Abstract
Psoriatic arthritis (PsA) is a complex inflammatory disease characterized by musculoskeletal and non-musculoskeletal manifestations. It is a distinct disease entity at the interface between rheumatology and dermatology, making it challenging to manage. The diverse clinical presentation and severity of PsA require a multidisciplinary approach for optimal care. Early diagnosis and management are necessary to improving quality of life for patients. In Saudi Arabia, there is currently no unified national consensus on the best practices for managing PsA. This lack of consensus leads to debate and uncertainty in the treatment of the disease, resulting in over or under prescribing of biological agents. To address this issue, a multidisciplinary work group was formed by the Saudi Ministry of Health. This group, consisting of dermatologists, rheumatologists, and pharmacists, aimed to develop evidence-based consensus recommendations for he use and monitoring of biological therapy in PsA management. The work group conducted five consensus workshops between December 2021 to March 2022. Using the nominal group technique, they discussed various aspects of PsA management, including eligibility criteria for biological treatment, monitoring of disease activity, treatment goals, screening, precautions, and management of PsA with biologic therapies. The group also considered special considerations for patients with comorbidities, pregnant and lactating women, as well as pediatric and adolescent populations. The resulting consensus document provides recommendations that are applicable to the Saudi setting, taking into account international guidelines and the specific needs of PsA patients in the country. The consensus document will be regularly updated to incorporate new data and therapeutic agents as they become available.
Key Points • In Saudi Arabia, there is a lack of unified national consensus on the optimal management of PsA, therefore, this article aims to provide up-to-date evidence-based consensus recommendations for the optimal use and monitoring of biologic therapy in the management of PsA in Saudi Arabia. • The consensus development process was undertaken by a multidisciplinary work group of 13 experts, including two dermatologists, six rheumatologists, and five pharmacists. • There is more than one disease activity tool used in PsA disease, depending on the disease domain – peripheral arthritis Disease Activity Index in Psoriatic Arthritis (DAPSA) or Minimal Disease Activity (MDA), axial PsA Ankylosing Spondylitis Disease Activity Score (ASDAS), and dactylitis and enthesitis MDA. • The main goal of therapy in all patients with PsA is to achieve the target of remission, or alternatively, low disease activity in all disease domains and improve quality of life (QoL). |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background and definition
Psoriatic arthritis (PsA) is a complex inflammatory disease characterized by both musculoskeletal and non-musculoskeletal manifestations, representing a distinct disease entity at the intersection of rheumatology and dermatology [1].
PsA is distinguished from other types of inflammatory arthritis by the fact that it is often preceded by psoriasis, observed in approximately 80% of cases [2]. The global annual incidence of PsA is 83 per 100,000 with no discernible gender predominance, and a prevalence of 133 per 100,000, reflecting consistent geographic variability [3].
Despite its importance, the Middle East and North Africa (MENA) region, including Saudi Arabia, lack adequate epidemiological data, reflecting a gap in understanding the specific characteristics of this population [4]. Within the region, managing PsA presents significant challenges due to the absence of local registries, reliable diagnostic methods, and effective reporting [4]. This has led to the misconception that PsA is relatively rare in MENA, although the actual burden remains unknown [4]. Existing insights are sporadic, arising from isolated studies [5,6,7].
The manifestations of PsA extend beyond peripheral arthritis, enthesitis, dactylitis, spondylitis, psoriatic skin, nail disease, and uveitis, encompassing the gastrointestinal system, often associated with inflammatory bowel disease (IBD) [8,9,10]. A recent study by Alunizi et. al., provided valuable insights into PsA presentation and therapeutic interventions specific to the Saudi population [7]. The study reported percentages of 92.3%, 28.2%, 15%, and 12.5% for peripheral arthritis, axial involvement, enthesitis, and dactylitis, respectively [7]. PsA patients also suffer from sleep disturbance, decreased work capacity, and social isolation [11]. These myriads of symptoms collectively impact the quality of life (QoL), inducing fatigue in 22% of patients [12]. The clinical diversity of PsA demands a multidisciplinary approach for effective management [13, 14].
The pivotal 2006 International Classification of Psoriatic Arthritis (CASPAR) study introduced standardized classification criteria for PsA [15]. Since then, additional guidelines have been developed to facilitate the management of PsA [16,17,18].
Due to the impairment of the QoL, early diagnosis and management of PsA are necessary for optimal care and good disease prognosis [19]. The management becomes more challenging in the MENA region due to the limited knowledge and awareness of this disease entity [4]. Consequently, the development of a specific guideline tailored to the Saudi Arabian population becomes imperative for addressing these challenges and enhancing PsA care in the region.
Purpose, aim, and scope
In Saudi Arabia, there is a lack of unified national consensus on the optimal management of PsA. As a result, there is often a debate among healthcare providers about how to make clinical decisions when managing the disease, which can result in either over-prescribing or under-prescribing biological agents. Al Rayes, et al.’s recently published consensus-based recommendations addressed the aspects of diagnosis, referral and clinical management of patients with PSA [20]. Therefore, this paper aims to deliver evidence-based consensus recommendations for the optimal use and monitoring of biological therapy in managing PsA. Due consideration was given to the specific characteristics of the patient population in Saudi Arabia. These recommendations are intended to aid physicians in managing their patients and should therefore be viewed as informative rather than prescriptive.
Target population, audience/end-users
The target population for the present consensus document are people in Saudi Arabia with PsA. This consensus statement is for rheumatologists, dermatologists, and other healthcare providers involved in managing people with PsA in the secondary care setting.
Materials & methods
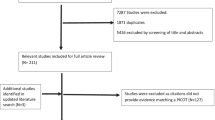
A multidisciplinary work group consisting of two dermatologists, six rheumatologists, and five pharmacists were convened by the Saudi Ministry of Health (MOH) based on their expertise in managing PsA. Throughout the process of developing the consensus recommendations, one method expert was invited and consulted. Over a period of four months (December 2021 – March 2022), five in-person consensus workshops were conducted to accomplish three main objectives: 1) discuss the need for national consensus recommendations for PsA management, 2) review existing international guidelines, and 3) create recommendations suitable for the Saudi context.
