Abstract
Purpose
Dementia and chronic pain (CP) are prevalent among older adults. However, no study has systematically reviewed the association between dementia and CP. Therefore, we performed this study to gather evidence about the potential relationship between the two.
Methods
Two authors independently searched PubMed, Embase, and Web of Science to identify all records published up to 1 September 2022 that explored the association between CP and dementia. The methodological quality of the studies was assessed using the Newcastle Ottawa Scale (NOS). A fixed or random-effects model was used to pool the risk estimates.
Results
Among the initial 3296 articles retrieved, 19 were included in the review (1 cross-sectional, and 18 cohort). The pooled result showed the risk of dementia was 1.42 times higher in CP patients (HR = 1.42, 95% CI 1.23–1.64, P < 0.001). dementia and CP subtypes, gender, and age did not significantly affect the results.
Conclusion
Our study shows that people who suffered from CP are at an increased risk of developing dementia, regardless of gender, age, and dementia and CP subtypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pain (CP) is defined by the International Association for the Study of Pain (IASP) as pain that lasts for more than 3 months (Turk et al. 2011; International Association for the Study of Pain 1986). It affects over 30% of people worldwide and is associated with secondary disabilities and comorbidities such as anxiety, depression, and suicide (Cohen et al. 2021; Vos et al. 2012; Dueñas et al. 2015; Fayaz et al. 2016). Arthritis and primary chronic pain syndromes are among the most common types of chronic pain conditions (Ossipov and Porreca 2006). The elderly population, particularly those over 65 years old, are particularly prone to CP, leading to significant suffering, including distress, social isolation, disability, and increased healthcare costs (Dahlhamer et al. 2018; Tsang et al. 2008; Patel and Guralnik 2013; Leveille et al. 2009; Pitcher and Korff 2018; Bernfort et al. 2015). Early identification and effective treatment of pain can greatly improve the quality of life for older adults, reducing the risk of falls, agitation, depression, and anxiety (Hellstrom et al. 2004; Smalbrugge et al. 2007; Frederick 2016). Therefore, the relief of pain holds great importance in both clinical practice and scientific research.
There is growing evidence indicating that the health consequences of pain are associated with the onset and progression of dementia (Whitlock et al. 2017; Belin and Gatt 2006; Wang et al. 2022; Wang and Liu 2021; Khalid et al. 2022, 2020; Innes and Sambamoorthi 2020; Whitlock et al. 2017 Aug 1b; Rouch et al. 2022; Tzeng et al. 2018; Cheng et al. 2022; Kao et al. 2021; Hurh et al. 2022; Morton et al. 2019; Hagen et al. 2014; Islamoska et al. 2020; George et al. 2020; Lee et al. 2019; Kostov et al. 2019; Chen et al. 2018; Huang et al. 2015), which is a critical issue. Neurodegenerative diseases, such as Alzheimer’s disease and related dementias, are increasingly prevalent worldwide due to the rapid aging of the global population. This poses a significant and urgent public health crisis (Abubakar et al. 2015; Feigin et al. 2017; Alzheimer’s Association 2021; Sanders and Morano 2008), leading to disability, institutionalization, and premature mortality. Dementia imposes a substantial burden on individuals, society, and the economy. By screening for dementia and implementing preventative and therapeutic interventions, utilizing pain as a risk factor, we aim to alleviate the burden of disability, reduce rates of institutionalization, and extend life expectancy. To explore the relationship between chronic pain and dementia, we conducted a systematic review and meta-analysis.
Methods and materials
This meta-analysis was reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA 2020) statement (Page et al. 2021).
Search strategy
A systematic search was conducted on PubMed, Embase, and Web of Science to identify studies related to chronic pain and dementia (Online Appendix 1). The following search terms were used: “Chronic pain,” “Pains, Chronic,” “Widespread or Chronic Pains,” “Intractable Pain,” “Refractory Pains,” “Pain, Refractory,” “Dementia,” “Alzheimer’s Disease,” “Alzheimer’s Type Dementia,” “ATD,” and “Alzheimer Type Dementia, Early Onset.” The literature search covered articles up until September 1, 2022. Two researchers independently screened the literature, and in cases where consensus could not be reached, a third researcher reviewed the full text and resolved any differences. There were no language restrictions or filters applied to the search. Additionally, we checked the bibliographies of relevant reviews, articles, and books for further references.
Inclusion and exclusion criteria
The studies included in the meta-analysis had to meet the following criteria: (a) being observational case–control, cohort, or cross-sectional studies; (b) focusing on chronic pain or specific subtypes of chronic pain as the primary exposure factor associated with the risk of dementia; (c) reporting effect estimates with corresponding 95% confidence intervals (CIs), or providing sufficient data to calculate crude risk ratios (HRs) for the association between chronic pain and dementia. Studies were excluded if they met any of the following criteria: (a) being published only as letters or abstracts; (b) not reporting quantitative outcome data; (c) not published in English; (d) being case reports; and (e)studies were excluded if they lacked access to the complete set of literature or if the full text was not obtainable.
