Abstract
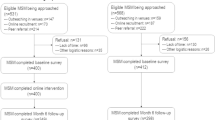
Southeast Michigan accounts for over 70 % of all HIV/STI cases in the state, with young men who have sex with men (YMSM) between the ages of 13 and 24 encumbering the largest burden in HIV/STI incidence. Using community-based participatory research principles, we developed and pilot tested a web-based, randomized control trial seeking to promote HIV/STI testing (“Get Connected!”) among YMSM (N = 130; ages 15–24). Randomized participants completed a baseline assessment and shown a test-locator condition (control) or a tailored, personalized site (treatment). At 30-day follow-up, we found high acceptability among YMSM in both conditions, yet higher credibility of intervention content among YMSM in the treatment group (d = .55). Furthermore, 30 participants reported testing by following, with the majority of these participants (73.3 %; n = 22) completing the treatment condition, a clinically meaningful effect (d = .34) suggesting preliminary efficacy for the intervention. These results demonstrate the potential of the intervention, and suggest that a larger efficacy trial may be warranted.
Resumen
El Sudeste de Michigan contiene más del 70 % de todos los casos de VIH/ETS en el estado, con JHCH (jóvenes hombres que tienen sexo con hombres) entre las edades de 13 y 24 sufriendo la mayor incidencia de VIH/ETS. Utilizando los principios de investigación participativa y comunitaria, hemos desarrollado y examinado un proyecto piloto, con diseñode ensayo aleatorizado de control basado en promover la prueba de VIH/ETS (“Get Connected!”) entre JHCH (N = 130 entre los 15 y 24 años). Los JHCH completaron un cuestionario inicial y asignados a una condición control (acceso a un localizador de pruebas) o a un grupo de tratamiento (un sitio web personalizado). A los 30 días de seguimiento, encontramos una alta aceptación a ambas condiciones de la intervención; sin embargo, encontramos una mayor credibilidad al contenido entre los JHCH en el grupo de tratamiento (d = .55). Treinta participantes se reportaron haberse hecho una prueba de VIH/ETS durante el seguimiento, con la mayoría de los participantes (73.3 %, n = 22) siendo parte de la condición de tratamiento, un efecto clínicamente significativo (d = .34) que sugiere la eficacia preliminar de la intervención. Estos resultados demuestran el potencial de laintervención, y sugieren un estudio de eficacia con una muestra más grande de JHCH.




Similar content being viewed by others
References
Michigan Department of Community Health. Annual HIV surveillance report, Michigan 2014 [Internet]. 2014. http://www.michigan.gov/documents/mdch/January_2014_ALL_446611_7.pdf. Accessed 4 Aug 2014.
U.S. Centers for Disease Control and Prevention. HIV among gay, bisexual, and other men who have sex with men [Internet]. 2014. http://www.cdc.gov/hiv/risk/gender/msm/facts/index.html. Accessed 23 Apr 2014.
Michigan Department of Community Health. Michigan 2012 sexually transmitted diseases report [Internet]. 2014. http://www.mdch.state.mi.us/pha/osr/Index.asp?Id=12. Accessed 4 Aug 2014.
Higa DH, Crepaz N, Marshall KJ, Kay L, Vosburgh HW, Spikes P, et al. A systematic review to identify challenges of demonstrating efficacy of HIV behavioral interventions for gay, bisexual, and other men who have sex with men (MSM). AIDS Behav. 2013;17:1231–44.
Grossman CI, Forsyth A, Purcell DW, Allison S, Toledo C, Gordon CM. Advancing novel HIV prevention intervention research with MSM-meeting report. Public Health Rep. 2011;126:472–9.
Harper GW. Sex isn’t that simple: culture and context in HIV prevention interventions for gay and bisexual male adolescents. Am Psychol. 2007;62:803–19.
Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48:218–53.
Allison S, Bauermeister JA, Bull S, Lightfoot M, Mustanski B, Shegog R, et al. The intersection of youth, technology, and new media with sexual health: moving the research agenda forward. J Adolesc Health. 2012;51:207–12.
Meanley S, Gale A, Harmell C, Jadwin-Cakmak L, Pingel E, Bauermeister JA. The role of provider interactions on comprehensive sexual healthcare among young men who have sex with men. AIDS Educ Prev. 2015;27(1):15–26.
Grov C, Breslow AS, Newcomb ME, Rosenberger JG, Bauermeister JA. Gay and bisexual men’s use of the Internet: research from the 1990s through 2013. J Sex Res. 2014;51:390–409.
Pingel ES, Thomas L, Harmell C, Bauermeister JA. Creating comprehensive, youth centered, culturally appropriate sex education: what do young gay, bisexual and questioning men want? Sex Res Soc Policy. 2013;10:293–301.
Pingel ES, Bauermeister JA, Johns MM, Eisenberg A, Leslie-Santana M. “A safe way to explore”: reframing risk on the internet amidst young gay men’s search for identity. J Adolesc Res. 2013;28:453–78.
Mustanski B, Lyons T, Garcia SC. Internet use and sexual health of young men who have sex with men: a mixed-methods study. Arch Sex Behav. 2011;40:289–300.
Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res. 2008;23:454–66.
