Abstract
Purpose
In stage IV breast cancer, the efficacy of human epidermal growth factor receptor 2 (HER2) targeted therapies in cases with discordance in HER2 expression between primary and metastatic site is not well known. We studied progression free (PFS) and overall survival (OS) by HER2 concordance when treating women with taxane–trastuzumab (± pertuzumab) in first or second line and trastuzumab-emtansine (T-DM1) or capecitabine–lapatinib in later lines.
Patients and methods
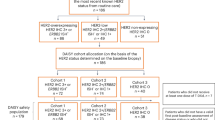
Retrospective monocentric study including all breast cancer patients receiving trastuzumab between January 2002 and September 2017 at the University Hospital in Leuven; we selected metastatic patients with an available HER2 status in primary and metastatic site. The Kaplan–Meier method was used for estimating PFS/OS and log-rank test for analyzing between group differences. A Cox model is used for testing difference between groups while correcting for Pertuzumab. Multivariable Cox regression is used to model overall survival as a function group, correcting for possible confounders.
Results
We included 74 patients; 46 had an unchanged HER2 status (positive/positive), 9 lost HER2 (positive/negative), while 19 acquired HER2 amplification (negative/positive). 25 out of 28 cases with a discordant HER2 status were positive for ER and/or PgR in the primary site. HER2 positive/negative cases had a significantly lower PFS for taxane–trastuzumab–(pertuzumab) (PFS = 5.5 months), compared to HER2 positive/positive (PFS 9 months, p = 0.01) and HER2 negative/positive (PFS 14 months, p = 0.01) patients. PFS for later line T-DM1 (n = 30) was significantly higher for the HER2 positive/positive group (PFS 6.0 months) than for the discordant groups HER2 negative/positive (PFS 1.0 month, p = 0.04) and HER2 positive/negative (PFS 1.5 month, p = 0.01). After correcting for possible confounders, the HER2 positive/negative group had a significantly worse OS compared to HER2 positive/positive (HR 0.19, 95% CI 0.08–0.44) and negative/positive (HR 0.15, 95% 0.06–0.38).
Conclusion
Conversion of HER2 status was seen in 28 out of 74 cases and was mostly observed in hormone receptor-positive tumors. In contrast to patients with HER2 loss, patients with a positive conversion of HER2 status derived substantial benefit from first line treatment with taxane–trastuzumab–(pertuzumab). This study highlights the importance of re-biopsying the metastatic lesion and changing treatment according to the last HER2 result.



Similar content being viewed by others
Abbreviations
- BC:
-
Breast cancer
- PgR:
-
Progesterone receptor
- CEP17:
-
Centromere enumerator probe 17
- TTM:
-
Time to metastasis
- NPI:
-
Nottingham Prognostic Index
- ASCO/CAP:
-
American Society of Clinical Oncology/College of American Pathologist
- ER:
-
Estrogen receptor
- OS:
-
Overall survival
- PFS:
-
Progression free survival
- HER2:
-
Human epidermal growth factor receptor 2
- CI:
-
Confidence intervals
References
Slamon DJ, Godolphin W, Jones LA, Holt JA, Wong SG, Keith DE, Levin WJ, Stuart SG, Udove J, Ullrich A et al (1989) Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 244:707–712
Ross JS, Slodkowska EA, Symmans WF, Pusztai L, Ravdin PM, Hortobagyi GN (2009) The HER-2 receptor and breast cancer: ten years of targeted anti-HER-2 therapy and personalized medicine. Oncologist 14(4):320–368
Yao Z, Lu L, Wang R, Jin L, Liu S, Li H et al (2013) Discordance and clinical significance of ER, PR, and HER2 status between primary breast cancer and synchronous axillary lymph node metastasis. Med Oncol 31(1):798
Gajria D, Chandarlapaty S (2011) HER2-amplified breast cancer: mechanisms of trastuzumab resistance and novel targeted therapies. Expert Rev Anticancer Ther 11(2):263–275
Amir E, Miller N, Geddie W, Freedman O, Kassam F, Simmons C et al (2012) Prospective study evaluating the impact of tissue confirmation of metastatic disease in patients with breast cancer. J Clin Oncol 30(6):587–592
Thompson AM, Jordan LB, Quinlan P, Anderson E, Skene A, Dewar JA, Purdie CA, The Breast Recurrence in Tissues Study Group (2010) Prospective comparison of switches in biomarker status between primary and recurrent breast cancer: the Breast Recurrence In Tissues Study (BRITS). Breast Cancer Res 12(6):R92
Pareja F, Murray MP, Jean RD, Konno F, Friedlander M, Lin O, Edelweiss M (2017) Cytologic assessment of estrogen receptor, progesterone receptor, and HER2 status in metastatic breast carcinoma. J Am Soc Cytopathol 6(1):33–40
Aurilio G, Disalvatore D, Pruneri G, Bagnardi V, Viale G, Curigliano G et al (2014) A meta-analysis of oestrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 discordance between primary breast cancer and metastases. Eur J Cancer 50(2):277–289
