml) at 37 °C in a humidified atmosphere containing 5% CO2. Cells between the third and sixth passages were used in the experiments. Since MG-63 cells are an osteosarcoma cell line, no ethical approval was required.
2.3 Cell proliferation/viability
Cell proliferation/viability was measured using a cell counting kit (CCK-8, Dojindo Laboratories, Japan) as described previously [6]. MG-63 osteoblast-like cells were seeded on different Ti surfaces or tissue culture plastic (TCP) controls at a density of 2 × 104 cells per well and cultured for 2 and 5 days. Afterward, CCK-8 reagent was added into each well, and plates were incubated at 37 °C for the additional 2 h. Four aliquots of 100 µl were transferred from each well into a new 96-well plate, and the optical density at 450 nm was measured using a microplate reader (Molecular Devices, Sunnyvale, USA).
2.4 Quantitative real-time PCR
The expression levels of different osteogenesis and bone-turnover-related genes in MG-63 osteoblast-like cells were quantified by real-time PCR similarly to methods described previously [30, 31]. MG-63 cells were seeded on titanium disks at a density of 2 × 104 cells in 0.5 ml of MEM and cultured for 2 and 5 days. Isolation of mRNA, transcription into cDNA, and qPCR were performed using the TaqMan_Gene Expression Cells-to-CTTM kit (Ambion/Applied Biosystems, Foster City, CA, USA). qPCR was performed on an ABI StepOnePlus device (Applied Biosystems) in paired reactions using the Taqman gene expression assays with following ID numbers (Applied Biosystems) according to the manufacturer’s instructions: alkaline phosphatase (ALP), Hs01029141_g1; osteocalcin (OC), Hs00609452_g1; OPG, Hs00171068_m1; COL1, Hs00164004_m1; receptor activator of nuclear factor kappa-B ligand (RANKL), Hs00243522_m1; and GAPDH, Hs99999905_m1 that was used as a housekeeping gene. The PCR reactions were done in duplicates and the following thermocycling conditions: 95 °C for 10 min; 40 cycles, each for 15 s at 95 °C, and 1 min at 60 °C. The point at which the PCR product was first detected above a fixed threshold (cycle threshold, Ct), was determined for each sample. Alterations in the expression of target genes were calculated using the 2−ΔΔCt method, where ΔΔCt = (Cttarget − CtGAPDH)sample − (Cttarget − CtGAPDH)control, taking MG-63 cells grown on TCP as a control.
2.5 Enzyme-linked immunosorbent assay (ELISA)
Commercially available ELISA kits were used for measurements of OC (BioSource International, Inc., Camarillo, CA, USA) and OPG (Biomedica, GmbH & CoKG, Vienna, Austria) in the supernatants. For the measurement of OC and OPG, the samples were diluted 1:10 and 1:50, respectively. The testing procedure was conducted according to the manufacturer’s instructions using a multi-mode reader Synergy HTX (Biotek, Winooski, VT, USA).
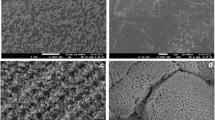
2.6 Scanning electron microscopy
MG-63 cells were seeded on the different surfaces at a density of 2 × 104 cells per well in 0.5 ml of MEM and cultured for 2 days. Afterward, disks were rinsed with PBS, and cells were fixed with 4% formalin for 24 h. Samples were dehydrated with gradient concentrations of ethanol and hexamethyldisilazane (Sigma-Aldrich, St.Louis, MO, USA). Finally, the discs were sputtered with gold for 30 s using the EM ACE200 sputtering device (Leica, Wetzlar, Germany). Samples were analyzed by a scanning electron microscopy (FEI Quanta 200) at an accelerating voltage of 15–20 kV.
