Abstract
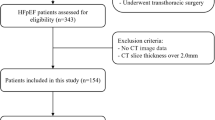
To explore the association of ventricle epicardial fat volume (EFV) calculated by cardiac magnetic resonance (CMR) and the insulin resistance indicator of triglyceride–glucose (TyG) index in patients with chronic HF (CHF), this retrospective cohort study included adult CHF patients with confirmed diagnosis of heart failure from January 2018 to December 2020. All patients underwent 3.0T CMR, and EFV were measured under short-axis cine. Spearman correlation, multivariate linear regression, and restricted cubic spline (RCS) regression were used to analyze their association. There were 516 patients with CHF, of whom 69.8% were male. Median EFV was 57.14mL and mean TyG index was 8.48. Spearman correlation analysis showed that TyG index was significantly correlated with the EFV in CHF patients (r = 0.247, P < 0.001). Further analysis showed that TyG index levels were significantly associated with EFV as both continuous variables (Unstandardized β = 6.556, P < 0.001) and across the increasing quartiles (β = 7.50, 95% CI [1.41, 13.59], P < 0.05). RCS demonstrated there were a positive trend and linear association between EFV and TyG index in CHF patients (P for nonliearity = 0.941). In patients with CHF, the TyG index was positively and linearly associated with the EFV, which supports the metabolic roles of epicardial adipose tissue regarding insulin resistance.


Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article. The data that support the findings of this study are available from the corresponding author, X.L., upon reasonable request.
References
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM et al (2022) 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation 145(18):e895–e1032. https://doi.org/10.1161/CIR.0000000000001063
Seferovic PM, Ponikowski P, Anker SD, Bauersachs J, Chioncel O, Cleland JGF et al (2019) Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 21(10):1169–1186. https://doi.org/10.1002/ejhf.1531
Roger VL (2021) Epidemiology of heart failure: a contemporary perspective. Circ Res 128(10):1421–1434. https://doi.org/10.1161/CIRCRESAHA.121.318172
Hao G, Wang X, Chen Z, Zhang L, Zhang Y, Wei B et al (2019) China hypertension survey investigators. prevalence of heart failure and left ventricular dysfunction in China: the China hypertension survey, 2012–2015. Eur J Heart Fail 21(11):1329–1337. https://doi.org/10.1002/ejhf.1629
Greene SJ, Hernandez AF, Dunning A, Ambrosy AP, Armstrong PW, Butler J et al (2017) Hospitalization for recently diagnosed versus worsening chronic heart failure: from the ASCEND-HF Trial. J Am Coll Cardiol 69(25):3029–3039. https://doi.org/10.1016/j.jacc.2017.04.043
Psotka MA, Fonarow GC, Allen LA, Joynt Maddox KE, Fiuzat M, Heidenreich P et al (2020) The hospital readmissions reduction program: nationwide perspectives and recommendations: a JACC: heart failure position paper. JACC Heart Fail 8(1):1–11. https://doi.org/10.1016/j.jchf.2019.07.012
Wu C, Zhang Z, Zhang W, Liu X (2022) Mitochondrial dysfunction and mitochondrial therapies in heart failure. Pharmacol Res 175:106038. https://doi.org/10.1016/j.phrs.2021.106038
Smith U, Kahn BB (2016) Adipose tissue regulates insulin sensitivity: role of adipogenesis, de novo lipogenesis and novel lipids. J Intern Med 280(5):465–475. https://doi.org/10.1111/joim.12540
Hammarstedt A, Gogg S, Hedjazifar S, Nerstedt A, Smith U (2018) Impaired adipogenesis and dysfunctional adipose tissue in human hypertrophic obesity. Physiol Rev 98(4):1911–1941. https://doi.org/10.1152/physrev.00034.2017
