Abstract
This systematic review aimed to identify factors significantly associated with the occurrence of epilepsy in autistic individuals and to consider the impact of study quality on findings. Electronic databases were systematically searched on October 2nd, 2020 and records retrieved were limited to those published from 2000 onwards. Study quality was categorised as ‘good’, ‘moderate’ or ‘weak’. Fifty-three studies were included and in studies where the prevalence of epilepsy was reported (n = 257,892), 18,254 (7%) had co-occurring epilepsy. Intellectual disability/cognitive impairment was the most commonly reported risk factor associated with occurrence of epilepsy in autistic individuals. The evidence supporting other, potentially relevant factors was weak and inconsistent and requires further evaluation. Only 9/53 studies were considered ‘good’ quality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Medical comorbidities are more prevalent in autistic individuals than those without autism (Kohane et al., 2012), especially neurological conditions (Pan et al., 2020) of which epilepsy is the most common (Pan et al., 2020); affecting between 12.1% and 17.2% (Lukmanji et al., 2019; Pan et al., 2020) compared with 0.5-1% in the general population. Prevalence estimates vary because studies have used different definitions of epilepsy/autism and assessment methods, but if epilepsy is present it is associated with increased mortality (Hirvikoski et al., 2016) and relatively high health care costs (Peacock et al., 2012). Studies of individuals with epilepsy have also noted an increased prevalence of autism (Strasser et al., 2018).
Epilepsy is a disease of the brain typically defined by the presence of two unprovoked (or reflex) seizures occurring > 24 h apart or the presence of an epilepsy syndrome (Fisher et al., 2014). The point prevalence of active epilepsy is 6.38 per 1,000 persons while the lifetime prevalence was 7.60 per 1,000 persons (Fiest et al., 2017). The prevalence and incidence rate of epilepsy are higher in low to middle income countries (Fiest et al., 2017).
Understanding factors associated with the co-occurrence of epilepsy in autistic individuals may improve identification of epilepsy in autistic individuals and may also aid in defining biological subtypes within autism and in the development of specific targeted interventions (Tye et al., 2019). A previous systematic review and meta-analysis undertaken in 2008 noted that epilepsy in autistic individuals was associated with the presence of intellectual disability and female gender (Amiet et al., 2008). Since this review was published new diagnostic criteria for autism have been published (American Psychiatric Association, 2013). Additionally, the prevalence and incidence of registered diagnoses of autism have increased significantly (Lundström et al., 2015; Russell et al., 2021) in the last 2 decades. These increases likely reflect changes in reporting and how diagnoses are applied and could have an impact on the reported association between epilepsy and autism with respect to associated factors. Thus, the aim of the present systematic review is to identify factors associated with the co-occurrence of epilepsy in autism since 2000. The impact of the quality of the studies assessed on the findings of the present review is also assessed.
Methods
Search Strategy
The current methodology used is a systematic literature review performed according to the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines (Liberati et al., 2009; Moher et al., 2009). Electronic databases PsycINFO, Medline, Web of Science, CINAHL and Cochrane were systematically searched on October 2, 2020 using the following search terms: (autis* or ASD or PDD or asperger* or pervasive developmental disorder*) combined with the ‘autism spectrum disorder’ subject heading and (epilep* or seizure*) combined with the ‘epilepsy’ subject heading. The records retrieved were limited to those available in the English language and published from 2000 onwards. In addition to the electronic search, we conducted a hand search of articles included from the electronic search to identify articles that may not have been indexed in the electronic databases.
Screening of abstracts and full text articles
Records were initially screened by title and abstract by two independent reviewers (CR and EZ) in Covidence (https://app.covidence.org) and then by full text leading to the final set of eligible papers. Predetermined exclusion and inclusion used in both search stages are listed in Supplement 1. Studies that included predominantly participants with neurogenetic syndromes (e.g., Tuberous Sclerosis Complex, Dravet Syndrome, Rett Syndrome) known to have a high association with intellectual disability and the findings of these studies are presented separately (see Supplement 9).
Data extraction
A data extraction form (Supplement 2) was developed to obtain the sample characteristics and main outcomes linked to the co-occurrence of epilepsy in autism in the eligible papers. Details of all studies included in the present review can be found in Table 1, and 2 referring to case-control studies and observational/cohort/cross-sectional studies respectively. For the purposes of this review, case-control studies were defined as studies that include at least two distinct groups of participants, one with autism and one without. Observational/cross-sectional/cohort studies are defined as studies featuring autistic individuals only differing with regards to particular characteristics (such as age or intellectual capacities) and compared in terms of the presence or lack of co-occurring epilepsy.
Study Quality
The quality of the studies reviewed was assessed by two independent reviewers (EZ and CR) on the basis of the National Institutes of Health (NIH) Quality Assessment Tool for Case-Control studies and Observational, Cohort and Cross-Sectional Studies (National Heart, Lung and Blood institute, https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools accessed November 15th 2020). Results of the quality assessment including scoring criteria are described in Tables 1 and 2 and Supplements 3 and 4 for observational/ cross sectional/cohort studies and case control studies respectively.
Data synthesis
Data was synthesised based on Synthesis Without Meta-analysis (SWIM) (Campbell et al., 2020) guidelines (see SWIM checklist Supplement 5).
The factors chosen for inclusion in the synthesis were based on a thorough reading of all full-text articles included in the review by EZ and CR and a previous review and meta-analysis (Amiet et al., 2008). In the absence of consensus, inclusion was also discussed with the wider review team. All included studies had to have at least one outcome determined to be clinically relevant by the review team and the outcome had to have been considered using standard statistical analysis.
All included studies were tabulated and in the tables (Table 3, Supplement 7 or Supplement 8) it was indicated whether or not the factor had been considered in statistical analysis and if so whether it was found to be statistically significant/not significant in relation to the occurrence of epilepsy in autistic individuals. In all studies, factors associated with occurrence of epilepsy in autistic individuals were deemed ‘statistically significant’ at the p < 0.05 level.
Reporting of results in the text were prioritised first with respect to total number of studies where the factor had been considered and then with respect to the quality of these studies.
Results
Search results
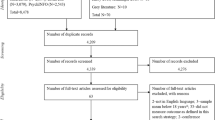
The initial search led to a total of 10,313 records, de-duplicated to 3,587, that were initially screened by two reviewers EZ and CR for relevance by ‘title’ and ‘abstract’. Of these, 3,077 were excluded while 510 were further assessed by full text against the exclusion and inclusion criteria (see Supplement 1). From this full text screening, 457 papers were excluded while the remaining 53 were deemed eligible for the present systematic review. A PRISMA diagram of the search and screening stages along with the reasons for exclusion are detailed in Fig. 1. The PRISMA checklist is in Supplement 6.