2.7 Statistical analysis
Normal data distribution was confirmed by K-S test. The statistical differences between the effects of the various titanium surfaces on the cultured cells were analyzed by one-way analysis of variance for repeated measures followed by t-test. All statistical analyses were performed using SPSS (Statistics Software v 19.0; IBM Corp, Armonk, NY). Differences were considered to be statistically significant at p < 0.05. Data are expressed as mean ± standard error of mean (SEM). All experiments were repeated at least three times.
3 Results
3.1 Scanning electron microscopy
Scanning electron microscopy pictures of MG-63 cells grown on untreated and Er:YAG laser-irradiated PT and SLA surfaces are presented in Fig. 1. Cells grown on PT surfaces showed no visible changes upon laser irradiation at both settings. Moderately rough surfaces showed macro- and microscopic differences, and melted areas representing the course of the laser spot action were observed at 160 mJ/20 Hz laser treatment (SLA I). At the same settings (SLA I), MG-63 cells appeared condensed in the core area affected by laser irradiation, which can also be observed in SLA II to a lower extent (Fig. 1).
Attachment of osteoblast-like cells on PT surfaces after laser irradiation. MG-63 cells were cultured on smooth or moderately rough surfaces treated with Er:YAG laser with 160 mJ/pulse at 20 Hz (PT I and SLA I), 80 mJ/pulse at 20 Hz (PT II and SLA II) or untreated (PT and SLA) surfaces for 2 days and analyzed by scanning electron microscopy (×400). Scale bars correspond to 200 µm
3.2 Proliferation/viability of MG-63 cells on titanium surfaces following laser treatment
Figure 2 shows the proliferation of MG-63 cells grown on untreated and laser-irradiated surfaces PT and SLA surfaces. There were no significant differences in the proliferation/viability between untreated surfaces and TCP group. Proliferation/viability of MG-63 cells grown on a smooth PT surface was not affected by laser irradiation. In contrast, cells grown on irradiated SLA I and SLA II surfaces exhibited lower proliferation compared to untreated SLA surface after 5 days of culture. No significant difference was observed between the surfaces treated with the different irradiation intensities (Fig. 2).
Proliferation/viability of MG-63 cells grown on different titanium surfaces irradiated with Er:YAG laser. MG-63 cells were cultured on smooth (A) or moderately rough (B) surfaces treated with Er:YAG laser with 160 mJ/pulse at 20 Hz (PT I and SLA I), 80 mJ/pulse at 20 Hz (PT II and SLA II) or untreated surfaces (PT and SLA), and proliferation/viability was measured after 2 and 5 days by CCK-8 method. Cells grown on tissue culture plastic (TCP) served as control. Y-axis represents the optical density (OD) values measured at 450 nm. Data are presented as mean ± SEM of three independent experiments
3.3 Expression of osteogenic differentiation markers in MG-63 osteoblast-like cells
Gene expression levels of osteogenic factors in MG-63 cells grown on untreated and differently treated PT and SLA surfaces are shown in Figs. 3 and 4, respectively. After 2 days of incubation, gene expression of ALP was significantly higher in cells on PT I compared to PT and PT II surfaces, and COL1 was expressed lower on PT II than on PT, and PT I. After 5 days, ALP gene expression on PT II was significantly higher than on PT and PT I, and OC expression on both laser-irradiated PT surfaces was lower compared to untreated PT surface (Fig. 3). In SLA surfaces after 2 days, gene expression of ALP and OC was increased on SLA I compared to SLA surfaces. OC expression on SLA I was also higher than on SLA II. Furthermore, gene expression of COL1 was lower on SLA II compared to SLA I and SLA surface. After 5 days, gene expression of ALP was higher on both SLA I and SLA II surfaces compared to the untreated SLA surface. Moreover, ALP gene expression on SLA II was higher than on SLA I surfaces. Laser irradiation at both intensities yielded lower OC expression than untreated control. No difference in COL1 expression was observed after 5 days (Fig. 4).
