Abstract
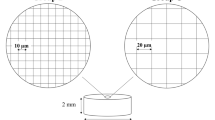
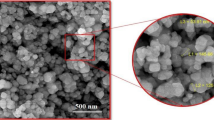
Zirconia has been regarded as a promising material for dental implants, and Nd:YAG laser treatment has been proposed as a potential strategy to improve its bioactivity. The main aim of the present study was to evaluate the in vitro behavior of human fetal osteoblasts in contact with laser-textured zirconia implant surfaces assessing the effect of different texture patterns, spacing between laser passes and number of laser passes. Zirconia discs were produced and treated with Nd:YAG laser according to test group variables: texture (microgrooves and micropillar array), distance between surface features (25 μm, 30 μm and 35 μm), and laser passes [1, 2, 4, and 8]. Untextured sandblasted and acid-etched zirconia discs (SBAE) were used as controls. Human osteoblasts (hFOB 1.19) were cultured for 14 days on test and control samples. Morphology and cellular adhesion were observed using scanning electron microscopy (SEM). Cell viability and proliferation were evaluated at 1, 3, 7, and 14 days using a commercial resazurin-based method. Collagen type I was evaluated at 3 days using ELISA. Alkaline phosphatase (ALP) activity was evaluated at 7 days using a colorimetric enzymatic technique. Group comparisons were tested using ANOVA or Mann-Whitney test (Tukey’s post hoc) using statistical software, and significance was set at p < 0.05. Cell viability and proliferation increased over time for all groups with statistically higher values for laser-textured groups when compared with control at 7 and 14 days in culture (p < 0.05). Collagen type I levels were higher for study groups (p < 0.05) when compared with control group. No statistically differences were detected for ALP activity levels between texture and control groups (p > 0.05). The results suggest that laser-machined zirconia implant surfaces may benefit biological osteoblast response. However, the type of texture, spacing at the range of 25–35 μm, and number of laser passes did not seem to be relevant variables.





Similar content being viewed by others
References
Kuroda K, Okido M (2012) Hydroxyapatite coating of titanium implants using hydroprocessing and evaluation of their osteoconductivity. Bioinorg Chem Appl 2012:730693
Wenz HJ, Bartsch J, Wolfart S, Kern M (2008) Osseointegration and clinical success of zirconia dental implants: a systematic review. Int J Prosthodont 21(1):27–36
Laranjeira MS, Carvalho A, Pelaez-Vargas A, Hansford D, Ferraz MP, Coimbra S et al (2014) Modulation of human dermal microvascular endothelial cell and human gingival fibroblast behavior by micropatterned silica coating surfaces for zirconia dental implant applications. Sci Technol Adv Mater 15(2):025001
Cho YD, Shin JC, Kim HL, Gerelmaa M, Yoon HI, Ryoo HM et al (2014) Comparison of the osteogenic potential of titanium- and modified zirconia-based bioceramics. Int J Mol Sci 15(3):4442–4452
Rezaei NM, Hasegawa M, Ishijima M, Nakhaei K, Okubo T, Taniyama T et al (2018) Biological and osseointegration capabilities of hierarchically (meso−/micro−/nano-scale) roughened zirconia. Int J Nanomedicine 13:3381–3395
Delgado-Ruiz RA, Calvo-Guirado JL, Abboud M, Ramirez-Fernandez MP (2014) Mate-Sanchez de Val JE, Negri B, et al. Histologic and histomorphometric behavior of microgrooved zirconia dental implants with immediate loading. Clin Implant Dent Relat Res 16(6):856–872
Hirano T, Sasaki H, Honma S, Furuya Y, Miura T, Yajima Y et al (2015) Proliferation and osteogenic differentiation of human mesenchymal stem cells on zirconia and titanium with different surface topography. Dent Mater J 34(6):872–880
Cionca N, Hashim D, Mombelli A (2017) Zirconia dental implants: where are we now, and where are we heading? Periodontol 2000 73(1):241–258
Andreiotelli M, Wenz HJ, Kohal RJ (2009) Are ceramic implants a viable alternative to titanium implants? A systematic literature review. Clin Oral Implants Res 20(Suppl 4):32–47
Manzano G, Herrero LR, Montero J (2014) Comparison of clinical performance of zirconia implants and titanium implants in animal models: a systematic review. Int J Oral Maxillofac Implants 29(2):311–320
von Wilmowsky C, Moest T, Nkenke E, Stelzle F, Schlegel KA (2014) Implants in bone: part I. a current overview about tissue response, surface modifications and future perspectives. Oral Maxillofac Surg 18(3):243–257
Al Qahtani WM, Schille C, Spintzyk S, Al Qahtani MS, Engel E, Geis-Gerstorfer J et al (2017) Effect of surface modification of zirconia on cell adhesion, metabolic activity and proliferation of human osteoblasts. Biomed Tech (Berl) 62(1):75–87
Zhu B, Lu Q, Yin J, Hu J, Wang Z (2005) Alignment of osteoblast-like cells and cell-produced collagen matrix induced by nanogrooves. Tissue Eng 11(5–6):825–834
Kohal RJ, Finke HC, Klaus G (2009) Stability of prototype two-piece zirconia and titanium implants after artificial aging: an in vitro pilot study. Clin Implant Dent Relat Res 11(4):323–329