Schrijver WAME, Suijkerbuijk KPM, van Gils CH, van der Wall E, Moelans CB, van Diest PJ (2018) Receptor conversion in distant breast cancer metastases: a systematic review and meta-analysis. J Natl Cancer Inst 110(6):568–580
Van Poznak C, Somerfield MR, Bast RC, Cristofanilli M, Goetz MP, Gonzalez-Angulo AM et al (2015) Use of biomarkers to guide decisions on systemic therapy for women with metastatic breast cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 33(24):2695–2704
Amir E, Clemons M, Purdie CA, Miller N, Quinlan P, Geddie W et al (2012) Tissue confirmation of disease recurrence in breast cancer patients: pooled analysis of multi-centre, multi-disciplinary prospective studies. Cancer Treat Rev 38(6):708–714
Wilking U, Karlsson E, Skoog L, Hatschek T, Lidbrink E, Elmberger G et al (2011) HER2 status in a population-derived breast cancer cohort: discordances during tumor progression. Breast Cancer Res Treat 125(2):553–561
Liedtke C, Broglio K, Moulder S, Hsu L, Kau S-W, Symmans WF et al (2009) Prognostic impact of discordance between triple-receptor measurements in primary and recurrent breast cancer. Ann Oncol 20(12):1953–1958
Lower EE, Khan S, Kennedy D, Baughman RP (2017) Discordance of the estrogen receptor and HER-2/neu in breast cancer from primary lesion to first and second metastatic site. Breast Cancer (London) 9:515–520
Kulka J, Székely B, Lukács LV, Kiss O, Tőkés A-M, Vincze E et al (2016) Comparison of predictive immunohistochemical marker expression of primary breast cancer and paired distant metastasis using surgical material: a practice-based study. J Histochem Cytochem 64(4):256–267
Li MH, Hou CL, Wang C, Sun AJ (2016) HER-2, ER, PR status concordance in primary breast cancer and corresponding metastatic lesion in lymph node in Chinese women. Pathol Res Pract 212(4):252–257
Lindström LS, Karlsson E, Wilking UM, Johansson U, Hartman J, Lidbrink EK et al (2012) Clinically used breast cancer markers such as estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 are unstable throughout tumor progression. J Clin Oncol 30(21):2601–2608
Yang Y-F, Liao Y-Y, Yang M, Peng N-F, Xie S-R, Xie Y-F (2014) Discordances in ER, PR and HER2 receptors between primary and recurrent/metastatic lesions and their impact on survival in breast cancer patients. Med Oncol 31(10):214
van de Ven S, Smit VTHBM, Dekker TJA, Nortier JWR, Kroep JR (2011) Discordances in ER, PR and HER2 receptors after neoadjuvant chemotherapy in breast cancer. Cancer Treat Rev 37(6):422–30
Dowsett M, Dunbier AK (2008) Emerging biomarkers and new understanding of traditional markers in personalized therapy for breast cancer. Clin Cancer Res. 14(24):8019–8026
Perou CM, Sørlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA et al (2000) Molecular portraits of human breast tumours. Nature 406:747
Wang R-X, Chen S, Jin X, Chen C-M, Shao Z-M (2017) Weekly paclitaxel plus carboplatin with or without trastuzumab as neoadjuvant chemotherapy for HER2-positive breast cancer: loss of HER2 amplification and its impact on response and prognosis. Breast Cancer Res Treat 161(2):259–267
Cardoso F, Fallowfield L, Costa A, Castiglione M, Senkus E, ESMO Guidelines Working Group On behalf of the EGW (2011) Locally recurrent or metastatic breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 22(suppl 6):vi25–vi30
Van Poznak C, Somerfield MR, Bast RC et al (2015) Use of biomarkers to guide decisions on systemic therapy for women with metastatic breast cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 33(24):2695–2704
McGranahan N, Swanton C et al (2015) Biological and therapeutic impact of intratumor heterogeneity in cancer evolution. Cancer Cell 27(1):15–26. https://doi.org/10.1016/j.ccell.2014.12.001
Gebhart G, Lamberts LE, Wimana Z et al (2016) Molecular imaging as a tool to investigate heterogeneity of advanced HER2-positive breast cancer and to predict patient outcome under trastuzumab emtansine (T-DM1): the ZEPHIR trial. Ann Oncol 27(4):619–624
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of retrospective study, formal consent is not required. The ethics committee of the University Hospitals Leuven approved the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Table 3.
Rights and permissions
About this article
Cite this article
Van Raemdonck, E., Floris, G., Berteloot, P. et al. Efficacy of anti-HER2 therapy in metastatic breast cancer by discordance of HER2 expression between primary and metastatic breast cancer. Breast Cancer Res Treat 185, 183–194 (2021). https://doi.org/10.1007/s10549-020-05935-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05935-5