Abstract
We evaluated the in vitro activity of ceftibuten-avibactam against Enterobacterales causing urinary tract infection (UTI). A total of 3216 isolates (1/patient) were consecutively collected from patients with UTI in 72 hospitals from 25 countries in 2021 then susceptibility tested by CLSI broth microdilution. Ceftibuten-susceptible breakpoints currently published by EUCAST (≤ 1 mg/L) and CLSI (≤ 8 mg/L) were applied to ceftibuten-avibactam for comparison. The most active agents were ceftibuten-avibactam (98.4%/99.6% inhibited at ≤ 1/ ≤ 8 mg/L), ceftazidime-avibactam (99.6% susceptible [S]), amikacin (99.1%S), and meropenem (98.2%S). Ceftibuten-avibactam (MIC50/90, 0.03/0.06 mg/L) was fourfold more potent than ceftazidime-avibactam (MIC50/90, 0.12/0.25 mg/L) based on MIC50/90 values. The most active oral agents were ceftibuten (89.3%S; 79.5% inhibited at ≤ 1 mg/L), levofloxacin (75.4%S), and trimethoprim-sulfamethoxazole (TMP-SMX; 73.4%S). Ceftibuten-avibactam inhibited 97.6% of isolates with an extended-spectrum β-lactamase phenotype, 92.1% of multidrug-resistant isolates, and 73.7% of carbapenem-resistant Enterobacterales (CRE) at ≤ 1 mg/L. The second most active oral agent against CRE was TMP-SMX (24.6%S). Ceftazidime-avibactam was active against 77.2% of CRE isolates. In conclusion, ceftibuten-avibactam was highly active against a large collection of contemporary Enterobacterales isolated from patients with UTI and exhibited a similar spectrum to ceftazidime-avibactam. Ceftibuten-avibactam may represent a valuable option for oral treatment of UTI caused by multidrug-resistant Enterobacterales.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infections (UTIs) are among the most common of all bacterial infections. Approximately 50% of all women experience at least 1 UTI by the age of 35, and approximately 20% of women between the ages of 18 and 24 have a UTI annually [1]. The majority of UTIs are treated on an outpatient basis. However, resistance to first-line oral antimicrobials that are used to treat UTIs has increased markedly in the last 2 decades, complicating outpatient treatment approaches [2]. In the USA, Escherichia coli resistant to trimethoprim-sulfamethoxazole (TMP-SMX) among adult females with UTI has exceeded 25%, and among females aged ≥ 65 years, ciprofloxacin resistance approaches 30% [3]. In parts of Europe, resistance to TMP-SMX and ciprofloxacin has also increased dramatically among E. coli [4]. Moreover, side effects of some first-line agents for treatment of UTI are of great concern [5, 6].
Other important mechanisms of resistance in UTI pathogens are the production of extended-spectrum β-lactamases (ESBLs) and, more recently, the production of carbapenemases. These resistance mechanisms are frequently associated with fluoroquinolone and/or aminoglycoside resistance determinants [7]. As the number of pathogens resistant to outpatient therapies has risen, the number of hospitalizations for UTIs has also grown [2].
Other oral agents used to treat UTI include fosfomycin and pivmecillinam, the oral version of mecillinam. Most clinical data available is on the effectiveness of fosfomycin to treatment and prevention of lower UTI, primarily cystitis [8]. Although fosfomycin remains very active against E. coli, including MDR and carbapenem-resistant isolates, it has more limited activity against Klebsiella spp. and other Enterobacterales responsible for UTI [9]. Mecillinam is also an old antibiotic that remains very active against E. coil even in regions where it is commonly used to treat UTI; however, a randomized clinical trial comparing this drug with standard of care regimes is warranted [10, 11].
