Abstract
Post-sepsis psychiatric disorder, encompassing anxiety, depression, post-traumatic stress disorder and delirium, is a highly prevalent complication secondary to sepsis, resulting in a marked increase in long-term mortality among affected patients. Regrettably, psychiatric impairment associated with sepsis is frequently disregarded by clinicians. This review aims to summarize recent advancements in the understanding of the pathophysiology, prevention, and treatment of post-sepsis mental disorder, including coronavirus disease 2019-related psychiatric impairment. The pathophysiology of post-sepsis psychiatric disorder is complex and is known to involve blood–brain barrier disruption, overactivation of the hypothalamic–pituitary–adrenal axis, neuroinflammation, oxidative stress, neurotransmitter dysfunction, programmed cell death, and impaired neuroplasticity. No unified diagnostic criteria for this disorder are currently available; however, screening scales are often applied in its assessment. Modifiable risk factors for psychiatric impairment post-sepsis include the number of experienced traumatic memories, the length of ICU stay, level of albumin, the use of vasopressors or inotropes, daily activity function after sepsis, and the cumulative dose of dobutamine. To contribute to the prevention of post-sepsis psychiatric disorder, it may be beneficial to implement targeted interventions for these modifiable risk factors. Specific therapies for this condition remain scarce. Nevertheless, non-pharmacological approaches, such as comprehensive nursing care, may provide a promising avenue for treating psychiatric disorder following sepsis. In addition, although several therapeutic drugs have shown preliminary efficacy in animal models, further confirmation of their potential is required through follow-up clinical studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is a major threat to human health worldwide. In 2017, there were an estimated 48.9 million cases of sepsis globally, resulting in approximately 11 million deaths, representing 19.7% of the total [1]. As knowledge of the pathogenesis of this condition has increased, treatments have become more effective, resulting in a steady decrease in sepsis-related in-hospital mortality over time [2]. However, many sepsis survivors experience cognitive, psychiatric, and physical impairment, collectively known as post-sepsis syndrome, which has emerged as a key area of concern [3]. The consequences of sepsis are long-lasting, and, although often overlooked, can lead to substantial morbidity and mortality [4]. By actively exploring the pathogenesis and strategies for the prevention of post-sepsis syndrome, the incidence of these disorders can be effectively decreased, and the health status and quality of life of sepsis survivors can be improved.
Typically, the psychiatric disorder of sepsis survivors manifests as depression, anxiety, and post-traumatic stress disorder (PTSD), all of which can have a profound influence on their daily life as well as their ability to return to work following recovery [5, 6]. Additionally, delirium is also a neuropsychiatric symptom that can occur after sepsis. It manifests in a complex form, characterized by cognitive deficits, attention deficits, circadian dysrhythmia, emotional dysregulation, and alteration in psychomotor function [7]. Over the last decade, many studies have focused on investigating cognitive dysfunction and functional disability following sepsis [8]. In comparison, relatively few studies have concentrated on the psychiatric impairment that can arise secondary to sepsis. Hence, the aim of this study was to systematically review current knowledge regarding the pathogenesis, prevention, and treatment of post-sepsis psychiatric disorder, including depression, anxiety, PTSD and delirium.
Epidemiology
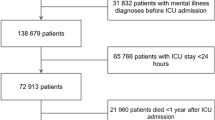
A study from Germany reported that sepsis survivors experience a high prevalence of psychiatric disorder in the first three years after discharge, with rates of 43.7%, 47.8%, and 48.5% in the first, second, and third years, respectively. The new onset of psychological impairment in the same period was respectively 17.9%, 12.8%, and 12.2% [9]. Delirium is a frequently observed complication in ICU patients with sepsis, with an incidence ranging from 17.7% to 48% [10, 11]. A retrospective cohort study revealed that patients with sepsis-associated delirium (SAD) had a higher mortality rate at 28 days and longer ICU stays compared to patients without SAD [12]. Moreover, individuals with SAD had a prolonged duration of mechanical ventilation and a significantly higher likelihood of needing professional care post-discharge [10]. Depression, anxiety, and PTSD often occur simultaneously, impacting overall health-related quality of life (HRQOL) [13]. One study reported incidences of anxiety, depression, and PTSD of respectively 67%, 49%, and 46% among sepsis survivors 24 h after discharge from the ICU. In comparison, patients who are re-evaluated one year after ICU discharge show incidence rates of respectively 38%, 50%, and 31%. The incidence of anxiety and PTSD decreases over time, whereas that of depression exhibits a significant increase [14]. The presence of persistent depressive symptoms has been found to strongly correlate with increased long-term mortality. This is supported by a large cohort study conducted in the UK, in which it was found that depressive symptoms are associated with an increased risk of mortality two years after discharge from the ICU [13]. A different study revealed that patients with post-sepsis depression had a five-year all-cause mortality rate of 46.2%, which was 1.29-fold higher than that of control patients. The same study also found that post-sepsis depression is independently linked to a higher five-year all-cause mortality among sepsis survivors [15]. To better understand the progression of depression following sepsis, Boede et al. identified three distinct trajectories of depressive symptoms one year after ICU discharge, namely, mild recovery, severe persistence, and severe recovery. Surprisingly, over one-third of patients did not recover from depression. Furthermore, the severity and duration of depression were found to be linked with chronic pain, PTSD, and a decrease in HRQOL [16]. These observations highlight the need to decrease the prevalence of post-sepsis psychiatric disorder among affected patients and enhance their quality of life.
Pathophysiology
Blood–brain barrier
The blood–brain barrier (BBB) is responsible for regulating the entry of nutrients and immune cells into the brain, while also excluding toxic substances. This crucial function helps maintain the homeostasis of the central nervous system [17]. The BBB is mainly composed of specialized endothelial cells, glycocalyx, and a basement membrane that includes pericytes and astrocyte end-feet [18]. Cerebrovascular endothelial cells are the key components of the BBB and are responsible for regulating the permeability of the BBB through tight junctions [17]. There is evidence supporting that the disruption of BBB structure may be associated with psychiatric disorder following sepsis. One study found that mice display anxiety and depression-like behaviors one day after cecal ligation and puncture (CLP) surgery, which mimics human sepsis, accompanied by a marked aggregation of endothelial cell nuclear chromatin at the edge of the nuclear membrane. Additionally, a significant increase in the permeability of the BBB to Evans blue was observed in the mouse brain, indicative of BBB disruption [19]. However, the exact cause of this effect is not clear but may involve astrocyte activation. Studies have demonstrated that astrocytes are activated during sepsis and release inflammatory mediators, such as interleukin-1 beta (IL-1β) and IL-6, which then disrupt the integrity of the BBB during the early phase post-CLP, thereby further promoting psychiatric impairment [20, 21].