Before the first workshop, a literature search was conducted using PubMed to identify relevant articles on PsA guidelines. Based on their reputation and relevance, three international guidelines were chosen as the starting point for developing the current recommendations: The Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA), the European Alliance of Associations for Rheumatology (EULAR) and the British Society of Rheumatology (BSR) guidelines [16, 21,22,23,24,25,26]. To ensure the recommendations were based on the latest evidence, the reference lists of these guidelines were evaluated and additional articles on emerging evidence were sought.
The workgroup assigned tasks to its members to develop evidence-based recommendations on various PsA management topics, taking into considering both the evidence and its applicability to real-world practice. During the workshops, a modified Nominal Group Technique (NGT) was used to reach agreements on the recommendations [27]. The NGT was chosen as the consensus methodology as it is a well-established and formal process that ensures a fair, inclusive, and rigorous consensus development process [27]. It allows for the integration of diverse perspectives and expertise, which was important given the multidisciplinary nature of the work group [27]. A recommendation was considered agreed upon if at least 75% of the members voted in favor. The strength of the recommendations was not indicated. A draft document containing all the consensus recommendations was compiled and shared with the expert workgroup and MOH experts for a 30-day feedback period. During the final workshop, the received comments were discussed, and further agreements were reached.
Results
Eligibility criteria for biological treatment
The following criteria are accepted as appropriate for initiating therapy with biologic disease-modifying antirheumatic drugs (bDMARDs) and Janus kinase inhibitors (JAKi) [16, 28,29,30,31,32,33,34,35,36,37,38,39]:
-
1.
Peripheral arthritis: patients who have failed, developed side effects, or have contraindications to conventional DMARDs.
-
2.
Axial PsA: patients who have failed, developed side effects, or have contraindications to non-steroidal anti-inflammatory drugs (NSAIDs) treatment.
-
3.
Enthesitis and dactylitis: patients who have failed, developed side effects, or have contraindications to NSAIDs treatment.
Monitoring for disease activity and assessment tools
Patients with PsA should be monitored regularly to assess the degree of disease activity and the need for therapy adjustment [16]. It is recommended to monitor patients with active disease more often, ranging from monthly to every three months. However, the data is lacking regarding the best interval for monitoring [23].
It has been suggested to use a treat-to-target (T2T) approach for patients treated for PsA, in which treatment is adjusted at frequent periods if the treatment goal, defined as inactive disease or minimal disease activity (MDA), was not met [16].
The best tool to monitor disease activity is not established. However, monitoring patients with PsA should focus on patient-reported measures and cover all domains of the disease; peripheral arthritis, axial disease, enthesitis, and dactylitis by comprehensive history and physical examination. Moreover, assessment should be supplemented with appropriate laboratory tests and imaging studies [22, 23]. Validated and quantified measurements should be considered when considering the use of assessment tools. Multiple validated assessment tools are available for patients with PsA [40]. Examples of available measurements are Disease Activity Index for Psoriatic Arthritis (DAPSA); minimal disease activity criteria (MDA); Disease Activity Score (DAS and DAS 28); the Simplified Disease Activity Index (SDAI); the Clinical Disease Activity Index (CDAI); Composite Psoriatic Disease Activity Index (CPDAI); and the Psoriatic Arthritis Disease Activity Score (PASDAS) [23, 40].
In peripheral arthritis, we recommend using either DAPSA or MDA as tools for disease activity monitoring in patients since both support T2T management in PsA [40].
DAPSA score is calculated by the sum of the following:
-
swollen joint count of 66 joints,
-
tender joint count of 68 joints,
-
patient’s global assessment on a 10 cm visual analogue score (VAS) (in cm): (0 for not active, up to 10 for very active)
-
patient’s pain score on a 10 cm VAS (in cm): (0 for none up to 10 for very severe), and
-
CRP (mg/dL).
On the other hand, a patient is classified as achieving MDA when meeting 5 of the 7 criteria shown in Table 1. Moreover, patients can be further classified as achieving very low disease activity (VLDA) when they meet all the criteria [40]. The interpretation of DAPSA scores and MDA criteria for PsA are shown in Table 1 [40].
In patients with axial disease, disease activity assessment with measures used for axial spondylarthritis is recommended [23, 41]. Examples of commonly used measures in axial spondylarthritis are the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and the Ankylosing Spondylitis Disease Activity Score (ASDAS) [41,42,43]. For the purposes of these consensus recommendations, the ASDAS tool is utilized as it combines acute phase reactants and patient- reported outcomes. The ASDAS disease activity score is classified as shown in Fig. 1 [44].
The recently updated T2T recommendations propose at least 50% improvement of the composite measure within 3 months and target achievement within 6 months from therapy initiation. Therefore, it is recommended to use a continuous measure of disease activity to follow patients longitudinally and reflect their perceptions [16].
Treatment goals
The main goal of therapy in all patients with PsA is to achieve the target of remission, or alternatively, low disease activity in all disease domains and improve QoL [16, 22, 23].
Any of the following criteria should be achieved for the treatment goal of PsA:
-
1.
Peripheral arthritis: at least 50% improvement of the DAPSA score within 3 months and reaching the target within 6 months from therapy initiation by either achieving complete remission (DAPSA ≤ 4) or low disease activity (DAPSA > 4 and ≤ 14) [45].
-
2.
Axial PsA: a change of 1.1 or more in the ASDAS score within 3 months and reaching the target within 6 months from therapy initiation by either achieving complete remission (ASDAS < 1.3) or low disease activity (ASDAS < 2.1) [42, 46].
-
3.
Enthesitis and dactylitis: meeting at least 5 of the 7 MDA criteria within 6 months from therapy initiation [45].
Screening, precautions, and monitoring of biologics
Baseline assessment should include complete blood count (CBC), liver enzymes test (alanine transaminase (ALT), aspartate aminotransferase (AST)), creatinine, serum albumin, hepatitis B and C serology, tuberculin skin test (TST) or interferon-gamma release assay (IGRA) as appropriate, and a chest X-ray (Table 2) [47,48,49,50,51,52,53,54,55,56]. Hepatitis B serology includes HBsAg, HBcAb, and HBsAb [50]. HIV screening is recommended for high-risk group patients [53]. Patients initiated on JAKi should have a baseline lipid profile including total cholesterol (TC), low-density lipoprotein (LDL) and high-density lipoprotein (HDL) [52].