Study selection and data extract
Two authors (WZZ and SZ) will independently extract data from the included studies. Before starting the review process, a pre-made Excel datasheet will be used to collect the following information: general details (title, author, country of study, year of publication), study characteristics (study design, inclusion and exclusion criteria), study population (age, sex, sample size, number of analyses, type of chronic pain, dementia subtype), exposure characteristics (type of chronic pain, duration, duration of follow-up), and outcomes (primary and secondary outcomes, time points, methods of outcome evaluation). If necessary, the authors of the original trials will be contacted for additional information and clarification of the data. Any discrepancies or disagreements will be resolved through discussion and consensus.
Statistical analysis
The data analysis for this study was conducted using Stata 17.0. Hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were used to assess the predictive effect of chronic pain on the risk of dementia. Heterogeneity between studies was assessed using Cochran’s Q-test and Higgins’ I2 statistics. If I2 and p-value for heterogeneity were greater than 0.05, fixed effects models were used to pool the results. In cases where significant heterogeneity existed, random-effects models were employed (Higgins et al. 2003). Univariate meta-regression analysis was conducted to identify potential sources of heterogeneity. Subgroup analyses were performed based on dementia subtype, chronic pain subtype, country, age (mean/median year < 65 or ≥ 65), severity, gender (male, female), follow-up time, education level (low, medium, high), and study design.
If there was insufficient validity data provided in a study for meta-analysis, a narrative approach was used to describe the relevant findings. Sensitivity analysis was conducted by excluding one study at a time to evaluate the stability of the results. Additionally, multiple studies were excluded simultaneously in sensitivity analysis to determine the robustness of the findings. Publication bias was assessed by examining funnel plot asymmetry and conducting Egger’s test and Begg’s test (significance threshold: p < 0.05). If both the p-values and funnel plots showed symmetry, it indicated no publication bias (Egger et al. 1997).
Study quality assessment
The quality of the included cohort studies was evaluated using the Newcastle–Ottawa Scale (NOS), which assesses three components: selection, comparability, and outcome. A NOS score of 7 indicates high quality, while a lower score suggests a higher risk of bias (Stang 2010). For the included cross-sectional studies, the quality assessment was conducted using the Agency for Healthcare Research and Quality (AHRQ) criteria. One author assessed the quality of individual studies, and another author independently checked the assessments. Any disagreements were resolved through consensus.
Results
Study characteristic
The included studies in this meta-analysis were conducted across eight countries: the United States (Wang et al. 2022; Wang and Liu 2021; Khalid et al. 2022, 2020; Innes and Sambamoorthi 2020; Whitlock et al. 2017; George et al. 2020), China (Tzeng et al. 2018; Cheng et al. 2022; Kao et al. 2021; Chen et al. 2018; Huang et al. 2015), France (Rouch et al. 2022), the United Kingdom (Kostov et al. 2019), Korea (Kao et al. 2021; Lee et al. 2019), Norway (Hagen et al. 2014), Canada (Morton et al. 2019), and Denmark (Islamoska et al. 2020). All of these studies were population-based and involved a total of 842,806 subjects, including 132,445 patients with chronic pain. Among the included studies, one was cross-sectional (Wang et al. 2022) and two were case–control designs (Lee et al. 2019; Chen et al. 2018), while the remaining 16 studies were cohort studies. Eighteen studies examined the risk of developing dementia after a diagnosis of chronic pain (Wang and Liu 2021; Khalid et al. 2022, 2020; Innes and Sambamoorthi 2020; Whitlock et al. 2017; Rouch et al. 2022; Tzeng et al. 2018; Cheng et al. 2022; Kao et al. 2021; Hurh et al. 2022; Morton et al. 2019; Hagen et al. 2014; Islamoska et al. 2020; George et al. 2020; Lee et al. 2019; Kostov et al. 2019; Chen et al. 2018; Huang et al. 2015), and one study explored the comorbidity of dementia in patients with chronic pain (Wang et al. 2022).
Diagnosis of chronic pain and dementia in the medical records databases relied on diagnostic codes such as the International Classification of Diseases. The gender distribution was generally balanced across the included studies, but the median/mean age varied among the studies, mostly being over 50 years, except for two studies where age information was not reported (Islamoska et al. 2020; Huang et al. 2015), and one study that included individuals aged > 20 years (Hagen et al. 2014). Fifteen cohort studies had follow-up periods ranging from 2 to 16 years, while one study did not provide follow-up duration (Wang et al. 2022; Lee et al. 2019; Chen et al. 2018). Age, gender, and comorbidities were matched and/or adjusted for in all studies. Table 1 provides detailed information for each study.