Ceftibuten is an oral third-generation cephalosporin which is highly potent against Enterobacterales and stable against many class A and C β-lactamases produced by these organisms, including some ESBLs [12, 13]. Avibactam is a synthetic diazabicyclooctane (DBO) non-β-lactam inhibitor. Avibactam is available for clinical use in combination with ceftazidime as an IV formulation; an avibactam formulation for oral use is currently being developed to be combined with ceftibuten for clinical use. Compared with clavulanic acid, sulbactam, and tazobactam, avibactam provides excellent inhibition of most clinically relevant class A and class C β-lactamases, such as ESBLs, KPCs, and AmpC β-lactamases [14]. In the present study, we evaluated the in vitro activity of ceftibuten-avibactam (fixed 4 mg/L) against a contemporary collection of Enterobacterales collected from patients with UTIs worldwide.
Materials and methods
Participant medical centers were invited to collect a specific number (25 to 60, depending on geographic region) of consecutive isolates (1/patient) from patients with UTI in 2021. Only bacterial isolates determined to be significant by local criteria as the reported probable cause of infection were included in this investigation. The organism collection included 3216 isolates from 72 medical centers in 25 countries. Isolates were mainly from the US (n = 1585; 29 centers) and Europe (n = 1410; 33 centers in 18 countries), but also included E. coli isolates from Latin America (n = 121; 6 centers in 5 countries) and Japan (n = 100; 4 centers).
Antimicrobial susceptibility was evaluated by reference broth microdilution method in a monitoring laboratory (JMI Laboratories, North Liberty, Iowa, USA) and conducted according to Clinical and Laboratory Standards Institute (CLSI) procedures (document M07) [15]. Current ceftibuten breakpoints published by CLSI (≤ 8 mg/L) and EUCAST (≤ 1 mg/L) were applied to ceftibuten-avibactam for comparison [16, 17]. Avibactam was present at a fixed concentration of 4 mg/L in combination with ceftibuten.
E. coli, K. pneumoniae, and P. mirabilis isolates were categorized as exhibiting an ESBL phenotype based on CLSI criteria; i.e., the isolate had an elevated MIC value (≥ 2 mg/L) for ceftazidime, ceftriaxone, or aztreonam [16]. Isolates were considered multidrug resistant (MDR) according to criteria defined in 2012 by the joint European and US Centers for Disease Control, which defines MDR as nonsusceptible to ≥ 1 agent in ≥ 3 antimicrobial classes [18]. The following representative agents from each antimicrobial class and their CLSI interpretive criteria were: ceftazidime (≥ 8 mg/L), ceftriaxone (≥ 2 mg/L), cefepime (≥ 4 mg/L), meropenem (≥ 2 mg/L), imipenem (≥ 2 mg/L), piperacillin/tazobactam (≥ 16/4 mg/L), levofloxacin (≥ 1 mg/L), ciprofloxacin (≥ 0.5 mg/L), gentamicin (≥ 8 mg/L), amikacin (≥ 32 mg/L), tobramycin (≥ 8 mg/L), colistin (≥ 4 mg/L; resistant), and tigecycline (≥ 4 mg/L; US-FDA interpretive criteria). CRE were defined as Enterobacterales that displayed imipenem or meropenem MIC values at ≥ 4 mg/L. Imipenem MIC results were not applied to Proteus mirabilis or indole-positive Proteeae due to their intrinsically elevated MIC values.
Results
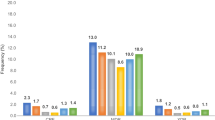
The frequencies of Enterobacterales isolated from patients with UTIs in the USA and Europe are presented in supplemental Figure S1. E. coli, Klebsiella pneumoniae, and Proteus mirabilis were the most common species and represented 77.3% and 81.3% of organisms from the USA and Europe, respectively. Ceftibuten-avibactam inhibited 98.4% and 99.6% of Enterobacterales isolates at ≤ 1 mg/L and ≤ 8 mg/L, respectively (MIC50/90, 0.03/0.06 mg/L; Tables 1 and 2). Ceftibuten-avibactam was the most active oral agent, exhibiting in vitro activity similar to the most active IV agents, such as ceftazidime-avibactam (MIC50/90, 0.12/0.25 mg/L; 99.6% susceptible per CLSI and EUCAST), amikacin (MIC50/90, 2/4 mg/L; 99.1%/97.8% susceptible per CLSI/EUCAST), and meropenem (MIC50/90, 0.03/0.06 mg/L; 98.2%/98.3% susceptible per CLSI/EUCAST; Table 2). Notably, ceftibuten-avibactam was fourfold more potent than ceftazidime-avibactam based on MIC50/90 values (Table 2).