Ding X, Wang X, Wu J, Zhang M, Cui M (2021) Triglyceride-glucose index and the incidence of atherosclerotic cardiovascular diseases: a meta-analysis of cohort studies. Cardiovasc Diabetol 20(1):76. https://doi.org/10.1186/s12933-021-01268-9
Kahleova H, Matoulek M, Malinska H, Oliyarnik O, Kazdova L, Neskudla T et al (2011) Vegetarian diet improves insulin resistance and oxidative stress markers more than conventional diet in subjects with type 2 diabetes. Diabet Med 28(5):549–559. https://doi.org/10.1111/j.1464-5491.2010.03209.x
Sanz CM, Ruidavets JB, Bongard V, Marquié JC, Hanaire H, Ferrières J et al (2013) Relationship between markers of insulin resistance, markers of adiposity, HbA1c, and cognitive functions in a middle-aged population-based sample: the MONA LISA study. Diabetes Care 36(6):1512–1521. https://doi.org/10.2337/dc12-1017
Wang L, Cong HL, Zhang JX, Hu YC, Wei A, Zhang YY et al (2020) Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc Diabetol 19(1):80. https://doi.org/10.1186/s12933-020-01054-z
Guo W, Zhao L, Mo F, Peng C, Li L, Xu Y et al (2021) The prognostic value of the triglyceride glucose index in patients with chronic heart failure and type 2 diabetes: a retrospective cohort study. Diabetes Res Clin Pract 177:108786. https://doi.org/10.1016/j.diabres.2021.108786
Tao LC, Xu JN, Wang TT, Hua F, Li JJ (2022) Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol 21(1):68. https://doi.org/10.1186/s12933-022-01511-x
Nagy E, Jermendy AL, Merkely B, Maurovich-Horvat P (2017) Clinical importance of epicardial adipose tissue. Arch Med Sci 13(4):864–874. https://doi.org/10.5114/aoms.2016.63259
Blumensatt M, Fahlbusch P, Hilgers R, Bekaert M, Herzfeld de Wiza D, Akhyari P et al (2017) Secretory products from epicardial adipose tissue from patients with type 2 diabetes impair mitochondrial β-oxidation in cardiomyocytes via activation of the cardiac renin-angiotensin system and induction of miR-208a. Basic Res Cardiol 112(1):2. https://doi.org/10.1007/s00395-016-0591-0
Nalliah CJ, Bell JR, Raaijmakers AJA, Waddell HM, Wells SP, Bernasochi GB et al (2020) Epicardial adipose tissue accumulation confers atrial conduction abnormality. J Am Coll Cardiol 76(10):1197–1211. https://doi.org/10.1016/j.jacc.2020.07.017
Christensen RH, Hansen CS, von Scholten BJ, Jensen MT, Pedersen BK, Schnohr P et al (2019) Epicardial and pericardial adipose tissues are associated with reduced diastolic and systolic function in type 2 diabetes. Diabetes Obes Metab 21(8):2006–2011. https://doi.org/10.1111/dom.13758
Iacobellis G (2022) Epicardial adipose tissue in contemporary cardiology. Nat Rev Cardiol 19(9):593–606. https://doi.org/10.1038/s41569-022-00679-9
Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P et al (2017) Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson 19(1):75. https://doi.org/10.1186/s12968-017-0389-8
van Woerden G, van Veldhuisen DJ, Gorter TM, van Empel VPM, Hemels MEW, Hazebroek EJ et al (2021) Importance of epicardial adipose tissue localization using cardiac magnetic resonance imaging in patients with heart failure with mid-range and preserved ejection fraction. Clin Cardiol 44(7):987–993. https://doi.org/10.1002/clc.23644
Zhou Y, Yu M, Cui J, Hu F, Yang Z, Yuan J et al (2021) The predictive value of epicardial adipose tissue volume assessed by cardiac magnetic resonance for atrial fibrillation in patients with hypertrophic obstructive cardiomyopathy. Int J Cardiovasc Imaging 37(4):1383–1393. https://doi.org/10.1007/s10554-020-02092-0