Table 2 shows that all cohort studies are of high quality (Scores of 8 to 11 are considered high quality). Despite the absence of follow-up data, this is because the cross-sectional design does not require follow-up data (Wang et al. 2022).
Results
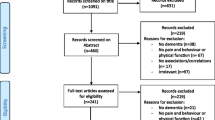
A total of 3311 potentially relevant papers were identified through the pre-developed search strategies. After removing 3025 duplicate records, the titles and abstracts of 3081 remaining records were screened for relevance. Following this screening process, 19 studies were included in this systematic review after a full-text reading of 230 papers. The study selection process and the reasons for exclusion after full-text reading are presented in Fig. 1.
The association between chronic pain and risk of dementia
A total of 19 studies involving 908,849 participants were included in the overall meta-analysis, heterogeneity testing indicated substantial heterogeneity among studies (I2 = 97.5%, P < 0.001), so the random-effects model was applied. The pooled results showed a 42% increased risk of dementia in CP participants. (HR = 1.42, 95% CI 1.23–1.64, P < 0.001) (Fig. 2).
Subgroup analyses
Stratified analyses were conducted to examine the potential effects of various factors on the association between dementia and chronic pain. These factors included subtypes of dementia, subtypes of chronic pain, country of study, study design, follow-up time, age, and gender.
Subgroup analyses showed that Trigeminal Neuralgia (HR = 4.47, 95% CI 3.09–6.47, P < 0.001), Fibromyalgia (HR = 2.77, 95% CI 2.61–2.95, P < 0.001), Widespread pain (HR = 1.43, 95% CI 1.06–1.92, P < 0.001), Osteoarthritis (HR = 1.31, 95% CI 1.14–1.52, P < 0.001), Migraine (HR = 1.26, 95% CI 1.16–1.36, P < 0.001), and chronic non-cancerous pain (CNCP) (HR = 1.15, 95% CI 1.09–1.21, P < 0.001) were significantly associated with subsequent higher dementia risk. Furthermore, Wang et al., Hurh et al., Kostev et al. explored the association between CP and the risk of different dementia subtypes. All dementia subtypes were associated with an increased risk of CP, ranging from 36 to 44%.
Only Kao et al. (2021) assessed the association between the duration of follow-up on CP and subsequent dementia risk. Their results showed that the association between CP and dementia risk was comparable between long-term follow-up (> 5 years) and follow-up periods of less than 5 years. In terms of impacts of age, the risk of dementia seems to be similar for people over 65 years of age and those under 65 years of age (HR = 1.53, 95% CI 1.21–1.93, P < 0.001 vs. HR = 1.33, 95% CI 1.16–1.52, P < 0.001, respectively). The association between CP and dementia risk was similar between the female and male subgroups (HR = 1.49, 95%CI 1.23–1.79, P = 0.000 vs. HR = 1.36, 95%CI 1.10–1.69, P = 0.005, respectively). The educational level did not affect dementia risk (Table 3). Notably, In the country subgroup analysis, the pooled results from the studies in America (HR = 1.12, 95% CI 0.99–1.27, P = 0.704) and French (HR = 1.23, 95% CI 0.88–1.73, P = 0.230) showed no significant correlation between CP and dementia. In other countries, CP was consistently associated with higher risks of dementia. In subgroups of study type, the association between CP and dementia risk was similar in cohort studies and case–control studies but was only statistically significant in the former. Interestingly, there was no association in the cross-sectional studies.
Sensitivity analysis and evaluation for publication bias
A sensitivity analysis was conducted by excluding one study at a time to assess the stability of the pooled results. The analysis revealed that the effect sizes remained stable, indicating the robustness of the findings (Fig. 3). The p-values for Begg’s and Egger’s tests were 0.036 and 0.805, respectively. The funnel plots displayed slight asymmetry, suggesting a potential publication bias (Fig. 4A). However, no missing hypothesis studies were identified in the trim-and-fill method (Fig. 4B), indicating that the current pooled result is relatively robust. Furthermore, due to the high heterogeneity observed, we examined the robustness of each meta-analysis by comparing the results of the random effects model with those of the fixed effects model. The pooled results of the fixed effects model showed consistent findings across all groups, except for the American group, where the results changed from insignificant to significant (Table 4).