Screening for Tuberculosis (TB)
The use of bDMARDs and JAKi therapy is associated with a higher likelihood of developing active TB and experiencing reactivation of latent TB, making it imperative to conduct screening for both active and latent TB before starting the treatment [53, 54]. The risk is higher with tumor necrosis factor inhibitors (TNFi) treatment than with other bDMARDs [53]. The screening for TB should include a chest X-ray and either TST or IGRA. Immunocompromised patients have lower sensitivity and specificity for TST, and to a lesser extent, IGRA test [55, 56]. Therefore, it is recommended to do both TST and IGRA tests in immunocompromised patients [57]. A patient with a positive TST or IGRA test should be diagnosed with latent TB and treated accordingly [57].
bDMARDs and JAKi therapies for the treatment of severe PsA
Table 3 lists all bDMARDs and JAKi therapies that are currently registered and approved by the Saudi Food and Drug Authority (SFDA) for the treatment of severe PsA. It provides a summary of the dosing scheme (loading and maintenance), evaluation of the efficacy, and half-life [34, 38, 58,59,60,61,62,63,64,65,66,67,68,69,70,71].
Treatment algorithm
Figure 2 represents the treatment algorithm proposed for the management of the following domains of PsA: peripheral arthritis, dactylitis, enthesitis, and axial PsA.
Peripheral arthritis
The treatment choice in patients with peripheral arthritis should be based on poor prognostic factors [28]. In the absence of poor prognostic factors, patients can be treated with NSAIDs [29]. If disease activity persists after four weeks of NSAIDs treatment, DMARDs should be initiated with methotrexate (MTX) being the preferred choice [30]. However, leflunomide can also be used [30]. Patients with one or more poor prognostic factors should start with MTX as the first line of treatment [30]. Poor prognostic factors include polyarthritis, joint damage, high sedimentation rate or CRP, and clinically relevant extra-articular features [72].
In patients with inadequate response or intolerance to NSAIDs and MTX, treatment with bDMARDs and JAKi is recommended [16]. Inadequate response to treatment is defined as a lack of symptom improvement within three months (50% or greater reduction in the DAPSA), or failure to achieve treatment target after six months (low disease activity or complete remission). Patients with inadequate treatment response to conventional DMARDs should be started on interleukin 17 inhibitors (IL-17i) [31, 32]. This recommendation is supported by research indicating that IL-17i optimize more disease domains, provide better skin responses, and demonstrate effective musculoskeletal efficacy in patients with skin psoriasis [73]. IL-17i also have better persistence and fewer safety concerns compared to TNFi [73]. Patients with inadequate response to treatment with IL-17i should be switched to JAKi, as the SELECT-PSA trial has shown that JAKi are superior to TNFi [36, 37]. Patients with inadequate response to IL-17i and JAKi can be started on IL-23i or TNFi [33,34,35]. The recommendation to prioritize IL-23i after inadequate response to IL-17i and JAKi is based on limited clinical practice experience in Saudi Arabia at present.
Phosphodiesterase 4 (PDE4) inhibitor is recommended for patients with mild peripheral arthritis who have failed conventional DMARDs and have a contraindication or intolerance to bDMARDs or JAKi [39]. Mild peripheral arthritis is defined as oligoarthritis or low disease activity by composite scores (DAPSA > 4–14).
Dactylitis and enthesitis
In patients with enthesitis and dactylitis, it is recommended to begin treatment with NSAIDs [16, 38]. IL-17i are recommended for patients with persistent enthesitis/dactylitis symptoms or intolerance to NSAIDs [31, 32]. Patients with inadequate response to IL-17i should be switched to IL-23i [33, 34, 74]. Patients with inadequate response to IL-23i can be switched to JAKi and TNFi, due to the shorter retention rate of TNFi [35,36,37].
Axial PsA
In patients with axial disease, we recommend using NSAID as the first line of treatment [16]. For patients with an inadequate response (ASDAS ≥ 2.1) within 4–12 weeks of treatment or have side effects or contraindications to NSAIDs treatment, IL-17i should be started [31, 32]. This is because IL-17i has shown efficacy in treating axial PsA in a randomized controlled trial (RCT), whereas there is current no RCT data available for TNFi in axial PsA [75]. If patient symptoms do not improve after three months of treatment (decrease of ≥ 1.1 points on ASDAS) or do not achieve the treatment target at six months (ASDAS < 2.1), we recommend switching to a TNFi. JAKi or IL-23i can be used if the patient fails TNFi treatment [33, 34, 36, 37].
Recommendations for the treatment of PsA with biological therapies
Adjusting/maintenance biological therapy
In patients with a well-controlled disease, there is insufficient consensus on whether their bDMARDs dose should be maintained, tapered, or discontinued altogether. There are limited data suggesting a particular risk of relapse with treatment tapering [76,77,78,79,80,81]. Therefore, physicians should explain the risk of relapse to the patient before tapering their medications. Tapering the treatment is considered appropriate for patients with the following criteria [16]: complete remission of peripheral arthritis (DAPSA ≤ 4), complete remission of axial PsA (ASDAS < 1.3), absence of extra-articular features, at least six consecutive months of complete remission, and normal acute phase reactants.
The total dose can be initially reduced by 20–50% by either decreasing the dose or increasing the dosing interval [81, 82]. Following tapering, the patient should be evaluated after eight weeks. If the patient remains in remission, follow-up visits may be scheduled every 12–16 weeks. Patients can contact the clinic coordinator for an early appointment if they feel their disease activity increases. Disease activity should be assessed every visit through clinical examination and inflammatory markers. Imaging studies can be utilized for further evaluation [83]. When remission is lost, the bDMARDs should be restored to the previous dose. Corticosteroids or NSAIDs can be used for symptomatic relief during this period.
Combination
There is little evidence that combining MTX with bDMARDs improves the efficacy of bDMARDs in PsA patients. However, some data suggest that combining MTX with TNFi is beneficial in terms of treatment maintenance and level of response, especially in patients using monoclonal antibodies [84, 85].
Biologic therapy discontinuation
Discontinuation of bDMARDs is not recommended as it is almost always associated with disease relapse [16, 78,79,80,81]. There are certain factors that can predict if loss of remission after discontinuing treatment, such as high disease activity, smoking, male gender, skin involvement, and synovial hypertrophy [81]. However, patient preference for stopping the medication should be acknowledged. If a patient is undergoing tapering, bDMARD discontinuation may be considered if they are at a minimal dose, have achieved the therapeutic goal for 6–12 months after the last dosage decrease, and there is no evidence of significant radiographic progression or active disease on ultrasound [82].