Study characteristics
The 53 studies included in the present review included a total of 452,743 autistic individuals. Studies used the DSM-IV (n = 29) followed by the ICD-10 (n = 13), ICD-9 (n = 9), and the DSM-5 (n = 5) criteria to define the presence of autism, with some studies reporting multiple measures. Two studies (Billstedt et al., 2007; Pavone et al., 2004) used the DSM-III and one (Mouridsen et al., 2012) used the ICD-8.
All studies included more males than females. Three studies did not report on the gender distribution of the sample. From those that did, 67% were male (n = 90,934) while 33% were female (n = 45,423). Of the autistic individuals where the prevalence of epilepsy was reported (n = 257,892), 18,254 (7%) had co-occurring epilepsy. In studies which focussed on children with neurogenetic syndromes the prevalence of epilepsy in autistic individuals (n = 5,145) was 26%, highlighting that children with these syndromes are a particularly high-risk group for having co-occurring epilepsy.
Criteria used in the diagnosis of epilepsy included the ICD-8 (n = 2), the ICD-9 (n = 4), the ICD-10 (n = 9), International League Against Epilepsy (ILAE) 1981 criteria (n = 3), ILAE 1989 criteria (n = 5), ILAE (1993) (n = 1), ILAE 2005 criteria (n = 1) criteria, parent questionnaires (n = 6) and reviews of the patients’ medical data, clinical histories and EEG (n = 26), with some studies employing more than one method.
Studies were undertaken in 20 different countries across five continents: North America (19 studies), Europe (18 studies), Asia (12 studies), Oceania (2 studies) and Africa (1 study). The most common country was the USA (19 studies), followed by Denmark (4 studies) and the UK (4 studies). In one study the location was not specified.
Ten studies included adult participants only (19 years or older); 22 studies included child participants only (aged 18 years or younger); and 12 studies included both child and adult participants. In nine studies, participant mean age and range were not reported.
Study characteristics can be found in detail in Tables 1 and 2 referring to case-control studies and observational/cohort/cross-sectional studies respectively.
Quality Assessment
Of the 39 observational, cohort and cross-sectional studies, seven were rated as ‘good’, 27 as ‘moderate’ and five as ‘weak’. The limited timeframe and lack of sample size justification were the most common reasons contributing to ‘moderate’ and ‘weak’ ratings in most studies (see supplement 3). Of the 14 case control studies, two were rated as ‘good’, 11 were rated as ‘moderate’ while the remaining one was deemed ‘weak’. All case control studies lacked sample size justification and blinding (see supplement 4). Detailed results of the quality assessments for observational, cohort and cross-sectional studies and case control studies can be found in supplements 3 and 4 respectively.
Factors Associated with the co-occurrence of Epilepsy and Autism
Details on the factors associated with the co-occurrence of epilepsy and autism can be found in Table 3. Factors are included in the table if they were considered in three or more studies. All factors considered including those only considered in one or two studies are available in supplement 7.
The most frequently considered factor was cognitive level and the presence of intellectual disability (13 studies), followed by gender (12 studies), history of developmental regression (9 studies), the presence of behavioral/psychiatric disorder(s) (7 studies), chronological age (8 studies), injuries/accidents (5 studies) and language (6 studies). Medical/Genetic factors were considered in four studies. Social skills, delayed walking, and family characteristics were considered in three studies. These are described in more detail below. All other factors were considered in two or fewer studies.
Level of Cognition or Presence of Intellectual Disability
Lowered cognitive level or the presence of intellectual disability (ID) was significantly associated with occurrence of epilepsy in 12 of 13 studies where it was considered. The one study where the presence of epilepsy in autistic people was not found to be significantly associated with ID/level of cognition was Ververi et al., (2012). In this study of 222 autistic children aged 1.5-9 years, 17 (8%) had epilepsy and 51 (23%) children had ID. In nine of the 11 studies which found a significant association between epilepsy and ID/Lower level of cognition, the relationship was between presence of epilepsy and ID typically defined as IQ < 70 or as ID recorded in medical registers. In one study which did not employ ID status, Bolton et al., (2011) found that autistic people with epilepsy had significantly lower nonverbal ability IQ as measured by Ravens Matrices (Raven & Court, 1986) than autistic people without epilepsy. Additionally, Pavone et al., (2004) reported that in autistic children and young adults (4–21 years), epilepsy was significantly more common in individuals with IQ < 55 compared with IQ > 55. Parmeggiani et al., (2010) reported that autistic adults and children were more likely to have severe/profound ID (IQ less than 35) than autistic children and adults without epilepsy. Two other studies also reported that epilepsy was significantly more common in individuals with a greater degree of intellectual disability. Danielsson et al., (2005) reported that the cognitive level was significantly lower in adults with epilepsy compared to those without. Among the autistic people with severe ID (IQ < 50), 48% had epilepsy compared with 20% with Mild ID (50–69) and 17% in autistic people without ID (IQ < 70) in this study. Jokiranta et al., (2014) noted that the risk for epilepsy in autistic people significantly increased among more severe cases of ID. Four of the thirteen studies which considered the role of ID/ lowered cognition were considered ‘good’ quality and in all of these studies a lower level of cognition or the presence of ID was associated with an increased occurrence of epilepsy in autistic individuals.
Gender
Gender was a significantly associated with the occurrence of epilepsy in six of 12 studies. For all significant findings with the exception of one study, female gender was associated with an increased risk of the occurrence of epilepsy in autistic individuals. The one exception was Wu et al., (2016) who found an increased risk for epilepsy in males with autism. Study quality was deemed ‘good’ in two of the studies with significant findings (both showed an increased occurrence of epilepsy in female autistic individuals) and ‘moderate’ in the other studies with significant findings.
Developmental Regression
The presence of developmental regression was significantly associated with an increased occurrence of epilepsy in autistic individuals in three of nine studies and not significantly associated in the other six studies. One of the studies which found an increased occurrence of epilepsy in autistic individuals had a ‘good’ rating whilst the other two had a ‘moderate’ rating.
Behavioral/Psychiatric Disorders
The presence of additional behavioral or psychiatric disorders were significantly associated with having epilepsy for autistic individuals in two of the six studies where it was considered. With respect to the type of behavioral/psychiatric disorders considered, the studies tended to combine disorders or included results of broad-based rating scales so no clear patterns with respect to which type of difficulty/disorder might be associated with an increased occurrence of epilepsy in autism were evident. One of the studies which considered the presence of behavioral/psychiatric disorders was considered ‘good’ and it found a significantly increased occurrence of epilepsy in autistic individuals with additional behavioral/psychiatric disorders.