The most active oral agents after ceftibuten-avibactam (MIC50/90, 0.03/0.06 mg/L; 98.4% inhibited at ≤ 1 mg/L) were ceftibuten (MIC50/90, 0.25/16 mg/L; 89.3%/79.5% susceptible per CLSI/EUCAST), levofloxacin (MIC50/90, 0.06/16 mg/L; 75.4% susceptible per CLSI and EUCAST), and trimethoprim-sulfamethoxazole (TMP-SMX; MIC50/90, ≤ 0.12/ > 4 mg/L; 73.4% susceptible per CLSI and EUCAST; Table 2).
Ceftibuten-avibactam retained potent activity and broad coverage against ESBL-phenotype (MIC50/90, 0.03/0.25 mg/L; 97.6%/98.3% inhibited at ≤ 1/ ≤ 8 mg/L), MDR (MIC50/90, 0.06/1 mg/L; 91.6%/95.3% inhibited at ≤ 1/ ≤ 8 mg/L), and CRE isolates (MIC50/90, 0.25/ > 16 mg/L; 73.7%/78.9% inhibited at ≤ 1/ ≤ 8 mg/L; Table 1); all other oral agents showed limited activity against these resistant subsets (Table 2). Moreover, ceftibuten-avibactam activity against CREs was similar to ceftazidime-avibactam (MIC50/90, 2/ > 32 mg/L; 77.2% susceptible per CLSI and EUCAST; Table 2). Ceftibuten-avibactam was also active against isolates non-susceptible to levofloxacin (MIC50/90, 0.03/0.12 mg/L; 97.8%/98.6% inhibited at ≤ 1/ ≤ 8 mg/L), nitrofurantoin (MIC50/90, 0.03/0.25 mg/L; 96.4%/99.0% inhibited at ≤ 1/ ≤ 8 mg/L), or TMP-SMX (MIC50/90, 0.03/0.12 mg/L; 98.0%/98.8% inhibited at ≤ 1/ ≤ 8 mg/L), which are oral agents commonly used to treat UTI (Table 1).
The 3 Enterobacterales species most frequently isolated from UTI, E. coli, K. pneumoniae, and P. mirabilis, were very susceptible to ceftibuten-avibactam, with 98.5% to 99.7% of isolates inhibited at ≤ 1 mg/L (Table 1). Indole-positive Proteeae were also highly susceptible to ceftibuten-avibactam (MIC50/90, ≤ 0.015/0.03 mg/L; 99.2% inhibited at ≤ 1 mg/L and ≤ 8 mg/L), while Enterobacter cloacae species complex isolates exhibited slightly higher ceftibuten-avibactam MIC values (MIC50/90, 0.12/4 mg/L; 73.8%/96.8% inhibited at ≤ 1/ ≤ 8 mg/L) than those other Enterobacterales species (Table 1).
Among isolates with ceftibuten-avibactam MICs > 2 mg/L (n = 28; 0.9%), susceptibility to meropenem and ceftazidime-avibactam was 42.9%/50.0% (CLSI/EUCAST) and 57.1% (CLSI and EUCAST), respectively; whereas among isolates with ceftibuten-avibactam MICs > 8 mg/L (n = 14; 0.4%), susceptibility to meropenem and ceftazidime-avibactam was 7.1%/14.3% (CLSI/EUCAST) and 14.3% (CLSI and EUCAST), respectively.
