Abstract
Previous literature documented that interpersonal strain arising from caregiving roles can negatively impact caregivers’ health and well-being, and interpersonal support can buffer this association. Using a social network approach, we evaluated interpersonal strain due to malfeasant and nonfeasant care-related interactions and behaviors and interpersonal support through uplifting care-related interactions and behaviors. We investigated whether caregivers’ perceptions of network members’ malfeasant, nonfeasant, and uplifting interactions and behaviors were associated with caregivers’ expectations regarding social network members’ involvement in caring for a child with a rare or undiagnosed disease. Qualitative data was further utilized to explain how caregivers interpret these concepts. One hundred sixty-six (n = 166) primary caregivers providing care to 104 relatives diagnosed with a rare genetic or undiagnosed disease were recruited through ongoing research, advocacy groups, and family referrals. Caregivers provided information about 2,806 familial network members and interactions with them. For each network member, perceived contribution to caregiving and whether the contributions met caregivers’ expectations, and interactions representing nonfeasance, malfeasance, and uplift were assessed. Confirmatory factor analysis for malfeasance, nonfeasance, and uplift demonstrated high construct validity for each and construct correlations were significant. Caregivers reported that network members whose care role contribution did not meet expectations were more likely to engage in malfeasance and nonfeasance (Odds Ratios range between 0.02 and 0.09, ps < 0.001); whereas network members providing uplift were meeting caregivers’ support expectations (OR = 1.98; p = 0.024). Thematic analysis demonstrated that respondents’ expectations of each network members’ care role involvement derived from social roles and attributes of both the network members and the child. These findings can inform strategies that maximize opportunities for interpersonal support and minimize interpersonal strain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is estimated that 19.2% of children in the United States are affected by at least one chronic condition, many of which are rare genetic or undiagnosed conditions (Data Resource Center for Child and Adolescent Health, 2018). In the United States, a rare disease is one that affects fewer than 200,000 people (Shimkus, 2002). It is estimated that there are about 7000 known rare diseases, 80% of which have a genetic etiology (Elliott, 2020; Ferreira, 2019). Approximately two-thirds of these rare conditions affect children (Nguengang Wakap et al., 2020). While many diagnosed with pediatric rare diseases die before reaching the age of 5 years, many also live into adulthood (Elliott, 2020). Taken together, it is estimated that 30 million people in the United States are living with a rare disease, half of whom are children (GAO, 2021).
Most rare diseases begin in childhood. Notably, the diagnostic odyssey for children with rare disease can be difficult and delayed (Schieppati et al., 2008; Valdez et al., 2016). Those affected by rare or undiagnosed conditions are often dependent on their parents and other family members to care for them in their daily lives across their life course. Family caregivers perform a wide range of care-related tasks. Not only do they help their relative with activities of daily living, but they also take on the role of expert, educator, and advocate (Bush et al., 2022; Whiting et al., 2018). As expert, caregivers perform complex medical tasks, often due to limited access to formal care support services. And, given the rarity of such conditions, caregivers are also called upon to educate health professionals about their relative’s condition and advocate for them with respect to treatment, intervention, and quality of life. Parental caregivers of children with rare genetic conditions experience greater distress and reduced well-being relative to parental caregivers of children with other chronic conditions or who are typically developing (Fitzgerald & Gallagher, 2022). Similarly, the 2018 National Alliance for Caregiving Rare Disease Report indicates that caregivers caring for a relative with a rare disease have significantly higher levels of caregiver burden than other caregivers (Whiting et al., 2018). Thus, understanding the experiences of rare disease caregivers is a necessary first step in developing strategies to reduce distress and improve their well-being.
It is well documented that many families experience various health and social consequences in response to providing care to their relatives. For example, caregivers of children with chronic conditions experience elevated levels of depression and parenting stress, as well as increased time constraints and financial burdens (Cohn et al., 2020; Pinquart, 2018a; Pinquart, 2018b; Zan & Scharff, 2015). Despite the challenges of caregiving, families often adjust and discover many benefits. For example, having a child with a chronic condition may foster greater teamwork and thus family cohesion (Chernoff et al., 2001). Caregivers perceive benefits from their caregiving experience and increased appreciation for life by focusing on positivity (Green, 2007; Larson, 2010). With a positive outlook as well as the use of outside resources such as social support, caregivers may exhibit resilience and have the ability to cope with demanding situations (Lin et al., 2013; Manalel et al., 2022). Understanding the factors that are important to such outcomes is key to reducing the negative impacts of caregiving and promoting the positive.
Caregiving and its impact on families has been most extensively studied in the context of older adult caregiving, including older adults living with dementia. In this literature, the Stress Process Model has been found useful to understand how caregiving impacts caregivers’ health and well-being as they care for adults with functional limitations (Lazarus & Folkman, 1984; Pearlin et al., 1990). This model identifies factors that affect how families cope with the stress of caregiving, illuminating potential strategies that can lead to successful adaptation and satisfying caregiving experiences. According to the Stress Process Model, caregiver attributes and their social contexts, primary stressors associated with caregiving tasks, secondary stressors arising from care roles such as interpersonal conflicts, and coping resources and capabilities impact caregivers’ health outcomes (Pearlin et al., 1990).
In the context of dementia caregiving, direct caregiving tasks such as helping with daily activities (e.g., eating, dressing, bathing, medical care) have been identified as primary stressors whereas conflicts with other family members and professional care providers regarding caregiving can act as secondary stressors (Ory et al., 1999; Pearlin et al., 1990). In addressing these stressors, social support from family and others are important coping resources that buffer the impact of both primary and secondary stressors on caregiver health. Social support that is directed towards caregiving behaviors and interactions has been described in the literature as uplifting care-related interactions and behaviors (Ashida et al., 2018; Brody et al., 1989), and satisfaction with social support received has been linked to fewer depressive and anxiety symptoms (Razurel & Kaiser, 2015). On the other hand, limited engagement of family members in caregiving tasks and care-related conflicts were negatively associated with caregivers’ psychological well-being (Ashida et al., 2018; Brody et al., 1989).