The minimal tapered dose is defined as 25% of the medication dose shown in the summary of product characteristics (SPC) [82]. Once the bDMARD is discontinued, the patient should be monitored closely by the physician.
Management of inadequate response
Switching therapy among patients who have failed a biological agent should preferably be to another agent with a different mechanism of action. Evidence has shown that the mean TNFi survival rate is reduced significantly after shifting to another TNFi agent (first TNFi 2.2 years, second TNFi 1.3 years and third TNFi 1.1 years) [86]. Moreover, an abstract published in EULAR 2021 indicates that if patients failed secukinumab and then shifted to ixekizumab (both agents are IL-17i), 65% will fail after a median time of eight months [87]. There were no head-to-head trials evaluating the best agents to be used in such patients’ population. This offers flexibility for the clinician to choose from the agents. Comorbidities, extra-articular manifestations, and active disease domains should be taken into consideration during the switching process, while some biological agents could be contraindicated or less/non-effective as compared with others. Moreover, a patient-centered approach could assist in selecting the agent, such as the preference of oral route or frequency of injections.
Use of bDMARDs and JAKi in special patient populations
With the increased introduction of biologics in PsA management, reaching disease remission is becoming a possible and desirable goal. Despite their efficacy in PsA, biologics carry some risks that clinicians should be aware of, especially in patients with special situations or comorbidities [47, 88].
Table 4 presents recommendations for treatment choices for people with the following comorbidities: infection, TB, HBV, HCV, HIV, malignancy, cardiovascular diseases, respiratory diseases, uveitis, demyelinating disease, connective tissue diseases, obesity, patients undergoing surgery, and IBD. It also covers the choice of therapy in pediatrics and adolescents, and pregnant and lactating women [16, 21, 23, 47, 53, 72, 76, 88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143].
Conclusion
In conclusion, these evidence-based consensus recommendations offer valuable guidance for the management of PsA in Saudi Arabia. They are rooted in the most up-to-date evidence and global consensus statements. The recommendations emphasize the importance of involving patients in shared decision-making and adopting a patient-centered approach to care. They also highlight the rational use of medications and advocate for a step-care approach in treatment, along with more frequent monitoring of active disease. Additionally, it is important for the treating physician to review the properties of SFDA-approved biologic agents, such as their efficacy, half-life, dosing scheme, and patient preference, before selecting a treatment option treatment selection. As more research develops, these recommendations may be subject to amendment and adjustment.
References
Savage L, Tinazzi I, Zabotti A, Laws PM, Wittmann M, McGonagle D (2020) Defining pre-clinical psoriatic arthritis in an integrated dermato-rheumatology environment. J Clin Med 9(10):3262. https://doi.org/10.3390/jcm9103262
Brockbank J, Gladman D (2002) Diagnosis and management of psoriatic arthritis. Drugs 62(17):2447–2457
Scotti L et al (2018) Prevalence and incidence of psoriatic arthritis: A systematic review and meta-analysis. Semin Arthritis Rheum 48(1):28–34
Bedaiwi M et al (2019) Disease burden and treatment challenges of psoriatic arthritis in Africa and the Middle East. Rheumatol Int 39(8):1321–1329
Alrubaiaan MT, Alsulaiman SA, Alqahtani A, Altasan AN, Almehrij FO, Alrashid A, Mohamed OL (2023) Prevalence and clinical predictors of psoriatic arthritis in saudi patients with psoriasis: a single-center retrospective cohort study. Cureus 15(10):e46632. https://doi.org/10.7759/cureus.46632
Elnady B et al (2019) Subclinical synovitis and enthesitis in psoriasis patients and controls by ultrasonography in Saudi Arabia; incidence of psoriatic arthritis during two years. Clin Rheumatol 38(6):1627–1635
Alunizi SR, AlShanqeeti A, Alenzi KA, Al-Homood IA (2022) Psoriatic arthritis: Saudi retrospective observational study of manifestations and treatments. Ann Rheumatol Autoimmun 2(2):53–57. https://doi.org/10.4103/ara.ara_14_22
Cassell SE et al (2007) The modified Nail Psoriasis Severity Index: validation of an instrument to assess psoriatic nail involvement in patients with psoriatic arthritis. J Rheumatol 34(1):123–129
Abbouda A et al (2017) Psoriasis and psoriatic arthritis-related uveitis: different ophthalmological manifestations and ocular inflammation features. Semin Ophthalmol 32(6):715–720
FitzGerald O et al (2021) Psoriatic arthritis. Nat Rev Dis Primers 7(1):59
Orbai AM et al (2017) International patient and physician consensus on a psoriatic arthritis core outcome set for clinical trials. Ann Rheum Dis 76(4):673–680
Eder L et al (2016) The incidence and risk factors for psoriatic arthritis in patients with psoriasis: a prospective cohort study. Arthritis Rheumatol 68(4):915–923
Ritchlin CT et al (2009) Treatment recommendations for psoriatic arthritis. Ann Rheum Dis 68(9):1387–1394
Abdulghani M et al (2011) Management of psoriasis in Africa and the Middle East: a review of current opinion, practice and opportunities for improvement. J Int Med Res 39(5):1573–1588
Taylor W et al (2006) Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 54(8):2665–2673
Gossec L et al (2020) EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2019 update. Ann Rheum Dis 79(6):700–712
Coates LC, Fransen J, Helliwell PS (2010) Defining minimal disease activity in psoriatic arthritis: a proposed objective target for treatment. Ann Rheum Dis 69(1):48–53