Xu L, Wu M, Chen S, Yang Y, Wang Y, Wu S et al (2022) Triglyceride-glucose index associates with incident heart failure: a cohort study. Diabetes Metab 101365. https://doi.org/10.1016/j.diabet.2022.101365
Villasante Fricke AC, Iacobellis G (2019) Epicardial adipose tissue: clinical biomarker of Cardio-metabolic risk. Int J Mol Sci 20(23):5989. https://doi.org/10.3390/ijms20235989
Nerlekar N, Muthalaly RG, Wong N, Thakur U, Wong DTL, Brown AJ, Marwick TH (2018) Association of volumetric epicardial adipose tissue quantification and cardiac structure and function. J Am Heart Assoc 7(23):e009975. https://doi.org/10.1161/JAHA.118.009975
Cheang I, Zhu X, Yue X, Tang Y, Gao Y, Lu X et al (2023) Prognostic value of ventricle epicardial fat volume by cardiovascular magnetic resonance in chronic heart failure. iScience 26(5):106755. https://doi.org/10.1016/j.isci.2023.106755
Mone P, De Gennaro S, Frullone S, Marro A, Santulli G (2023) Hyperglycemia drives the transition from pre-frailty to frailty: the monteforte study. Eur J Intern Med 111:135–137. https://doi.org/10.1016/j.ejim.2023.01.006Epub 2023 Jan 10. PMID: 36635128; PMCID: PMC10122706
Pansini A, Lombardi A, Morgante M, Frullone S, Marro A, Rizzo M et al (2022) Hyperglycemia and physical impairment in frail hypertensive older adults. Front Endocrinol (Lausanne) 13:831556. https://doi.org/10.3389/fendo.2022.831556PMID: 35498439; PMCID: PMC9048203
Mone P, Lombardi A, Salemme L, Cioppa A, Popusoi G, Varzideh F et al (2023) Stress hyperglycemia drives the risk of hospitalization for chest pain in patients with ischemia and nonobstructive coronary arteries (INOCA). Diabetes Care 46(2):450–454. https://doi.org/10.2337/dc22-0783PMID: 36478189; PMCID: PMC9887616
Chouchani ET, Kajimura S (2019) Metabolic adaptation and maladaptation in adipose tissue. Nat Metab 1(2):189–200. https://doi.org/10.1038/s42255-018-0021-8Epub 2019 Jan 21. PMID: 31903450; PMCID: PMC6941795
Hasebe H, Yoshida K, Nogami A, Ieda M (2020) Difference in epicardial adipose tissue distribution between paroxysmal atrial fibrillation and coronary artery disease. Heart Vessels 35(8):1070–1078. https://doi.org/10.1007/s00380-020-01575-3
González N, Moreno-Villegas Z, González-Bris A, Egido J, Lorenzo Ó (2017) Regulation of visceral and epicardial adipose tissue for preventing cardiovascular injuries associated to obesity and diabetes. Cardiovasc Diabetol 16(1):44. https://doi.org/10.1186/s12933-017-0528-4
Parisi V, Cabaro S, D’Esposito V, Petraglia L, Conte M, Campana P et al (2020) Epicardial adipose tissue and IL-13 response to myocardial injury drives left ventricular remodeling after ST elevation myocardial infarction. Front Physiol 11:575181. https://doi.org/10.3389/fphys.2020.575181
Smith U, Kahn BB (2016) Adipose tissue regulates insulin sensitivity: role of adipogenesis, de novo lipogenesis and novel lipids. J Intern Med 280(5):465–475. https://doi.org/10.1111/joim.12540Epub 2016 Oct 3
Iacobellis G, Sharma AM (2007) Epicardial adipose tissue as new cardio-metabolic risk marker and potential therapeutic target in the metabolic syndrome. Curr Pharm Des 13(21):2180–2184. https://doi.org/10.2174/138161207781039670
Li B, Po SS, Zhang B, Bai F, Li J, Qin F et al (2020) Metformin regulates adiponectin signalling in epicardial adipose tissue and reduces atrial fibrillation vulnerability. J Cell Mol Med 24(14):7751–7766. https://doi.org/10.1111/jcmm.15407