Neuroinflammation
Systemic inflammation during sepsis leads to the production of proinflammatory cytokines. Peripheral proinflammatory cytokines, such as IL-1β and tumor necrosis factor-alpha (TNF-α), can enter the brain parenchyma by binding to receptors on brain endothelial cells, and subsequently activate glial cells and induce neuroinflammation, resulting in a vicious circle [22,23,24]. Evidence suggests that there may be a correlation between neuroinflammation and psychiatric symptoms following sepsis. Indeed, mice display anxiety-like behavior 10 days after CLP, along with increased levels of TNF-α, interferon-gamma (IFN-γ), IL-1β, and IL-6 in brain tissue [25]. Additionally, the inhibition of the nuclear factor-kappa B (NF-κB) pathway can reduce microglial activation, thereby alleviating psychiatric symptoms in septic mice [26]. Nevertheless, the precise mechanism underlying how neuroinflammation leads to post-sepsis psychiatric disorder is incompletely understood. We have previously found that the activation of the NOD-like receptor pyrin domain-containing protein 3 (NLRP3) inflammasome induces a notable rise in the levels of IL-1β, IL-18, and TNF-α in the hippocampus of septic mice and promotes the activation of microglia [27], which can then further activate the NLRP3 inflammasome [28]. Activated microglia also promote the production and release of a significant number of inflammatory mediators, which facilitate the expression of indoleamine 2,3-dioxygenase (IDO), a key enzyme in endotoxin-induced depression [29]. Heightened IDO activity not only results in tryptophan depletion but also triggers the production of neurotoxic products such as 3-hydroxytryptophan and quinolinic acid, which jointly contribute to the development of depression [30].
Oxidative stress
Oxidative stress and neuroinflammation are interrelated and can exacerbate each other. Oxidative stress occurs when there is an overproduction of reactive oxygen species (ROS) and an inadequate capacity for scavenging these molecules through the antioxidant system [31]. Studies have confirmed that neuroinflammation triggers the release of proinflammatory mediators, which subsequently activate microglia and promote the production of ROS, ultimately leading to neuronal damage. Oxidative stress also contributes to the propagation of inflammatory signaling pathways [32]. Emerging evidence supports that oxidative stress plays a role in the development of psychiatric disorder following sepsis. For instance, mice exhibit anxiety- and depression-like behaviors one month after intraperitoneal injection of lipopolysaccharide (LPS), concomitant with an increase in the expression of the inducible nitric oxide synthase (iNos) gene and oxidative stress markers in the hippocampus and prefrontal cortex [33]. Similarly, rats display marked anxiolytic behavior following CLP, accompanied by an increase in malondialdehyde content and a significant decrease in superoxide dismutase activity [34]. The mechanisms involved in how oxidative stress contributes to post-sepsis psychiatric disorder are not clear. Nevertheless, as oxidative stress is closely related to neuroinflammation, it is likely that a close relationship exists between oxidative stress and neuroinflammation in the occurrence of post-sepsis psychiatric disorder.
Programmed cell death
Programmed cell death (PCD) comprises apoptosis, cuproptosis, pyroptosis, autophagy, necroptosis, and ferroptosis [35]. An increasing number of studies have suggested that PCD is involved in the occurrence of psychiatric impairment secondary to sepsis. Mice exhibit depressive behavior 14 days after CLP, which is accompanied by increased neuronal apoptosis and necroptosis in the hippocampus [36]. Additionally, the expression of myelocyte differentiation factor 2 (MD2), an intermediary regulator of apoptosis and necroptosis [37], is significantly increased in hippocampal neurons 24 h after CLP. Compared with wild-type mice, transgenic mice exhibiting excitatory neuron-specific MD2 knockout display less depression-like behavior two weeks following CLP, along with a reduction in the expression of apoptosis- and necroptosis-related proteins, as well as fewer dead neurons in the hippocampus. These findings indicate that MD2-mediated apoptosis and necroptosis are associated with the onset of post-sepsis depression [36]. Another study reported that mice show obvious anxiety- and depression-like behaviors on days 1 and 7 post-CLP concurrently with an increase in the levels of pyroptosis-related proteins in the cerebral cortex. However, this increase is blocked following the administration of a caspase-1 inhibitor, ultimately leading to an improvement in anxiolytic and depressive behaviors in the animals [19]. These findings implicate pyroptosis in the onset of psychiatric symptoms after sepsis.
Neuroplasticity
There is evidence to suggest that impaired neuroplasticity, a process involving neurogenesis, axon sprouting, axon regeneration, and synaptic plasticity [38], is linked to the occurrence of psychiatric disorder following sepsis. Mice display anxiety- and depression-like behaviors one month after LPS injection, along with a notable decrease in the expression of activity-regulated cytoskeletal-associated protein (ARC) and early growth response 1 (EGR1), synaptic plasticity-related early gene products. There is also a marked reduction in neural stem cell proliferation in the subgranular zone of the dentate gyrus in these animals [26]. The reduction in the expression of synaptic proteins and the elimination of synapses is indicative of impaired synaptic plasticity. One study revealed that mice exhibiting noticeable signs of psychiatric disorder after CLP also display a decrease in the expression levels of the presynaptic protein synapsin 1 and the postsynaptic proteins N-methyl-D-aspartate receptor subunit 2B (NR2B) and postsynaptic density protein 95 (PSD-95) in the hippocampus and cortex. However, treatment with a caspase-1 inhibitor recovered the levels of above-mentioned proteins [19]. The C1q complement pathway is thought to mediate synaptic elimination. A recent study demonstrated that translocator protein (Tspo)-knockout mice display more severe psychiatric symptoms 17 days after CLP, together with an upregulation of C1q complement pathway-related genes in the hippocampus [39]. These observations indicate that post-sepsis psychiatric disorder is associated with synaptic elimination mediated by the C1q complement pathway. Brain-derived neurotrophic factor (BDNF) and its related signaling pathways have been confirmed to play a crucial role in neuroplasticity. Rats exhibit evident depressive behavior 10 days post CLP, concomitant with a reduction in BDNF levels in the hippocampus [40], indirectly suggesting that neuroplasticity is associated with psychiatric impairment secondary to sepsis.