Chronological age
Chronological age was significantly associated with the occurrence of epilepsy in autistic individuals in six of eight studies where it was considered. In five studies increasing age was associated with an increased occurrence of epilepsy in autistic indivdiuals. Two of these studies focused on child populations, two on adult populations and one on a mixed child/adult population. Zhang et al., (2018) found that autistic children aged between 13 and 17 years were more likely to have epilepsy compared with younger children (under 13). McCue et al., (2016) conducted analysis of data from a registry based retrospective cohort study of 731 autistic children (2–18 years) and increasing age was significantly associated with the presence of non-febrile (i.e. epileptic) seizures. Fortuna et al. (2016) collected cross-sectional data on 255 autistic adults aged 18 to 71. Compared to younger autistic adults (aged 18–29), autistic adults aged 40 years and older had an increased prevalence of epilepsy but not compared with those aged 30–39. Bishop et al., (2020) found that for autistic adults there was increasing prevalence with increasing age (until the oldest category (60 years+) in which death likely attenuated estimates. There was however, no association between age and epilepsy prevalence in autistic adults without ID. Parmeggiani et al., (2010) included both autistic adults and children (aged 2–37 years) and noted and a significant association between epilepsy and increasing age. In one study, younger age (3-5years as opposed to 7–9 and 10-12years) was more strongly associated with an increased occurrence of epilepsy (Zhang et al., 2019). None of the studies which considered age received a ‘good’ quality rating. Interestingly, Hara (2007) noted that the median age for epilepsy onset in a sample of 130 autistic adults (18–35 years) was 14 years whilst Parmeggiani et al., (2010) suggested that age of onset of seizures had two peaks (0–5 years and between 10 and 15 years). However, no statistical analyses were reported for these findings.
Injuries/Accidents
The presence of injuries or accidents was significant in two of the five studies where it was considered and not significant in the other three studies. In the two studies where it was significant there was an association between the presence of accidents/injures and an increased risk for epilepsy in autistic individuals. One of the studies where an increased risk for epilepsy was found had a ‘good’ rating whilst the other four studies were ‘moderate’ or ‘weak’.
Language Difficulties
Difficulties with language was associated with the occurrence of epilepsy in autistic individuals in three of the four studies where it was considered. Two of these three studies where a significant association with language difficulties and the occurrence of epilepsy in autistic individuals was found were considered ‘good’ quality and both noted a significant relationship between language difficulties and the co-occurrence of epilepsy and autism. Bolton et al., (2011) followed up 150 autistic individuals diagnosed in childhood at 21 + years. 33 (22%) had developed epilepsy. Language was measured via items from the ADI-R (Rutter et al., 2003) including ‘loss of language skills’and ‘overall level of language’, and the British Picture Vocabulary Scale (BPVS) (Dunn et al. 1982). Epilepsy was significantly more common in individuals with very limited overall level of language and those who had significantly lower verbal ability measured using the BPVS. Oslejeskova et al. (2007) reported on 205 autistic children of whom 64 (31%) had epileptic seizures. Categorization of speech impairment was performed in collaboration with a speech therapist. Epilepsy in autistic children was associated with delay in development of speech as well as with severe language impairment /no development of speech. Shubrata et al., (2015) found that the autistic with children with epilepsy had a greater level of impairment on the Speech and Language domain of the PDD Assessment scale (Grossman R. The PDD Assessment Scale/screening questionnaire 2000 (Available at: http://www.infantsandchildren.net/wp-content/uploads/2009/06/website-autism-formfinal2.pdf) than autistic children without epilepsy. However, Valvo et al. (2016) did not find a relationship between the presence of epilepsy and expressive language development assessed through clinical observation in autistic people (2-21years).
Delayed Walking
Delayed walking was found to be significantly associated with the occurrence of epilepsy in autistic individuals in one of the three studies where it was considered. Bishop et al., (2016) measured delayed walking using information about age of walking from question 5 on the ADI-R (Rutter et al., 2003) which asks “At what age did [subject] walk without holding on?”. Delayed walking was not associated with presence of seizures in the autistic individuals (aged 4–12 years). Saltik et al.’s (2012) definition of delayed walking was based on data from medical records and parental interviews. Autistic people with epilepsy (34%) had a higher rate of delay in onset of independent walking (later than age 18 months) as compared to autistic people without epilepsy (14%). Hara (2007) did not find a relationship between ‘age of walking alone’ and occurrence of epilepsy in autistic adults. All three studies received a ‘moderate’ quality rating.
Social Skills
A greater level of impaired social skills in autistic individuals was associated with an increased occurrence of epilepsy in all three studies where it was considered and one of these studies received a good quality rating. Ko et al., (2016) found that autistic children with epilepsy scored significantly higher on the total score of the Social Responsiveness Scale (SRS; Constanino et al. 2003) than autistic children without epilepsy. Similarly, Shubrata et al., (2015) found that the autistic children with epilepsy had a greater level of impairment on the Social interaction subscale of the PDD Assessment scale (Grossman R. The PDD Assessment Scale/screening questionnaire 2000 (Available at: http://www.infantsandchildren.net/wp-content/uploads/2009/06/website-autism-formfinal2.pdf). Billstedt et al., (2007) found that presence of early onset epilepsy was associated with more impairment on the social interaction items of the DISCO (Diagnostic Interview for Social and Communication disorders; Wing et al. 2002) interview in a follow-up study of autistic adults diagnosed with autism as children.
Family characteristics
Family characteristics were considered in three studies and found to be significant in two studies one of which received a ‘good’ quality rating. In one of the studies with significant findings, an older sibling having autism, an older sibling having epilepsy or an older sibling having both autism and autism were significantly linked to the co-occurrence of epilepsy in autistic individuals (Christensen et al., 2016). In the other study family history of seizures was significantly associated with the co-occurrence of epilepsy (Valvo et al., 2013).
Medical/Genetic factors and Epilepsy in autistic individuals with Neurogenetic Conditions
Medical/Genetic Factors were considered in four studies and were found to be significant in one study. Parmeggiani et al., (2010) found that autistic children and adults with epilepsy had a significantly greater occurrence in cerebral lesions than those without epilepsy. Hara (2007) did not find that birth weight was associated with the co-occurrence of autism and epilepsy, whilst Su et al., (2016) did not find the presence of meningitis and Schuch et al., (2014) the presence of β3 integrin gene variants significantly associated with the co-occurrence. Details of studies where epilepsy was reported in autistic individuals with neurogenetic conditions are in supplement 9. The only factor found to be significantly associated with the co-occurrence was the presence of intellectual disability or lower cognitive level.
Factors found to be significantly associated with the occurrence of epilepsy in autistic individuals in ‘good’ quality studies
All factors associated with the occurrence of epilepsy in individuals with autism in ‘good’ quality studies are shown in supplement 8. Regarding factors considered in less than two ‘good’ quality studies, a significant association between occurrence with epilepsy in autistic individuals was found for severity of autism symptoms (Pavone et al., 2004), increased hospitalisations (Jain et al., 2014) and lowered adaptive behavior (Danielsson et al., 2005).