Kreuter MW, Strecher VJ, Glassman B. One size does not fit all: the case for tailoring print materials. Ann Behav Med. 1999;21:276–83.
Outlaw AY, Naar-King S, Parsons JT, Green-Jones M, Janisse H, Secord E. Using motivational interviewing in HIV field outreach with young African American men who have sex with men: a randomized clinical trial. Am J Public Health. 2010;100(Suppl):S146–51.
Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: a community-level HIV prevention intervention for young gay men. Am J Public Health. 1996;86(8_Pt_1):1129–36.
Noar SM, Pierce LB, Black HG. Can computer-mediated interventions change theoretical mediators of safer sex? A meta-analysis. Hum Commun Res. 2010;36:261–97.
Strecher V. Internet methods for delivering behavioral and health-related interventions (eHealth). Annu Rev Clin Psychol. 2007;3:53–76.
Chiasson MA, Hirshfield S, Rietmeijer C. HIV prevention and care in the digital age. J Acquir Immune Defic Syndr. 2010;55:S94–7.
Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20:1447–50.
Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39:446–53.
Knight RE, Shoveller JA, Carson AM, Contreras-Whitney JG. Examining clinicians’ experiences providing sexual health services for LGBTQ youth: considering social and structural determinants of health in clinical practice. Health Educ Res. 2014;29(4):662–70.
Pingel ES, Sullivan S, Jadwin-Cakmak L, Alapati D, Moore M, Meanley S, Lowther M, Wade R, Harper G, Bauermeister JA. “I have your results”: delivering evaluation data to HIV/STI testing sites regarding issues of LGBT sensitivity and inclusivity. In: Oral presentation offered at the 2014 American Public Health Association annual meeting, New Orleans, LA (November 19); 2014.
Millett G, Ding H, Marks G, Jeffries W, Bingham T, Lauby J, et al. Mistaken assumptions and missed opportunities: correlates of undiagnosed HIV infection among Black and Latino men who have sex with men. AIDS. 2011;58:64–71.
Israel BA, Schulz AJ, Parker EA, Becker AB, Allen A, Guzman JR. Critical issues in developing and following community-based participatory research principles. In: Minkler M, Wallerstein N, editors. Community-based participatory research for health. San Francisco: Jossey-Bass; 2003. p. 53–76.
Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78.
Hornik R, Ajzen I, Albarracín D. An extension of the theory of reasoned action and its successors to multiple behavior interventions. In: Predicting change in a health behavior: applying a reasoned action approach. Mahwah: Lawrence Erlbaum Associates; 2007. p. 53–67.
Kalichman SC, Ajzen I, Albarracin D, Hornik R. The theory of reasoned action and advances in HIV/AIDS prevention. In: Predicting change in a health behavior: applying a reasoned action approach. Mahwah: Lawrence Erlbaum Associates; 2007. p. 265–72.
Bauermeister JA, Hickok AM, Meadowbrooke C, Veinot T, Loveluck J. Self-efficacy among young men who have sex with men: an exploratory analysis of HIV/AIDS risk behaviors across partner types. AIDS Behav. 2013;18:69–77.
Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63:484–9.
Dittus PJ, De Rosa CJ, Jeffries RA, Afifi AA, Cumberland WG, Chung EQ, et al. The Project Connect Health Systems intervention: linking sexually experienced youth to sexual and reproductive health care. J Adolesc Health. 2014; http://www.ncbi.nlm.nih.gov/pubmed/24856358.
Kubicek K, Carpineto J, McDavitt B, Weiss G, Kipke M. Use and perceptions of the internet for sexual information and partners: a study of young men who have sex with men. Arch Sex Behav. 2010;2010:1–14.
Kubicek K, Carpineto J, McDavitt B, Weiss G, Iverson EF, Au C-W, et al. Integrating professional and folk models of HIV risk: YMSM’s perceptions of high-risk sex. AIDS Educ Prev. 2008;20:220–38.
Mimiaga MJ, Goldhammer H, Belanoff C, Tetu AM, Mayer KH. Men who have sex with men: perceptions about sexual risk, HIV and sexually transmitted disease testing, and provider communication. Sex Transm Dis. 2007;34:113–9.
Eaton LA, Huedo-Medina TB, Kalichman SC, Pellowski JA, Sagherian MJ, Warren M, et al. Meta-analysis of single-session behavioral interventions to prevent sexually transmitted infections: implications for bundling prevention packages. Am J Public Health. 2012;102:e34–44.
Glick SN, Winer RL, Golden MR. Web-based sex diaries and young adult men who have sex with men: assessing feasibility, reactivity, and data agreement. Arch Sex Behav. 2013;42:1327–35.
Acknowledgments
This research was supported by an award from the National Association of County and City Health Officials (NACHHO) and the MAC AIDS Fund to Dr. Bauermeister. Dr. Bauermeister was supported through a NIH Career Development Award (K01-MH087242). We thank our CAB and YAB for their contributions during the development and implementation of the intervention.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bauermeister, J.A., Pingel, E.S., Jadwin-Cakmak, L. et al. Acceptability and Preliminary Efficacy of a Tailored Online HIV/STI Testing Intervention for Young Men who have Sex with Men: The Get Connected! Program. AIDS Behav 19, 1860–1874 (2015). https://doi.org/10.1007/s10461-015-1009-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1009-y