In the current paper, we focus specifically on these interpersonal mechanisms that reflect both secondary stressors, such as difficulties with family relationships, and coping resources, such as caregiving related support. According to the Stress Process Model (Pearlin et al., 1990), secondary stressors can be interpersonal in nature and may relate to disagreements about caregiving interactions and behaviors (i.e., malfeasance) or disengagement in the caregiving process (i.e., nonfeasance) (Ashida et al., 2018; Brody et al., 1989). At the same time, as the Stress Process Model posits, interpersonal mechanisms can also be coping resources, often leveraged through uplifting care-related social support. Understanding the characteristics of interpersonal interactions that family caregivers have with their personal network members is important to inform strategies for maximizing interactions that facilitate coping and minimizing interactions that act as secondary stressors.
The concepts of malfeasance, nonfeasance, and uplift were first introduced by Brody and colleagues in their qualitative study evaluating inter-sibling interactions in the context of older parent care (Brody et al., 1989). Building upon this initial work, Ashida and colleagues considered these interpersonal mechanisms within the broader caregiving network and evaluated whether the quality of care-related interactions can explain caregivers’ perceptions of the extent to which network members meet their expectations. For example, whether they have uplifting interactions such as helping with care or showing appreciation to the caregiver (uplift), conflictual interactions such as receipt of unwanted advice or criticism (malfeasance), or care-related disengagement such as not checking in or not showing appreciation (nonfeasance) (Ashida et al., 2018). Consistent with the Stress Process Model, this prior work also demonstrated that caregivers report poorer well-being when they perceive that network members are not meeting care-related expectations. However, this previous literature focused on caring for adults, primarily in the context of dementia. There is limited research examining aspects of the Stress Process Model in the context of caring for a relative with a rare or undiagnosed condition, particularly the interpersonal mechanisms that may function as secondary stressors or coping resources.
Here, we use an ego-centered network approach and measures of malfeasance, nonfeasance and uplift previously developed in the context of dementia caregiving, to investigate caregivers’ interpersonal landscape as it relates to secondary stressors (i.e., malfeasance and nonfeasance) and coping resources (i.e., uplift). Specifically, we address three primary aims. First, we aim to confirm whether the items comprising these subscales (Ashida et al., 2018) hold in the context of caring for a relative with a rare or undiagnosed condition, a population that has not been widely studied in caregiving research. Second, to assess the relevance of these secondary stressors and coping resources, we determine whether malfeasant, nonfeasant, and uplifting caregiving interactions and behaviors are associated with caregivers’ expectations of network members’ involvement in specific care roles. We hypothesize that network members who are not meeting caregivers’ expectations with regards to various care roles are more likely to engage in malfeasant and nonfeasant care-related interactions and behaviors, and less likely to engage in uplifting care-related interactions and behaviors – that is, more likely to act as secondary stressors rather than coping resources. Finally, given that the unique experiences of these caregivers have been understudied, we utilize qualitative data to further elucidate how caregivers interpret malfeasant, nonfeasant, and uplifting caregiving interactions and behaviors, with a focus on the care roles network members are expected to play. The qualitative data allows us to assess the relevance of these caregiving interactions to the families caring for relatives with rare or undiagnosed conditions. In doing so, we are better able to understand the extent to which existing knowledge of older adult caregiving may apply to the context of rare conditions that primarily affect children with some moving into adulthood, and whether unique approaches need to be developed to enable interactions that are beneficial to their caregivers.
Methods
Data were collected as part of the Inherited Diseases, Caregiving, and Social Networks protocol at the National Human Genome Research Institute, National Institutes of Health, which investigates the cognitive, emotional, and social factors experienced by caregivers of family members affected by rare genetic or undiagnosed diseases. The study was approved by the Institutional Review Boards of the National Human Genome Research Institute and the National Institutes of Health in the United States. Participants were recruited from ongoing research activities investigating the natural history of children affected by rare inherited metabolic (IM) conditions or undiagnosed diseases (UD), advocacy groups engaging families with relatives affected by rare genetic metabolic conditions, and through family referral. Of the 342 prospective participants referred into study, 282 agreed to participate and were consented into study. Of those consented into study, 79% (n = 222) completed the online survey and semi-structured qualitative interviews.
Procedures
Following the informed consent process, participants completed online survey, an online network enumeration, followed by semi-structured interviews; interviews were conducted either in person or by phone by trained study staff. The online survey evaluated participant demographics, mental and physical health, coping processes, and care roles. Using standard ego-centered network assessment approaches, participants enumerated members of the caregiving network and their own personal network, providing demographic information for each enumerated network member (Valente, 2010). Assessment of network members’ care roles and whether expectations related to care roles were met was conducted through a semi-structured interview specific to network engagement in caregiving for a subset of participants (n = 187) and online for the remainder (n = 35); the semi-structured interview specific to network engagement in caregiving was shifted to an online survey to reduce participant burden. Next, all participants completed a separate semi-structured qualitative interview in which they described the social resources provided by their network members, including interactions describing malfeasant, nonfeasant, and uplifting care-related behaviors. All interviews were transcribed verbatim; personally, identifiable information of network members was redacted from interview transcripts prior to analysis. This study was pre-registered in clinicaltrials.gov [NCT01498263].
For the current report, our sample includes 166 primary caregivers (IM = 143; UD = 23) providing care to 104 relatives with an inherited metabolic or undiagnosed condition (IM = 91; UD = 13). Primary caregiving status was determined by self-nomination (94.6%) or nomination by another participant in response to the question: “Who do you consider to be the primary caregiver or caregivers to [relative]?” A total of 269 network members were enumerated as primary caregivers (M = 2.6 per family), 62% of whom participated in the current study. Most primary caregivers participating in this study are parents (91.6%), with 6.0% being grandparents. Table 1 summarizes sample characteristics. The majority are female (65.2%), white (86.7%) and married (90.1%). Just over half (58.0%) were employed full-time. Each participant enumerated an average 19.55 network members in their social network; on average about 9 of these network members were family members. Caregivers were caring for relatives who were, on average, 11 years of age, and were diagnosed approximately 10 years prior to assessment. Of note, though children at the time of diagnosis, several care recipients were adults over 18 years at the time of assessment (n = 18 of 104). Primary care needs were in social (M = 2.03, Range: 1 to 4) and life skill (M = 2.78, Range 1 to 4) domains (State of Main DHHS, 2011).