Discussion
Increasing antimicrobial resistance coupled with the lack of new oral antimicrobial agents for MDR organisms represents a major challenge for the treatment of complicated and uncomplicated UTI. Infections caused by ESBL-producing Enterobacterales or CRE usually require IV antimicrobial therapy with very limited options for oral step-down treatment [7, 19].
The results of the present study showed that ceftibuten-avibactam was very active against a large collection of Enterobacterales isolates causing UTI in various regions of the world. Moreover, ceftibuten-avibactam retained strong activity against isolates with an MDR and/or ESBL phenotype, as well as isolates nonsusceptible to levofloxacin, nitrofurantoin, and/or TMP-SMX. Ceftibuten-avibactam also retained activity against most CRE isolates, inhibiting 73.7% and 78.9% at ≤ 1 mg/L and ≤ 8 mg/L, respectively. Characterization of the isolates with increased ceftibuten-avibactam MIC values (≥ 2 mg/L) is ongoing. Once completed, these characterizations will provide a better understanding of the spectrum of activity for this antimicrobial combination.
The limitations of the study should be considered when interpreting the data. The absence of fosfomycin and pivmecillinam as comparator agents represents a limitation of this investigation since these oral agents are commonly used to treat UTI in some regions. Another limitation of the study is the lack of β-lactamase characterization of ESBL-phenotype and CRE isolates, as well as those with decreased susceptibility to ceftibuten-avibactam. Despite the limitations of the study, the results presented here provide valuable information on the in vitro activity of this novel agent against contemporary isolates from patients with UTI. In summary, these results indicate that ceftibuten-avibactam may represent a valuable addition for the treatment of UTI caused by MDR Enterobacterales. Further pharmacokinetic/pharmacodynamic and clinical studies are warranted to define the role of ceftibuten-avibactam for the treatment of UTI.
Data availability
The data evaluated in this investigation is part of the SENTRY Antimicrobial Surveillance Program; available at: https://sentry-mvp.jmilabs.com/app/sentry-public
References
Simmering J, Tang F, Cavanaugh J, Polgreen L, Polgreen P (2017) The increase in hospitalizations for urinary tract infections and the associated costs in the United States, 1998–2011. Open Forum Infect Dis 4(1):ofw281. https://doi.org/10.1093/ofid/ofw281
Zilberberg MD, Shorr AF (2013) Secular trends in gram-negative resistance among urinary tract infection hospitalizations in the United States, 2000–2009. Infect Control Hosp Epidemiol 34(9):940–946. https://doi.org/10.1086/671740
Sanchez GV, Babiker A, Master RN, Luu T, Mathur A, Bordon J (2016) Antibiotic resistance among urinary isolates from female outpatients in the United States in 2003 and 2012. Antimicrob Agents Chemother 60(5):2680–2683. https://doi.org/10.1128/AAC.02897-15
Kahlmeter G, Åhman J, Matuschek E (2015) Antimicrobial resistance of Escherichia coli causing uncomplicated urinary tract infections: a European update for 2014 and comparison with 2000 and 2008. Infect. Dis. Ther. 4:417–423. https://doi.org/10.1007/s40121-015-0095-5
US FDA (2016) FDA Drug Safety Communication: FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections; warns about disabling side effects that can occur together. July 26, 2016. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-advises-restricting-fluoroquinolone-antibiotic-use-certain. Accessed July 2022
American Geriatrics Society Beers Criteria Update Expert Panel (2019) American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc 67(4):674–694. https://doi.org/10.1111/jgs.15767