Discussion
The results of this systematic review suggest that having an intellectual disability or cognitive impairment is the most well-studied and the most frequently associated factor with the occurrence of epilepsy in autistic individuals. A range of other outcomes including female gender, presence of psychiatric/behavioral disorders and older age have been found to be associated with the occurrence, but not in all studies where they have been considered. Additionally, some features including language difficulties and a greater degree of social impairment have been considered less frequently but have been found to be associated with the occurrence in most of the studies where they have been considered. However, these associations were almost universally considered in the absence of attention to the role of intellectual functioning. In general, study quality was frequently ‘weak’ or ‘moderate’ meaning that there is a need for more robust designs including longitudinal studies to better elucidate why certain autistic individuals are at higher risk for epilepsy.
The increased association between epilepsy and autism in individuals with intellectual disability was noted in a previous systematic review (Amiet et al., 2008). When epilepsy and autism coexist, they likely share common pathophysiological mechanisms (Tuchman, 2017), and it is also likely that the occurrence of the two conditions in individuals with intellectual disability involves shared mechanisms for all three conditions (Tuchman, 2017). The mechanisms underlying the increased risks for the co-occurrence of the three conditions are likely to include both environmental and genetic factors (Besag, 2018). We identified a much higher prevalence of epilepsy in autistic individuals who have neurogenetic syndromes associated with intellectual disability (Supplement 9) highlighting that children with genetic syndromes associated with both autism and intellectual disability are a particularly high-risk group for co-occurring epilepsy. This is likely to reflect a shared pathophysiology and impact on early brain development manifesting as epilepsy, autism and intellectual disability. Studies of these conditions have revealed that in some cases early treatments may reduce seizures and intellectual impairments (O’Callaghan et al. 2018; Kotulska et al., 2021) but as of yet there is little data regarding autistic symptoms.
Males are at higher risk for autism than females, but this higher risk is attenuated in individuals with epilepsy (Lukmanji et al., 2019). The results of the current study suggest that female gender may even be a risk factor for the occurrence of epilepsy in individuals with autism. An issue with regard to gender distribution in populations of autistic individuals is the increasing recognition that autistic females have historically been under recognized (Mandy et al., 2012) and this could lead to ascertainment bias in that autistic males are more likely to be diagnosed than females (Schuck et al., 2019). This under recognition of females may also impact the gender distribution with respect to the co-occurrence of both epilepsy and autism.
The co-occurrence of behavioral/psychiatric disorders in individuals with autism is common, affecting more than 70% of individuals with autism (Simonoff et al., 2008), and results of the current review suggest that this occurrence may also increase the risk for epilepsy. Studies have predominantly not focused on individual psychiatric/behavioral disorders, so it is not clear if it is a general risk or a more specific risk. Studies of individuals with ADHD suggest a similar or slightly increased occurrence for epilepsy compared to the non-ADHD population (Socanksi et al. 2013; Davis et al., 2010) but the prevalence is lower than that observed in autistic individuals. Reasons for the higher prevalence of epilepsy in autism compared with ADHD could include that the genetic risk for autism and epilepsy is shared with intellectual disability whereas the risk for ADHD and epilepsy is somewhat different. It will, therefore, be useful to consider the occurrence of epilepsy in individuals with both autism and ADHD as opposed to just autism alone whilst also considering the role of intellectual functioning. Future studies should also examine the association between epilepsy and autism with respect to disorders such as depression likely to emerge in older children and adults.
It has been claimed that ‘developmental regression’ occurs in approximately one in five autistic individuals and in half of these the ‘regression’ is from typical development (Thompson et al. 2019). Developmental regression was significantly associated with occurrence of epilepsy in three of nine studies in the current review. Differences between study samples but also definitions of regression may have led to this mixed finding. It is important that in future studies ‘regression’ is clearly defined to identify whether children with autism who lose or have lost skills have an increased occurrence of epilepsy.
In the current study increasing age was found to be associated with an increased risk for the occurrence of epilepsy in some but not all studies where it was considered. It has been suggested that there may be two peak periods for the development of epilepsy in autism, namely early childhood and adolescence (Hara et al. 2006; Parmegiani et al. 2010), although this second peak in adolescence was not noted in one longitudinal study (Danielsson et al., 2005). Differences between findings are likely to reflect study design but also definitions of both epilepsy and ‘remission’ from epilepsy. More longitudinal studies, which employ accepted definitions of epilepsy and remission, but which also track autism symptoms over time are needed to determine if age of onset of epilepsy in the autistic population is actually different from the onset of epilepsy in the non-autistic population.
Difficulties in language or verbal abilities was significantly associated with the occurrence of epilepsy in some autistic individuals. However, delays or difficulties in language have predominantly been considered using univariable statistical methods and intellectual ability has not been reported or not considered in statistical analysis. It is therefore, unclear if specific difficulties in language are independently associated with an increased occurrence of epilepsy in individuals with epilepsy or whether the co-occurrence is predominantly driven by broader intellectual difficulties. Similarly, it is not known if more difficulties in social skills or delayed walking in individuals with autism is associated with an increased risk for epilepsy independently of difficulties in intellectual functioning.
Future research directions
Study quality was mixed with only one in five of included studies receiving a ‘good’ rating. This highlights the need for more robust study designs. The increase in the incidence and prevalence of registered diagnosed of autism likely due to rising diagnosis among adults, females and higher functioning individuals (Russell et al., 2021; Lundström et al., 2015) highlights the need to consider that cohorts in older studies may not be representative of current diagnostic practices. The use of longitudinal designs following autistic individuals into adulthood will be helpful. Additionally, following children at high risk for autism such as siblings, as well as following children with early onset seizures in the first two years of life will also be helpful in establishing what factors might play a role in the development of epilepsy and autism at different time periods. It is particularly important to use multivariable analysis methods to understand whether language difficulties, motor difficulties or ADHD symptoms are associated with the occurrence of epilepsy in autistic individuals independent of global intellectual impairment. More research is also needed from low- and middle-income countries given the higher incidence of epilepsy but also more challenging conditions with respect to screening and diagnosis in these settings. Additionally, there is a paucity of studies considering the economic impact of having both epilepsy and autism and studies of this nature are needed.
Limitations
We excluded articles not in the English language and could not obtain full texts for a small number of articles which may have been relevant. We did not explore heterogeneity with respect to reported statistical methods, but this was considered in our quality analysis. Employing meta-analytic methods may have yielded more objective results with respect to the nature of relationships between factors associated with the occurrence of epilepsy in autistic individuals. We chose to exclude studies published prior to 2000 as it was felt studies undertaken before this may not reflect the broadening of the concept of autism evident since the publication of DSM-IV in 1994 (American Psychiatric Association, 1994). The chosen exclusion cut-off of prior to 2000 is arbitrary and may have influenced our findings. In relation to autism, we included only studies where individuals were diagnosed with respect to DSM/ICD criteria. However, our inclusion criteria for individuals diagnosed with epilepsy was not as stringent and this may also have impacted on findings. Although we provide basic details of studies that included predominantly participants with neurogenetic syndromes a thorough discussion of neurogenetic conditions associated with autism and epilepsy is beyond the scope of this systematic review.