The hypothalamic–pituitary–adrenal axis
The hypothalamic–pituitary–adrenal (HPA) axis is an important component of the neuroendocrine system. Under conditions of stress, neurons in the hypothalamic paraventricular nucleus (PVN) synthesize and release corticotropin-releasing hormone (CRH), which then binds to CRH1 and CRH2 receptors in the anterior pituitary, thus inducing the release of adrenocorticotropic hormone (ACTH) into the bloodstream. ACTH promotes the secretion of glucocorticoid (GC) from the adrenal gland. GC, in turn, binds to the glucocorticoid receptor (GR) in the hippocampus, PVN, and anterior pituitary, thus creating a negative feedback loop that inhibits the release of CRH and contributes to the maintenance of body homeostasis [41]. Studies have shown that overactivation of the HPA axis is associated with systemic inflammation-induced anxiety and depression [42, 43], suggesting that it may also be involved in post-sepsis psychiatric disorder. In addition to depression-like behavior, sepsis survivor rats exhibit increased adrenal weight and corticosterone and ACTH contents [40], suggesting that activation of the HPA axis is involved in the onset of depression after sepsis. A subsequent study showed that the heightened reactivity of the HPA axis may be attributed to the dysfunction of the ventral hippocampus [44].
Neurotransmitters
Neurotransmitter abnormalities are closely related to the occurrence of neuropsychiatric disorders. Neurotransmitters such as gamma amino butyric acid (GABA), dopamine, norepinephrine, glutamate, and acetylcholine have been reported to be abnormally expressed during sepsis [45], suggesting that they may be involved in post-sepsis psychiatric disorder. One study noted that the anxiety-like behavior seen in rats after CLP was correlated with the activation of the IL-1β/GABA type A receptor (GABAAR) pathway in the hippocampus [34]. Meanwhile, a different study found that post-sepsis anxiety is associated with a decrease in the expression of 5-hydroxytryptamine 1A receptor (5-HT1AR) and an increase in that of 5-HT2AR [46]. Glutamate is an excitatory neurotransmitter. Enhanced intracellular system xc− activity leads to the release of glutamate from activated microglia, which contributes to the depression-like behavior seen in septic mice after the intraperitoneal injection of LPS. Interestingly, the use of the glutamate receptor antagonists MK801 and DNQX alleviated these depressive symptoms [47], indicating that a link may exist between glutamate and the occurrence of depression following sepsis. During neuroinflammation, IDO converts tryptophan, the precursor of serotonin, into quinolinic acid, which can bind to the N-methyl-D-aspartate (NMDA) receptor and exert excitatory neurotoxic effects [48]. It has been observed that the heightened expression of IDO in the hippocampus and prefrontal cortex is related to psychiatric symptoms following LPS injection [33]. In summary, the disruption of the neurotransmitter system promotes the occurrence of psychiatric disorder following sepsis.
Diagnosis
Given the lack of uniform diagnostic criteria for psychiatric disorder after sepsis, screening scales are frequently used to assess the occurrence of anxiety, depression, delirium and PTSD in sepsis survivors. The Beck Anxiety Inventory (BAI) and the Self-rating Anxiety Scale (SAS) are commonly utilized for the self-assessment of anxiety, while the Major Depression Inventory (MDI), Beck Depression Inventory-II (BDI-II), Self-rating Depression Scale (SDS), and Patient Health Questionnaire-9 (PHQ-9) are widely employed for the self-assessment of depression. In hospital settings, the Hospital Anxiety and Depression Scale (HADS) is often used for the screening of patients for anxiety and depression. The Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) and the Intensive Care Delirium Screening Checklist (ICDSC) are widely used assessment tools for detecting delirium in intensive care unit patients. Self-assessment tools such as the PTSD checklist for DSM-5 (PCL-5), Posttraumatic Symptom Scale-10 (PTSS-10), and Impact of Events Scale-Revised (IES-R) are normally used to evaluate the symptoms of PTSD. However, for a formal diagnosis, professionals rely on the more complex and comprehensive structured interview Clinician-administered PTSD Scale for DSM-5 (CAPS-5), which is considered the gold standard in PTSD diagnosis. A detailed summary of these scales is provided in Table 1. In 2019, the Society of Critical Care Medicine (SCCM) of the United States issued a consensus statement regarding the prediction and identification of post-intensive care syndrome [49]. In this statement, HADS was highly recommended for assessing anxiety and depression, with a score of 8 or higher indicating significant anxiety or depression. For assessing PTSD, IES-R and IES-6 were weakly recommended, with respective optimal cut-off values of 1.6 and 1.75. These suggestions could also serve as a reference for identifying post-sepsis psychiatric disorder.
Prevention
Psychiatric disorder following sepsis significantly impacts the daily life and long-term prognosis of sepsis survivors. Thus, implementing targeted preventive measures to reduce the incidence of related psychiatric disorder is of great clinical significance. According to the consensus statement issued by the SCCM, individuals who experience anxiety, depression, and PTSD before the onset of severe illness; acquire fear memories in the ICU; and lack social support during their illness are at a higher risk for long-term psychiatric impairment after critical illness. Accordingly, it is recommended that these patients undergo early screening and evaluation for psychiatric problems after discharge, as well as following important changes in health or life status [49].
The precipitating factors for post-sepsis psychiatric disorder may be multifactorial. In a prospective cohort study involving 135 patients with abdominal sepsis, 28% of participants reported moderate PTSD symptom scores while 10% reported high PTSD symptom scores one year after laparotomy. Correlations were observed between the occurrence of PTSD and factors such as age, length of stay in the ICU, and traumatic memories during hospitalization. After multivariate adjustment, the acquisition of more than four traumatic memories during hospitalization and longer stay in the ICU were determined to be independent risk factors for PTSD [67]. A prospective cohort study conducted on 439 elderly survivors of severe sepsis reported that 28% of patients experienced depressive symptoms following sepsis. Interestingly, clinical characteristics such as organ dysfunction score, length of hospital stay, and mechanical ventilation were not found to be associated with subsequent depression. However, suffering from depression before sepsis and functional impairment after sepsis were identified as independent risk factors for post-sepsis depression [73]. In another single-center study involving 33 patients with severe sepsis or septic shock, a positive association was identified between serum S100β levels and the incidence of PTSD. The cumulative dose of dobutamine during ICU stay was also positively correlated with the development of depression [14]. According to a study conducted in Korea, several risk factors for SAD were identified. These include older age (≥ 65), dependency in activities, high care needs, low awareness, shortness of breath, and thrombocytopenia. On the other hand, high level of albumin and the use of vasopressors or inotropes were found to potentially reduce the risk of SAD. Moreover, the risk of delirium was observed to increase with the severity of organ dysfunction [10]. The studies presented above suggest that there are several modifiable risk factors for psychiatric impairment after sepsis, including the number of traumatic memories, length of stay in the ICU, level of albumin, the use of vasopressors or inotropes, daily activity function after sepsis, and the cumulative dose of dobutamine. Primary care management includes evidence-based, post-sepsis care training for patients and their primary caregivers, case management by trained nurses, and clinical decision support provided by consulting physicians. It has been observed that, compared with usual care, primary care management can effectively reduce the incidence of PTSD among sepsis survivors one year after intervention [74]. Furthermore, in a prospective multicenter cohort study involving patients with sepsis, it was found that complete performance of the ABCDEF (Assess, prevent, and manage pain; Both spontaneous awakening and breathing trials; Choice of Analgesia and Sedation; Delirium assess, prevent, and manage; Early Mobility and Exercise; Family engagement/empowerment) bundle was associated with a reduced likelihood of delirium [75].