Taniguchi Y, Kakura K, Yamamoto K, Kido H, Yamazaki J (2016) Accelerated osteogenic differentiation and bone formation on zirconia with surface grooves created with fiber laser irradiation. Clin Implant Dent Relat Res 18(5):883–894
Kim HK, Woo KM, Shon WJ, Ahn JS, Cha S, Park YS (2015) Comparison of peri-implant bone formation around injection-molded and machined surface zirconia implants in rabbit tibiae. Dent Mater J 34(4):508–515
Delgado-Ruiz RA, Gomez Moreno G, Aguilar-Salvatierra A, Markovic A, Mate-Sanchez JE, Calvo-Guirado JL (2016) Human fetal osteoblast behavior on zirconia dental implants and zirconia disks with microstructured surfaces. An experimental in vitro study. Clin Oral Implants Res 27(11):e144–ee53
Gabriella M, Penarrieta-Juanito MC, Costa M, Georgina Miranda JM, Magini RS, Antonio Mata JCMS, Caramês J, Silva FS (2018) A novel gradated zirconia implant material embedding bioactive ceramics: physicochemical assessment and human osteoblast behavior. Materialia 1:3–14
Carvalho BMPEPM, Falcón-Antenucci RM, Júnior JSF (2009) Tratamentos de superfície nos implantes dentários. Rev Cir Traumatol Buco-Maxilo-fac 9(1):123–130
Hao L, Lawrence J, Chian KS (2004) Effects of CO2 laser irradiation on the surface properties of magnesia-partially stabilised zirconia (MgO-PSZ) bioceramic and the subsequent improvements in human osteoblast cell adhesion. J Biomater Appl 19(2):81–105
Ketabi M, Deporter D (2013) The effects of laser microgrooves on hard and soft tissue attachment to implant collar surfaces: a literature review and interpretation. Int J Periodontics Restorative Dent 33(6):e145–e152
Kohal RJ, Bachle M, Att W, Chaar S, Altmann B, Renz A et al (2013) Osteoblast and bone tissue response to surface modified zirconia and titanium implant materials. Dent Mater 29(7):763–776
Anselme K, Bigerelle M, Noel B, Dufresne E, Judas D, Iost A et al (2000) Qualitative and quantitative study of human osteoblast adhesion on materials with various surface roughnesses. J Biomed Mater Res 49(2):155–166
Rompen E, Domken O, Degidi M, Pontes AE, Piattelli A (2006) The effect of material characteristics, of surface topography and of implant components and connections on soft tissue integration: a literature review. Clin Oral Implants Res 17(Suppl 2):55–67
Hafezeqoran A, Koodaryan R (2017) Effect of zirconia dental implant surfaces on bone integration: a systematic review and meta-analysis. Biomed Res Int 2017:9246721
Sivaraman K, Chopra A, Narayan AI, Balakrishnan D (2018) Is zirconia a viable alternative to titanium for oral implant? A critical review. J Prosthodont Res 62(2):121–133
Stranciuc AM, Flamant Q, Sprecher CM, Alini M (2018) Anglada Marc, Peroglio M. Femtosecond laser multi-patterning of zirconia for screening of cell-surface interactions. J Eur Ceram Soc 38(3):939–948
Lopes P (2017) Desenvolvimento de texturas superficiais em ZrO2 recorrendo a laser Para aplicações biomédicas [Dissertação de Mestrado em Engenharia de Materiais]: Universidade do Minho
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39(2):175–191
da Cruz MB, Marques JF, Penarrieta-Juanito GM, Costa M, Souza JC, Magini RS et al (2019) Hard and soft tissue cell behavior on polyetheretherketone, zirconia, and titanium implant materials. Int J Oral Maxillofac Implants 34(1):39–46
Shah FA, Thomsen P, Palmquist A (2019) Osseointegration and current interpretations of the bone-implant interface. Acta Biomater 84:1–15
Jeon H, Simon CG Jr, Kim G (2014) A mini-review: cell response to microscale, nanoscale, and hierarchical patterning of surface structure. J Biomed Mater Res B Appl Biomater 102(7):1580–1594
Dinca VS, Sima LE, Rusen L, Bonciu A, Lipper T, Dinescu M, Farsari M. Bio-interfaces engineering using laser-based methods for controlled regulation of mesenchymal stem cell response in vitro. 2016. In: Recent Advances in Biopolymers. [221–51]
Schunemann FH, Galarraga-Vinueza ME, Magini R, Fredel M, Silva F, Souza JCM et al (2019) Zirconia surface modifications for implant dentistry. Mater Sci Eng C Mater Biol Appl 98:1294–1305
Baino F, Montealegre MA, Minguella-Canela J, Vitale-Brovarone C (2019) Laser surface texturing of alumina/zirconia composite ceramics for potential use in hip joint prosthesis. MDPI - Coatings. 9(369)
Samant AN, Dahotre NB (2009) Physical effects of multipass two-dimensional laser machining of structural ceramics. Adv Eng Mater 11(7):579–585
Samant AN, Dahotre NB (2009) Laser machining of structural ceramics—a review. J Eur Ceram Soc 29:969–993
Funding
This work was supported by the FCT (Foundation for Science and Techonology, Portugal) with the reference FunImp project 01-0145-FEDER-030498 and co-financed by.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 5992 kb)
Rights and permissions
About this article
Cite this article
Fernandes, B.F., da Cruz, M.B., Marques, J.F. et al. Laser Nd:YAG patterning enhance human osteoblast behavior on zirconia implants. Lasers Med Sci 35, 2039–2048 (2020). https://doi.org/10.1007/s10103-020-03066-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03066-3