Measures
Perceived Caregiving Interactions and Behaviors: Malfeasance, Nonfeasance, Uplift
The Perceived Caregiving Interactions and Behaviors network-based subscales were previously validated in a dementia care context (Ashida et al., 2018). Items assess malfeasant caregiving interactions and behaviors (7 items), nonfeasant interactions and behaviors (4 items), and uplifting interactions and behaviors (8 items). Through interview, participants responded to each item by naming those enumerated network members engaged in the specific caregiving interactions and behaviors. Participants could also indicate if none of their network members engaged in the specific caregiving interactions and behaviors. Responses were recorded such that a ‘1’ was assigned to each network member named in response to the specific item, otherwise a ‘0’ was recorded for that item.
Though not directly asked to elaborate on why or why not certain network members engaged in the elicited interactions or behaviors, the majority of participants (84%) elaborated on their rationale for identifying individual network members as engaging in the specific caregiving interactions and behaviors. The interviews were transcribed verbatim. Participants’ responses to each subscale item were extracted from the transcripts into a database organized by item within construct. A total of 3995 spontaneous utterances (i.e., words other than network member name or a ‘no one’ response) were identified from the transcripts for analysis. These spontaneous utterances were classified as ‘meaningful’ if they included comments about expectations for caregiving, family member involvement, and interpretation of the items assessing malfeasance, nonfeasance, and uplift. The meaningful utterances (n = 882) are the basis of the qualitative themes that provide context for the constructs.
Caregiving Role Expectations
Participants indicated whether each enumerated network member was involved in providing direct care to the care recipient, making care decisions for the care recipient, or providing support to caregivers. As follow-up, participants indicated if the enumerated network member was meeting expectations in their care roles; specifically, were they “helping enough, or should they be doing more or less, with providing care”, “helping enough, or should they be doing more or less, in making decisions about care”, and “helping enough, or should they be doing more or less, in supporting you (the caregiver)”. For the majority of participants (N = 136), care roles and caregiving role expectations were assessed through interview. Transcripts were coded by two independent coders, resulting in high inter-rater reliability (kappa = 0.98) across domains. The remainder (N = 30) responded to these questions within the online enumeration survey.
Analyses
To investigate aim 1 – that is, whether the factor structure previously identified in the dementia care context was observed within the current sample of caregivers (Ashida et al., 2018) – a confirmatory factor analysis (CFA) was fitted, allowing for correlated factors. Two models were fitted, one with uncorrelated errors across items and a second which correlated errors among similar items reflecting opposite sentiments (e.g., who doesn’t spend enough time and who spends enough time). All models controlled for within family clustering, with ordered, categorical specifications for the set of binary items. McDonald’s omegas, rather than Cronbach’s alphas, were calculated for each scale based on the resulting CFA as an index of construct validity, given that this index does not assume tau equivalence among items (Hayes & Coutts, 2020). The CFA models were fitted using the lavaan package (Rosseel, 2012) in the R Statistical System (R Core Team, 2020).
To address aim 2, a series of logistic regression models, which are appropriate for a dichotomous outcome variable, were fitted to evaluate the association between meeting care role expectations for each network member (unmet = 0, met = 1) and the number of malfeasant, nonfeasant and uplifting interactions and behaviors. For each logistic regression, a series of mixed models were estimated to control for clustering of network members within participant and family. All analyses controlled for disease context (i.e., inherited metabolic conditions or undiagnosed diseases), participant age, and the source of the role expectation data (i.e., through interview or online). To assess our hypotheses, we first evaluated the association between the caregiving role expectations and perceived caregiving interactions and behaviors subscales separately, controlling for covariates. We then fitted a multivariate model which included the perceived caregiving interaction and behavior subscales jointly, controlling for covariates. Models were fitted using geepack package (Halekoh et al., 2006) in the R Statistical System (R Core Team, 2020).
To address aim 3, thematic analysis was conducted by subscale using the meaningful utterances for each item comprising the subscale obtained through the semi-structured interview. Coders (LK, SS) read through the utterances to identify themes. The team then discussed themes arising from the coding and identified commonly occurring perceptions, experiences, and interpretations relevant to the interpersonal stress and support constructs across participants. The items prompting exemplar utterances provided in the results are denoted for each quote using item notation from Table 2.
Results
Aim 1. Confirmatory Factor Analysis for Caregiving Interactions and Behaviors Subscales
The modified model with correlated errors resulted in a significantly better fit compared to uncorrelated model (change in chi-squared = 493.08, df = 6), and the fit indices reflect adequate to good fit (Sun, 2005; CFI/TLI > 0.90; RMSEA < 0.06, SRMR < 0.08.). Table 2 provides factor loadings and construct validities. All factor loadings range from 0.40 to 0.95, and construct validities as measured by McDonald’s omega are high (McDonald, 1999). Notably, construct correlations were significant, with malfeasance positively correlated with both nonfeasance (r = 0.39) and uplift (r = 0.45), and nonfeasance negatively correlated with uplift (r = −0.22).
Aim 2. Association between Caregiving Interactions and Behaviors Subscales and Care Role Expectations
When looking at each subscale individually, we observe a negative association between a network member meeting care role expectations and nonfeasance and malfeasance (Odds Ratios range between 0.02 and 0.09, ps < 0.001; see Table 3). Thus, participants indicate that a given network member is not meeting care role expectations – including direct care, decisions about care, and support of the caregiver – when that network member engaged in malfeasant and nonfeasant care-related interactions and behaviors. Participants report that network members are meeting expectations related to support provision when they engage in uplift (OR = 1.98; p = 0.024); however, uplift was not associated with meeting expectations related to direct care or decisions about care. When all three subscales are included in the models, the effect of malfeasance and nonfeasance remain for all care roles, but uplift is no longer significantly related to support role expectations (Table 4). Given the correlation between subscales, these results reflect the effects of a given caregiving interaction and behavior subscale, controlling for the others. Thus, with the positive correlation between uplift and malfeasance, this multivariate model controls for the variance in support role expectations explained by interpersonal ambivalence in close relationships – or when both malfeasant and uplifting behaviors are jointly present.