In summary, interventions targeting these modifiable risk factors, coupled with primary care management and the ABCDEF bundle, potentially serve as an effective strategy for the prevention of post-sepsis psychiatric disorder. However, there is still a lack of relevant research on prevention, which necessitates the further implementation of high-quality studies.
Treatment
No established treatment for post-sepsis psychiatric disorder is currently available. Research in this area is still in its infancy. Potential effective treatment options include both pharmacological and non-pharmacological therapies.
Non-pharmacological therapy
Internet-based cognitive behavioral therapy (ICBT) is a web-based writing intervention that is accessible and spatially independent. The treatment encompasses three aspects, namely, resource-oriented biographical reconstruction, in sensu trauma exposure, and cognitive reconstruction. After each writing session, a professional psychotherapist provides timely feedback. However, the therapeutic value of ICBT is inconclusive. For instance, in one case report, ICBT ameliorated PTSD symptoms in a sepsis survivor and his spouse [69], whereas in a different study, this intervention was reported to be ineffective at treating PTSD symptoms after severe sepsis. However, the small sample size in the latter study may have contributed to the negative result [63]. More studies with larger sample sizes are required to determine the efficacy of ICBT. Comprehensive nursing care is a widely utilized approach in the clinical care of surgical patients and individuals with chronic diseases. To ensure high-quality nursing care, all aspects of nursing work should be comprehensively carried out following established nursing procedures. Comprehensive nursing care is effective at reducing the levels of anxiety and depression in sepsis patients, leading to improved prognosis and quality of life [53]. In addition, it has demonstrated that early physical and occupational therapy can effectively decrease the duration of delirium in critically ill patients who require mechanical ventilation, including those with sepsis [76].
Pharmacological therapy
CLP and intraperitoneal injection of LPS are the most commonly used strategies for generating animal models of sepsis for the investigation of psychiatric disorder secondary to sepsis. Several drugs, such as imipramine, dexamethasone, guanosine, and nicotine, are effective therapies in animal models. These drugs exert their effects through a variety of mechanisms, including improving the neuroinflammatory response, reducing oxidative stress, inhibiting HPA axis activation, and decreasing BBB permeability (see Table 2 for details). Recent years have seen rapid development in cell therapy, particularly in the use of mesenchymal stem cells, with studies having shown that these cells possess anti-inflammatory and neuroprotective properties [77]. Mesenchymal stem cells and their conditioned medium can alleviate anxiety-like behavior in rats following CLP, effects that are achieved through the alleviation of the inflammatory response and astrocyte activation [20, 46]. These preliminary findings provide promising prospects for the management of psychiatric conditions following sepsis.
COVID-19 related psychiatric disorder
Psychiatric disorder can occur during both the acute phase and recovery period following a coronavirus disease 2019 (COVID-19) infection. This disorder includes anxiety, depression, PTSD, mania, delirium, and insomnia [84]. The main mechanism is direct neuroinvasion and neuroinflammation [85]. Unlike common sepsis, the development of COVID-19-related psychiatric impairment is influenced by pandemic-related stress and social isolation [84]. Managing and preventing COVID-19-related psychiatric disorder have become more challenging in the pandemic context. It has been demonstrated that supplementing with omega-3 can effectively decrease the likelihood of experiencing psychiatric consequence, such as depression, anxiety, and insomnia, after contracting COVID-19 [86]. In addition, Strict social isolation measures further hinder the implementation of the ABCDEF bundle, which makes it more difficult to control delirium [87]. Similarly, non-drug therapy is the primary approach to treating COVID-19-related psychiatric impairment at the moment. For example, narrative exposure therapy (NET) has been found to significantly ameliorate PTSD symptom after discharge [88]. Additionally, computerized cognitive behavioral therapy (cCBT) and progressive muscle relaxation training can greatly improve depression, anxiety, and sleep quality in COVID-19 patients [89, 90]. Furthermore, effective screening, early identification, and appropriate treatment are practical measures for managing delirium [91].
Conclusion
Psychiatric disorder secondary to sepsis has a significant impact on the quality of life of sepsis survivors. The pathogenesis of this condition includes BBB disruption, neuroinflammation, oxidative stress, PCD, impaired neuroplasticity, neurotransmitter dysfunction, and overactivation of the HPA axis (Fig. 1). The incidence of post-sepsis psychiatric disorder may be reduced by avoiding related risk factors. Currently, there is a dearth of effective treatments for psychiatric disorder following sepsis, and additional basic research is needed to identify potential therapeutic drugs targeting the underlying pathophysiology of the condition. Furthermore, non-pharmacological therapy should be considered as a viable treatment option in clinical practice. Additional research is required on the mechanism, prevention, and treatment of psychiatric impairment that arises after sepsis.
Overview of the pathophysiology of post-sepsis psychiatric disorder. During sepsis, the HPA axis becomes activated, resulting in increased release of glucocorticoids. Peripheral proinflammatory cytokines (TNF-α, IL-1β, and IL-6) enter the brain and induce neuroinflammation. Additionally, microglia and astrocyte activation leads to the release of proinflammatory cytokines, which disrupt the BBB. NLRP3 inflammasome activation promotes pyroptosis, and the increased production of IDO, ROS, and MD2 collectively leads to neuronal damage. Moreover, abnormal expression of plasticity-related proteins and genes results in impaired neuroplasticity. The dysfunction of the neurotransmitter system is a consequence of the atypical expression of neurotransmitters and their receptors
Data availability
All data analysed are included in this article.