Faine B, Rech M, Vakkalanka P, Gross A, Brown C, Harding S, Slocum G, Zimmerman D, Zepeski A, Rewitzer S, Howington G, Campbell M, Dawson J, Treu C, Nelson L, Jones M, Flack T, Porter B, Sarangarm P, Mattson A, Bailey A, Kelly G, Talan D (2022) High prevalence of fluoroquinolone-resistant UTI among US emergency department patients diagnosed with urinary tract infection, 2018–2020. Acad Emerg Med. https://doi.org/10.1111/acem.14545
Falagas ME, Vouloumanou EK, Samonis G, Vardakas KZ (2016) Fosfomycin. Clin Microbiol Rev 29(2):321–347. https://doi.org/10.1128/CMR.00068-15
Candel F, David M, Lopez J (2019) New perspectives for reassessing fosfomycin: applicablity in current clinical practice. Rev Esp Quimioter 32:01–07
Frimodt-Moller N, Simonsen GS, Larsen AR, Kahlmeter G (2023) Pivmecillinam, the paradigm of an antibiotic with low resistance rates in Escherichia coli urine isolates despite high consumption. J Antimicrob Chemother 78:289–295. https://doi.org/10.1093/jac/dkac396
Jansaker F, Frimodt-Moller N, Benfield T, Knudson J (2018) Mecillinam for the treatment of acute pyelonephritis and bacteremia caused by Enterobacteriaceae: a literature review. Infect Drug Resist 11:761–771. https://doi.org/10.2147/IDR.S163280
Wiseman LR, Balfour JA (1994) Ceftibuten. A review of its antibacterial activity, pharmacokinetic properties and clinical efficacy. Drugs 47(5):784–808. https://doi.org/10.2165/00003495-199447050-00006
Perilli M, Segatore B, Franceschini N, Gizzi G, Mancinelli A, Caravelli B, Setacci D, del Tavio-Perez MM, Bianchi B, Amicosante G (2001) Ceftibuten stability to active-site serine and metallo-beta-lactamases. Int J Antimicrob Agents 17(1):45–50. https://doi.org/10.1016/s0924-8579(00)00319-8
Wong D, van Duin D (2017) Novel beta-lactamase inhibitors: unlocking their potential in therapy. Drugs 77(6):615–628. https://doi.org/10.1007/s40265-017-0725-1
CLSI (2018) M07Ed11 Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Clinical and Laboratory Standards Institute, Wayne, PA.
CLSI (2022) M100d32. Performance standards for antimicrobial susceptibility testing. Clinical and Laboratory Standards Institute, Wayne, PA
EUCAST (2022) v12.0 Breakpoint tables for interpretation of MICs and zone diameters. Version 12.0, January 2022. European Committee on Antimicrobial Susceptibility Testing, Växjö, Sweden
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson-Liljequist B, Paterson DL, Rice LB, Stelling J, Struelen MJ, Vatopoulos A, Weber JT, Monnet DL (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18(3):268–281. https://doi.org/10.1111/j.1469-0691.2011.03570.x
Suay-García B, Pérez-Gracia M (2019) Present and future of carbapenem-resistant Enterobacteriaceae (CRE) infections. Antibiotics (Basel) 8(3):122. https://doi.org/10.3390/antibiotics8030122
Acknowledgements
The authors thank all participants of the SENTRY Antimicrobial Surveillance Program for their work in providing isolates. Editorial support was provided by Amy Chen at JMI Laboratories and was funded by Pfizer.
Funding
This study was supported by Pfizer Inc. Helio S. Sader, Cecilia G. Carvalhaes, Michael D. Huband, Rodrigo E. Mendes, and Mariana Castanheira are employees of JMI Laboratories, which was a paid consultant to Pfizer in connection with the development of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: HS, MC; data curation: HS, CC, MH, RM; funding acquisition: HS, MC; formal analysis: HS, CC, MH, RM; investigation: MH, RM; methodology: CC, MH, RM; project administration: CC; resources: MC; software: CC, RM; supervision: RM, MC; validation: CC, MC; visualization: HS, RM, MC; writing—original draft preparation: HS; writing—review and editing: RM, MC. All authors have read and agreed to the content of the manuscript.
