Abstract
Purpose
This study sought to assess the behavior of soft and hard tissue cells on Nd:YAG laser-textured zirconia implant surfaces with parameters that simulate roughness and topography of sandblasting and acid-etching.
Methods
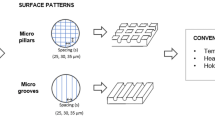
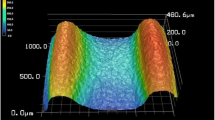
Zirconia discs were prepared and treated with sandblasting and acid-etching, laser 10 μm spacing 10% power (D10P10) or laser 20 μm spacing 1% power (D20P1). Roughness and wettability were measured. Human osteoblasts and fibroblasts were cultivated on the zirconia disks, and their viability was evaluated. IL-1β and IL-6 production was evaluated by ELISA. Morphology and adhesion were analyzed by fluorescence microscopy and Field Emission Gun Scanning Electron Microscopy (FEG-SEM). Groups were compared using one-way ANOVA (fibroblasts viability, mechanical tests, interleukins) or Kruskal-Wallis (osteoblasts viability) tests, as appropriate.
Results
No statistically significant differences were observed in the viability of osteoblasts over time. Fibroblasts showed a higher viability for laser 10 μm spacing 10% power then for sandblasting and acid-etching at 1 and 7 days of culture. There were no statistically significant differences in inflammatory interleukin production. Microscopy images revealed early cell adhesion, normal morphology, and more fibroblasts in laser groups.
Conclusion
Laser texturing seems to allow the production of sandblasting and acid-etching-like surfaces, with a similar behavior for osteoblasts and an improved behavior for fibroblasts.







Similar content being viewed by others
Data Availability
The authors declare that the data supporting the findings of this study are available within the article.
References
Esposito, M., Ardebili, Y., Worthington, H.V.: Interventions for replacing missing teeth: different types of dental implants.Cochrane Database Syst Rev. (2014). Jul 22;2014.
Kohal, R.J., Weng, D., Bächle, M., Strub, J.R.: Loaded Custom-Made Zirconia and Titanium Implants Show Similar Osseointegration: An Animal Experiment. J. Periodontol. 75, 1262–1268 (2004)
Al Qahtani, W.M.S., Schille, C., Spintzyk, S., Al Qahtani, M.S.A., Engel, E., Geis-Gerstorfer, J., et al.: Effect of surface modification of zirconia on cell adhesion, metabolic activity and proliferation of human osteoblasts. Biomed. Tech. 62, 75–87 (2017)
Kalucrossed, D., Signerović, M.R., Schreckenbach, J.P., Graf, H.L.: Zirconia coated titanium for implants and their interactions with osteoblast cells. Mater. Sci. Eng. C. 44, 254–261 (2014)
Yoshinari, M.: Future prospects of zirconia for oral implants —A review. Dent. Mater. J. 39, 37–45 (2020)
Hirano, T., Sasaki, H., Honma, S., Furuya, Y., Miura, T., Yajima, Y., et al.: Proliferation and osteogenic differentiation of human mesenchymal stem cells on zirconia and titanium with different surface topography. Dent. Mater. J. 34, 872–880 (2015)
Delgado-Ruiz, R.A., Calvo-Guirado, J.L., Abboud, M., Ramirez-Fernandez, M.P., Mate-Sanchez, J.E., Negri, B., et al.: Histologic and Histomorphometric Behavior of Microgrooved Zirconia Dental Implants with Immediate Loading. Clin. Implant Dent. Relat. Res. 16, 856–872 (2014 Dec)
Nishihara, H., Haro Adanez, M., Att, W.: Current status of zirconia implants in dentistry: preclinical tests. J. Prosthodont. Res. 63, 1–14 (2019)
Soon, G., Pingguan-Murphy, B., Lai, K.W., Akbar, S.A.: Review of zirconia-based bioceramic: Surface modification and cellular response. Ceram. Int. 42, 12543–12555 (2016)