Abbreviations
- CMI :
-
3-[(4-Chlorophenyl)selany1]-1-methyl-1H-indole
- Tat-CIRP :
-
Tat–cold-inducible RNA binding protein
- IgG :
-
Immunoglobulin G
- IgGAM :
-
Immunoglobulins enriched with IgA and IgM
- IgM :
-
Immunoglobulin M
- IgA :
-
Immunoglobulin A
- ip :
-
Intraperitoneal
- iv :
-
Intravenous
- BBB :
-
Blood–brain barrier
- CLP :
-
Cecal ligation and puncture
- NLRP3 :
-
NOD-like receptor pyrin domain-containing protein 3
- NF-κB :
-
Nuclear factor-kappa B
- EGR1 :
-
Early growth response 1
- LPS :
-
Lipopolysaccharide
- MD2 :
-
Myelocyte differentiation factor 2
- IL-1β :
-
Interleukin-1beta
- ACTH :
-
Adrenocorticotropic hormone
- BDNF :
-
Brain-derived neurotrophic factor
- HPA :
-
Hypothalamic–pituitary–adrenal
- 5-HT :
-
5-Hydroxytryptamine
- TNF-alpha :
-
Tumor necrosis factor-α
- IFN-γ :
-
Interferon-gamma
- PVN :
-
Paraventricular nucleus
- CRH :
-
Corticotropin-releasing hormone
- ROS :
-
Reactive oxygen species
- iNos :
-
Inducible nitric oxide synthase
- PCD :
-
Programmed cell death
- NMDA :
-
N-methyl-D-aspartate
- Tspo :
-
Translocator protein
- GR :
-
Glucocorticoid receptor
- IDO :
-
Indoleamine 2,3-dioxygenase
- 5-HT2AR :
-
5-Hydroxytryptamine 2A receptor
- 5-HT1AR :
-
5-Hydroxytryptamine 1A receptor
- GABAAR :
-
Gamma amino butyric acid type A receptor
- NR2B :
-
N-methyl-D-aspartate receptor subunit 2B
- PSD-95 :
-
Postsynaptic density protein 95
- EGR1 :
-
Early growth response 1
- ARC :
-
Activity-regulated cytoskeletal-associated protein
- BAI :
-
Beck Anxiety Inventory
- SAS :
-
Self-Rating Anxiety Scale
- HADS-A :
-
Hospital Anxiety and Depression Scale-Anxiety
- MDI :
-
Major depression inventory
- BDI-II :
-
Beck Depression Inventory-II
- SDS :
-
Self Rating Depression Scale
- PHQ-9 :
-
Patient Health Questionnaire -9
- HADS-D :
-
Hospital Anxiety and Depression Scale-Depression
- PCL-5 :
-
PTSD checklist for DSM-5
- PTSS-10 :
-
Posttraumatic symptom scale-10
- CAPS-5 :
-
Clinician Administered PTSD Scale for DSM-5
- IES-R :
-
Impact of Events Scale–Revised
- PTSD :
-
Post-traumatic Stress Disorder
- DSM :
-
Diagnostic and Statistical Manual of Mental Disorders
- HRQOL :
-
Health-related quality of life
- IES-6 :
-
Impact of Event Scale-6
- SCCM :
-
Society of Critical Care Medicine
- ICBT :
-
Internet-based Cognitive Behavioral Therapy
- COVID-19 :
-
Coronavirus disease 2019
- cCBT :
-
Computerized cognitive behavioral therapy
- NET :
-
Narrative exposure therapy
- SAD :
-
Sepsis-associated delirium
- CAM-ICU :
-
Confusion Assessment Method for the Intensive Care Unit
- ICDSC :
-
Intensive Care Delirium Screening Checklist
- ABCDEF :
-
Assess, prevent, and manage pain; Both spontaneous awakening and breathing trials; Choice of Analgesia and Sedation; Delirium assess, prevent, and manage; Early Mobility and Exercise; Family engagement/empowerment
References
Rudd KE, Johnson SC, Agesa KM et al (2020) Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the global burden of disease study. Lancet 395:200–211. https://doi.org/10.1016/S0140-6736(19)32989-7
Fleischmann C, Scherag A, Adhikari NK et al (2016) Assessment of global incidence and mortality of hospital-treated sepsis. current estimates and limitations. Am J Respir Crit Care Med 193:259–272. https://doi.org/10.1164/rccm.201504-0781OC
Mostel Z, Perl A, Marck M et al (2019) Post-sepsis syndrome - an evolving entity that afflicts survivors of sepsis. Mol Med 26:6. https://doi.org/10.1186/s10020-019-0132-z
Angus DC (2010) The lingering consequences of sepsis: a hidden public health disaster? JAMA 304:1833–1834. https://doi.org/10.1001/jama.2010.1546
Jones C, Griffiths RD (2013) Mental and physical disability after sepsis. Minerva Anestesiol 79:1306–1312
Prescott HC, Angus DC (2018) Enhancing recovery from sepsis: a review. JAMA 319:62–75. https://doi.org/10.1001/jama.2017.17687
Maldonado JR (2018) Delirium pathophysiology: an updated hypothesis of the etiology of acute brain failure. Int J Geriatr Psychiatry 33:1428–1457. https://doi.org/10.1002/gps.4823
Iwashyna TJ, Ely EW, Smith DM, Langa KM (2010) Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 304:1787–1794. https://doi.org/10.1001/jama.2010.1553
Fleischmann-Struzek C, Rose N, Freytag A et al (2021) Epidemiology and costs of postsepsis morbidity, nursing care dependency, and mortality in Germany, 2013 to 2017. JAMA Netw Open 4:e2134290. https://doi.org/10.1001/jamanetworkopen.2021.34290
Kim Y, Jin Y, Jin T, Lee SM (2020) Risk factors and outcomes of sepsis-associated delirium in intensive care unit patients: a secondary data analysis. Intensive Crit Care Nurs 59:102844. https://doi.org/10.1016/j.iccn.2020.102844
Yamamoto T, Mizobata Y, Kawazoe Y et al (2020) Incidence, risk factors, and outcomes for sepsis-associated delirium in patients with mechanical ventilation: a sub-analysis of a multicenter randomized controlled trial. J Crit Care 56:140–144. https://doi.org/10.1016/j.jcrc.2019.12.018
Zhang Y, Hu J, Hua T et al (2023) Development of a machine learning-based prediction model for sepsis-associated delirium in the intensive care unit. Sci Rep 13:12697. https://doi.org/10.1038/s41598-023-38650-4
Hatch R, Young D, Barber V et al (2018) Anxiety, depression and post traumatic stress disorder after critical illness: a UK-wide prospective cohort study. Crit Care 22:310. https://doi.org/10.1186/s13054-018-2223-6
Calsavara AJ, Costa PA, Nobre V, Teixeira AL (2021) Prevalence and risk factors for post-traumatic stress, anxiety, and depression in sepsis survivors after ICU discharge. Braz J Psychiatry 43:269–276. https://doi.org/10.1590/1516-4446-2020-0986
Oh TK, Park HY, Song IA (2021) Depression and long-term survival among south korean sepsis survivors: a Nationwide cohort study from 2011 to 2014. Crit Care Med 49:1470–1480. https://doi.org/10.1097/CCM.0000000000005030
Boede M, Gensichen JS, Jackson JC et al (2021) Trajectories of depression in sepsis survivors: an observational cohort study. Crit Care 25:161. https://doi.org/10.1186/s13054-021-03577-7