Aim 3. Describing Caregiving Interactions and Behaviors and How They Relate to Role Expectations
The qualitative data provided a deeper understanding of the decision process caregivers used when responding to the items comprising malfeasant, nonfeasant, and uplifting caregiving interactions and behaviors – overwhelmingly, responses were based on expectations regarding network members’ care involvement. In large part, expectations were adjusted based on their relative’s care needs, and how those care needs aligned with network member attributes. However, socially constructed roles – that is parents, grandparents, and aunts or uncles – also played a large part in setting expectations with regards to how network members are involved, resulting in perceived malfeasance and nonfeasance.
Malfeasance: Experiences with Close Social Ties
Figuring it out together
Interactions characterizing malfeasance were often described as differences in opinions about the child’s abilities and care needs or varying approaches to caregiving among others who are also actively involved in caregiving activities, such as the respondent’s spouse or mother. Several caregivers report that malfeasant interactions often stem from primary stressors of navigating this new role of caring for a child with a rare condition: “-- finding what works is usually trial and error and there’s always a lot of arguing.” [M4]. This process of trial and error can result in caregivers expressing differences of opinion – and often those divergent views are shared among network members who are closest or involved in daily care (“We have differences of opinions on what’s right or wrong or how children, you know, shouldn’t do things, and I think that is frustrating sometimes. But I think that’s normal in probably every parenting situation. (laughter) So, I guess I would say …. maybe the ones that are closest and most involved.” [M2]; “-- I think he’s doing well in one area, and she doesn’t, or vice versa. So, probably she and I, because we have the most, you know, day to day experience with him.” [M1]). At times, these differing opinions result in an expanded view of what is possible, and thus creating opportunities for the child to develop in ways that they might not have thought possible:
“but my husband was really like, No, he needs to try this. I think he can do it. I’ve seen him… And so, you know, it’s not always all or nothing. You know, sometimes it just depends on what it’s about. And you know, as it turns out, my husband was right … And so, sometimes it’s just kind of stepping out. So -- I mean, [my husband] and I might disagree sometimes and have to flesh that out.” [M3].
Strained social ties
Malfeasance was also reported with network members who are not necessarily closely involved in caregiving. One caregiver explained unwanted advice she receives from her mother, “She’s always telling us what we should do. Do this, do that. I’m like, All right, all right. But any mother does that” [M6]. In some cases, caregivers feel that the advice they receive is not always relevant or helpful to their specific situation: “A lot of times she makes comments about how we’re parenting… she doesn’t understand what we’re dealing with, so some of her comments -- she’s trying to be helpful and beneficial -- do kind of hurt feelings. So, I would say [name] is more critical. I mean, she raised … kids with no issues.” [M5]). In other cases, caregivers experience difficulty observing how network members interact with the child, leading to a feeling of malfeasance: “Yeah, that he [grandfather] just has trouble connecting with them and then whenever he is with them, not consistent with them,…sometimes [child] gets angry” [M2].
Nonfeasance: Expectations Based on Social Roles, Family’s Experience and Caregiver Attributes and Capabilities
It’s parents’ responsibility
Many caregivers, primarily parents, reported that they had no expectations that others would participate in caregiving activities, thus, others’ lack of engagement in caregiving activities was mostly justified. In large part, parents felt that they have the primary responsibility to provide care to their children, and others should not be expected to do so: “But those people don’t have to take care of my kid, you know?” [N1]. In these cases, expectations are often considered to be met regardless of the levels of actual involvement: “some of them spend more time with him than others, but they’re still meeting… what I would expect for their relationship with him” [N1]. At the same time caregivers may express dissatisfaction when caregiving responsibilities are not being taken to the full extent. As one caregiver said, “Although, [the child] spends 50 percent of his time at their house, they’re often not there, and pass off responsibilities to daycare and …, and sometimes extended family.” [N1]. Some parents, however, expressed that they sometimes wished they had additional support:
“She’s our child. So, it should fall, but sometimes it, sometimes it’s like some of the help we have where you, like, wish they could do more, and they just either, like, aren’t interested, or they’re not -- or they just don’t understand -- like, they don’t have a background enough to be able to help” [N1].
Being part of the child’s life
When network member involvement does not fall in line with role expectations, caregivers report nonfeasance and disappointment with the network member. Several caregivers talked about their expectations for grandparents to spend more time with their children: “When she [grandmother] comes to visit, she doesn’t really spend much time interacting with the kids” [N2]; “They don’t necessarily come down and visit -- as much as one might expect from retired grandparents who don’t live that far away. I mean, it seems to me that most grandparents would want to take advantage of any opportunity that they had to spend time with their grandkids” [N2]. These statements suggest that caregivers are not necessarily expecting others to perform physical care-related tasks, rather, they want others to be involved or interested in the child’s life, generally. One caregiver also discussed expectations for their sibling based on family traditions, “from my experience growing up, my aunts and uncles were always there for me. And my brother is not there for my kids. And so, I feel like he could be there more for helping him, for taking care of him for a weekend or whatever, if I need a break” [N1]. Thus, caregivers experience nonfeasance when they perceive a general lack of involvement, and their expectations may be shaped not only by socially constructed family roles but also by family’s past experiences.
Characteristics of network members
Network member attributes can result in adjustments to caregivers’ expectations about members’ involvement in caregiving to help caregivers cope, or they can result in distress due to perceptions that expectations are not met. For the former, the network members’ age (“for their age and where they’re at in their life, they feel they help enough” [N1]), geographical proximity (“And, again, it goes back to distance. I think they want to help out more and … would try to help out more if they were closer” [N1]), and time constraints (“my mom wants to spend more time, but she can’t financially take off of work to do it. So, that’s a little more understanding” [N1]) were all characteristics often referred to in caregivers adjusting expectations.
Network member capacity and interests
In addition, caregivers often discussed network members’ knowledge and capabilities to help with care when explaining nonfeasance. Such capabilities were often couched in the individual’s interest in learning about the child’s condition and care needs: “it’s really not something they seem capable of or interested in doing, and that’s fine” [N2]. Caregivers also talked about how some family members may not feel comfortable: “most of them feel scared of the environment, I guess, with [child]” [N2]. And such feelings lead to some caregivers receiving less support even when network members may have time to provide it: “they provide a lot more assistance for my sister’s children than they ever have for mine” [N2]. In some cases, differential capabilities among members can result in unequal distribution of care role involvement that creates concerns for caregivers. As one participant described, “I don’t want to ask my mom…she’s here all week with the kids. And, you know, you can see she’s frustrated when she leaves here. And that shouldn’t be an issue, but it always is. But outside of that, family, brothers, sisters, aunts, uncles, you know, friends, no. There’s no additional support” [N2].
