Abstract
Purpose
To determine embryo and cycle-specific parameters associated with twin live birth in day 3 cryopreserved double embryo transfer (DET) cycles, and to propose a new prediction model for external validation.
Methods
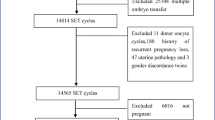
All cycles with autologous or donor cryopreserved DET of day 3 embryos from 2002 to 2011 at a single academic institution with a singleton or twin live birth were included (n = 207). Patient characteristics, post-thaw embryo morphology and freeze-thaw parameters were compared between patients with a single and twin live birth.
Results
Demographic characteristics were similar, except that patients delivering twins were younger at age of cryopreserved embryo transfer (CET), fewer were parous and more were anovulatory. Duration of embryo storage, time in culture post-thaw, endometrial thickness and use of assisted hatching were comparable. Six predictors of twin delivery were identified: patient age <35 year at CET, intact survival of the lead embryo, resumption of mitosis, 7–8 viable cells in the non-lead embryo, transfer of a lead embryo with ≥7 cells and a sum of ≥14 viable cells in the two transferred embryos. Regression modeling predicted a step-wise increase in the probability of twins with addition of each predictor; with all six present, the risk of twins was predicted to be 53 % and with none present, the risk decreased to 6 %.
Conclusions
The six identified variables associated with twin live birth following day 3 cryopreserved DET have been applied to derive a prediction model for estimating the risk of twin delivery. External validation of the model is required prior to clinical application.

Similar content being viewed by others
References
Aflatoonian A, Oskouian H, Ahmadi S, Oskouian L. Can fresh embryo transfers be replaced by cryopreserved-thawed embryo transfers in assisted reproductive cycles? A randomized controlled trial. J Assist Reprod Genet. 2010;27:357–63.
Balaban B, Urman B, Yakin K, Isiklar A. Laser-assisted hatching increases pregnancy and implantation rates in cryopreserved embryos that were allowed to cleave in vitro after thawing: a prospective randomized study. Hum Reprod. 2006;21:2136–40.
Borini A, Bianchi L, Violini F, Maccolini A, Cattoli M, Flamigni C. Oocyte donation program: pregnancy and implantation rates in women of different ages sharing oocytes from single donor. Fertil Steril. 1996;65:94–7.
Burns WN, Gaudet TW, Martin MB, Leal YR, Schoen H, Eddy CA, et al. Survival of cryopreservation and thawing with all blastomeres intact identifies multicell embryos with superior frozen embryo transfer outcome. Fertil Steril. 1999;72:527–32.
Centers for Disease Control and Prevention, American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2009 Assisted Reproductive Technology Success Rates: National Summary and Fertility Clinic Reports. Atlanta: U.S. Department of Health and Human Services; 2011.
Conde-Agudelo A, Belizán JM, Lindmark G. Maternal morbidity and mortality associated with multiple gestations. Obstet Gynecol. 2000;95:899–904.
El-Toukhy T, Khalaf Y, Al-Darazi K, Andritsos V, Taylor A, Braude P. Effect of blastomere loss on the outcome of frozen embryo replacement cycles. Fertil Steril. 2003;79:1106–11.
El-Toukhy T, Coomarasamy A, Khairy M, Sunkara K, Seed P, Khalaf Y, et al. The relationship between endometrial thickness and outcome of medicated frozen embryo replacement cycles. Fertil Steril. 2008;89:832–9.
Gabrielsen A, Fedder J, Agerholm I. Parameters predicting the implantation rate of thawed IVF/ICSI embryos: a retrospective study. Reprod Biomed Online. 2006;12:70–6.
Guerif F, Bidault R, Cadoret V, Couet ML, Lansac J, Royere D. Parameters guiding selection of best embryos for transfer after cryopreservation: a reappraisal. Hum Reprod. 2002;17:1321–6.
Kalra SK, Ratcliffe SJ, Coutifaris C, Molinaro T, Barnhart KT. Ovarian stimulation and low birth weight in newborns conceived through in vitro fertilization. Obstet Gynecol. 2011;118:863–71.
Kaser DJ, Ginsburg ES, Missmer SA, Correia K, Racowsky C. Intramuscular progesterone versus 8% Crinone vaginal gel for luteal phase support for day 3 cryopreserved embryo transfer. Fertil Steril. 2012;98:1464–9.
Kochanek KD, Kirmeyer SE, Martin JA, Strobino DM, Guyer B. Annual summary of vital statistics: 2009. Pediatrics. 2012;129:338–48.
Lannon BM, Choi B, Hacker MR, Dodge LE, Malizia BA, Barrett B, et al. Predicting personalized multiple birth risks after in vitro fertilization-double embryo transfer. Fertil Steril. 2012;98:69–76.
Legro RS, Wong IL, Paulson RJ, Lobo RA, Sauer MV. Recipient’s age does not adversely affect pregnancy outcome after oocyte donation. Am J Obstet Gynecol. 1995;172:96–100.