Expression of osteogenesis-related genes in MG-63 grown on smooth surfaces irradiated with Er:YAG laser. MG-63 cells were cultured on PT, PT I, and PT II surfaces for 2 and 5 days, and the expression levels of ALP (A), OC (B), and COL1 (C) were measured by quantitative real-time PCR. Y-axis represents n-fold expression related to MG-63 grown on tissue culture plastic calculated using 2−ΔΔCt method, using GAPDH as housekeeping gene. Data are presented as the mean ± SEM of four independent experiments
Expression of osteogenesis-related genes in MG-63 grown on moderately rough surfaces irradiated with Er:YAG laser. Following cell culture of MG-63 cells for 2 and 5 days on SLA, SLA I, and SLA II surfaces, the expression levels of ALP (A), OC (B), and COL1 (C) were measured by quantitative real-time PCR. Y-axis represents n-fold expression related to MG-63 grown on tissue culture plastic calculated using 2−ΔΔCt method, using GAPDH as housekeeping gene. Data are presented as the mean ± SEM of four independent experiments
3.4 OC content in conditioned media
Figure 5 shows the content of OC protein in the conditioned media of MG-63 cells grown on untreated and laser-irradiated surfaces. No significant differences in the OC content after 2 and 5 days were observed between cells grown on the differently treated surfaces (Fig. 5).
Osteocalcin production by MG-63 cells grown on titanium disks irradiated with Er:YAG laser. MG-63 cells were cultured on smooth (A) or moderately rough (B) surfaces treated with Er:YAG laser with 160 mJ/pulse at 20 Hz (PT I and SLA I), 80 mJ/pulse at 20 Hz (PT II and SLA II) or untreated surfaces (PT and SLA) for 2 and 5 days, and the levels of OC protein in conditioned media were measured by commercially available ELISA. Data are presented as mean ± SEM of five independent experiments
3.5 Expression of bone turnover markers in MG-63 osteoblast-like cells
Gene expression of the bone turnover proteins OPG and RANKL in MG-63 cells grown on the untreated and laser-irradiated PT and SLA surfaces is shown in Figs. 6 and 7, respectively. In cells cultivated on smooth surfaces for 2 days, OPG gene expression was higher on PT I compared to PT II, however, both laser-irradiated groups exhibited no difference compared to the untreated control. On PT II, RANKL gene expression was higher than on PT after 5 days (Fig. 6). In cells growing on SLA surfaces for 2 days, RANKL gene expression was significantly lower on SLA II compared to SLA I and untreated SLA. No significant difference in the gene expression of OPG was observed. After 5 days, there was no difference in OPG expression among all surfaces, however, RANKL expression in laser-irradiated groups SLA I and SLA II were higher than non-treated control (Fig. 7).
Expression of bone-turnover-related genes in MG-63 grown on smooth surfaces irradiated with Er:YAG laser. MG-63 cells were cultured on smooth surfaces treated with Er:YAG laser with 160 mJ/pulse at 20 Hz (PT II), 80 mJ/pulse at 20 Hz (PT II) or untreated (PT) surfaces for 2 and 5 days, and the expression levels of OPG (A) and RANKL (B) were measured by quantitative real-time PCR. Y-axis represents n-fold expression related to MG-63 grown on tissue culture plastic calculated using 2−ΔΔCt method, using GAPDH as housekeeping gene. Data are presented as the mean ± SEM of four independent experiments
Expression of bone-turnover-related genes in MG-63 grown on moderately rough surfaces irradiated with Er:YAG laser. MG-63 cells were cultured on moderately rough surfaces treated with Er:YAG laser with 160 mJ/pulse at 20 Hz (SLA I), 80 mJ/pulse at 20 Hz (SLA II) or untreated (SLA) surfaces for 2 and 5 days, and the expression levels of OPG (A) and RANKL (B) were measured by quantitative real-time PCR. Y-axis represents n-fold expression related to MG-63 grown on tissue culture plastic calculated using 2−ΔΔCt method, using GAPDH as housekeeping gene. Data are presented as the mean ± SEM of four independent experiments
3.6 OPG production in MG-63 osteoblast-like cells
Figure 8 shows the concentration of OPG in the conditioned media of MG-63 cells grown on the untreated and laser-irradiated PT and SLA surfaces for 2 and 5 days. OPG protein production was unaffected by laser irradiation (Fig. 8).