Cash A, Theus MH (2020) Mechanisms of blood-brain barrier dysfunction in traumatic brain injury. Int J Mol Sci 21:3344. https://doi.org/10.3390/ijms21093344
Galea I (2021) The blood-brain barrier in systemic infection and inflammation. Cell Mol Immunol 18:2489–2501. https://doi.org/10.1038/s41423-021-00757-x
Xu XE, Liu L, Wang YC et al (2019) Caspase-1 inhibitor exerts brain-protective effects against sepsis-associated encephalopathy and cognitive impairments in a mouse model of sepsis. Brain Behav Immun 80:859–870. https://doi.org/10.1016/j.bbi.2019.05.038
Silva AYO, Amorim ÉA, Barbosa-Silva MC et al (2020) Mesenchymal stromal cells protect the blood-brain barrier, reduce astrogliosis, and prevent cognitive and behavioral alterations in surviving septic mice. Crit Care Med 48:e290–e298. https://doi.org/10.1097/ccm.0000000000004219
Shulyatnikova T, Verkhratsky A (2020) Astroglia in sepsis associated encephalopathy. Neurochem Res 45:83–99. https://doi.org/10.1007/s11064-019-02743-2
Skelly DT, Hennessy E, Dansereau MA, Cunningham C (2013) A systematic analysis of the peripheral and CNS effects of systemic LPS, IL-1β, [corrected] TNF-α and IL-6 challenges in C57BL/6 mice. PLoS ONE 8:e69123. https://doi.org/10.1371/journal.pone.0069123
Sekino N, Selim M, Shehadah A (2022) Sepsis-associated brain injury: underlying mechanisms and potential therapeutic strategies for acute and long-term cognitive impairments. J Neuroinflammation 19:101. https://doi.org/10.1186/s12974-022-02464-4
Gu M, Mei XL, Zhao YN (2021) Sepsis and cerebral dysfunction: BBB damage, neuroinflammation, oxidative stress, apoptosis and autophagy as key mediators and the potential therapeutic approaches. Neurotox Res 39:489–503. https://doi.org/10.1007/s12640-020-00270-5
Calsavara AC, Rodrigues DH, Miranda AS et al (2013) Late anxiety-like behavior and neuroinflammation in mice subjected to sublethal polymicrobial sepsis. Neurotox Res 24:103–108. https://doi.org/10.1007/s12640-012-9364-1
Anderson ST, Commins S, Moynagh PN, Coogan AN (2015) Lipopolysaccharide-induced sepsis induces long-lasting affective changes in the mouse. Brain Behav Immun 43:98–109. https://doi.org/10.1016/j.bbi.2014.07.007
Zhu W, Cao FS, Feng J et al (2017) NLRP3 inflammasome activation contributes to long-term behavioral alterations in mice injected with lipopolysaccharide. Neuroscience 343:77–84. https://doi.org/10.1016/j.neuroscience.2016.11.037
Fang H, Wang Y, Deng J et al (2022) Sepsis-Induced Gut Dysbiosis Mediates the Susceptibility to Sepsis-Associated Encephalopathy in Mice. mSystems 7:e0139921. https://doi.org/10.1128/msystems.01399-21
Yang JM, Rui BB, Chen C et al (2014) Acetylsalicylic acid enhances the anti-inflammatory effect of fluoxetine through inhibition of NF-kappaB, p38-MAPK and ERK1/2 activation in lipopolysaccharide-induced BV-2 microglia cells. Neuroscience 275:296–304. https://doi.org/10.1016/j.neuroscience.2014.06.016
Kohl C, Sperner-Unterweger B (2007) IDO and clinical conditions associated with depressive symptoms. Curr Drug Metab 8:283–287. https://doi.org/10.2174/138920007780362572
Pisoschi AM, Pop A, Iordache F et al (2021) Oxidative stress mitigation by antioxidants - an overview on their chemistry and influences on health status. Eur J Med Chem 209:112891. https://doi.org/10.1016/j.ejmech.2020.112891
Zong Q, Pan Y, Liu Y et al (2023) pNaktide mitigates inflammation-induced neuronal damage and behavioral deficits through the oxidative stress pathway. Int Immunopharmacol 116:109727. https://doi.org/10.1016/j.intimp.2023.109727
Casaril AM, Domingues M, Lourenco DA et al (2020) 3-[(4-chlorophenyl)selanyl]-1-methyl-1H-indole ameliorates long-lasting depression- and anxiogenic-like behaviors and cognitive impairment in post-septic mice: involvement of neuroimmune and oxidative hallmarks. Chem Biol Interact 331:109278. https://doi.org/10.1016/j.cbi.2020.109278
Ranjbaran M, Kianian F, Ashabi G et al (2023) Beneficial effects of tannic acid on comorbid anxiety in cecal ligation and puncture-induced sepsis in rats and potential underlying mechanisms. Naunyn Schmiedebergs Arch Pharmacol 396:1019–1030. https://doi.org/10.1007/s00210-022-02374-5
Liu S, Pan Y, Li T et al (2023) The Role of Regulated Programmed Cell Death in Osteoarthritis: From Pathogenesis to Therapy. Int J Mol Sci 24. https://doi.org/10.3390/ijms24065364
Fan Z, Ma H, Li Y et al (2022) Neuronal MD2 induces long-term mental impairments in septic mice by facilitating necroptosis and apoptosis. Front Pharmacol 13:884821. https://doi.org/10.3389/fphar.2022.884821
Fang Z, Wu D, Deng J et al (2021) An MD2-perturbing peptide has therapeutic effects in rodent and rhesus monkey models of stroke. Sci Transl Med 13. https://doi.org/10.1126/scitranslmed.abb6716
Qin S, Zhang Z, Zhao Y et al (2022) The impact of acupuncture on neuroplasticity after ischemic stroke: a literature review and perspectives. Front Cell Neurosci 16:817732. https://doi.org/10.3389/fncel.2022.817732
Kikutani K, Hosokawa K, Giga H et al (2023) GENETIC deletion of translocator protein exacerbates post-sepsis syndrome with activation of the C1Q pathway in septic mouse model. Shock 59:82–90. https://doi.org/10.1097/shk.0000000000002030
Comim CM, Cassol OJ Jr, Constantino LC et al (2010) Depressive-like parameters in sepsis survivor rats. Neurotox Res 17:279–286. https://doi.org/10.1007/s12640-009-9101-6
Menke A (2019) Is the HPA Axis as target for depression outdated, or is there a new Hope? Front Psychiatry 10:101. https://doi.org/10.3389/fpsyt.2019.00101
Shen F, Song Z, Xie P et al (2021) Polygonatum sibiricum polysaccharide prevents depression-like behaviors by reducing oxidative stress, inflammation, and cellular and synaptic damage. J Ethnopharmacol 275:114164. https://doi.org/10.1016/j.jep.2021.114164
Babaei F, Mirzababaei M, Mohammadi G et al (2022) Saccharomyces boulardii attenuates lipopolysaccharide-induced anxiety-like behaviors in rats. Neurosci Lett 778:136600. https://doi.org/10.1016/j.neulet.2022.136600
