Abstract
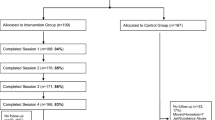
PrEP use remains suboptimal among Black sexual minority men (SMM) partly due to low perceived risk for HIV (PRH). This study describes baseline results of POSSIBLE, a multicomponent pilot intervention including a peer change agent (PCA) to increase PRH among Black SMM. POSSIBLE was a theoretically guided two-session, single-group feasibility intervention in Baltimore, MD conducted between 2019 and 2021 (N = 69). Baseline study visits involved a 20-minute session with a PrEP-using PCA who used a motivational interview-based script to discuss participants’ lifestyles, goals, and values, HIV risk behaviors, and PRH and tailor communication to encourage PrEP use. Bivariate analyses were conducted to assess differences in PRH before and after baseline sessions along with the correlates of PrEP referral willingness. A total of 75% of participants identified as gay; 73% were employed; 84% reported having insurance; 78% were single; 51% reported ever being diagnosed with an STI. Baseline results showed a statistically significant improvement in PRH after the first session (t=-3.09; p < .01). Additionally, 64% were willing to be referred to PrEP care after baseline; 45% of whom made a PrEP appointment. PRH was not associated with referral willingness. However, receptive anal intercourse in the previous 6 months was statistically significantly associated with referral willingness. Findings suggests that a scripted PCA could independently improve PRH among Black SMM quickly. The person-centered nature of the scripted PCA could be key to improving PrEP use among a highly marginalized and elusive community.

Similar content being viewed by others
References
Centers for Disease Control and Prevention. Brief | African American | Gay and Bisexual Men | HIV by Group | HIV/AIDS | CDC [Internet]. 2020 [cited 2020 Feb 24]. Available from: https://www.cdc.gov/hiv/group/msm/brief.html.
Hess KL, Crepaz N, Rose C, Purcell D, Paz-Bailey G. Trends in sexual behavior among men who have sex with men (MSM) in high-income countries, 1990–2013: a systematic review. AIDS Behav. 2017;21(10):2811–34.
PrEP Effectiveness | PrEP | HIV Basics | HIV/AIDS | CDC [Internet]. 2021 [cited 2021 Jun 8]. Available from: https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html.
Anderson PL, Glidden DV, Liu A, Buchbinder S, Lama JR, Guanira JV, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):ra151125–151125.
Dangerfield IIDT, Anderson JN, Wylie C, Arrington-Sanders R, Bluthenthal RN, Beyrer C, et al. Refining a multicomponent intervention to increase perceived HIV risk and PrEP initiation: Focus group study among Black sexual minority men. JMIR Form Res. 2022;6(8):e34181.
Quinn K, Dickson-Gomez J, Zarwell M, Pearson B, Lewis M. A gay man and a doctor are just like, a recipe for destruction: how racism and homonegativity in healthcare settings influence PrEP uptake among young Black MSM. AIDS Behav [Internet]. 2019;23:1951–63. https://doi.org/10.1007/s10461-018-2375-z.
Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, Mayer KH. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in Black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS Care. 2017;29(11):1351–8.
Babel RA, Wang P, Alessi EJ, Raymond HF, Wei C. Stigma, HIV risk, and access to HIV prevention and treatment services among men who have sex with men (MSM) in the United States: a scoping review. AIDS Behav. 2021;25(11):3574–3604. https://doi.org/10.1007/s10461-021-03262-4.
Blumenthal J, Jain S, Mulvihill E, Sun S, Hanashiro M, Ellorin E, et al. Perceived Versus calculated HIV Risk: implications for pre-exposure Prophylaxis Uptake in a Randomized Trial of men who have sex with men. J Acquir Immune Defic Syndr. 2019;80(2):7.
Oostrom L, Rosentel K, Motley D, Hill BJ. Discordance in objective and self-perceived HIV Risk: a potential barrier to pre-exposure Prophylaxis in Young Gay and Bisexual men. J Assoc Nurses AIDS Care. 2020;31(1):103–9.
Felsher M, Szep Z, Krakower D, Martinez-Donate A, Tran N, Roth AM. I don’t need PrEP right now: a qualitative exploration of the barriers to PrEP Care Engagement through the application of the Health Belief Model. AIDS Educ Prev. 2018;30(5):369–81.
Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries 4th WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in Black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, et al. HIV among Black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2013;18(1):10–25.
Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in Black and White men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
Huang W, Lockard A, Kelley CF, Serota DP, Rolle CPM, Sullivan PS, et al. From declining PrEP to PrEP initiation as first nature – what changes PrEP initiation decisions among young, Black MSM. AIDS Care. 2022;34(3):284–93.
Gallagher T, Link L, Ramos M, Bottger E, Aberg J, Daskalakis D. Self-perception of HIV Risk and Candidacy for Pre-exposure Prophylaxis among men who have sex with men testing for HIV at Commercial Sex Venues in New York City. LGBT Health. 2014;1(3):218–24.
Weeks MR, Convey M, Dickson-Gomez J, Li J, Radda K, Martinez M, et al. Changing drug users’ risk environments: peer health advocates as Multi-level Community Change agents. Am J Community Psychol. 2009;43(3):330–44.
Young LE, Schumm P, Alon L, Bouris A, Ferreira M, Hill B et al. PrEP Chicago: a randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clin Trials. 2017;1740774517730012.
Schneider JA, Zhou AN, Laumann EO. A new HIV prevention network approach: sociometric peer change agent selection. Soc Sci Med. 2015;125(Supplement C):192–202.
Turpin RE, Hawthorne DJ, Rosario AD. Pre-exposure Prophylaxis interventions among Black sexual minority men: a systematic literature review. Int J Environ Res Public Health. 2022;19(4):1934.
Fuqua V, Chen YH, Packer T, Dowling T, Ick TO, Nguyen B, et al. Using Social Networks to Reach Black MSM for HIV Testing and linkage to Care. AIDS Behav. 2011;16(2):256–65.
Harawa NT, Schrode KM, McWells C, Weiss RE, Hilliard CL, Bluthenthal RN. Small randomized controlled trial of the New Passport to Wellness HIV Prevention Intervention for Black Men Who have sex with men (BMSM). AIDS Educ Prev. 2020;32(4):311–24.
Quinn KG, Christenson E, Spector A, Amirkhanian Y, Kelly JA. The Influence of Peers on PrEP Perceptions and Use Among Young Black Gay, Bisexual, and Other Men Who Have Sex with Men: A Qualitative Examination. Arch Sex Behav [Internet]. 2020 Feb 3 [cited 2020 Feb 10]; Available from: http://link.springer.com/https://doi.org/10.1007/s10508-019-01593-x.
Miller WR, Rollnick S. Motivational interviewing: Helping people Change. Guilford Press; 2012. p. 497.
Rollnick S, Miller WR. What is motivational interviewing? Behav Cogn Psychother. 1995;23(4):325–34.
Dangerfield II DT, Davis G, Pandian V, Anderson JN. Using motivational interviewing to increase HIV PrEP initiation and adherence: a scoping review. Prev Sci [Internet]. 2023;24:1365–75. https://doi.org/10.1007/s11121-023-01554-w.
Rollnick S, Butler CC, Kinnersley P, Gregory J, Mash B. Motivational interviewing. BMJ. 2010;340:c1900.
Elder GH. The Life Course as Developmental Theory. Child Dev. 1998;69(1):1.
Elder GH Jr. Human lives in changing societies: life course and developmental insights. In: Cairns RB, Elder GH Jr, Costello EJ, editors. Developmental science. New York, NY, US: Cambridge University Press; 1996. pp. 31–62. (Cambridge studies in social and emotional development.).
Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2(4):354–86.
Rosenstock IM. Historical origins of the health belief model. Health Educ Monographs. 1974 Dec;2(4):328–35.
Markus H, Nurius P. Possible selves. Am Psychol. 1986;41(9):954–69.
Dangerfield IIDT, Smith LR, Anderson JN, Bruce OJ, Farley J, Bluthenthal R. Sexual positioning practices and sexual risk among Black gay and bisexual men: a life course perspective. AIDS Behav. 2017;22(6):1919–31.
Bak W. Possible selves: implications for psychotherapy. Int J Ment Health Addict. 2015;13(5):650–8.
Dangerfield IIDT. A principal investigator as a PrEP-Using peer change agent for HIV prevention among Black gay and bisexual men: an autoethnography. Int J Environ Res Public Health. 2023;20(7):5309.