Osteoprotegerin production by MG-63 cells grown on titanium disks irradiated with Er:YAG laser MG-63 cells was cultured on smooth (A) or moderately rough (B) surfaces treated with Er:YAG laser with 160 mJ/pulse at 20 Hz (PT I and SLA I), 80 mJ/pulse at 20 Hz (PT II and SLA II) or untreated (PT and SLA) surfaces for 2 and 5 days, and the levels of OC protein in conditioned media were measured by commercially available ELISA. Data are presented as mean ± SEM of five independent experiments
4 Discussion
Surface decontamination of dental implants is a key requirement in the treatment of biofilm-associated peri-implant diseases such as peri-implant mucositis and peri-implantitis [32]. Although studies have investigated the impact of Er:YAG laser irradiation on titanium surfaces and reported also bactericidal properties [27, 33], evidence on the impact of laser treatment on the topography of Ti surfaces and response of osteogenic cell growing on those surfaces has been rarely shown so far. However, re-osseointegration plays a critical role in the clinical outcome following laser therapy at implant sites affected by peri-implantitis.
The present study demonstrates that irradiation of moderately rough titanium surfaces using the Er.YAG laser impacted the cell morphology of MG-63 osteoblast-like cells that were afterwards cultivated on those surfaces. This effect, however, was not observed for smooth surfaces. The laser parameters used in this study represent actual settings that are applied in patient treatment, and a similar range of settings has been used frequently in clinical trials [34, 35]. Some previous studies already reported the alteration of Ti surface morphology after laser irradiation, notably, Galli et al. [24] using Er:YAG laser with slightly different settings (200 mJ/pulse at 10 Hz) showed that irradiation alters the morphology of sandblasted and acid-etched but not that of machined surfaces. Likewise, Stubinger et al. [23] also reported the alteration of Ti surface morphology by Er:YAG laser used at higher intensities (300 mJ/10 Hz). In contrast, Shin et al. [36] showed that SLA surfaces did not exhibit significant changes of surface texture upon laser irradiation time of fewer than 2 min at power up to 140 mJ/pulse. Interestingly, we observed the irradiation of Er:YAG laser with 80 mJ/pulse and 20 Hz caused changes in the SLA surface topography. Thus, titanium surfaces seem sensitive to changes in irradiation settings such as irradiation time or feed speed, which have to be considered a crucial factor during laser application in clinical treatment.
According to the present findings, laser irradiation of moderately rough Ti surfaces at 160 mJ/20 Hz negatively affects osteoblast proliferation/viability as measured by CCK-8 assay, which is based on the measurements of cell mitochondrial activity and therefore reflects the combination of two functional parameters, cell proliferation, and cell viability. Decreased osteoblasts proliferation on moderately rough Ti surface after laser irradiation might imply its negative effect on the initial osteogenic process. Our results are supported by Galli et al. [24], who also reported that Er:YAG irradiation at somewhat different settings negatively influenced the proliferation/viability of osteoblast-like cells. In contrast, two other studies showed a significantly higher osteoblasts proliferation/viability upon laser irradiation [37, 38]. In this context, it has to be taken into account that all of the referred studies have been performed with Saos-2 cells, an osteosarcoma cell line that might exhibit different traits than the MG-63 osteoblast-like cells used in the present study. MG-63 cells are an osteosarcoma cell line with osteoblastic features and have been demonstrated to keep stable properties during passaging [39, 40], whereas primary osteoblasts may exhibit different traits depending on the source, donor, and isolation method [41].