Rohekar S et al (2015) 2014 Update of the Canadian Rheumatology Association/spondyloarthritis research consortium of Canada treatment recommendations for the management of spondyloarthritis. Part I: principles of the management of spondyloarthritis in Canada. J Rheumatol 42(4):654–64
Freites Nuñez D et al (2021) Factors associated with health-related quality of life in psoriatic arthritis patients: A longitudinal analysis. Rheumatol Ther 8(3):1341–1354
Al Rayes H et al (2022) Consensus-based recommendations on the diagnosis, referral and clinical management of patients with psoriatic arthritis. Rheumatol Int 42(3):391–401
Coates LC et al (2016) Group for research and assessment of psoriasis and psoriatic arthritis 2015 treatment recommendations for psoriatic arthritis. Arthritis Rheumatol 68(5):1060–1071
Kavanaugh A et al (2020) GRAPPA treatment recommendations: updates and methods. J Rheumatol Suppl 96:41–45
Gossec L et al (2016) European League Against Rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 update. Ann Rheum Dis 75(3):499–510
Coates LC et al (2013) The 2012 BSR and BHPR guideline for the treatment of psoriatic arthritis with biologics. Rheumatology 52(10):1754–1757 (Oxford)
Flint J et al (2016) BSR and BHPR guideline on prescribing drugs in pregnancy and breastfeeding-Part I: standard and biologic disease modifying anti-rheumatic drugs and corticosteroids. Rheumatology 55(9):1693–1697 (Oxford)
Flint J et al (2016) BSR and BHPR guideline on prescribing drugs in pregnancy and breastfeeding—Part I: standard and biologic disease modifying anti-rheumatic drugs and corticosteroids. Rheumatology 55(9):1693–1697
Horton JN (1980) Nominal group technique. A method of decision-making by committee. Anaesthesia 35(8):811–4
Ogdie A, Coates LC, Gladman DD (2020) Treatment guidelines in psoriatic arthritis. Rheumatology 59(Suppl 1):i37–i46 (Oxford)
Sarzi-Puttini P et al (2001) The role of NSAIDs in psoriatic arthritis: evidence from a controlled study with nimesulide. Clin Exp Rheumatol 19(1 Suppl 22):S17-20
Kingsley GH et al (2012) A randomized placebo-controlled trial of methotrexate in psoriatic arthritis. Rheumatology 51(8):1368–1377 (Oxford)
McInnes IB et al (2014) Efficacy and safety of secukinumab, a fully human anti-interleukin-17A monoclonal antibody, in patients with moderate-to-severe psoriatic arthritis: a 24-week, randomised, double-blind, placebo-controlled, phase II proof-of-concept trial. Ann Rheum Dis 73(2):349–356
Mease PJ et al (2017) Ixekizumab, an interleukin-17A specific monoclonal antibody, for the treatment of biologic-naive patients with active psoriatic arthritis: results from the 24-week randomised, double-blind, placebo-controlled and active (adalimumab)-controlled period of the phase III trial SPIRIT-P1. Ann Rheum Dis 76(1):79–87
Deodhar A et al (2018) Efficacy and safety of guselkumab in patients with active psoriatic arthritis: a randomised, double-blind, placebo-controlled, phase 2 study. Lancet 391(10136):2213–2224
Kristensen LE et al (2022) Efficacy and safety of risankizumab for active psoriatic arthritis: 24-week results from the randomised, double-blind, phase 3 KEEPsAKE 1 trial. Ann Rheum Dis 81(2):225–231
Gladman DD et al (2007) Adalimumab for long-term treatment of psoriatic arthritis: forty-eight week data from the adalimumab effectiveness in psoriatic arthritis trial. Arthritis Rheum 56(2):476–488
Paik J, Deeks ED (2019) Tofacitinib: A Review in Psoriatic Arthritis. Drugs 79(6):655–663
Mease PJ et al (2021) Upadacitinib in Patients with Psoriatic Arthritis and Inadequate Response to Biologics: 56-Week Data from the Randomized Controlled Phase 3 SELECT-PsA 2 Study. Rheumatol Ther 8(2):903–919
Mourad A, Gniadecki R (2020) Treatment of Dactylitis and Enthesitis in Psoriatic Arthritis with Biologic Agents: A Systematic Review and Metaanalysis. J Rheumatol 47(1):59–65
Schafer PH et al (2010) Apremilast, a cAMP phosphodiesterase-4 inhibitor, demonstrates anti-inflammatory activity in vitro and in a model of psoriasis. Br J Pharmacol 159(4):842–855
Gladman DD, Ritchlin C (2021) Treatment of psoriatic arthritis. In: Sieper J, editor. UpToDate [Internet]. [cited 2021 Dec 24]. Available from: https://www.uptodate.com/contents/treatment-of-psoriatic-arthritis?search=psoriatic%20arthritis%20treatment&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
Mease PJ (2011) Measures of psoriatic arthritis: Tender and Swollen Joint Assessment, Psoriasis Area and Severity Index (PASI), Nail Psoriasis Severity Index (NAPSI), Modified Nail Psoriasis Severity Index (mNAPSI), Mander/Newcastle Enthesitis Index (MEI), Leeds Enthesitis Index (LEI), Spondyloarthritis Research Consortium of Canada (SPARCC), Maastricht Ankylosing Spondylitis Enthesis Score (MASES), Leeds Dactylitis Index (LDI), Patient Global for Psoriatic Arthritis, Dermatology Life Quality Index (DLQI), Psoriatic Arthritis Quality of Life (PsAQOL), Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F), Psoriatic Arthritis Response Criteria (PsARC), Psoriatic Arthritis Joint Activity Index (PsAJAI), Disease Activity in Psoriatic Arthritis (DAPSA), and Composite Psoriatic Disease Activity Index (CPDAI). Arthritis Care Res 63(Suppl 11):S64-85 (Hoboken)
van der Heijde D et al (2017) 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis 76(6):978–991
Carneiro S et al (2021) Brazilian Society of Rheumatology 2020 guidelines for psoriatic arthritis. Adv Rheumatol 61(1):69
Machado PM, Landewé R, Heijde DV (2018) Ankylosing Spondylitis Disease Activity Score (ASDAS): 2018 update of the nomenclature for disease activity states. Ann Rheum Dis 77(10):1539–1540
Grappanetwork.org (2022) Home. [online] Available at: <https://www.grappanetwork.org/>. Accessed 12 Jan 2022
Braun J et al (2003) International ASAS consensus statement for the use of anti-tumour necrosis factor agents in patients with ankylosing spondylitis. Ann Rheum Dis 62(9):817–824
Holroyd CR et al (2019) The British Society for Rheumatology biologic DMARD safety guidelines in inflammatory arthritis-Executive summary. Rheumatology 58(2):220–226 (Oxford)