Spencer-Segal JL, Singer BH, Laborc K et al (2020) Sepsis survivor mice exhibit a behavioral endocrine syndrome with ventral hippocampal dysfunction. Psychoneuroendocrinology 117:104679. https://doi.org/10.1016/j.psyneuen.2020.104679
Tang C, Jin Y, Wang H (2022) The biological alterations of synapse/synapse formation in sepsis-associated encephalopathy. Front Synaptic Neurosci 14:1054605. https://doi.org/10.3389/fnsyn.2022.1054605
Ranjbaran M, Kianian F, Kadkhodaee M et al (2022) Mesenchymal stem cells and their conditioned medium as potential therapeutic strategies in managing comorbid anxiety in rat sepsis induced by cecal ligation and puncture. Iran J Basic Med Sci 25:690–697. https://doi.org/10.22038/IJBMS.2022.61860.13690
Kitagawa Y, Nakaso K, Horikoshi Y et al (2019) System x(c)(-) in microglia is a novel therapeutic target for post-septic neurological and psychiatric illness. Sci Rep 9:7562. https://doi.org/10.1038/s41598-019-44006-8
Parrott JM, Redus L, Santana-Coelho D et al (2016) Neurotoxic kynurenine metabolism is increased in the dorsal hippocampus and drives distinct depressive behaviors during inflammation. Transl Psychiatry 6:e918. https://doi.org/10.1038/tp.2016.200
Mikkelsen ME, Still M, Anderson BJ et al (2020) Society of critical care medicine’s international consensus conference on prediction and identification of long-term impairments after critical illness. Crit Care Med 48:1670–1679. https://doi.org/10.1097/CCM.0000000000004586
Julian LJ (2011) Measures of anxiety: state-trait anxiety inventory (STAI), Beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A). Arthritis Care Res (Hoboken) 63(Suppl 11):S467-472. https://doi.org/10.1002/acr.20561
Inoue S, Nakanishi N, Sugiyama J et al (2022) Prevalence and Long-Term Prognosis of Post-Intensive Care Syndrome after Sepsis: A Single-Center Prospective Observational Study. J Clin Med 11. https://doi.org/10.3390/jcm11185257
Whelan-Goodinson R, Ponsford J, Schonberger M (2009) Validity of the hospital anxiety and depression scale to assess depression and anxiety following traumatic brain injury as compared with the structured clinical interview for DSM-IV. J Affect Disord 114:94–102. https://doi.org/10.1016/j.jad.2008.06.007
Shen G, He Y, Ni J et al (2021) Effects of comprehensive nursing on negative emotion and prognosis of patients with sepsis. Am J Transl Res 13:8221–8227
Dunstan DA, Scott N, Todd AK (2017) Screening for anxiety and depression: reassessing the utility of the zung scales. BMC Psychiatry 17:329. https://doi.org/10.1186/s12888-017-1489-6
Dunstan DA, Scott N (2018) Assigning clinical significance and symptom severity using the zung scales: levels of misclassification arising from confusion between index and raw scores. Depress Res Treat 2018:9250972. https://doi.org/10.1155/2018/9250972
Cuijpers P, Dekker J, Noteboom A et al (2007) Sensitivity and specificity of the major depression inventory in outpatients. BMC Psychiatry 7:39. https://doi.org/10.1186/1471-244X-7-39
Kosilek RP, Schmidt K, Baumeister SE et al (2021) Frequency and risk factors of post-intensive care syndrome components in a multicenter randomized controlled trial of german sepsis survivors. J Crit Care 65:268–273. https://doi.org/10.1016/j.jcrc.2021.07.006
Fountoulakis KN, Iacovides A, Kleanthous S et al (2003) Reliability, validity and psychometric properties of the greek translation of the major depression inventory. BMC Psychiatry 3:2. https://doi.org/10.1186/1471-244x-3-2
Bech PER, Wermuth L (1998) Applicability and validity of the major depression inventory in patients with parkinson’s disease. Nord J Psychiatry 52:305–310. https://doi.org/10.1080/08039489850149741
Smarr KL, Keefer AL (2011) Measures of depression and depressive symptoms: Beck depression inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), geriatric depression scale (GDS), hospital anxiety and depression scale (HADS), and patient health Questionnaire-9 (PHQ-9). Arthritis Care Res (Hoboken) 63(Suppl 11):S454-466. https://doi.org/10.1002/acr.20556
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16:606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Inoue T, Tanaka T, Nakagawa S et al (2012) Utility and limitations of PHQ-9 in a clinic specializing in psychiatric care. BMC Psychiatry 12:73. https://doi.org/10.1186/1471-244x-12-73
Gawlytta R, Kesselmeier M, Scherag A et al (2022) Internet-based cognitive-behavioural writing therapy for reducing post-traumatic stress after severe sepsis in patients and their spouses (REPAIR): results of a randomised-controlled trial. BMJ Open 12:e050305. https://doi.org/10.1136/bmjopen-2021-050305
Gerta Bardhoshi BTE, Duncan K et al (2016) Choosing assessment instruments for posttraumatic stress disorder screening and outcome research. J Couns Dev 94:184–194. https://doi.org/10.1002/jcad.12075
Kramer LB, Whiteman SE, Petri JM et al (2022) Self-Rated Versus Clinician-Rated Assessment of Posttraumatic Stress Disorder: An Evaluation of Discrepancies Between the PTSD Checklist for DSM-5 and the Clinician-Administered PTSD Scale for DSM-5. Assessment:10731911221113571. https://doi.org/10.1177/10731911221113571
Rosendahl J, Kisyova H, Gawlytta R, Scherag A (2019) Comparative validation of three screening instruments for posttraumatic stress disorder after intensive care. J Crit Care 53:149–154. https://doi.org/10.1016/j.jcrc.2019.06.016
Boer KR, van Ruler O, van Emmerik AA et al (2008) Factors associated with posttraumatic stress symptoms in a prospective cohort of patients after abdominal sepsis: a nomogram. Intensive Care Med 34:664–674. https://doi.org/10.1007/s00134-007-0941-3
Stoll C, Kapfhammer HP, Rothenhäusler HB et al (1999) Sensitivity and specificity of a screening test to document traumatic experiences and to diagnose post-traumatic stress disorder in ARDS patients after intensive care treatment. Intensive Care Med 25:697–704. https://doi.org/10.1007/s001340050932