Laser treatment seems to have partly influenced the expression of osteogenesis-related genes in MG-63 cells, depending on the type of titanium surface. In our study, we focused on the expression of ALP, OC, and collagen type 1. These proteins play an essential role in osteogenesis and bone formation. ALP is considered a marker for early osteogenic differentiation and is detected in high levels in cells that mineralize their matrix, such as osteoblasts [42]. OC is the most abundant non-collagenous protein in bone and is crucial for bone formation and remodeling [43]. Collagen type 1 is a bone matrix protein secreted by osteoblasts and used as a marker for osteoblast differentiation [44]. Although we observed lower gene expression of OC following laser irradiation in moderately rough surfaces, our results suggest that the production of OC on protein level was generally unaffected by laser irradiation in both surface groups at 2 and 5 days compared to untreated control. These findings again are supported by Galli et al. [24], who used similar irradiation settings (150 mJ/10 Hz pulse), investigating OC production in osteoblast-like cells after 3 and 6 days.
Some effects of laser irradiation on the OPG/RANKL ratio in MG-63 cells were observed. After 5 days, RANKL gene expression was higher on laser-irradiated moderately rough surfaces compared to untreated control. OPG and RANKL are critical factors involved in bone metabolism [45]. By activating osteoclasts, RANKL promotes bone resorption, whereas OPG is known to bind to RANKL, thus inhibiting its ability to activate osteoclasts. Therefore, a lower OPG/RANKL ratio might indicate higher bone resorption on the moderately rough surface after laser irradiation. Unfortunately, we could not prove the alteration of the OPG/RANKL ratio on the protein level because the content of RANKL in conditioned media was below the detection limit. The data on OPG protein were in agreement with PCR data, and there was no effect of laser irradiation on OPG production. Although our data imply the alteration of bone turnover upon laser irradiation in the in vitro setting, the clinical relevance of this effect should be confirmed by further studies.
One limitation of the study might be a relatively low number of independent experiments. We repeated cell viability/proliferation experiments three times, which agrees with previous studies using a similar design (e.g., [24, 46] who performed three repetitions). PCR and ELISA experiments were repeated four and five times, respectively, because these experiments showed more considerable variability. Another potential limitation is that we used the osteosarcoma MG-63 cell line. Although these cells largely reflect the properties of osteoblasts [40], our findings should be further confirmed by the experiments with primary osteoblasts or mesenchymal stromal cells.
5 Conclusion
In general, the use of Er:YAG laser for surface decontamination aims to perform debridement of implant surfaces from bacteria, without impairing the surface itself. The present findings only partly reflect clinical conditions and might be repeated utilizing biofilm-contaminated titanium surfaces, which was beyond the focus of this research project. Taken together, we conclude that the use of Er:YAG laser for decontamination of titanium surfaces does not impair the expression of specific osteogenesis marker at the gene and protein level; however, it might influence bone turnover. Therefore, the application has to be performed with caution, as inappropriate high laser irradiation might compromise implant re-osseointegration into surrounding bone.
References
Karoussis IK, Brägger U, Salvi GE, Bürgin W, Lang NP. Effect of implant design on survival and success rates of titanium oral implants: a 10-year prospective cohort study of the ITI Dental Implant System. Clin Oral Implants Res. 2004;15:8–17.
Howe MS, Keys W, Richards D. Long-term (10-year) dental implant survival: a systematic review and sensitivity meta-analysis. J Dent. 2019;84:9–21. https://doi.org/10.1016/j.jdent.2019.03.008.
Smeets R, Stadlinger B, Schwarz F, Beck-Broichsitter B, Jung O, Precht C, et al. Impact of dental implant surface modifications on osseointegration. Biomed Res Int. 2016;2016:6285620. https://doi.org/10.1155/2016/6285620.
Wall I, Donos N, Carlqvist K, Jones F, Brett P. Modified titanium surfaces promote accelerated osteogenic differentiation of mesenchymal stromal cells in vitro. Bone. 2009;45:17–26. https://doi.org/10.1016/j.bone.2009.03.662.