Conclusions
A wide range of factors were considered with respect to possible factors associated with the occurrence of epilepsy in autistic individuals. The presence of intellectual disability or cognitive impairment is the factor most consistently associated with this occurrence. A number of other factors are potentially important with respect to the occurrence, but study quality and lack of significant findings in all studies where these other factors have been considered means better quality research is needed to establish what factors independent of intellectual impairment are important in the co-occurrence.
References
American Psychiatric Association. (1994). Diagnostic criteria from DSM-IV-TR. American Psychiatric Pub
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders
American Psychiatric Association (1987). Diagnostic and statistical manual of mental disorders, 3rd. revised edn. Washington, DC: American Psychiatric Association,
Amiet, C., Gourfinkel-An, I., Bouzamondo, A., Tordjman, S., Baulac, M., Lechat, P. … Cohen, D. (2008). Epilepsy in autism is associated with intellectual disability and gender: evidence from a meta-analysis. Biological psychiatry, 64(7), 577–582. https://doi.org/10.1016/j.biopsych.2008.04.030
Ayta, S., Gürses, C., Bilgen, Z. T., Kılınçarslan, A., & Eraksoy, M. (2016). The Clinical and Electroencephalography Findings of Children with Pervasive Developmental Disorder. Turkish Journal of Neurology, 22(4), 167–176
Baron-Cohen, S., Wheelwright, S., Skinner, R., Martin, J., & Clubley, E. (2001). The autism-spectrum quotient (AQ): Evidence from asperger syndrome/high-functioning autism, malesand females, scientists and mathematicians. Journal of autism and developmental disorders, 31(1), 5–17. https://doi.org/10.1023/A:1005653411471
Berg, A. T., Berkovic, S. F., Brodie, M. J., Buchhalter, J., Cross, J. H., van Emde Boas, W. … Scheffer, I. E. (2010). Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. https://doi.org/10.1111/j.1528-1167.2010.02522.x
Besag, F. M. (2018). Epilepsy in patients with autism: links, risks and treatment challenges. Neuropsychiatric disease and treatment, 14, 1. https://doi.org/10.2147/NDT.S120509
Billstedt, E., Carina Gillberg, I., & Gillberg, C. (2007). Autism in adults: symptom patterns and early childhood predictors. Use of the DISCO in a community sample followed from childhood. Journal of Child Psychology and Psychiatry, 48(11), 1102–1110. https://doi.org/10.1111/j.1469-7610.2007.01774.x
Bishop, L., McLean, K. J., & Rubenstein, E. (2020). Epilepsy in adulthood: Prevalence, incidence, and associated antiepileptic drug use in autistic adults in a state Medicaid system. Autism, 1362361320942982. https://doi.org/10.1177%2F1362361320942982
Bishop, S. L., Thurm, A., Farmer, C., & Lord, C. (2016). Autism spectrum disorder, intellectual disability, and delayed walking. Pediatrics, 137(3), https://doi.org/10.1542/peds.2015-2959
Bolton, P. F., Carcani-Rathwell, I., Hutton, J., Goode, S., Howlin, P., & Rutter, M. (2011). Epilepsy in autism: features and correlates. The British Journal of Psychiatry, 198(4), 289–294. https://doi.org/10.1192/bjp.bp.109.076877
Campbell, M., McKenzie, J. E., Sowden, A., Katikireddi, S. V., Brennan, S. E., Ellis, S. … Thomson, H. (2020). Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. bmj, 368. https://doi.org/10.1136/bmj.l6890
Christensen, J., Overgaard, M., Parner, E. T., Vestergaard, M., & Schendel, D. (2016). Risk of epilepsy and autism in full and half siblings—A population-based cohort study. Epilepsia, 57(12), 2011–2018. https://doi.org/10.1111/epi.13595
Commission on Classification and Terminology, International League Against Epilepsy. (1981). Proposal for revised clinical and electroencephalographic classification of epileptic seizures. Epilepsia, 22, 489–501
Commission on Classification and Terminology of the International League Against Epilepsy. (1989). Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia, 30, 389–399
Constantino, J. N., Davis, S. A., Todd, R. D., Schindler, M. K., Gross, M. M., Brophy, S. L. … Reich, W. (2003). Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. Journal of autism and developmental disorders, 33(4), 427–433. https://doi.org/10.1023/A:1025014929212
Danielsson, S., Gillberg, I. C., Billstedt, E., Gillberg, C., & Olsson, I. (2005). Epilepsy in young adults with autism: a prospective population-based follow‐up study of 120 individuals diagnosed in childhood. Epilepsia, 46(6), 918–923. https://doi.org/10.1111/j.1528-1167.2005.57504.x
Davis, S. M., Katusic, S. K., Barbaresi, W. J., Killian, J., Weaver, A. L., Ottman, R., & Wirrell, E. C. (2010). Epilepsy in children with attention-deficit/hyperactivity disorder. Pediatric neurology, 42(5), 325–330. https://doi.org/10.1016/j.pediatrneurol.2010.01.005
Doshi-Velez, F., Ge, Y., & Kohane, I. (2014). Comorbidity clusters in autism spectrum disorders: an electronic health record time-series analysis. Pediatrics, 133(1), e54–e63. https://doi.org/10.1542/peds.2013-0819
Dunn, L. M., Dunn, L. M., & Whetton, C. (1982). The British Picture Vocabulary Scale: Manual for the short and long forms. NFER-Nelson
Eriksson, M. A., Westerlund, J., Hedvall, Å., Åmark, P., Gillberg, C., & Fernell, E. (2013). Medical conditions affect the outcome of early intervention in preschool children with autism spectrum disorders. European child & adolescent psychiatry, 22(1), 23–33. https://doi.org/10.1007/s00787-012-0312-7
Fiest, K. M., Sauro, K. M., Wiebe, S., Patten, S. B., Kwon, C. S., Dykeman, J. … Jetté, N. (2017). Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology, 88(3), 296–303. https://doi.org/10.1212/WNL.0000000000003509
Fisher, R. S., Acevedo, C., Arzimanoglou, A., Bogacz, A., Cross, J. H., Elger, C. E. … Wiebe, S. (2014). ILAE official report: a practical clinical definition of epilepsy. Epilepsia, 55(4), 475–482. https://doi.org/10.1111/epi.12550
Fombonne, E., Heavey, L., Smeeth, L., Rodrigues, L. C., Cook, C., Smith, P. G. … Hall, A. J. (2004). Validation of the diagnosis of autism in general practitioner records. BMC public health, 4(1), 1–9. https://doi.org/10.1186/1471-2458-4-5