Dozio E, Vianello E, Malavazos AE, Tacchini L, Schmitz G, Iacobellis G et al (2019) Epicardial adipose tissue GLP-1 receptor is associated with genes involved in fatty acid oxidation and white-to-brown fat differentiation: a target to modulate cardiovascular risk? Int J Cardiol 292:218–224. https://doi.org/10.1016/j.ijcard.2019.04.039
Masson W, Lavalle-Cobo A, Nogueira JP (2021) Effect of SGLT2-inhibitors on epicardial adipose tissue: a meta-analysis. Cells 10(8):2150. https://doi.org/10.3390/cells10082150. PMID
Requena-Ibáñez JA, Santos-Gallego CG, Rodriguez-Cordero A, Vargas-Delgado AP, Mancini D, Sartori S et al (2021) Mechanistic insights of empagliflozin in nondiabetic patients with HFrEF: from the EMPA-TROPISM study. JACC Heart Fail 9(8):578–589. https://doi.org/10.1016/j.jchf.2021.04.014
Payne GA, Kohr MC, Tune JD (2012) Epicardial perivascular adipose tissue as a therapeutic target in obesity-related coronary artery disease. Br J Pharmacol 165(3):659–669. https://doi.org/10.1111/j.1476-5381.2011.01370.x
Packer M (2021) Differential pathophysiological mechanisms in heart failure with a reduced or preserved ejection fraction in diabetes. JACC Heart Fail 9(8):535–549. https://doi.org/10.1016/j.jchf.2021.05.019
Xourgia E, Papazafiropoulou A, Melidonis A (2018) Effects of antidiabetic drugs on epicardial fat. World J Diabetes 9(9):141–148. https://doi.org/10.4239/wjd.v9.i9.141
Rossi VA, Gruebler M, Monzo L, Galluzzo A, Beltrami M (2023) The different pathways of epicardial adipose tissue across the heart failure phenotypes: from pathophysiology to therapeutic target. Int J Mol Sci 24(7):6838. https://doi.org/10.3390/ijms24076838
Funding
This work was supported by Key Program of National Natural Science Foundation of China (81730106 to XL Li), General Program of National Natural Science Foundation of China (82370389, 81970339 to XL Li, 82270394 to HF Zhang), The National High Technology Research and Development Program of China (2017YFC1700505 to XL Li), and project from Gusu School (GSRCKY20210204 to HF Zhang). Dr. XL Li and HF Zhang are Associate Fellows at the Collaborative Innovation Center for Cardiovascular Disease Translational Medicine.
Author information
Authors and Affiliations
Contributions
Conceptualization, Iokfai Cheang and Xinli Li; Data curation, Xin Yue, Yuan Tang and Yujie Gao; Formal analysis, Iokfai Cheang; Funding acquisition, Xinli Li; Investigation, Iokfai Cheang, Xu Zhu, Xinyi Lu and Shi Shi; Methodology, Xu Zhu; Project administration, Yinsu Zhu, Yi Xu and Xinli Li; Resources, Yinsu Zhu and Yi Xu; Software, Xu Zhu and Xinyi Lu; Supervision, Shengen Liao and Wenming Yao; Validation, Shi Shi, Yanli Zhou and Haifeng Zhang; Visualization, Xin Yue, Yuan Tang and Yujie Gao; Writing – original draft, Iokfai Cheang; Writing – review & editing, Iokfai Cheang, Xu Zhu and Xinli Li. All authors have reviewed and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Statement of ethics
This study protocol was reviewed and approved by the independent institutional ethical committee of the First Affiliated Hospital of Nanjing Medical University (Approval No. 2022-SR-052), and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from patients to participate in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.



Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cheang, I., Zhu, X., Lu, X. et al. Correlation of ventricle epicardial fat volume and triglyceride-glucose index in patients with chronic heart failure. Int J Cardiovasc Imaging 40, 789–799 (2024). https://doi.org/10.1007/s10554-024-03048-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-024-03048-4