Thrastardottir T, Love TJ (2018) Infections and the risk of psoriatic arthritis among psoriasis patients: a systematic review. Rheumatol Int 38(8):1385–1397
Haddad A et al (2016) The incidence and predictors of infection in psoriasis and psoriatic arthritis: results from longitudinal observational cohorts. J Rheumatol 43(2):362–366
Cantini F et al (2014) HBV Reactivation in Patients Treated with Antitumor Necrosis Factor-Alpha (TNF-α) Agents for Rheumatic and Dermatologic Conditions: A Systematic Review and Meta-Analysis. Int J Rheumatol 2014:926836
National Institute for Health and Care Excellence (NICE) (2016) HIV testing: increasing uptake among people who may have undiagnosed HIV. NICE Guideline 60. London: NICE. https://www.nice.org.uk/guidance/ng60. (May 2018, date last accessed)
Wolk R et al (2017) Effect of tofacitinib on lipid levels and lipid-related parameters in patients with moderate to severe psoriasis. J Clin Lipidol 11(5):1243–1256
Tubach F et al (2009) Risk of tuberculosis is higher with anti-tumor necrosis factor monoclonal antibody therapy than with soluble tumor necrosis factor receptor therapy: The three-year prospective French Research Axed on Tolerance of Biotherapies registry. Arthritis Rheum 60(7):1884–1894
Maiga M et al (2012) Risk of tuberculosis reactivation with tofacitinib (CP-690550). J Infect Dis 205(11):1705–1708
Bélard E et al (2011) Prednisolone treatment affects the performance of the QuantiFERON gold in-tube test and the tuberculin skin test in patients with autoimmune disorders screened for latent tuberculosis infection. Inflamm Bowel Dis 17(11):2340–2349
Ruan Q et al (2016) Screening of latent tuberculosis infection by interferon-γ release assays in rheumatic patients: a systemic review and meta-analysis. Clin Rheumatol 35(2):417–425
Sterling TR et al (2020) Guidelines for the Treatment of Latent Tuberculosis Infection: Recommendations from the National Tuberculosis Controllers Association and CDC, 2020. MMWR Recomm Rep 69(1):1–11
Antoni C et al (2005) Infliximab improves signs and symptoms of psoriatic arthritis: results of the IMPACT 2 trial. Ann Rheum Dis 64(8):1150–1157
Dressler C et al (2019) Efficacy and safety of systemic treatments in psoriatic arthritis: a systematic review, meta-analysis and GRADE evaluation. J Eur Acad Dermatol Venereol 33(7):1249–1260
Mease P (2020) Enthesitis in psoriatic arthritis (Part 3): clinical assessment and management. Rheumatology 59(Supplement_1):i21–i28
Mease PJ et al (2021) Comparative effectiveness of guselkumab in psoriatic arthritis: results from systematic literature review and network meta-analysis. Rheumatology 60(5):2109–2121 (Oxford)
McInnes IB et al (2019) Efficacy of ustekinumab in biologic-naïve patients with psoriatic arthritis by prior treatment exposure and disease duration: data from PSUMMIT 1 and PSUMMIT 2. RMD Open 5(2):e000990
AbbVie Inc (2015) HUMIRA subcutaneous injection, adalimumab subcutaneous injection Prescribing Information. North Chicago, IL. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/125057s410lbl.pdf
UCB Inc (2019) CIMZIA subcutaneous injection, Certolizumab pegol subcutaneous injection Prescribing Information. Smyrna, GA. Available at: https://www.cimzia.com/themes/custom/cimzia/docs/CIMZIA_full_prescribing_information.pdf
Amgen Inc (2015) ENBREL subcutaneous injection solution, etanercept subcutaneous injection solution Prescribing Information. Thousand Oaks, CA. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/103795s5503lbl.pdf
Janssen Biotech Inc ( 2011) REMICADE lyophilized concentrate for intravenous injection, infliximab lyophilized concentrate for intravenous injection prescribing information. Horsham, PA. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/103772s5359lbl.pdf
Novartis Pharmaceuticals Corporation (2018) COSENTYX subcutaneous injection, secukinumab subcutaneous injection Prescribing Information. East Hanover, NJ. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/125504s001s002lbl.pdf
Eli Lilly and Company ( 2019) TALTZ subcutaneous injection, ixekizumab subcutaneous injection Prescribing Information. Indianapolis, IN. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/125521s016lbl.pdf
Janssen Biotech Inc (2019) STELARA subcutaneous injection, intravenous injection, ustekinumab subcutaneous injection, intravenous injection Prescribing Information. Horsham, PA. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/761044lbl.pdf
Janssen Biotech Inc (2019) TREMFYA subcutaneous injection, guselkumab subcutaneous injection Prescribing Information. Horsham, PA. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761061s001lbl.pdf
Amgen Inc (2014) OTEZLA oral tablets, apremilast Prescribing Information. Thousand Oaks, CA. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/205437s011lbl.pdf
Menter A et al (2019) Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol 80(4):1029–1072
Jadon DR, Kavanaugh A, Leung YY (2022) Clinical controversies in psoriatic disease: the use of IL-17i/IL-23i versus TNFi as first-line advanced therapy in psoriatic arthritis. J Rheumatol 49(6 Suppl 1):26–31. https://doi.org/10.3899/jrheum.211325
Ayan G et al (2023) Pharmacologic treatment strategies in psoriatic arthritis. Clin Ther 45(9):826–840
Baraliakos X et al (2021) Secukinumab in patients with psoriatic arthritis and axial manifestations: results from the double-blind, randomised, phase 3 MAXIMISE trial. Ann Rheum Dis 80(5):582–590
Moverley A et al (2015) A feasibility study for a randomised controlled trial of treatment withdrawal in psoriatic arthritis (REmoval of treatment for patients in REmission in psoriatic ArThritis (RETREAT (F)). Clin Rheumatol 34(8):1407–1412
Cantini F et al (2008) Frequency and duration of clinical remission in patients with peripheral psoriatic arthritis requiring second-line drugs. Rheumatology 47(6):872–876 (Oxford)