Fombonne, E., Snyder, L. G., Daniels, A., Feliciano, P., & Chung, W. (2020). Psychiatric and Medical Profiles of Autistic Adults in the SPARK Cohort. Journal of autism and developmental disorders, 50(10), 3679–3698. https://doi.org/10.1007/s10803-020-04414-6
Fortuna, R. J., Robinson, L., Smith, T. H., Meccarello, J., Bullen, B., Nobis, K., & Davidson, P. W. (2016). Health conditions and functional status in adults with autism: a cross-sectional evaluation. Journal of General Internal Medicine, 31(1), 77–84. https://doi.org/10.1007/s11606-015-3509-x
Gadow, K. D., Perlman, G., & Weber, R. J. (2017). Parent-reported developmental regression in autism: epilepsy, IQ, schizophrenia spectrum symptoms, and special education. Journal of Autism and Developmental Disorders, 47(4), 918–926. DOI https://doi.org/10.1007/s10803-016-3004-1
Gadow, K. D., & Sprafkin, J. (2005). Child and adolescent symptom inventory-4R. Stony Brook, NY: Checkmate Plus
Gilmore, D., Harris, L., Longo, A., & Hand, B. N. (2020). Health status of Medicare-enrolled autistic older adults with and without co-occurring intellectual disability: An analysis of inpatient and institutional outpatient medical claims. Autism, 25(1), 266–274. https://doi.org/10.1177%2F1362361320955109
Hara, H. (2007). Autism and epilepsy: a retrospective follow-up study. Brain and Development, 29(8), 486–490. https://doi.org/10.1016/j.braindev.2006.12.012
Hashimoto, T., Sasaki, M., Sugai, K., Hanaoka, S., Fukumizu, M., & Kato, T. (2001). Paroxysmal discharges on EEG in young autistic patients are frequent in frontal regions. Journal of Medical Investigation, 48(3/4), 175–180
Hirvikoski, T., Mittendorfer-Rutz, E., Boman, M., Larsson, H., Lichtenstein, P., & Bölte, S. (2016). Premature mortality in autism spectrum disorder. The British Journal of Psychiatry, 208(3), 232–238. https://doi.org/10.1192/bjp.bp.114.160192
Hwang, Y. I., Srasuebkul, P., Foley, K. R., Arnold, S., & Trollor, J. N. (2019). Mortality and cause of death of Australians on the autism spectrum. Autism research, 12(5), 806–815. https://doi.org/10.1002/aur.2086
Jain, A., Spencer, D., Yang, W., Kelly, J. P., Newschaffer, C. J., Johnson, J. … Dennen, T. (2014). Injuries among children with autism spectrum disorder. Academic pediatrics, 14(4), 390–397. https://doi.org/10.1016/j.acap.2014.03.012
Jokiranta, E., Sourander, A., Suominen, A., Timonen-Soivio, L., Brown, A. S., & Sillanpää, M. (2014). Epilepsy among children and adolescents with autism spectrum disorders: a population-based study. Journal of Autism and Developmental Disorders, 44(10), 2547–2557. https://doi.org/10.1007/s10803-014-2126-6
Kaye, J. A., del, Mar Melero-Montes, M., & Jick, H. (2001). Mumps, measles, and rubella vaccine and the incidence of autism recorded by general practitioners: a time trend analysis. Bmj, 322(7284), 460–463. https://doi.org/10.1136/bmj.322.7284.460
Ko, C., Kim, N., Kim, E., Song, D. H., & Cheon, K. A. (2016). The effect of epilepsy on autistic symptom severity assessed by the social responsiveness scale in children with autism spectrum disorder. Behavioral and Brain Functions, 12(1), 1–9. https://doi.org/10.1186/s12993-016-0105-0
Kohane, I. S., McMurry, A., Weber, G., MacFadden, D., Rappaport, L., Kunkel, L. … Churchill, S. (2012). The co-morbidity burden of children and young adults with autism spectrum disorders. PloS one, 7(4), e33224. https://doi.org/10.1371/journal.pone.0033224
Kommu, J. V. S., Gayathri, K. R., Srinath, S., Girimaji, S. C., Seshadri, S. P., & Gopalakrishna, G. (2017). Profile of two hundred children with Autism Spectrum Disorder from a tertiary child and adolescent psychiatry centre. Asian journal of psychiatry, 28, 51–56. https://doi.org/10.1016/j.ajp.2017.03.017
Kotulska, K., Kwiatkowski, D. J., Curatolo, P., Weschke, B., Riney, K., Jansen, F. … Wojdan, K. (2021). Prevention of epilepsy in infants with tuberous sclerosis complex in the EPISTOP trial. Annals of neurology, 89(2), 304–314. https://doi.org/10.1002/ana.25956
Krug, D. A., Arick, J. R., & Almond, P. J. (1978). ABC—Autism behaviour checklist. Portland, OR: ASIEP Education Co
Lamb, G. V., Green, R. J., & Olorunju, S. (2019). Tracking epilepsy and autism. The Egyptian Journal of Neurology Psychiatry and Neurosurgery, 55(1), 1–8. https://doi.org/10.1186/s41983-019-0103-x
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P. … Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of clinical epidemiology, 62(10), e1–e34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Lord, C., Rutter, M., Goode, S., Heemsbergen, J., Jordan, H., Mawhood, L., & Schopler, E. (1989). Austism diagnostic observation schedule: A standardized observation of communicative and social behavior. Journal of autism and developmental disorders, 19(2), 185–212. https://doi.org/10.1007/BF02211841
Lord, C., Rutter, M., & Le Couteur, A. (1994). Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of autism and developmental disorders, 24(5), 659–685. https://doi.org/10.1007/BF02172145
Lukmanji, S., Manji, S. A., Kadhim, S., Sauro, K. M., Wirrell, E. C., Kwon, C. S., & Jetté, N. (2019). The co-occurrence of epilepsy and autism: A systematic review. Epilepsy & Behavior, 98, 238–248. https://doi.org/10.1016/j.yebeh.2019.07.037
Lundström, S., Reichenberg, A., Anckarsäter, H., Lichtenstein, P., & Gillberg, C. (2015). Autism phenotype versus registered diagnosis in Swedish children: prevalence trends over 10 years in general population samples. bmj, 350. doi: https://doi.org/10.1136/bmj.h1961
Mandy, W., Chilvers, R., Chowdhury, U., Salter, G., Seigal, A., & Skuse, D. (2012). Sex differences in autism spectrum disorder: evidence from a large sample of children and adolescents. Journal of autism and developmental disorders, 42(7), 1304–1313. https://doi.org/10.1007/s10803-011-1356-0
McCue, L. M., Flick, L. H., Twyman, K. A., Xian, H., & Conturo, T. E. (2016). Prevalence of non-febrile seizures in children with idiopathic autism spectrum disorder and their unaffected siblings: a retrospective cohort study. BMC neurology, 16(1), 1–9. https://doi.org/10.1186/s12883-016-0764-3