Gawlytta R, Brunkhorst F, Niemeyer H et al (2020) Dyadic post-traumatic stress after intensive care: case report of a sepsis patient and his wife. Intensive Crit Care Nurs 58:102806. https://doi.org/10.1016/j.iccn.2020.102806
Sharif Nia H, Kaur H, Fomani FK et al (2021) Psychometric properties of the impact of events scale-revised (IES-R) among general iranian population during the COVID-19 pandemic. Front Psychiatry 12:692498. https://doi.org/10.3389/fpsyt.2021.692498
Hosey MM, Bienvenu OJ, Dinglas VD et al (2019) The IES-R remains a core outcome measure for PTSD in critical illness survivorship research. Crit Care 23:362. https://doi.org/10.1186/s13054-019-2630-3
Chen TJ, Chung YW, Chang HR et al (2021) Diagnostic accuracy of the CAM-ICU and ICDSC in detecting intensive care unit delirium: a bivariate meta-analysis. Int J Nurs Stud 113:103782. https://doi.org/10.1016/j.ijnurstu.2020.103782
Davydow DS, Hough CL, Langa KM, Iwashyna TJ (2013) Symptoms of depression in survivors of severe sepsis: a prospective cohort study of older americans. Am J Geriatr Psychiatry 21:887–897. https://doi.org/10.1016/j.jagp.2013.01.017
Schmidt KF, Schwarzkopf D, Baldwin LM et al (2020) Long-term courses of sepsis survivors: effects of a primary care management intervention. Am J Med 133(381–385):e385. https://doi.org/10.1016/j.amjmed.2019.08.033
Pun BT, Balas MC, Barnes-Daly MA et al (2019) Caring for critically ill patients with the ABCDEF bundle: results of the ICU liberation collaborative in over 15,000 adults. Crit Care Med 47:3–14. https://doi.org/10.1097/ccm.0000000000003482
Schweickert WD, Pohlman MC, Pohlman AS et al (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 373:1874–1882. https://doi.org/10.1016/s0140-6736(09)60658-9
Zhang Y, Deng Z, Li Y et al (2020) Mesenchymal stem cells provide neuroprotection by regulating heat stroke-induced brain inflammation. Front Neurol 11:372. https://doi.org/10.3389/fneur.2020.00372
Cassol OJ Jr, Comim CM, Petronilho F et al (2010) Low dose dexamethasone reverses depressive-like parameters and memory impairment in rats submitted to sepsis. Neurosci Lett 473:126–130. https://doi.org/10.1016/j.neulet.2010.02.036
Petronilho F, Perico SR, Vuolo F et al (2012) Protective effects of guanosine against sepsis-induced damage in rat brain and cognitive impairment. Brain Behav Immun 26:904–910. https://doi.org/10.1016/j.bbi.2012.03.007
Leite FB, Prediger RD, Silva MV et al (2013) Role of nicotine on cognitive and behavioral deficits in sepsis-surviving rats. Brain Res 1507:74–82. https://doi.org/10.1016/j.brainres.2013.02.036
Ozcan PE, Senturk E, Orhun G et al (2015) Effects of intravenous immunoglobulin therapy on behavior deficits and functions in sepsis model. Ann Intensive Care 5:62. https://doi.org/10.1186/s13613-015-0062-z
Chen L, Qing W, Yi Z et al (2021) NU9056, a KAT 5 inhibitor, treatment alleviates brain dysfunction by inhibiting NLRP3 inflammasome activation, affecting gut microbiota, and derived metabolites in LPS-treated mice. Front Nutr 8:701760. https://doi.org/10.3389/fnut.2021.701760
Zhang J, Ma L, Wan X et al (2021) (R)-ketamine attenuates LPS-induced endotoxin-derived delirium through inhibition of neuroinflammation. Psychopharmacology 238:2743–2753. https://doi.org/10.1007/s00213-021-05889-6
Smith CJ, Renshaw P, Yurgelun-Todd D, Sheth C (2022) Acute and chronic neuropsychiatric symptoms in novel coronavirus disease 2019 (COVID-19) patients: a qualitative review. Front Public Health 10:772335. https://doi.org/10.3389/fpubh.2022.772335
Ng JH, Sun A, Je HS, Tan EK (2023) Unravelling pathophysiology of neurological and psychiatric complications of COVID-19 using brain organoids. Neuroscientist 29:30–40. https://doi.org/10.1177/10738584211015136
Liu TH, Ho CH, Chen DT et al (2023) Omega-3 polyunsaturated fatty acids and the psychiatric post-acute sequelae of COVID-19: a one-year retrospective cohort analysis of 33,908 patients. Brain Behav Immun 114:453–461. https://doi.org/10.1016/j.bbi.2023.09.008
Tokuda R, Nakamura K, Takatani Y et al (2023) Sepsis-Associated Delirium: A Narrative Review. J Clin Med 12. https://doi.org/10.3390/jcm12041273
Fan Y, Shi Y, Zhang J et al (2021) The effects of narrative exposure therapy on COVID-19 patients with post-traumatic stress symptoms: a randomized controlled trial. J Affect Disord 293:141–147. https://doi.org/10.1016/j.jad.2021.06.019
Liu Z, Qiao D, Xu Y et al (2021) The efficacy of computerized cognitive behavioral therapy for depressive and anxiety symptoms in patients with COVID-19: randomized controlled trial. J Med Internet Res 23:e26883. https://doi.org/10.2196/26883
Xiao CX, Lin YJ, Lin RQ et al (2020) Effects of progressive muscle relaxation training on negative emotions and sleep quality in COVID-19 patients: a clinical observational study. Medicine (Baltimore) 99:e23185. https://doi.org/10.1097/md.0000000000023185
White L, Jackson T (2022) Delirium and COVID-19: a narrative review of emerging evidence. Anaesthesia 77(Suppl 1):49–58. https://doi.org/10.1111/anae.15627
Acknowledgements
Figure 1 was created with MedPeer (www.medpeer.cn). We thank the website for its support.
Funding
This work was supported by the Key R&D Program of Hubei Province (grant number. 2022BCA038).
Author information
Authors and Affiliations
Contributions
WZ conceived the idea for the article and performed the literature search. DYL analysed the data, wrote the original manuscript and drew the figure. XJZ and YRL drew the tables. LJ, HJH, YQS, and SHW revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Informed consent
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, D., Zhang, X., Lu, Y. et al. Post-sepsis psychiatric disorder: Pathophysiology, prevention, and treatment. Neurol Sci 45, 3093–3105 (2024). https://doi.org/10.1007/s10072-024-07409-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-024-07409-8