Discussion
Principal findings
Our findings indicate a positive association between chronic pain (CP) and dementia. Overall, individuals with chronic pain have a 42% increased risk of developing dementia (HR = 1.42, 95% CI 1.23–1.64, p < 0.001), suggesting that chronic pain may serve as a risk factor for dementia. Notably, this risk remains consistent regardless of age, indicating that age does not significantly influence the relative risk of developing dementia in individuals with chronic pain. Additionally, we conducted subgroup analyses to explore the effects of different factors on the association between dementia and chronic pain. These factors include subtypes of dementia, subtypes of chronic pain, age, gender, region, follow-up time, educational level, and study design.
Comparison with other reviews
A systematic review published in 2020 suggested that chronic pain and specific chronic pain conditions may be associated with an increased risk of developing dementia (Innes and Sambamoorthi 2020). However, most studies included in their review were conducted in Taiwan (China), which may have introduced a geographic bias in the results.
In contrast, our meta-analysis included studies from various countries worldwide, providing a more comprehensive and reliable estimate of the association. We not only conducted a qualitative analysis of the association between different subtypes of chronic pain and dementia, but also performed a quantitative pooling of hazard ratios to draw comprehensive conclusions. This approach minimizes bias and provides a more accurate estimation of the true risk measure. While our study’s overall findings regarding the increased risk of dementia in individuals with chronic pain were consistent with the previous review, we found a 42% increased risk of dementia in chronic pain patients compared to those without chronic pain (HR = 1.42, 95% CI 1.23–1.64, p < 0.001). It is important to note that the study samples in our meta-analysis were drawn from diverse cultural, social, and economic backgrounds. However, due to the limited number of studies available from each country or region, we were unable to fully consider the potential impactof these factors. Mendelian randomization analysis could be a valuable approach to further explore the causal relationships in future research.
Potential interpretations of the results
It is important to interpret subgroup comparisons cautiously due to the small number of studies available. In our subgroup analysis, we found that individuals with chronic pain (CP) were significantly more likely to develop dementia across multiple subtypes of chronic pain, except in one cross-sectional study. In this particular cross-sectional study, dementia was associated with a lower risk of pain. However, due to the nature of cross-sectional study design, it is difficult to determine whether dementia was caused by other factors or if it influenced the perception of pain (Wang et al. 2022).
In this particular cross-sectional study, dementia was associated with a lower risk of pain. However, due to the nature of cross-sectional study design, it is difficult to determine whether dementia was caused by other factors or if it influenced the perception of pain (Wang et al. 2022). Furthermore, a majority of the studies included in our analysis indicated that the risk of dementia increased as the age of individuals with chronic pain advanced (Wang and Liu 2021; Khalid et al. 2022, 2020; Innes and Sambamoorthi 2020; Whitlock et al. 2017; Rouch et al. 2022; Tzeng et al. 2018; Cheng et al. 2022; Kao et al. 2021; Hurh et al. 2022; Morton et al. 2019; Hagen et al. 2014; Islamoska et al. 2020; George et al. 2020; Lee et al. 2019; Kostov et al. 2019; Chen et al. 2018; Huang et al. 2015). This suggests that older age may be a contributing factor to the development of dementia in individuals with chronic pain.
It is important to note that a study conducted by Wang et al. (2022) found that older Americans with dementia are less likely to report the use of pain medications when they experience pain. This finding aligns with previous research highlighting the issue of pain undertreatment among older individuals with dementia (Boltz et al. 2021; Wang et al. 2020; Gilmore-Bykovskyi et al. 2019). Several factors contribute to this phenomenon, including the potential for forgetfulness in reporting pain, lack of recognition of symptoms by clinicians or family members, and the presence of other symptoms such as anxiety, depression, hallucinations, and paranoia, which may lead to medication non-adherence. Additionally, individuals with dementia may face barriers in receiving regular medical checkups, such as mobility issues, forgetfulness, or caregiver constraints. Caregivers themselves may also be unaware of the potential benefits of anti-inflammatory drugs in managing the conditions of these patients. Therefore, healthcare providers need to consider these barriers to appropriate care when treating patients with dementia. While the exact reasons behind this phenomenon cannot be fully determined from research data alone, there is a growing body of literature suggesting that anti-inflammatory drugs may hold promise in preventing Alzheimer’s disease (McGeer and McGeer 1990; Canadian Study of Health and Aging 1994; Breitner et al. 1994). Thus, it is crucial to monitor the occurrence of Alzheimer’s disease and implement preventive measures in individuals with chronic pain to reduce their risk of developing the disease. By remaining vigilant and applying suitable interventions, we may be able to mitigate the impact of chronic pain on cognitive health and improve the overall quality of life for those affected.