Miles, J. H., Hadden, L. L., Takahashi, T. N., & Hillman, R. E. (2000). Head circumference is an independent clinical finding associated with autism. American journal of medical genetics, 95(4), 339–350. https://doi.org/10.1002/1096-8628(20001211)95:4%3C339::AID-AJMG9%3E3.0.CO;2-B
Ming, X., Brimacombe, M., Chaaban, J., Zimmerman-Bier, B., & Wagner, G. C. (2008). Autism spectrum disorders: concurrent clinical disorders. Journal of child neurology, 23(1), 6–13. https://doi.org/10.1177%2F0883073807307102
Miot, S., Akbaraly, T., Michelon, C., Couderc, S., Crepiat, S., Loubersac, J. … Baghdadli, A. (2019). Comorbidity burden in adults with autism spectrum disorders and intellectual disabilities—a report from the EFAAR (Frailty Assessment in Ageing Adults With Autism Spectrum and Intellectual Disabilities) study. Frontiers in psychiatry, 10, 617. https://doi.org/10.3389/fpsyt.2019.00617
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Prisma Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
Moon, J. P., Tan, H. T., Lam, K. F., Lim, J. M., Cheak, C. C., Wei, K. C. … Tan, G. M. Y. (2020). Adult neurodevelopmental services in Singapore: A sociodemographic and clinical profile at a tertiary psychiatric hospital. Asia-Pacific Psychiatry, 12(2), e12388. https://doi.org/10.1111/appy.12388
Mouridsen, S. E., Rich, B., & Isager, T. (2012). Fractures in individuals with and without a history of infantile autism. A Danish register study based on hospital discharge diagnoses. Journal of autism and developmental disorders, 42(4), 619–624. https://doi.org/10.1007/s10803-011-1286-x
Mouridsen, S. E., Rich, B., & Isager, T. (2013). Epilepsy in individuals with a history of Asperger’s syndrome: a Danish nationwide register-based cohort study. Journal of autism and developmental disorders, 43(6), 1308–1313. https://doi.org/10.1007/s10803-012-1675-9
Mouridsen, S. E., Rich, B., & Isager, T. (2016). Injury patterns among individuals diagnosed with infantile autism during childhood: A case-control study. Scandinavian Journal of Child and Adolescent Psychiatry and Psychology, 4(2), 88–95. https://doi.org/10.21307/sjcapp.2016.013
Mulligan, C. K., & Trauner, D. A. (2014). Incidence and behavioral correlates of epileptiform abnormalities in autism spectrum disorders. Journal of autism and developmental disorders, 44(2), 452–458. https://doi.org/10.1007/s10803-013-1888-6
National Center for Health Statistics. (2014). National Health Interview Survey (NHIS) public use data release: NHIS survey description. Hyattsville, MD: National Center of Health Statistics
O’Callaghan, F. J., Edwards, S. W., Alber, F. D., Borja, M. C., Hancock, E., Johnson, A. L. … Natarajan, J. (2018). Vigabatrin with hormonal treatment versus hormonal treatment alone (ICISS) for infantile spasms: 18-month outcomes of an open-label, randomised controlled trial. The Lancet Child & Adolescent Health, 2(10), 715–725. https://doi.org/10.1016/S2352-4642(18)30244-X
Oslejskova, H., Dusek, L., Makovska, Z., & Rektor, I. (2007). Epilepsia, epileptiform abnormalities, non-right-handedness, hypotonia and severe decreased IQ are associated with language impairment in autism. Epileptic Disorders, 9(5), 9–18
Pan, P. Y., Bölte, S., Kaur, P., Jamil, S., & Jonsson, U. (2020). Neurological disorders in autism: A systematic review and meta-analysis. Autism, 1362361320951370. https://doi.org/10.1177%2F1362361320951370
Parmeggiani, A., Barcia, G., Posar, A., Raimondi, E., Santucci, M., & Scaduto, M. C. (2010). Epilepsy and EEG paroxysmal abnormalities in autism spectrum disorders. Brain and Development, 32(9), 783–789. https://doi.org/10.1016/j.braindev.2010.07.003
Pavone, P., Incorpora, G., Fiumara, A., Parano, E., Trifiletti, R. R., & Ruggieri, M. (2004). Epilepsy is not a prominent feature of primary autism. Neuropediatrics, 35(04), 207–210
Peacock, G., Amendah, D., Ouyang, L., & Grosse, S. D. (2012). Autism spectrum disorders and health care expenditures: the effects of co-occurring conditions. Journal of Developmental & Behavioral Pediatrics, 33(1), 2–8. https://doi.org/10.1097/DBP.0b013e31823969de
Raven, J. C., & Court, J. H. (1986). Raven’s progressive matrices and Raven’s coloured matrices. London: HK Lewis
Russell, G., Stapley, S., Newlove-Delgado, T., Salmon, A., White, R., Warren, F. … Ford, T. (2021). Time trends in autism diagnosis over 20 years: a UK population‐based cohort study. Journal of Child Psychology and Psychiatry. https://doi.org/10.1111/jcpp.13505
Saltık, S., & Başgül, Ş. S. (2012). Neurological disorders combined with autism in children. HELİCOBACTER, 18, 23
Rutter, M., Le Couteur, A., & Lord, C. (2003). ADI-R. Autism diagnostic interview revised. Manual. Los Angeles: Western Psychological Services
Saltik, S., & Basgul, S. S. (2014). When do we recommend an EEG and cranial MRI evaluation for autistic children? Dusunen Adam The Journal of Psychiatry and Neurological Sciences, 27(2), 147
Schopler, E., Reichler, R. J., DeVellis, R. F., et al. (1980). Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). Journal Of Autism And Developmental Disorders, 10, 91–103. https://doi.org/10.1007/BF02408436
Schopler, E., Van Bourgondien, M. E., Wellman, G. J., & Love, S. R. (2010). Childhood Autism Rating Scale–Second Edition (CARS-2). Los Angeles, CA: Western Psychological Services
Schuch, J. B., Muller, D., Endres, R. G., Bosa, C. A., Longo, D., Schuler-Faccini, L. … Roman, T. (2014). The role of β3 integrin gene variants in autism spectrum disorders—diagnosis and symptomatology. Gene, 553(1), 24–30. https://doi.org/10.1016/j.gene.2014.09.058
Schuck, R. K., Flores, R. E., & Fung, L. K. (2019). Brief report: Sex/gender differences in symptomology and camouflaging in adults with autism spectrum disorder. Journal of autism and developmental disorders, 49(6), 2597–2604. https://doi.org/10.1007/s10803-019-03998-y
Shubrata, K. S., Sinha, S., Seshadri, S. P., Girimaji, S., Subbakrishna, D. K., & Srinath, S. (2015). Childhood autism spectrum disorders with and without epilepsy: clinical implications. Journal of child neurology, 30(4), 476–482. https://doi.org/10.1177%2F0883073814540521
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child & Adolescent Psychiatry, 47(8), 921–929. https://doi.org/10.1097/CHI.0b013e318179964f