Araujo EG et al (2015) High incidence of disease recurrence after discontinuation of disease-modifying antirheumatic drug treatment in patients with psoriatic arthritis in remission. Ann Rheum Dis 74(4):655–660
Chimenti MS et al (2013) Remission of psoriatic arthritis after etanercept discontinuation: analysis of patients’ clinical characteristics leading to disease relapse. Int J Immunopathol Pharmacol 26(3):833–838
Janta I et al (2015) Comparison between full and tapered dosages of biologic therapies in psoriatic arthritis patients: clinical and ultrasound assessment. Clin Rheumatol 34(5):935–942
Ye W, Tucker LJ, Coates LC (2018) Tapering and discontinuation of biologics in patients with psoriatic arthritis with low disease activity. Drugs 78(16):1705–1715
González-Álvaro I et al (2015) Spanish Rheumatology Society and Hospital Pharmacy Society Consensus on recommendations for biologics optimization in patients with rheumatoid arthritis, ankylosing spondylitis and psoriatic arthritis. Rheumatology 54(7):1200–1209 (Oxford)
Mandl P et al (2015) EULAR recommendations for the use of imaging in the diagnosis and management of spondyloarthritis in clinical practice. Ann Rheum Dis 74(7):1327
Fagerli KM et al (2014) The role of methotrexate co-medication in TNF-inhibitor treatment in patients with psoriatic arthritis: results from 440 patients included in the NOR-DMARD study. Ann Rheum Dis 73(1):132–137
Mease PJ et al (2019) Etanercept and Methotrexate as Monotherapy or in Combination for Psoriatic Arthritis: Primary Results From a Randomized Controlled Phase III Trial. Arthritis Rheumatol 71(7):1112–1124
Glintborg B et al (2013) Clinical response, drug survival, and predictors thereof among 548 patients with psoriatic arthritis who switched tumor necrosis factor α inhibitor therapy: results from the Danish Nationwide DANBIO Registry. Arthritis Rheum 65(5):1213–1223
Berman J et al (2021) AB0551 TREATMENT WITH IXEKIZUMAB FOLLOWING SECUKINUMAB FAILURE IN PATIENTS WITH PSORIATIC ARTHRITIS: REAL-LIFE EXPERIENCE FROM A RESISTANT POPULATION. Ann Rheum Dis 80(Suppl 1):1309–1310
Holroyd CR et al (2018) The British Society for Rheumatology biologic DMARD safety guidelines in inflammatory arthritis. Rheumatology 58(2):e3–e42
Patel S, Kumthekar A (2022) Psoriatic arthritis: the influence of co-morbidities on drug choice. Rheumatol Ther 9(1):49–71. https://doi.org/10.1007/s40744-021-00397-7
Yang K, Oak ASW, Elewski BE (2021) Use of IL-23 inhibitors for the treatment of plaque psoriasis and psoriatic arthritis: a comprehensive review. Am J Clin Dermatol 22(2):173–192
Mease PJ (2014) Apremilast: a phosphodiesterase 4 inhibitor for the treatment of psoriatic arthritis. Rheumatol Ther 1(1):1–20
Gladman DD et al (2018) Therapeutic benefit of apremilast on enthesitis and dactylitis in patients with psoriatic arthritis: a pooled analysis of the PALACE 1–3 studies. RMD Open 4(1):e000669
Nash P et al (2018) Early and sustained efficacy with apremilast monotherapy in biological-naïve patients with psoriatic arthritis: a phase IIIB, randomised controlled trial (ACTIVE). Ann Rheum Dis 77(5):690–698
Wells AF et al (2018) Apremilast monotherapy in DMARD-naive psoriatic arthritis patients: results of the randomized, placebo-controlled PALACE 4 trial. Rheumatology 57(7):1253–1263 (Oxford)
Kavanaugh A et al (2019) Long-term experience with apremilast in patients with psoriatic arthritis: 5-year results from a PALACE 1–3 pooled analysis. Arthritis Res Ther 21(1):118
National Institute for Health and Care Excellence (NICE) (2016) Tuberculosis Clinical Guideline. London: NICE. Updated 2019. https://www.nice.org.uk/guidance/ng33/resources/tuberculosis-pdf-1837390683589 (Feb 2022, date last accessed)
British Thoracic Society Standards of Care Committee (2005) BTS recommendations for assessing risk and for managing Mycobacterium tuberculosis infection and disease in patients due to start anti-TNF-alpha treatment. Thorax 60(10):800–805. https://doi.org/10.1136/thx.2005.046797
Patel S, Kumthekar A (2022) Psoriatic arthritis: the influence of co-morbidities on drug choice. Rheumatol Ther 9(1):49–71
Askling J et al (2005) Risk and case characteristics of tuberculosis in rheumatoid arthritis associated with tumor necrosis factor antagonists in Sweden. Arthritis Rheum 52(7):1986–1992
Dixon WG et al (2010) Drug-specific risk of tuberculosis in patients with rheumatoid arthritis treated with anti-TNF therapy: results from the British Society for Rheumatology Biologics Register (BSRBR). Ann Rheum Dis 69(3):522–528
Fonseca JE et al (2006) Tuberculosis in rheumatic patients treated with tumour necrosis factor alpha antagonists: the Portuguese experience. Acta Reumatol Port 31(3):247–253
Gómez-Reino JJ et al (2003) Treatment of rheumatoid arthritis with tumor necrosis factor inhibitors may predispose to significant increase in tuberculosis risk: a multicenter active-surveillance report. Arthritis Rheum 48(8):2122–2127
Keane J et al (2001) Tuberculosis associated with infliximab, a tumor necrosis factor alpha-neutralizing agent. N Engl J Med 345(15):1098–1104
Nast A et al (2017) European S3-Guideline on the systemic treatment of psoriasis vulgaris - Update Apremilast and Secukinumab - EDF in cooperation with EADV and IPC. J Eur Acad Dermatol Venereol 31(12):1951–1963
Evangelatos G et al (2020) Tuberculosis and targeted synthetic or biologic DMARDs, beyond tumor necrosis factor inhibitors. Ther Adv Musculoskelet Dis 12:1759720X20930116
Lee YH, Bae SC, Song GG (2013) Hepatitis B virus (HBV) reactivation in rheumatic patients with hepatitis core antigen (HBV occult carriers) undergoing anti-tumor necrosis factor therapy. Clin Exp Rheumatol 31(1):118–121
Lee YH, Bae SC, Song GG (2013) Hepatitis B virus reactivation in HBsAg-positive patients with rheumatic diseases undergoing anti-tumor necrosis factor therapy or DMARDs. Int J Rheum Dis 16(5):527–531