Furthermore, Cheng et al. found that depression may be one of the reasons why individuals with trigeminal neuralgia (TN) have a 4.47-fold higher risk of developing dementia compared to those without TN. This finding is consistent with previous research suggesting that the incidence of depression, anxiety, and functional impairment can increase with the severity of pain (Melek et al. 2018). Chronic depression itself is a known factor that predisposes individuals to dementia (Maˇ cianskyt˙e et al. 2011). It has been proposed that the synthesis of NMDA glutamate agonists, such as quinolinic acid and kynurenine metabolites, can lead to oxidative stress and result in a chronic inflammatory state (Leonard 2017). Therefore, it is plausible to suggest that TN may increase the risk of dementia by promoting depression. This novel insight is supported by the study conducted by Cheng et al., which provides additional scientific evidence for this possibility.
The mechanisms underlying the interaction between chronic pain (CP) and dementia are not fully understood. However, current evidence suggests that CP may contribute to an increased risk of dementia through multiple pathways. Several studies have demonstrated that brain pathology associated with dementia can be influenced by pain-related psychopathology. Chronic pain can also provoke dysfunction in the locus coeruleus (LC) and neuroinflammation in dementia patients, leading to neurodegeneration (Monroe et al. 2017, 2012; Cao et al. 2019; Cole et al. 2006, 2011). These changes have been observed in various regions of the brain, including the frontal cortex, where anomalies in the noradrenergic system are frequently observed (Hayashida and Obata 2019). Microglial activation in areas like the LC and increased central neuroinflammation in these regions have also been implicated (Salter and Stevens 2017). The LC plays a crucial role in norepinephrine (NE) synthesis and subsequent neurotransmission in the central nervous system, and dysfunction in the LC-NE signaling pathway has been associated with microglial dysfunction (Gyoneva and Traynelis 2013).
In addition, chronic pain is associated with increased levels of systemic inflammation (Coe et al. 2008; Marchand et al. 2005). Moreover, markers of systemic inflammation can vary among different ethnic and racial groups (Paalani et al. 2011). Inflammation associated with aging has also been linked to dementia and Alzheimer’s disease pathology (Schain and Kreisl 2017; Eldik et al. 2016). Therefore, understanding the underlying mechanisms that contribute to sociodemographic findings requires considering inflammatory factors and their potential impact on the association between chronic pain and dementia.
Recommendations for research and clinical practice
We found that there is a limited number of studies investigating the association between different subtypes of chronic pain in individuals with dementia, most of which were retrospective cohort studies. To improve pain management in this population, we propose that the first step is to evaluate changes in pain management interventions by monitoring pain intensity. However, distinguishing between behaviors associated with pain and those arising from the dementia process itself can be challenging, posing a significant clinical and research dilemma.
It is essential to recognize that while some pain assessment scales primarily focus on identifying the presence of pain, others, such as the Visual Analog Scale (VAS) and the Numerical Rating Scale (NRS), are specifically designed to evaluate the intensity of pain. Therefore, the choice of a pain assessment scale should align with the specific objectives of the assessment, considering both the identification and quantification of pain. Therefore, we emphasize the use of pain assessment tools that have been validated and tested for responsiveness in well-powered trials of analgesics specifically conducted in moderate to severe dementia patients for future research. Adopting such an approach will allow us to better understand the relationship between different subtypes of chronic pain and dementia, ultimately informing the development of effective pain management strategies in this population. Caregivers in community settings, residential care facilities, nursing homes, and hospitals play a crucial role in enhancing early management and treatment of pain in individuals with dementia and providing appropriate care to prevent adverse outcomes. Finally, further research investigating end-of-life care in this population is necessary to address the unique challenges posed by pain management in individuals with dementia during this stage of life.
Limitations
Although we conducted a comprehensive literature search and rigorous methodological evaluation, there are some limitations to our findings on the relationship between chronic pain and dementia. Firstly, it’s important to note that there is a wide range of subtypes of chronic pain, and limited original research exists that specifically examines the impact of each subtype on dementia. Therefore, further studies are needed to explore the association between chronic pain subtypes and dementia in more detail. Secondly, pain is subjective and highly personal, making it challenging to measure accurately. Most studies rely solely on self-reported measures of pain, which may be less specific and sensitive compared to clinical trials. This subjectivity can contribute to publication bias and heterogeneity in meta-analyses. However, it’s worth mentioning that heterogeneity is not necessarily invalidating for observational study meta-analyses (Noubiap et al. 2019). Additionally, as dementia progresses slowly and insidiously, it becomes difficult to draw definitive conclusions regarding causality. Furthermore, the studies included in our review were conducted in different countries and regions, where the research sample may be influenced by diverse cultural, social, and economic backgrounds. The limited number of studies from each country/region makes it challenging to assess how these factors may impact the results. In conclusion, while our review provides valuable insights into the relationship between frailty, chronic pain, and dementia, it is important to consider these limitations. Encouraging further research in this area, including studies that examine specific subtypes of chronic pain and consider cultural and social factors, will help obtain a more comprehensive understanding of the association between chronic pain and dementia.