Smith, K. R., & Matson, J. L. (2010a). Social skills: Differences among adults with intellectual disabilities, co-morbid autism spectrum disorders and epilepsy. Research in developmental disabilities, 31(6), 1366–1372. https://doi.org/10.1016/j.ridd.2010.07.002
Smith, K. R., & Matson, J. L. (2010b). Behavior problems: Differences among intellectually disabled adults with co-morbid autism spectrum disorders and epilepsy. Research in Developmental Disabilities, 31(5), 1062–1069. https://doi.org/10.1016/j.ridd.2010.04.003
Smith, K. R., & Matson, J. L. (2010c). Social skills: Differences among adults with intellectual disabilities, co-morbid autism spectrum disorders and epilepsy. Research in developmental disabilities, 31(6), 1366–1372. https://doi.org/10.1016/j.ridd.2010.07.002
Socanski, D., Aurlien, D., Herigstad, A., Thomsen, P. H., & Larsen, T. K. (2013). Epilepsy in a large cohort of children diagnosed with attention deficit/hyperactivity disorders (ADHD). Seizure, 22(8), 651–655. https://doi.org/10.1016/j.seizure.2013.04.021
Strasser, L., Downes, M., Kung, J., Cross, J. H., & De Haan, M. (2018). Prevalence and risk factors for autism spectrum disorder in epilepsy: a systematic review and meta-analysis. Developmental Medicine & Child Neurology, 60(1), 19–29. https://doi.org/10.1111/dmcn.13598
Su, C. C., Chi, M. H., Lin, S. H., & Yang, Y. K. (2016). Bidirectional association between autism spectrum disorder and epilepsy in child and adolescent patients: a population-based cohort study. European child & adolescent psychiatry, 25(9), 979–987. https://doi.org/10.1007/s00787-016-0817-6
Thompson, L., Gillberg, C., Landberg, S., Kantzer, A. K., Miniscalco, C., Olsson, M. B. … Fernell, E. (2019). Autism with and without regression: A two-year prospective longitudinal study in two population-derived Swedish cohorts. Journal of autism and developmental disorders, 49(6), 2281–2290. https://doi.org/10.1007/s10803-018-03871-4
Tuchman, R. (2017, November). What is the relationship between autism spectrum disorders and epilepsy?. In Seminars in pediatric neurology (Vol. 24, No. 4, pp. 292–300). WB Saunders. https://doi.org/10.1016/j.spen.2017.10.004
Tye, C., Runicles, A. K., Whitehouse, A. J., & Alvares, G. A. (2019). Characterizing the interplay between autism spectrum disorder and comorbid medical conditions: an integrative review. Frontiers in psychiatry, 9, 751. https://doi.org/10.3389/fpsyt.2018.00751
Valvo, G., Baldini, S., Brachini, F., Apicella, F., Cosenza, A., Ferrari, A. R. … Sicca, F. (2013). Somatic overgrowth predisposes to seizures in autism spectrum disorders. PLoS One, 8(9), e75015. https://doi.org/10.1371/journal.pone.0075015
Ververi, A., Vargiami, E., Papadopoulou, V., Tryfonas, D., & Zafeiriou, D. I. (2012). Clinical and laboratory data in a sample of Greek children with autism spectrum disorders. Journal of autism and developmental disorders, 42(7), 1470–1476. https://doi.org/10.1007/s10803-011-1414-7
Waddington, H., McLay, L., Woods, L., & Whitehouse, A. J. (2020). Child and family characteristics associated with sleep disturbance in children with autism spectrum disorder. Journal of autism and developmental disorders, 50(11), 4121–4132. https://doi.org/10.1007/s10803-020-04475-7
Weber, R. J., & Gadow, K. D. (2017). Relation of psychiatric symptoms with epilepsy, asthma, and allergy in youth with ASD vs. psychiatry referrals. Journal of abnormal child psychology, 45(6), 1247–1257. https://doi.org/10.1007/s10802-016-0212-2
Wing, L., Leekam, S. R., Libby, S. J., Gould, J., & Larcombe, M. (2002). The diagnostic interview for social and communication disorders: Background, inter-rater reliability and clinical use. Journal of child psychology and psychiatry, 43(3), 307–325. https://doi.org/10.1111/1469-7610.00023
Wise, E. A., Smith, M. D., & Rabins, P. V. (2017). Aging and autism spectrum disorder: a naturalistic, longitudinal study of the comorbidities and behavioral and neuropsychiatric symptoms in adults with ASD. Journal of autism and developmental disorders, 47(6), 1708–1715. https://doi.org/10.1007/s10803-017-3095-3
World Health Organization. (1971). International classification of diseases (8th ed.). Copenhagen: Sundhedsstyrelsen (National Board of Health)
World Health Organization. (1978). International classification of diseases: Mental disorders: Glossary and guide to their classification (9th ed.). Geneva: World Health Organization
World Health Organization. (1992). The ICD-10 classification of mental and behavioural disorders. Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization
Wong, V. C., Fung, C. K., & Wong, P. T. (2014). Use of dysmorphology for subgroup classification on autism spectrum disorder in Chinese children. Journal of autism and developmental disorders, 44(1), 9–18. https://doi.org/10.1007/s10803-013-1846-3
Wu, Y. T., Maenner, M. J., Wiggins, L. D., Rice, C. E., Bradley, C. C., Lopez, M. L. … Lee, L. C. (2016). Retention of autism spectrum disorder diagnosis: The role of co-occurring conditions in males and females. Research in autism spectrum disorders, 25, 76–86. https://doi.org/10.1016/j.rasd.2016.02.001
Zhang, W., Baranek, G., & Boyd, B. (2018). Brief Report: Factors Associated with Emergency Department Visits for Epilepsy Among Children with Autism Spectrum Disorder. Journal of autism and developmental disorders, 48(5), 1854–1860. https://doi.org/10.1007/s10803-017-3433-5
Zhang, A., Li, J., Zhang, Y., Jin, X., & Ma, J. (2019). Epilepsy and Autism Spectrum Disorder: An Epidemiological Study in Shanghai, China. Frontiers in psychiatry, 10, 658. https://doi.org/10.3389/fpsyt.2019.00658
Acknowledgements and Funding
This systematic review was funded by Autistica, Young Epilepsy and Epilepsy Research UK. We are grateful for the support of Heather Chesters, Deputy Librarian UCL Great Ormond Street Institute of Child Health for her help with the systematic search.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zarakoviti, E., Shafran, R., Skuse, D. et al. Factor associated with the occurrence of epilepsy in autism: a systematic review. J Autism Dev Disord 53, 3873–3890 (2023). https://doi.org/10.1007/s10803-022-05672-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-022-05672-2