White JJ, Dangerfield IIDT, Grieb SM. Methodological considerations for conducting focus groups in HIV prevention research among Black men who have sex with men. Public Health Nurs. 2019;36(3):439–45.
Dangerfield IIDT, Wylie C, Anderson JN. Conducting virtual, synchronous focus groups among Black sexual minority men: qualitative study. JMIR Public Health Surveill. 2021;7(2):e22980.
Dangerfield IID, Wylie C. Identifying ethical and culturally responsive research activities to build trust and improve participation of Black sexual minority men in pre-exposure prophylaxis telehealth clinical trials: qualitative study. JMIR Hum Factors. 2022;9(1):e28798.
Dangerfield IIDT, Harawa NT, McWells C, Hilliard C, Bluthenthal RN. Exploring the preferences of a culturally congruent, peer-based HIV prevention intervention for Black men who have sex with men. Sex Health. 2018;15(5):424–30.
Dangerfield IIDT, Cooper J, Heidari O, Allen S, Winder TJA, Lucas GM. Nursing and health care preferences among opioid and stimulant using Black sexual minority men: an exploratory study. J Assoc Nurses AIDS Care. 2021;32(5):e30–9.
Miller WR, Rollnick S. Ten things that Motivational interviewing is not. Behav Cogn Psychother. 2009;37(2):129–40.
Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1(1):91–111.
Napper LE, Fisher DG, Reynolds GL. Development of the Perceived risk of HIV Scale. AIDS Behav. 2012;16(4):1075–83.
Wanyonyi KL, Themessl-Huber M, Humphris G, Freeman R. A systematic review and meta-analysis of face-to-face communication of tailored health messages: implications for practice. Patient Educ Couns. 2011;85(3):348–55.
Bauermeister JA, Pingel ES, Jadwin-Cakmak L, Harper GW, Horvath K, Weiss G, et al. Acceptability and preliminary efficacy of a tailored online HIV/STI Testing Intervention for Young Men who have sex with men: the get connected! Program. AIDS Behav. 2015;19(10):1860–74.
Hosek SG, Lemos D, Hotton AL, Fernandez MI, Telander K, Footer D, et al. An HIV intervention tailored for Black young men who have sex with men in the House Ball Community. AIDS Care. 2015;27(3):355–62.
Dangerfield II DT, Lipson A, Anderson JN. HIV PrEP clinician communication preferences among Black sexual minority men. AIDS Educ Prev. 2022;34(2):168–81.
Underhill K, Guthrie KM, Colleran C, Calabrese SK, Operario D, Mayer KH. Temporal fluctuations in Behavior, Perceived HIV Risk, and willingness to Use Pre-exposure Prophylaxis (PrEP). Arch Sex Behav. 2018;47(7):2109–21.
Dangerfield II DT, Cooper J, Heidari O, Allen S, Winder TJA, Lucas GM. Nursing and health care preferences among opioid and stimulant using Black sexual minority men: an exploratory study. J Assoc Nurses AIDS Care. 2021 Oct;32(5):e30–9. https://journals.lww.com/janac/Abstract/9000/Nursing_and_Health_Care_Preferences_Among_Opioid.99850.aspx.
Dangerfield IIDT, Heidari O, Cooper J, Allen S, Lucas GM. Motivations for opioid and stimulant use among drug using Black sexual minority men: a life course perspective. Drug Alcohol Depend. 2020;215:108224.
Dangerfield IIDT, Harawa NT, Fernandez MI, Hosek S, Lauby J, Joseph H, et al. Age cohort differences in sexual behaviors among Black men who have sex with men and women. J Sex Res. 2018;55(8):1012–21.
Acknowledgements
This study was supported by the National Institute of Mental Health (K01MH118943) and has been facilitated by the infrastructure and resources provided by the Johns Hopkins University Center for AIDS Research, an NIH funded program (1P30AI094189), which is supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIGMS, NIDDK, NIMHD. The content is solely the responsibility of the author and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dangerfield II, D.T., Anderson, J.N. A Scripted, PrEP-Using Peer Change Agent Improves Perceived Risk for HIV and Willingness to Accept Referrals Quickly Among Black Sexual Minority Men: Preliminary Findings from POSSIBLE. AIDS Behav (2024). https://doi.org/10.1007/s10461-024-04313-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s10461-024-04313-2