Rezaei, N.M., Hasegawa, M., Ishijima, M., Nakhaei, K., Okubo, T., Taniyama, T., et al.: Biological and osseointegration capabilities of hierarchically (meso-/micro-/nano-scale) roughened zirconia.Int J Nanomedicine. 2018 Jun;Volume13:3381–95
Jinyang Xu*, M., Ji, L., Li, Y., Wu, Q., Yu, M., Chen: Improving wettability, antibacterial and tribological behaviors of zirconia ceramics through surface texturing. Ceram. Int. 48(3), 3702–3710 (2022)
Ji, M., Zhang, H., Xu*, J., Li, C., Yu, D., Chen, M., Mohamed El Mansori:. Toward the mechanisms of surface texturing on the wear behavior of dental zirconia ceramics under dry and saliva lubricated conditions.Wear,484–485: 203845. (2021)
Pellegrini, G., Francetti, L., Barbaro, B., del Fabbro, M.: Novel surfaces and osseointegration in implant dentistry. J. Investig Clin. Dent. 9, e12349 (2018 Nov)
Rompen, E., Domken, O., Degidi, M., Farias Pontes, A.E., Piattelli, A.: The effect of material characteristics, of surface topography and of implant components and connections on soft tissue integration: a literature review. Clin. Oral Implants Res. 17, 55–67 (2006 Oct)
de Souza, V.Z., Manfro, R., Joly, J.C., Elias, C.N., Peruzzo, D.C., Napimoga, M.H., et al.: Viability and collagen secretion by fibroblasts on titanium surfaces with different acid-etching protocols. Int. J. Implant Dent. 5, 0–5 (2019)
Gómez-Florit, M., Ramis, J.M., Xing, R., Taxt-Lamolle, S., Haugen, H.J., Lyngstadaas, S.P., et al.: Differential response of human gingival fibroblasts to titanium- and titanium-zirconium-modified surfaces. J. Periodontal Res. 49, 425–436 (2014 Aug)
Delgado-Ruíz, R.A., Gomez Moreno, G., Aguilar-Salvatierra, A., Markovic, A., Mate-Sánchez, J.E., Calvo-Guirado, J.L.: Human fetal osteoblast behavior on zirconia dental implants and zirconia disks with microstructured surfaces. An experimental in vitro study.Clin Oral Implants Res. 2016Nov;27:e144–53
Iinuma, Y., Hirota, M., Hayakawa, T., Ohkubo, C.: Surrounding tissue response to surface-treated zirconia implants. Mater. (Basel). 13, 30 (2020)
Rezaei, N.M., Hasegawa, M., Ishijima, M., Nakhaei, K., Okubo, T., Taniyama, T., et al.: Biological and osseointegration capabilities of hierarchically (Meso-/micro-/nano-scale) roughened zirconia. Int. J. Nanomedicine. 13, 3381–3395 (2018)
Taniguchi, Y., Kakura, K., Yamamoto, K., Kido, H., Yamazaki, J.: Accelerated Osteogenic Differentiation and Bone Formation on Zirconia with Surface Grooves Created with Fiber Laser Irradiation.Clin Implant Dent Relat Res. 2016 Oct1;18:883–94
Schünemann, F.H., Galárraga-Vinueza, M.E., Magini, R., Fredel, M., Silva, F., Souza, J.C.M., et al.: Zirconia surface modifications for implant dentistry. Mater. Sci. Eng. C. 98, 1294–1305 (2019 May)
Albrektsson, T., Wennerberg, A.: On osseointegration in relation to implant surfaces.Clin Implant Dent Relat Res. 2019 Mar28;21:4–7
Hafezeqoran, A., Koodaryan, R.: Effect of Zirconia Dental Implant Surfaces on Bone Integration: A Systematic Review and Meta-Analysis. Biomed. Res. Int. 2017, 1–12 (2017)
Damiati, L., Eales, M.G., Nobbs, A.H., Su, B., Tsimbouri, P.M., Salmeron-Sanchez, M., et al.: Impact of surface topography and coating on osteogenesis and bacterial attachment on titanium implants. J Tissue Eng. 2018 Jan 2;9:204173141879069
Albrektsson, T., Jemt, T., Mölne, J., Tengvall, P., Wennerberg, A.: On inflammation-immunological balance theory—A critical apprehension of disease concepts around implants: Mucositis and marginal bone loss may represent normal conditions and not necessarily a state of disease. Clin. Implant Dent. Relat. Res. 21, 183–189 (2019)