Uplift: Unexpected sources of support
When caregivers generally did not expect others to help with caregiving, they appreciated the support and help spontaneously provided by others, and such support provision led to uplifting experiences:
“my aunt, she -- we only see her once a year, but she never fails to visit when she’s in town, or call, or email -- you know what I mean? So, I would say yes, she does, even though that’s only once a year” [U8].
In addition to the roles that family members play, non-family members also play important and unexpected caregiving roles. This statement from a caregiver -- “I mean, they’ve got lives, too, right? Like, my friend has his own family and three kids. Like, you know, I’d love to talk to him all the time, but, you know, I recognize that I’m probably only going to talk to him once or twice a week” [U8] -- shows that these friends and neighbors are also sources of uplift. Caregivers also highlighted the importance of support provided by others who have similar experiences in caring for a child with chronic health conditions: “I talk to other [condition] moms on Facebook… I think they understand that part. I don’t really talk a lot about it with the other parents because they don’t get it” [U7].
Discussion
We investigated the extent to which social network-based subscales aimed to assess three constructs of interpersonal interactions and behaviors (i.e., malfeasance, nonfeasance, uplift) in older adult caregiving translate to the context of caring for relatives, primarily children, with rare or undiagnosed conditions. The results indicate that the subscales appear to be generalizable to this caregiving context with high construct validity. Furthermore, each subscale assessing the constructs of malfeasance, nonfeasance, and uplift are associated with caregivers’ expectations of each network members’ engagement in care-related activities; members not meeting caregiver’s expectations are more likely to exhibit malfeasant and nonfeasant interactions and behaviors, secondary stressors as described in the Stress Process Model. And, as hypothesized, caregivers reported that expectations of support are met for those who engage in uplifting interactions. These findings suggest that the quality of network members’ care-related interactions and behaviors can partly explain whether caregivers’ expectations of network members’ involvement are satisfied. Thus, these subscales identify care-related interactions and behaviors that can potentially inform strategies to reduce interpersonal strain and improve interpersonal support for family caregivers. For example, questions in subscales ask about network member behaviors, such as calling, visiting, being critical or angry, showing appreciation, and spending or not spending time with their affected relative. Interventions addressing these behaviors with caregivers and/or other family members, likely will influence caregiver expectations that can have implications on their psychosocial well-being (Ashida et al., 2018).
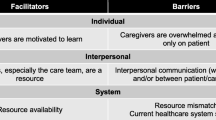
The qualitative data provided an in-depth understanding of how malfeasance, nonfeasance, and uplift operate in the unique context of caring for relatives with rare or undiagnosed diseases and how they intersect with the key elements of the Stress Process Model (i.e., primary stressor, secondary stressor, coping resources). As shown in Figure 1, caregivers explained that primary stressors of caregiving can give rise to malfeasant interactions (secondary stressors) among heavily involved caregivers as multiple people try to do what they believe is best for the child. Interpersonal strain can also arise from nonfeasant behaviors (secondary stressors), when family members are not a part of the child’s life in ways that caregivers view are meaningful. When faced with these primary and secondary stressors, caregivers may cope by either adjusting their expectations for their family members or turning to outside support such as friends or others who also care for a relative with a rare or undiagnosed disease who understand and provide uplift that facilitates coping.
The caregivers explained how the expectations they form about each network member may shape their interpretation of malfeasant, nonfeasant, and uplifting caregiving interactions and behaviors. Often, these expectations stem from network members’ social roles and individual attributes, as well as the care needs of the child. Parents largely see caregiving as their own responsibility and feel that others should not have to help. Because of this belief, parents express difficulties asking for help and try to bear most of the primary caregiving stress on their own without considering available interpersonal coping resources. This makes them vulnerable to caregiving burden as they may not reach out to others for support even when support is available; a finding reported previously (Broese van Groenou et al., 2013). Our results point to the importance of helping caregivers understand the need to address stressors by becoming aware of the presence of primary and secondary stressors, strengthening caregivers’ ability to communicate their needs to others, or by increasing awareness among network members about caregiver needs and how to offer help.
Secondary stressors associated with malfeasant interactions mostly occur among those who are actively involved in caregiving processes. This result points to the possibility that aspects of malfeasant interactions and behaviors may be adaptive as caregivers seek best ways to care for their relative. High levels of involvement among multiple network members can result in a need to resolve differences in opinions on how care should be provided. One might consider differences of opinion among caregivers to reflect divergent thinking, a factor that, in conjunction with convergent thinking, can improve innovation in organizational teams (Cropley, 2006). Though mostly considered in the context of organizational teams, these ideas of divergent and convergent thinking may also be important components to effective caregiving teams. Differences in opinion and approaches among highly involved caregivers can result in positive outcomes as caregivers discuss their differing perspectives and arrive at a shared approach to caregiving. In such contexts, reducing malfeasant interactions and behaviors may not be the goal of intervention.
Role-based expectations were also reported as important considerations in network members’ involvement in care-related activities. For example, parent caregivers generally expected that the grandparents, aunts, and uncles of the child would be part of the child’s life, and experienced secondary stressors when these members did not show interest or were not involved at an expected level, thereby engaging in nonfeasant behaviors. Because the goal of caregiving often focuses on quality of life rather than improving health status of the care-recipient in this context (Nasmith et al., 2013), reducing nonfeasance and improving the quality of family relationships is particularly important for both caregivers and care recipients diagnosed with a rare or undiagnosed condition. Although many caregiver intervention studies focused on reducing malfeasant interactions (Mendenhall & Mount, 2011), our results highlight the value of focusing on nonfeasance as it also appears to function as a secondary stressor. It is important to increase awareness among network members about the benefits of social interactions even when they may not help with direct care.