Corresponding author
Ethics declarations
JMI Laboratories was contracted to perform services in 2018–2021 for AbbVie, Achaogen, Inc., Affinity Biosensors, Albany College of Pharmacy and Health Sciences, Allecra Therapeutics, Allergan, Amicrobe Advanced Biomaterials, Inc., American Proficiency Institute, AmpliPhi Biosciences Corp., Amplyx Pharma, Antabio, Arietis Corp., Arixa Pharmaceuticals, Inc., Artugen Therapeutics USA, Inc., Astellas Pharma Inc., Athelas, Becton, Basilea Pharmaceutica Ltd., Bayer AG, Becton, Beth Israel Deaconess Medical Center, BIDMC, bioMerieux, Inc., bioMerieux SA, BioVersys Ag, Boston Pharmaceuticals, Bugworks Research Inc., CEM-102 Pharmaceuticals, Cepheid, Cidara Therapeutics, Inc., Cipla, Contrafect, Cormedix Inc., Crestone, Inc., Curza, CXC7, DePuy Synthes, Destiny Pharma, Dickinson and Company, Discuva Ltd., Dr. Falk Pharma GmbH, Emery Pharma, Entasis Therapeutics, Eurofarma Laboratorios SA, Fedora Pharmaceutical, F. Hoffmann-La Roche Ltd., Fimbrion Therapeutics, US Food and Drug Administration, Fox Chase Chemical Diversity Center, Inc., Gateway Pharmaceutical LLC, GenePOC Inc., Geom Therapeutics, Inc., GlaxoSmithKline plc, Guardian Therapeutics, Hardy Diagnostics, Harvard University, Helperby, HiMedia Laboratories, ICON plc, Idorsia Pharmaceuticals Ltd., IHMA, Iterum Therapeutics plc, Janssen Research & Development, Johnson & Johnson, Kaleido Biosciences, KBP Biosciences, Laboratory Specialists, Inc., Luminex, Matrivax, Mayo Clinic, Medpace, Meiji Seika Pharma Co., Ltd., Melinta Therapeutics, Inc., Menarini, Merck & Co., Inc., Meridian Bioscience Inc., Micromyx, Microchem Laboratory, MicuRx Pharmaceutics, Inc., Mutabilis Co., N8 Medical, Nabriva Therapeutics plc, National Institutes of Health, NAEJA-RGM, National University of Singapore, North Bristol NHS Trust, Novartis AG, Novome Biotechnologies, Oxoid Ltd., Paratek Pharmaceuticals, Inc., Pharmaceutical Product Development, LLC, Polyphor Ltd., Prokaryotics Inc., QPEX Biopharma, Inc., Ra Pharmaceuticals, Inc., Rhode Island Hospital, RIHML, Roche, Roivant Sciences, Ltd., Safeguard Biosystems, Salvat, Scynexis, Inc., SeLux Diagnostics, Inc., Shionogi and Co., Ltd., SinSa Labs, Specific Diagnostics, Spero Therapeutics, Summit Pharmaceuticals International Corp., SuperTrans Medical LT, Synlogic, T2 Biosystems, Taisho Pharmaceutical Co., Ltd., TenNor Therapeutics Ltd., Tetraphase Pharmaceuticals, The Medicines Company, The University of Queensland, Theravance Biopharma, Thermo Fisher Scientific, Tufts Medical Center, Universite de Sherbrooke, University of Colorado, University of Southern California-San Diego, University of Iowa, University of Iowa Hospitals and Clinics, University of North Texas Health Science Center, University of Wisconsin, UNT System College of Pharmacy, URMC, UT Southwestern, VenatoRx, Viosera Therapeutics, Vyome Therapeutics Inc., Wayne State University, Wockhardt, Yukon Pharmaceuticals, Inc., Zai Lab, and Zavante Therapeutics, Inc. There are no speakers’ bureaus or stock options to declare.
Ethical approval
Not required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sader, H.S., Carvalhaes, C.G., Huband, M.D. et al. Antimicrobial activity of ceftibuten-avibactam against a global collection of Enterobacterales from patients with urinary tract infections (2021). Eur J Clin Microbiol Infect Dis 42, 453–459 (2023). https://doi.org/10.1007/s10096-023-04562-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-023-04562-4