Conclusions
In conclusion, there is an association between CP and dementia, with individuals with CP being at a higher risk of developing dementia regardless of gender, age, or specific dementia subtypes. Enhancing the quality of life for individuals with CP requires providing education about dementia and implementing regular dementia screening measures. Further extensive research is needed to confirm and extend the findings of this study, identify potential mediating factors, and explore the underlying mechanisms for the observed association between CP and dementia. Through more comprehensive studies, we can gain a better understanding of this relationship and develop targeted interventions to mitigate the impact of CP on dementia.
Availability of data and materials
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
References
Abubakar I, Tillmann T, Banerjee A (2015) Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet 385:117–171
(2021) Alzheimer's disease facts and figures. Alzheimers Dement. 17(3):327–406. https://doi.org/10.1002/alz.12328
Belin C, Gatt MT (2006) Douleur et démence Pain and dementia. Psychol Neuropsychiatr Vieil 4(4):247–254
Bernfort L, Gerdle B, Rahmqvist M, Husberg M, Levin LÅ (2015) Severity of chronic pain in an elderly population in Sweden—impact on costs and quality of life. Pain 156(3):521–527
Boltz M, Resnick B, Kuzmik A et al (2021) Pain incidence, treatment, and associated symptoms in hospitalized persons with dementia. Pain Manag Nurs 22:158–163
Breitner CS, Gau BA, Welsh KA et al (1994) Inverse association of anti-inflammatory treatments and Alzheimer’s disease: initial results of a co-twin control study. Neurology 44:227–232
Canadian Study of Health and Aging (1994) Risk factors for Alzheimer’s disease in Canada. Neurology 44:2073–2080
Cao S, Fisher DW, Yu T, Dong H (2019) The link between chronic pain and Alzheimer’s disease. J Neuroinflammation 16:204
Chen JH, Lin KP, Chen YC (2009) Risk factors for dementia. J Formos Med Assoc 108:754–764
Chen KT, Chen YC, Fan YH et al (2018) Rheumatic diseases are associated with a higher risk of dementia: a nation-wide, population-based, case-control study. Int J Rheum Dis 21(2):373–380
Cheng YH, Wu CH, Wang WT et al (2022) Trigeminal neuralgia is a dementia risk factor: a retrospective cohort study. Int J Environ Res Public Health 19(10):6073. https://doi.org/10.3390/ijerph19106073.PMID:35627610;PMCID:PMC9142042
Coe CL, Muller DA, Schell K (2008) Altered cytokine levels in the blood and cerebrospinal fluid of chronic pain patients. J Neuroimmunol 195:157–163
Cohen SP, Vase L, Hooten WM (2021) Chronic pain: an update on burden, best practices, and new advances. Lancet 397(10289):2082–2097. https://doi.org/10.1016/S0140-6736(21)00393-7
Cole LJ, Farrell MJ, Duff EP et al (2006) Pain sensitivity and fMRI pain-related brain activity in Alzheimer’s disease. Brain 129:2957–2965
Cole LJ, Gavrilescu M, Johnston LA et al (2011) The impact of Alzheimer’s disease on the functional connectivity between brain regions underlying pain perception. Eur J Pain 15:568
Dahlhamer J et al (2018) Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. MMWR Morb Mortal Wkly Rep 67:1001–1006
Dueñas M, Salazar A, Ojeda B et al (2015) A nationwide study of chronic pain prevalence in the general Spanish population: identifying clinical subgroups through cluster analysis. Pain Med 16:811–822
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Fayaz A, Croft P, Langford RM et al (2016) Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open 6(6):e010364
Feigin VL, Abajobir AA, Abate KH et al (2017) Global, regional, and national burden of neurological disorders during 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet Neurol 16:877–897
Frederick E (2016) Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Mil Med 181(5):397–399
George KM, Folsom AR, Sharrett AR et al (2020) Migraine headache and risk of dementia in the atherosclerosis risk in communities neurocognitive study. Headache 60(5):946–953
Gilmore-Bykovskyi AL, Block L, Hovanes M et al (2019) Analgesic use patterns among patients with dementia during transitions from hospitals to skilled nursing facilities. Res Gerontol Nurs 12:61–69
Gyoneva S, Traynelis SF (2013) Norepinephrine modulates the motility of resting and activated microglia via different adrenergic receptors. J Biol Chem 288:15291–15302. https://doi.org/10.1074/jbc.M113.458901
Hagen K, Stordal E, Linde M et al (2014) Headache as a risk factor for dementia: a prospective population-based study. Cephalalgia 34(5):327–335