There were two ways in which caregivers coped with primary and secondary stressors associated with caring for their relative: adjusting expectations for family network member participation and seeking uplifting interactions from non-family network members. Caregivers reported adjusting their expectations based on the network members’ attributes and how they match to the needs of the care recipient. Caregivers sometimes justified non-participation of network members based on physical distance, time limitations, and their interest and ability to interact with the child with illness. In some cases, caregivers noted that individuals not knowing how to interact with the child effectively causes stress to the child and the caregivers themselves; in turn, caregivers will reduce the opportunity for those individuals to see the child. Such characteristics as geographic distance and limited time have also been identified in previous literature as barriers to caregiving support provision within networks (Brown & Murphy, 2018; Joseph & Hallman, 1998). Our study further provides insight into how caregivers refer to these factors to justify the presence of unmet expectations to cope with the impact of secondary stressors.
Caregivers reported little or no expectations for non-family members to be involved in direct care or care decisions, and experienced uplift when non-family network members provided support. Other caregivers, outside of the family, were identified as especially important sources of uplift as they shared similar experiences and knew what types of support and information were needed, serving as important outside coping resources. The importance of peer caregivers in providing social support to parents of chronically ill children has been documented previously (Acri et al., 2017; Hoagwood et al., 2010). Interactions with other caregiving parents are largely mutual and uplifting. Thus, they likely serve as coping resources to help reduce caregiving burden (Silva et al., 2015). Although parents of children with complex medical conditions value peer support, whether facilitating peer caregiver support would improve their emotional and physical well-being is still unclear (Sartore et al., 2021), and warrants additional investigation.
Limitations
There are several limitations to consider when interpreting these results. Families contributing to this work were recruited through clinical research protocols at the National Institutes of Health in the United States and advocacy groups, so it is important to note the potentially self-selective nature of study participants which may limit generalizability of these results. Our sample was mostly white, limiting our ability to understand how caregiving roles and expectations may vary in families identifying from other racial or ethnic backgrounds. The relatives being cared for by our participants are affected by rare genetic conditions with broad phenotypic variation, which can influence their care needs and thus, the support needs of caregivers. The qualitative data arising from this study are based on participants’ spontaneous utterances, and thus, represent a sampling of the rationales that caregivers use when making determinations that network members engage in nonfeasant, malfeasant, and uplifting interactions and behaviors. Despite these limitations, this study is novel in that it provides important information on the interpersonal landscape surrounding family caregivers of relatives with rare genetic conditions, and the value of a mixed-methods approach to understand their experience.
Practice Implications
Caregivers value close family relationships that contribute to uplift, but family members engaged in uplifting behaviors may also be directly involved in caregiving tasks that lead to expression of differing opinions (i.e., malfeasance). Interventions may need to focus on helping caregivers shift to connective thinking that recognizes the value of these differing opinions and identifies ways to jointly establish strategies to reach common care goals, such as, the child’s well-being or facilitating their development to their maximum potential (Post et al., 2009). It may also be beneficial to support caregivers in understanding the reasons behind interpersonal conflict and how to effectively collaborate with each other to enhance family functioning and support health and well-being outcomes for those with a rare or undiagnosed condition (Brown et al., 2017). When these secondary stressors (i.e., malfeasance, nonfeasance) occur within the family, it may be necessary for some to turn to outside coping resources to experience uplift. The network approach applied here can be used in a clinical setting by integrating the subscale items into family systems assessments, such as the genogram or colored eco-genetic relationship map (Peters et al., 2006; Joseph et al., 2023). Doing so can help families see the multiplex interactions and behaviors that can arise through their caregiving roles, disentangling how malfeasant interactions stand alone, or intersect either with uplift and nonfeasance and potentially incorporating outside coping resources.
The benefits of increasing uplifting experiences while reducing nonfeasant interactions are clear. However, the importance of addressing nonfeasance has not been considered much in previous caregiving studies. In describing nonfeasance, caregivers discussed the importance of others being a part of the child’s life rather than providing direct assistance in caregiving. Caregivers also value emotional support, an interpersonal coping resource (James et al., 2002). Interventions that consider these interpersonal mechanisms to facilitate caregiver well-being may help caregivers (1) become aware of behaviors representing nonfeasance among the network members, (2) consider what their expectations may be for those members, and (3) communicate their desire for how the members may interact with the child and the family. Such training can be especially beneficial for caregivers who feel that they should assume all caregiving responsibilities empowering them to effectively communicate their needs and desires for others’ involvement. Doing so can potentially increase the frequency of uplifting experiences that can ultimately help improve their health and quality of life (Collins et al., 2020; Hatzmann et al., 2009). As well, family members may benefit from interventions that help them identify how they may be more involved in ways other than direct care provision, such as checking in frequently and showing appreciation (Ashida et al., 2018).
Research Implications
Future work should investigate the role of these caregiving interactions and behaviors in the broader Stress Process Model, investigating whether the secondary stressors of interpersonal strain relate to caregiver well-being and health, and if care-related uplift buffers the stress response. Given recent work suggesting that caregivers of individuals with rare disease may be particularly vulnerable to negative health outcomes (Fitzgerald & Gallagher, 2022), comparative work that identifies whether such vulnerabilities are due to differences in primary and secondary stressors, or coping resources, across different disease contexts (e.g., autism, ADHD, cerebral palsy) may be a fruitful avenue of inquiry. Here we found that aspects of malfeasance, nonfeasance, and uplift may coexist within relationships which represent multiplex network ties, pointing to a need to understand these network ties and investigate how they jointly impact caregiver well-being. For example, future work might investigate whether malfeasance, when embedded in uplift, adaptive in some caregiving contexts. Obtaining rich qualitative data in such efforts will help clarify the meaning of patterns in interpersonal strain and support and provide insights into what strategies should be used to reduce caregiver burden. Though we used the term malfeasance throughout this paper to be consistent with prior literature, qualitative efforts can also identify caregivers’ perceived intentionality of these interactions and behaviors, potentially distinguishing between, for example, malfeasant and misfeasant care-related interactions and behaviors. Finally, an intervention study can assess whether reducing the interpersonal stress associated with malfeasance and nonfeasance by adjusting expectations or shifting behaviors towards uplift lead to better caregiver and care-recipient well-being.
Data availability
The data that support the findings of this study are available from the senior author upon reasonable request.
References
Acri, M., Zhang, S., Adler, J. G., & Gopalan, G. (2017). Peer-delivered models for caregivers of children and adults with health conditions: a review. Journal of Child and Family Studies, 25(2), 337–344. https://doi.org/10.1007/s10826-016-0616-1.