Albrektsson T, Wennerberg A. Oral implant surfaces: part 1-review focusing on topographic and chemical properties of different surfaces and in vivo responses to them. Int J Prosthodont. 2004;17:536–43.
Andrukhov O, Huber R, Shi B, Berner S, Rausch-Fan X, Moritz A, et al. Proliferation, behavior, and differentiation of osteoblasts on surfaces of different microroughness. Dent Mater. 2016;32:1374–84. https://doi.org/10.1016/j.dental.2016.08.217.
Subramani K, Jung RE, Molenberg A, Hammerle CH. Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants. 2009;24:616–26.
Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Periodontol. 2018;89 Suppl 1:S267–90. https://doi.org/10.1002/JPER.16-0350.
Lee CT, Huang YW, Zhu L, Weltman R. Prevalences of peri-implantitis and peri-implant mucositis: systematic review and meta-analysis. J Dent. 2017;62:1–12. https://doi.org/10.1016/j.jdent.2017.04.011.
Jepsen S, Berglundh T, Genco R, Aass AM, Demirel K, Derks J, et al. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol. 2015;42 Suppl 16:S152–7. https://doi.org/10.1111/jcpe.12369.
Suárez-López Del Amo F, Yu SH, Wang HL. Non-surgical therapy for peri-implant diseases: a systematic review. J Oral Maxillofac Res. 2016;7:e13. https://doi.org/10.5037/jomr.2016.7313.
Ramanauskaite A, Daugela P, Faria de Almeida R, Saulacic N. Surgical non-regenerative treatments for peri-implantitis: a systematic review. J Oral Maxillofac Res. 2016;7:e14 https://doi.org/10.5037/jomr.2016.7314.
Renvert S, Polyzois I, Persson GR. Treatment modalities for peri-implant mucositis and peri-implantitis. Am J Dent. 2013;26:313–8.
Mombelli A, Feloutzis A, Bragger U, Lang NP. Treatment of peri-implantitis by local delivery of tetracycline. Clinical, microbiological and radiological results. Clin Oral Implants Res. 2001;12:287–94.
Heitz-Mayfield LJA, Salvi GE, Mombelli A, Faddy M, Lang NP. Anti-infective surgical therapy of peri-implantitis. A 12-month prospective clinical study. Clin Oral Implants Res. 2012;23:205–10. https://doi.org/10.1111/j.1600-0501.2011.02276.x.
Bassetti M, Schär D, Wicki B, Eick S, Ramseier CA, Arweiler NB, et al. Anti-infective therapy of peri-implantitis with adjunctive local drug delivery or photodynamic therapy: 12-month outcomes of a randomized controlled clinical trial. Clin Oral Implants Res. 2014;25:279–87. https://doi.org/10.1111/clr.12155.
Kreisler M, Kohnen W, Christoffers AB, Götz H, Jansen B, Duschner H, et al. In vitro evaluation of the biocompatibility of contaminated implant surfaces treated with an Er: YAG laser and an air powder system. Clin Oral Implants Res. 2005;16:36–43. https://doi.org/10.1111/j.1600-0501.2004.01056.x.
Coluzzi DJ, Goldstein AJ. Lasers in dentistry. An overview. Dent Today. 2004;23:120–2.
Kuo HN, Mei HI, Liu TK, Liu TY, Lo LJ, Lin CL. In vitro laser treatment platform construction with dental implant thread surface on bacterial adhesion for peri-implantitis. Biomed Res Int. 2017;2017:4732302. https://doi.org/10.1155/2017/4732302.
Kreisler M, Al Haj H, d’Hoedt B. Temperature changes at the implant-bone interface during simulated surface decontamination with an Er:YAG laser. Int J Prosthodont. 2002;15:582–7.
Romanos G, Crespi R, Barone A, Covani U. Osteoblast attachment on titanium disks after laser irradiation. Int J Oral Maxillofac Implants. 2006;21:232–6.