Hayashida KI, Obata H (2019) Strategies to treat chronic pain and strengthen impaired descending noradrenergic inhibitory system. Int J Mol Sci 20:822. https://doi.org/10.3390/ijms20040822
Hellstrom Y, Persson G, Hallberg IR (2004) Quality of life and symptoms among older people living at home. J Adv Nurs 48:584–593
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Huang SW, Wang WT, Chou LC et al (2015) Osteoarthritis increases the risk of dementia: a nationwide cohort study in Taiwan. Sci Rep 18(5):10145
Hurh K, Jeong SH, Kim SH et al (2022) Increased risk of all-cause, Alzheimer’s, and vascular dementia in adults with migraine in Korea: a population-based cohort study. J Headache Pain 23(1):108
Innes KE, Sambamoorthi U (2020) The association of osteoarthritis and related pain burden to incident Alzheimer’s disease and related dementias: a retrospective cohort study of US medicare beneficiaries. J Alzheimers Dis 75(3):789–805
Innes KE, Sambamoorthi U (2020) The potential contribution of chronic pain and common chronic pain conditions to subsequent cognitive decline, new onset cognitive impairment, and incident dementia: a systematic review and conceptual model for future research. J Alzheimers Dis 78(3):1177–1195
International Association for the Study of Pain (1986) Classification of chronic pain: introduction. Pain 24:S3–S8. https://doi.org/10.1016/0304-3959(86)90107-7
Islamoska S, Hansen ÅM, Wang HX et al (2020) Mid- to late-life migraine diagnoses and risk of dementia: a national register-based follow-up study. J Headache Pain 21(1):98
Kao PH, Jang FL, Ho CH et al (2021) Chronic pain increases the risk of dementia: a nationwide population-based cohort study. Pain Phys 24(6):E849–E856 (PMID: 34554705)
Khalid S, Sambamoorthi U, Innes KE (2020) Non-cancer chronic pain conditions and risk for incident Alzheimer’s disease and related dementias in community-dwelling older adults: a population-based retrospective cohort study of United States medicare beneficiaries, 2001–2013. Int J Environ Res Public Health 17(15):5454
Khalid S, Sambamoorthi U, Umer A et al (2022) Increased odds of incident Alzheimer’s disease and related dementias in presence of common non-cancer chronic pain conditions in Appalachian older adults. J Aging Health 34(2):158–172
Kostov K, Bohlken J, Jacob L (2019) Association between migraine headaches and dementia in more than 7400 patients followed in general practices in the United Kingdom. J Alzheimers Dis 71(1):353–360
Lee SY, Lim JS, Oh DJ, Kong IG, Choi HG (2019) Increased risk of neurodegenerative dementia in women with migraines: a nested case-control study using a national sample cohort. Medicine 98(7):e14467
Leonard BE (2017) Major depression as a neuroprogressive prelude to dementia: what is the evidence? Mod T Rends Pharmacopsychiatr 31:56–66
Leveille SG et al (2009) Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA 302:2214–2221
Mačianskytė D, Janužis G, Kubilius R, Adomaitienė V, Ščiupokas A (2011) Associations between chronic pain and depressive symptoms in patients with trigeminal neuralgia. Medicina 47(7):386
Marchand F, Perretti M, McMahon SB (2005) Role of the immune system in chronic pain. Nat Rev Neurosci 6:521–532
McGeer PL, Rogers J, McGeer EG (2006) Inflammation, anti-inflammatory agents and Alzheimer disease: the last 12 years. J Alzheimer’s Dis 9(s3):271–276
Melek L, Devine M, Renton T (2018) The psychosocial impact of orofacial pain in trigeminal neuralgia patients: a systematic review. Int J Oral Maxillofac Surg 47:869–878
Monroe TB, Gore JC, Min Chen L et al (2012) Pain in people with Alzheimer disease: potential applications for psychophysical and neurophysiological research. J Geriatr Psychiatry Neurol 25:240–255
Monroe TB, Beach PA, Bruehl SP et al (2017) The impact of Alzheimer’s disease on resting state functional connectivity of brain regions modulating pain: a cross-sectional study. J Alzheimers Dis 57:71–83
Morton RE, St John PD, Tyas SL (2019) Migraine and the risk of all-cause dementia, Alzheimer’s disease, and vascular dementia: a prospective cohort study in community-dwelling older adults. Int J Geriatr Psychiatry 34(11):1667–1676
Noubiap JJ, Balti EV, Bigna JJ et al (2019) Dyslipidaemia in Africa-comment on a recent systematic review—authors’ reply. Lancet Glob Health 7(3):e308–e309
Ossipov MH, Porreca F (2006) Chronic pain: multiple manifestations, multiple mechanisms. Drug Discov Today Dis Mech 3:301–303. https://doi.org/10.1016/j.ddmec.2006.09.008