Ashida, S., Marcum, C. S., & Koehly, L. M. (2018). Unmet expectations in Alzheimer’s family caregiving: interactional characteristics associated with perceived under-contribution. The Gerontologist, 58(2), e46–e55. https://doi.org/10.1093/geront/gnx141.
Brody, E. M., Hoffman, C., Kleban, M. H., & Schoonover, C. B. (1989). Caregiving daughters and their local siblings: perceptions, strains, and interactions. The Gerontologist, 29(4), 529–538.
Broese van Groenou, M. I., de Boer, A., & Iedema, J. (2013). Positive and negative evaluation of caregiving among three different types of informal care relationships. European Journal of Ageing, 10(4), 301–311. https://doi.org/10.1007/s10433-013-0276-6.
Brown, A., Crowe, L., Boneh, A., & Anderson, V. (2017). Parent coping and the behavioural and social outcomes of children diagnosed with inherited metabolic disorders. JIMD Reports, 31, 29–36. https://doi.org/10.1007/8904_2016_544.
Brown, C. R., & Murphy, M. M. (2018). Barriers to informal caregiving of persons living with dementia in barbados: a phenomenological inquiry. West Indian Medical Journal, 67(3), 206–211.
Bush, L., Davidson, H., Gelles, S., Lea, D., & Koehly, L. M. (2022). Experiences of families caring for children with newborn screening-related conditions: implications for the expansion of genomics in population-based neonatal public health programs. International Journal of Neonatal Screening, 8(2). https://doi.org/10.3390/ijns8020035.
Chernoff, R. G., List, D. G., DeVet, K. A., & Ireys, H. T. (2001). Maternal reports of raising children with chronic illnesses: the prevalence of positive thinking. Ambulatory Pediatrics, 1(2), 104–107. https://doi.org/10.1367/1539-4409(2001)001<0104:mrorcw>2.0.co;2.
Cohn, L. N., Pechlivanoglou, P., Lee, Y., Mahant, S., Orkin, J., Marson, A., & Cohen, E. (2020). Health outcomes of parents of children with chronic illness: a systematic review and meta-analysis. Journal of Pediatrics, 218, 166–177.e162. https://doi.org/10.1016/j.jpeds.2019.10.068.
Collins, A., Burchell, J., Remedios, C., & Thomas, K. (2020). Describing the psychosocial profile and unmet support needs of parents caring for a child with a life-limiting condition: a cross-sectional study of caregiver-reported outcomes. Palliative Medicine, 34(3), 358–366. https://doi.org/10.1177/0269216319892825.
Cropley, A. (2006). In praise of convergent thinking. Creativity Research Journal, 18, 391–404. https://doi.org/10.1207/s15326934crj1803_13.
Data Resource Center for Child and Adolescent Health (2018). Child and Adolescent Health Measurement Initiative. 2018 National Survey of Children’s Health (NSCH) data query. www.childhealthdata.org. Retrieved 4/28/21, from U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB).
Elliott, A. M. (2020). Genetic counseling and genome sequencing in pediatric rare disease. Cold Spring Harbor Perspectives in Medicine, 10(3). https://doi.org/10.1101/cshperspect.a036632
Ferreira, C. R. (2019). The burden of rare diseases. American Journal of Medical Genetics A, 179(6), 885–892. https://doi.org/10.1002/ajmg.a.61124. Jun.
Fitzgerald, J., & Gallagher (2022). Parental stress and adjustment in the context of rare genetic syndromes: a scoping review. Journal of Intellectual Disabilities, 26(2), 522–544.
GAO. (2021). Rare diseases: although limited, available evidence suggests medical and other costs can be substantial. https://www.gao.gov/assets/gao-22-104235.pdf.
Green, S. E. (2007). “We’re tired, not sad”: benefits and burdens of mothering a child with a disability. Social Science & Medicine, 64(1), 150–163. https://doi.org/10.1016/j.socscimed.2006.08.025.
Halekoh, U., Højsgaard, S., & Yan, J. (2006). The R package geepack for generalized estimating equations. Journal of Statistical Software, Foundation for Open Access Statistics, 15(2), 1–11.
Hatzmann, J., Valstar, M. J., Bosch, A. M., Wijburg, F. A., Heymans, H. S., & Grootenhuis, M. A. (2009). Predicting health-related quality of life of parents of children with inherited metabolic diseases. Acta Paediatrica, 98(7), 1205–1210. https://doi.org/10.1111/j.1651-2227.2009.01269.x.
Hayes, A. F., & Coutts, J. J. (2020). Use omega rather than Cronbach’s alpha for estimating reliability. But. Communication Methods and Measures, 14(1), 1–24. https://doi.org/10.1080/19312458.2020.1718629.
Hoagwood, K. E., Cavaleri, M. A., Serene Olin, S., Burns, B. J., Slaton, E., Gruttadaro, D., & Hughes, R. (2010). Family support in children’s mental health: a review and synthesis. Clinical Child and Family Psychology Review, 13(1), 1–45. https://doi.org/10.1007/s10567-009-0060-5.
James, K., Keegan-Wells, D., Hinds, P. S., Kelly, K. P., Bond, D., Hall, B., & Speckhart, B. (2002). The care of my child with cancer: parents’ perceptions of caregiving demands. Journal of Pediatric Oncology Nursing, 19(6), 218–228. https://doi.org/10.1177/104345420201900606.
Joseph, B., Dickenson, S., McCall, A., & Roga, E. (2023). Exploring the therapeutic effectiveness of genogram in family therapy: a literature review. The Family Journal, 31(1), 21–30.
Joseph, A. E., & Hallman, B. C. (1998). Over the hill and far away: distance as a barrier to the provision of assistance to elderly relatives. Social Science & Medicine, 46(6), 631–639. https://doi.org/10.1016/s0277-9536(97)00181-0.
Larson, E. (2010). Psychological well-being and meaning-making when caregiving for children with disabilities: growth through difficult times or sinking inward. OTJR: Occupation, Participation and Health, 30(2), 78–86. https://doi.org/10.3928/15394492-20100325-03.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer.