Friedmann A, Antic L, Bernimoulin JP, Purucker P. In vitro attachment of osteoblasts on contaminated rough titanium surfaces treated by Er:YAG laser. J Biomed Mater Res A. 2006;79:53–60. https://doi.org/10.1002/jbm.a.30699.
Stubinger S, Etter C, Miskiewicz M, Homann F, Saldamli B, Wieland M, et al. Surface alterations of polished and sandblasted and acid-etched titanium implants after Er:YAG, carbon dioxide, and diode laser irradiation. Int J Oral Maxillofac Implants. 2010;25:104–11.
Galli C, Macaluso GM, Elezi E, Ravanetti F, Cacchioli A, Gualini G, et al. The effects of Er:YAG laser treatment on titanium surface profile and osteoblastic cell activity: an in vitro study. J Periodontol. 2011;82:1169–77. https://doi.org/10.1902/jop.2010.100428.
Taniguchi Y, Aoki A, Mizutani K, Takeuchi Y, Ichinose S, Takasaki AA, et al. Optimal Er:YAG laser irradiation parameters for debridement of microstructured fixture surfaces of titanium dental implants. Lasers Med Sci. 2013;28:1057–68. https://doi.org/10.1007/s10103-012-1171-7.
Matsuyama T, Aoki A, Oda S, Yoneyama T, Ishikawa I. Effects of the Er:YAG laser irradiation on titanium implant materials and contaminated implant abutment surfaces. J Clin Laser Med Surg. 2003;21:7–17. https://doi.org/10.1089/10445470360516680.
Kreisler M, Kohnen W, Marinello C, Götz H, Duschner H, Jansen B, et al. Bactericidal effect of the Er:YAG laser on dental implant surfaces: an in vitro study. J Periodontol. 2002;73:1292–8. https://doi.org/10.1902/jop.2002.73.11.1292.
Rausch-fan X, Qu Z, Wieland M, Matejka M, Schedle A. Differentiation and cytokine synthesis of human alveolar osteoblasts compared to osteoblast-like cells (MG63) in response to titanium surfaces. Dent Mater. 2008;24:102–10.
Shi B, Andrukhov O, Berner S, Schedle A, Rausch-Fan X. The angiogenic behaviors of human umbilical vein endothelial cells (HUVEC) in co-culture with osteoblast-like cells (MG-63) on different titanium surfaces. Dent Mater. 2014;30:839–47. https://doi.org/10.1016/j.dental.2014.05.005.
Blufstein A, Behm C, Nguyen PQ, Rausch-Fan X, Andrukhov O. Human periodontal ligament cells exhibit no endotoxin tolerance upon stimulation with Porphyromonas gingivalis lipopolysaccharide. J Periodontal Res. 2018. https://doi.org/10.1111/jre.12549.
Behm C, Blufstein A, Gahn J, Kubin B, Nemec M, Moritz A, et al. 1,25(OH)2D3 differently affects immunomodulatory activities of mesenchymal stem cells depending on the presence of TNF-alpha, IL-1beta and IFN-gamma. J clin med. 2019;8. https://doi.org/10.3390/jcm8122211.
Figuero E, Graziani F, Sanz I, Herrera D, Sanz M. Management of peri-implant mucositis and peri-implantitis. Periodontol 2000. 2014;66:255–73. https://doi.org/10.1111/prd.12049.
Eick S, Meier I, Spoerlé F, Bender P, Aoki A, Izumi Y, et al. In vitro-activity of Er:YAG laser in comparison with other treatment modalities on biofilm ablation from implant and tooth surfaces. PLoS ONE. 2017;12:e0171086. https://doi.org/10.1371/journal.pone.0171086.
Ashnagar S, Nowzari H, Nokhbatolfoghahaei H, Yaghoub Zadeh B, Chiniforush N, Choukhachi Zadeh N. Laser treatment of peri-implantitis: a literature review. J Lasers Med Sci. 2014;5:153–62.