Paalani M, Lee JW, Haddad E, Tonstad S (2011) Determinants of inflammatory markers in a bi-ethnic population. Ethn Dis 21:142–149
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 29(372):n71. https://doi.org/10.1136/BMJ.n71.PMID:33782057;PMCID:PMC8005924
Patel KV, Guralnik JM, Dansie EJ, Turk DC (2013) Prevalence and impact of pain among older adults in the United States: findings from the 2011 national health and aging trends study. Pain 154(12):2649–2657
Pitcher MH, Von Korff M, Bushnell MC, Porter L (2019) Prevalence and profile of high-impact chronic pain in the United States. J Pain 20(2):146–160
Rouch I, Edjolo A, Laurent B et al (2022) Chronic pain, and long-term dementia risk in older adults: results from a 24-year longitudinal study. Int J Geriatr Psychiatry. https://doi.org/10.1002/gps.5713
Salter MW, Stevens B (2017) Microglia emerge as central players in brain disease. Nat Med 23:1018–1027. https://doi.org/10.1038/nm.4397
Sanders S, Morano C (2008) Alzheimer’s disease and related dementias. J Gerontol Soc Work 50(Suppl 1):191–214. https://doi.org/10.1080/01634370802137900. (PMID: 18924393)
Schain M, Kreisl WC (2017) Neuroinflammation in neurodegenerative disorders—a review. Curr Neurol Neurosci Rep 17:25
Smalbrugge M, Jongenelis LK, Pot AM et al (2007) Pain among nursing home patients in the Netherlands: prevalence, course, clinical correlates, recognition and analgesic treatment—an observational cohort study. BMC Geriatr 7:3
Stang A (2010) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Tsang A et al (2008) Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain 9:883–891
Turk D, Melzack R (2011) The measurement of pain and the assessment of people experiencing pain. In: Turk D, Melzack R (eds) Handbook of pain assessment, 3rd edn. Guilford Press, New York, p 542
Tzeng NS, Chung CH, Liu FC et al (2018) Fibromyalgia and risk of dementia-a nationwide, population-based. Cohort Study Am J Med Sci 355(2):153–161. https://doi.org/10.1016/j.amjms.2017.09.002. (Epub 2017 Sep 15 PMID: 29406043)
Van Eldik LJ, Carrillo MC, Cole PE et al (2016) The roles of inflammation and immune mechanisms in Alzheimer’s disease. Alzheimer’s & Dementia: Transl Res Clin Interv 2:99–109
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J (2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. The Lancet 380(9859):2163–2196
Wang K, Liu H (2021) Association between widespread pain and dementia, Alzheimer’s disease and stroke: a cohort study from the Framingham heart study. Reg Anesth Pain Med 46(10):879–885. https://doi.org/10.1136/rapm-2021-102733
Wang J, Monroe TB, Simning A, Conwell Y, Caprio TV, Cai X, Temkin-Greener H, Muench U, Yu F, Ge S, Li Y (2021) Pain management in home health care: relationship with dementia and facility admissions. Pain Manag Nurs 22(1):36–43
Wang J, Cheng Z, Kim Y, Yu F et al (2022) Pain, and the Alzheimer’s disease and related dementia spectrum in community-dwelling older Americans: a nationally representative study. J Pain Symptom Manag 63(5):654–664
Whitlock EL, Diaz-Ramirez LG, Glymour MM, Boscardin WJ, Covinsky KE, Smith AK (2017) Association between persistent pain and memory decline and dementia in a longitudinal cohort of elders. JAMA Intern Med 177(8):1146–1153
Whitlock EL, Diaz-Ramirez LG, Glymour MM et al (2017) Association between persistent pain and memory decline and dementia in a longitudinal cohort of elders. JAMA Intern Med 177(8):1146–1153
Acknowledgements
None.
Funding
This work was supported by the Sichuan Youth Science and Technology Innovation Research Team (no. 2021JDTD0007) and a grant support from Chengdu University of TCM for evidence based medicine research (no. XKTD2021004).
Author information
Authors and Affiliations
Contributions
Zhenzhi Wang and Zhen Sun developed the protocol, participated in the literature search, extracted data, and drafted the manuscript; Hui Zheng was critical revision of the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable. We declare that the research was conducted in the absence of any commercial or financial relationships.
Informed consent
Not applicable.
Competing interests
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Responsible Editor: Matthias Kliegel.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Z., Sun, Z. & Zheng, H. Association between chronic pain and dementia: a systematic review and meta-analysis. Eur J Ageing 21, 17 (2024). https://doi.org/10.1007/s10433-024-00812-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s10433-024-00812-2