Lin, F. Y., Rong, J. R., & Lee, T. Y. (2013). Resilience among caregivers of children with chronic conditions: a concept analysis. Journal of Multidisciplinary Healthcare, 6, 323–333. https://doi.org/10.2147/jmdh.S46830.
Manalel, J. A., Sumrall, S., Davidson, H., Grewal, M., Granovetter, M. A., & Koehly, L. M. (2022). Stress, coping, and positive aspects of caregiving among caregivers of children with rare disease. Psychology and Health, 1-17. https://doi.org/10.1080/08870446.2022.2057494.
McDonald, R. P. (1999). Test theory: a unified treatment. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.
Mendenhall, A. N., & Mount, K. (2011). Parents of children with mental illness: exploring the caregiver experience and caregiver-focused interventions. Families in Society, 92(2), 183–190. https://doi.org/10.1606/1044-3894.4097.
Nasmith, L., Kupka, S., Ballem, P., & Creede, C. (2013). Achieving care goals for people with chronic health conditions. Canadian Family Physician, 59(1), 15–17. 11-13.
Nguengang Wakap, S., Lambert, D. M., Olry, A., Rodwell, C., Gueydan, C., Lanneau, V., Murphy, D., Le Cam, Y., & Rath, A. (2020). Estimating cumulative point prevalence of rare diseases: analysis of the Orphanet database. Eur J Hum Genet, 28(2), 165–173. https://doi.org/10.1038/s41431-019-0508-0.
Ory, M. G., Hoffman Iii, R. R., Yee, J. L., Tennstedt, S., & Schulz, R. (1999). Prevalence and impact of caregiving: a detailed comparison between dementia and nondementia caregivers. The Gerontologist, 39(2), 177–185.
Pearlin, L. L. I., Mullan, J. J. T., Semple, S. S. J., & Skaff, M. M. M. (1990). Caregiving and the stress process: an overview of concepts and their measures. The Gerontologist, 30(5), 583–594.
Peters, J. A., Hoskins, L., Prindiville, S., Kenen, R., & Greene, M. H. (2006). Evolution of the colored ego-genetic relationship map (CEGRM) for assessing social functioning in women in hereditary breast-ovarian (HBOC) families. Journal of Genetic Counseling, 15(6), 477–489.
Pinquart, M. (2018a). Featured article: depressive symptoms in parents of children with chronic health conditions: a meta-analysis. Journal of Pediatric Psychology, 44(2), 139–149. https://doi.org/10.1093/jpepsy/jsy075.
Pinquart, M. (2018b). Parenting stress in caregivers of children with chronic physical condition-A meta-analysis. Stress Health, 34(2), 197–207. https://doi.org/10.1002/smi.2780.
Post, C., De Lia, E., DiTomaso, N., Tirpak, T. M., & Borwankar, R. (2009). Capitalizing on thought diversity for innovation. Research-Technology Management, 52(6), 14–25. https://doi.org/10.1080/08956308.2009.11657596.
Razurel, C., & Kaiser, B. (2015). The role of satisfaction with social support on the psychological health of primiparous mothers in the perinatal period. Women & Health, 55(2), 167–186. https://doi.org/10.1080/03630242.2014.979969.
R Core Team. (2020). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/.
Rosseel, Y. (2012). lavaan: an R package for structural equation modeling. Journal of Statistical Software, Foundation for Open Access Statistics, 48(i02), 1–36.
Sartore, G. M., Pourliakas, A., & Lagioia, V. (2021). Peer support interventions for parents and carers of children with complex needs. Cochrane Database Syst Rev, 12(12), Cd010618. https://doi.org/10.1002/14651858.CD010618.pub2.
Schieppati, A., Henter, J. I., Daina, E., & Aperia, A. (2008). Why rare diseases are an important medical and social issue. Lancet, 371(9629), 2039–2041. https://doi.org/10.1016/s0140-6736(08)60872-7.
Shimkus (2002) Rare diseases act of 2002, https://www.congress.gov/bill/107th-congress/house-bill/4013/titles.
Silva, N., Carona, C., Crespo, C., & Canavarro, M. C. (2015). Caregiving burden and uplifts: a contradiction or a protective partnership for the quality of life of parents and their children with asthma. Journal of Family Psychology, 29(2), 151–161. https://doi.org/10.1037/fam0000071.
State of Maine, Department of Health and Human Services (DHHS) Children’s Behavioral Health Services (2011). Children’s Habilitation Assessment Tool (CHAT). https://www.maine.gov/future/sites/maine.gov.dhhs/files/documents/ocfs/cbhs/provider/word/chat.doc. Accessed 14 January 2016.
Sun, J. (2005). Assessing goodness of fit in confirmatory factor analysis. Measurement and Evaluation in Counseling and Development, 37(4), 240–256. https://doi.org/10.1080/07481756.2005.11909764.
Valdez, R., Ouyang, L., & Bolen, J. (2016). Public health and rare diseases: oxymoron no more. Prev Chronic Dis, 13, E05. https://doi.org/10.5888/pcd13.150491.
Valente, T. W. (2010). Social networks and health: models, methods, and applications. Oxford University Press. https://doi.org/10.1093/acprof:oso/9780195301014.001.0001.
Whiting, C. G., Boice, N., & Weber-Raley, L. (2018). Rare Disease Caregiving in America. https://www.caregiving.org/wp-content/uploads/2020/05/NAC-RareDiseaseReport_February-2018_WEB.pdf.
Zan, H., & Scharff, R. L. (2015). The heterogeneity in financial and time burden of caregiving to children with chronic conditions. Maternal and Child Health Journal, 19(3), 615–625. https://doi.org/10.1007/s10995-014-1547-3.
Acknowledgements
The authors thank Luis Lopez for reading a previous version of this manuscript, as well as Drs. Peter McGuire, Cynthia Tifft, and Charles Venditti for referring the participants in this study. Finally, we thank the participants and their families for their involvement in this study.
Funding
This research was supported by funding from the Intramural Research Program of the National Human Genome Research Institute (ZIAHG200395).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koehly, L.M., Ashida, S., Sumrall, S. et al. Caregiving Interactions and Behaviors in the Care of Children with Rare Genetic or Undiagnosed Conditions. J Child Fam Stud 32, 3501–3514 (2023). https://doi.org/10.1007/s10826-023-02645-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-023-02645-6