Persson GR, Roos-Jansåker AM, Lindahl C, Renvert S. Microbiologic results after non-surgical erbium-doped:yttrium, aluminum, and garnet laser or air-abrasive treatment of peri-implantitis: a randomized clinical trial. J Periodontol. 2011;82:1267–78. https://doi.org/10.1902/jop.2011.100660.
Shin SI, Min HK, Park BH, Kwon YH, Park JB, Herr Y, et al. The effect of Er:YAG laser irradiation on the scanning electron microscopic structure and surface roughness of various implant surfaces: an in vitro study. Lasers Med Sci. 2011;26:767–76. https://doi.org/10.1007/s10103-010-0819-4.
Ayobian-Markazi N, Karimi M, Safar-Hajhosseini A. Effects of Er: YAG laser irradiation on wettability, surface roughness, and biocompatibility of SLA titanium surfaces: an in vitro study. Lasers Med Sci. 2015;30:561–6. https://doi.org/10.1007/s10103-013-1361-y.
Ayobian-Markazi N, Fourootan T, Zahmatkesh A. An in vitro evaluation of the responses of human osteoblast-like SaOs-2 cells to SLA titanium surfaces irradiated by erbium:yttrium-aluminum-garnet (Er:YAG) lasers. Lasers Med Sci. 2014;29:47–53. https://doi.org/10.1007/s10103-012-1224-y.
Boyan BD, Batzer R, Kieswetter K, Liu Y, Cochran DL, Szmuckler-Moncler S. et al. Titanium surface roughness alters responsiveness of MG63 osteoblast-like cells to 1 alpha,25-(OH)2D3. J Biomed Mater Res. 1998;39:77–85. https://doi.org/10.1002/(SICI)1097-4636(199801)39:13.0.CO;2-L.
Pautke C, Schieker M, Tischer T, Kolk A, Neth P, Mutschler W, et al. Characterization of osteosarcoma cell lines MG-63, Saos-2 and U-2 OS in comparison to human osteoblasts. Anticancer Res. 2004;24:3743–8.
Jonsson KB, Frost A, Nilsson O, Ljunghall S, Ljunggren O. Three isolation techniques for primary culture of human osteoblast-like cells: a comparison. Acta Orthop Scand. 1999;70:365–73.
Owen TA, Holthuis J, Markose E, van Wijnen AJ, Wolfe SA, Grimes SR, et al. Modifications of protein-DNA interactions in the proximal promoter of a cell-growth-regulated histone gene during onset and progression of osteoblast differentiation. Proc Natl Acad Sci USA. 1990;87:5129–33. https://doi.org/10.1073/pnas.87.13.5129.
Boskey AL, Gadaleta S, Gundberg C, Doty SB, Ducy P, Karsenty G. Fourier transform infrared microspectroscopic analysis of bones of osteocalcin-deficient mice provides insight into the function of osteocalcin. Bone. 1998;23:187–96. https://doi.org/10.1016/s8756-3282(98)00092-1.
Aubin JE, Liu F, Malaval L, Gupta AK. Osteoblast and chondroblast differentiation. Bone. 1995;17 2 Suppl:77s–83S.
Belibasakis GN, Bostanci N. The RANKL-OPG system in clinical periodontology. J Clin Periodontol. 2012;39:239–48. https://doi.org/10.1111/j.1600-051X.2011.01810.x.
Ramenzoni LL, Hirsiger C, Weber FE, Attin T, Schmidlin PR. Similar inductive effects of enamel and dentin matrix derivatives on osteoblast-like cell response over SLA titanium surface. Arch oral Biol. 2020;109:104552. https://doi.org/10.1016/j.archoralbio.2019.104552.
Acknowledgements
We thank Mrs. Nguyen Phuong Quynh for excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wehner, C., Laky, M., Shokoohi-Tabrizi, H.A. et al. Effects of Er:YAG laser irradiation of different titanium surfaces on osteoblast response. J Mater Sci: Mater Med 32, 22 (2021). https://doi.org/10.1007/s10856-021-06493-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-021-06493-y