Faria, D., Madeira, S., Buciumeanu, M., Silva, F.S., Carvalho, O.: Novel laser textured surface designs for improved zirconia implants performance. Mater. Sci. Eng. C. 108, 110390 (2020)
Fernandes, B.F., da Cruz, M.B., Marques, J.F., Madeira, S., Carvalho, Ã., Silva, F.S., et al.: Laser Nd:YAG patterning enhance human osteoblast behavior on zirconia implants.Lasers Med Sci. ; (2020)
Peñarrieta-Juanito, G., Cruz, M., Costa, M., Miranda, G., Marques, J., Magini, R., et al.: A novel gradated zirconia implant material embedding bioactive ceramics: Osteoblast behavior and physicochemical assessment [Internet]. Vol. 1, Materialia. Elsevier B.V.; [cited 2019 Nov 2]. p. 3–14. (2018)
Faul, F., Erdfelder, E., Lang, A.G., Buchner, A.: G*Power 3: A flexible statistical power analysisprogram for the social, behavioral, andbiomedical sciences. Behav. Res. Methods. 39, 175–191 (2007)
Peñarrieta-Juanito, G.M., Costa, M., Cruz, M., Miranda, G., Henriques, B., Marques, J., et al.: Bioactivity of novel functionally structured titanium-ceramic composites in contact with human osteoblasts. J. Biomed. Mater. Res. Part. A. 106, 1923–1931 (2018 Jul)
da Cruz, M.B., Marques, J.F., Fernandes, B.F., Costa, M., Miranda, G., da Mata, A.D.S.P., et al.: Gingival fibroblasts behavior on bioactive zirconia and titanium dental implant surfaces produced by a functionally graded technique. J. Appl. Oral Sci. 28, 1–10 (2020)
da Cruz, M., Marques, J., Peñarrieta-Juanito, G., Costa, M., Souza, J., Magini, R., et al.: Hard and Soft Tissue Cell Behavior on Polyetheretherketone, Zirconia, and Titanium Implant Materials. Int. J. Oral Maxillofac. Implants. 34, 39–46 (2019 Jan)
Corvino, E., Pesce, P., Mura, R., Marcano, E., Canullo, L.: Influence of Modified Titanium Abutment Surface on Peri-implant Soft Tissue Behavior: A Systematic Review of In Vitro Studies. Int. J. Oral Maxillofac. Implants. 35, 503–519 (2020)
Cho, Y.D., Shin, J.C., Yoon, H.I., Ku, Y., Ryoo, H.M., Kim, D.J., et al.: Characterization of human gingival fibroblasts on zirconia surfaces containing niobium oxide. Mater. (Basel). 8, 6018–6028 (2015)
Esfahanizadeh, N., Motalebi, S., Daneshparvar, N., Akhoundi, N., Bonakdar, S.: Morphology, proliferation, and gene expression of gingival fibroblasts on Laser-Lok, titanium, and zirconia surfaces. Lasers Med. Sci. 31, 863–873 (2016)
Wang, Y., Zhang, Y., Miron, R.J.: Health, Maintenance, and Recovery of Soft Tissues around Implants. Clin. Implant Dent. Relat. Res. 18, 618–634 (2016)
Agarwal, S., Baran, C., Piesco, N.P., Quintero, J.C., Langkamp, H.H., Johns, L.P., et al.: Synthesis of proinflammatory cytokines by human gingival fibroblasts in response to lipopolysaccharides and interleukin-1β. J. Periodontal Res. 30, 382–389 (1995 Nov)
Bartold, P.M., Narayanan, A.S.: 2006 Feb;40:29–49. (2000)
Bartold, P.M., Haynes, D.R.: Interleukin-6 production by human gingival fibroblasts.J Periodontal Res. 1991Jul;26:339–45
Cionca, N., Hashim, D., Cancela, J., Giannopoulou, C., Mombelli, A.: Pro-inflammatory cytokines at zirconia implants and teeth. A cross-sectional assessment.Clin Oral Investig. 2016 Nov2;20:2285–91
Acknowledgements
This work was supported by the FCT (Foundation for Science and Technology, Portugal) with the reference FunImp project 01-0145-FEDER-030498.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marques, A.F.S., Loureiro, F.A.P., Sahoo, N. et al. Nd-YAG Laser Texturing of Zirconia Implant Surfaces. Lasers Manuf. Mater. Process. 10, 1–18 (2023). https://doi.org/10.1007/s40516-022-00191-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40516-022-00191-5