Leibo SP. A one step method for direct nonsurgical transfer of frozenthawed bovine embryos. Theriogenology. 1984;21:767–90.
Leuhuis E, van der Steeg J, Steures P, Bossuyt PMM, Eijkemans MJC, van der Veen F, et al. Prediction models in reproductive medicine: a critical appraisal. Hum Reprod Update. 2009;15:537–52.
Luke B, Keith LG. The contribution of singletons, twins and triplets to low birth weight, infant mortality and handicap in the United States. J Reprod Med. 1992;37:661–6.
Maheshwari A, Pandey S, Shetty A, Hamilton M, Bhattacharya S. Obstetric and perinatal outcomes in singleton pregnancies resulting from the transfer of frozen thawed versus fresh embryos generated through in vitro fertilization treatment: a systematic review and meta-analysis. Fertil Steril. 2012;98:368–77.
Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Kirmeyer S, Mathews TJ, et al. Births: final data for 2009. Natl Vital Stat Rep. 2011;60:1–104.
Meldrum DR. Female reproductive aging—ovarian and uterine factors. Fertil Steril. 1993;59:1–5.
Moomjy M, Cholst I, Mangieri R, Rosenwaks Z. Oocyte donation: insights into implantation. Fertil Steril. 1999;71:15–21.
Paulson RJ, Hatch IE, Lobo RA, Sauer MV. Cumulative conception and live birth rates after oocyte donation: implications regarding endometrial receptivity. Hum Reprod. 1997;12:835–9.
Racowsky C, Combelles CMH, Nureddin A, Pan Y, Finn A, Miles L, et al. Day 3 and day 5 morphological predictors of embryo viability. Reprod BioMed Online. 2003;6:323–31.
Reichman DE, Jackson KV, Racowsky C. Incidence and development of zygotes exhibiting abnormal pronuclear disposition after identification of two pronuclei at the fertilization check. Fertil Steril. 2010;94:965–70.
Roberts SA, McGowan L, Mark Hirst W, Vail A, Rutherford A, Lieberman BA, et al. Reducing the incidence of twins from IVF treatments: predictive modeling from a retrospective cohort. Hum Reprod. 2011;26:569–75.
Roque M, Lattes K, Serra S, Solà I, Geber S, Carreras R, et al. Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and meta-analysis. Fertil Steril. 2013;99:156–62.
Rozenwaks Z, Davis OK, Damario MA. The role of maternal age in assisted reproduction. Hum Repord. 1995;10:165–73.
Salumets A, Tuuri T, Makinen S, Vilska S, Husu L, Tainio R, et al. Effect of developmental stage of embryo at freezing on pregnancy outcome of frozen-thawed embryo transfer. Hum Reprod. 2003;18:1890–5.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfer in normal responders. Fertil Steril. 2011;96:344–8.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Evidence of impaired endometrial receptivity after ovarian stimulation for in vitro fertilization: a prospective randomized trial comparing fresh and frozen-thawed embryo transfers in high responders. Fertil Steril. 2011;96:516–8.
Shapiro BS, Daneshmand ST, De Leon L, Garner FC, Aguirre M, Hudson C. Frozen-thawed embryo transfer is associated with a significantly reduced incidence of ectopic pregnancy. Fertil Steril. 2012;98:1490–4.
Sibai BM, Hauth J, Caritis S, Lindheimer MD, MacPherson C, Klebanoff M, et al. Hypertensive disorders in twin versus singleton gestations. National Institute of Child Health and Human Development network of maternal-Fetal medicine units. Am J Obstet Gynecol. 2000;182:938–42.
Steer CV, Tan SL, Mason BA, Campbell S. Midluteal-phase vaginal color Doppler assessment of uterine artery impedance in a subfertile population. Fertil Steril. 1994;61:53–8.
Toner JP, Grainger DA, Frazier LM. Clinical outcomes among recipients of donated eggs: an analysis of the U.S. national experience, 1996–1998. Fertil Steril. 2002;78:1038–45.
Williams Z, Banks E, Bkassiny M, Jayaweera SK, Elias R, Veeck L, et al. Reducing multiples: a mathematical formula that accurately predicts rates of singletons, twins, and higher-order multiples in women undergoing in vitro fertilization. Fertil Steril. 2012;98:1474–80.
Young BC, Wylie BJ. Effects of twin gestation on maternal morbidity. Semin Perinatol. 2012;36:162–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
A prediction model has been derived to estimate an individualized risk of twin live birth following transfer of two thawed cleavage stage embryos.
Rights and permissions
About this article
Cite this article
Kaser, D.J., Missmer, S.A., Correia, K.F. et al. Predictors of twin live birth following cryopreserved double embryo transfer on day 3. J Assist Reprod Genet 30, 1023–1030 (2013). https://doi.org/10.1007/s10815-013-0039-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-013-0039-5