Pérez-Alvarez R et al (2011) Hepatitis B virus (HBV) reactivation in patients receiving tumor necrosis factor (TNF)-targeted therapy: analysis of 257 cases. Medicine 90(6):359–371 (Baltimore)
Urata Y et al (2011) Prevalence of reactivation of hepatitis B virus replication in rheumatoid arthritis patients. Mod Rheumatol 21(1):16–23
Chen YM et al (2015) A comparison of safety profiles of tumour necrosis factor α inhibitors and rituximab therapy in patients with rheumatoid arthritis and chronic hepatitis C. Ann Rheum Dis 74(3):626–627
EASL clinical practice guidelines (2012) Management of chronic hepatitis B virus infection. J Hepatol 57(1):167–185
Reddy KR et al (2015) American Gastroenterological Association Institute guideline on the prevention and treatment of hepatitis B virus reactivation during immunosuppressive drug therapy. Gastroenterology 148(1):215–9; quiz e16–7
Chiu HY et al (2013) The safety profile of ustekinumab in the treatment of patients with psoriasis and concurrent hepatitis B or C. Br J Dermatol 169(6):1295–1303
Armstrong AW (2020) Treatment selection for moderate to severe plaque psoriasis in special populations. UpToDate. Retrieved February 11, 2022, from. https://www.uptodate.com/contents/treatment-selection-for-moderate-to-severe-plaque-psoriasis-in-special-populations?source=history_widget
Akiyama S, Cotter TG, Sakuraba A (2021) Risk of hepatitis B virus reactivation in patients with autoimmune diseases undergoing non-tumor necrosis factor-targeted biologics. World J Gastroenterol 27(19):2312–2324
Duncan JR, Orlowski TJ, Elewski BE (2019) Safety of guselkumab in hepatitis B virus infection. Dermatol Online J 25(10):13030/qt47h636rx
Iannone F et al (2014) Safety of etanercept and methotrexate in patients with rheumatoid arthritis and hepatitis C virus infection: a multicenter randomized clinical trial. J Rheumatol 41(2):286–292
Costa L et al (2014) Long-term safety of anti-TNF-α in PsA patients with concomitant HCV infection: a retrospective observational multicenter study on 15 patients. Clin Rheumatol 33(2):273–276
Temel T et al (2015) The long-term effects of anti-TNF-α agents on patients with chronic viral hepatitis C and B infections. Int J Rheum Dis 18(1):40–45
Cavazzana I et al (2008) Treatment with etanercept in six patients with chronic hepatitis C infection and systemic autoimmune diseases. Autoimmun Rev 8(2):104–106
Pappas DA et al (2019) Therapy with biologic agents after diagnosis of solid malignancies: results from the corrona registry. J Rheumatol 46(11):1438–1444
Nast A et al (2021) EuroGuiDerm Guideline on the systemic treatment of Psoriasis vulgaris - Part 2: specific clinical and comorbid situations. J Eur Acad Dermatol Venereol 35(2):281–317
Smith CH et al (2017) British Association of Dermatologists guidelines for biologic therapy for psoriasis 2017. Br J Dermatol 177(3):628–636
Álvaro-Gracia JM et al (2021) Update on the safety profile of tofacitinib in rheumatoid arthritis from clinical trials to real-world studies: a narrative review. Rheumatol Ther 8(1):17–40
Havrdová E et al (2016) Activity of secukinumab, an anti-IL-17A antibody, on brain lesions in RRMS: results from a randomized, proof-of-concept study. J Neurol 263(7):1287–1295
van Vollenhoven RF et al (2018) Efficacy and safety of ustekinumab, an IL-12 and IL-23 inhibitor, in patients with active systemic lupus erythematosus: results of a multicentre, double-blind, phase 2, randomised, controlled study. Lancet 392(10155):1330–1339
Micheroli R et al (2017) Impact of obesity on the response to tumor necrosis factor inhibitors in axial spondyloarthritis. Arthritis Res Ther 19(1):164
Fujino S et al (2003) Increased expression of interleukin 17 in inflammatory bowel disease. Gut 52(1):65–70
Clowse ME et al (2017) Minimal to no transfer of certolizumab pegol into breast milk: results from CRADLE, a prospective, postmarketing, multicentre, pharmacokinetic study. Ann Rheum Dis 76(11):1890–1896
Mariette X et al (2018) Lack of placental transfer of certolizumab pegol during pregnancy: results from CRIB, a prospective, postmarketing, pharmacokinetic study. Ann Rheum Dis 77(2):228–233
Ringold S et al (2019) 2019 American College of Rheumatology/Arthritis Foundation guideline for the treatment of juvenile idiopathic arthritis: therapeutic approaches for non-systemic polyarthritis, sacroiliitis, and enthesitis. Arthritis Care Res 71(6):717–734 (Hoboken)
Huemer C et al (2002) Patterns of joint involvement at onset differentiate oligoarticular juvenile psoriatic arthritis from pauciarticular juvenile rheumatoid arthritis. J Rheumatol 29(7):1531–1535
Lewkowicz D, Gottlieb AB (2004) Pediatric psoriasis and psoriatic arthritis. Dermatol Ther 17(5):364–375
Osier E et al (2017) Pediatric psoriasis comorbidity screening guidelines. JAMA Dermatol 153(7):698–704
Menter A et al (2020) Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis in pediatric patients. J Am Acad Dermatol 82(1):161–201
Guzman J et al (2015) The outcomes of juvenile idiopathic arthritis in children managed with contemporary treatments: results from the ReACCh-Out cohort. Ann Rheum Dis 74(10):1854–1860
Sobel RE et al (2014) Safety of celecoxib and nonselective nonsteroidal anti-inflammatory drugs in juvenile idiopathic arthritis: results of the Phase 4 registry. Pediatr Rheumatol Online J 12:29
van Rossum MA et al (2007) Long-term outcome of juvenile idiopathic arthritis following a placebo-controlled trial: sustained benefits of early sulfasalazine treatment. Ann Rheum Dis 66(11):1518–1524
Ruperto N et al (2021) Tofacitinib in juvenile idiopathic arthritis: a double-blind, placebo-controlled, withdrawal phase 3 randomised trial. Lancet 398(10315):1984–1996
Ruperto N et al (2021) LB0004 efficacy and safety of secukinumab in enthesitis-related arthritis and juvenile psoriatic arthritis: primary results from a randomised, double-blind, placebo-controlled, treatment withdrawal, phase 3 study (junipera). Ann Rheum Dis 80(Suppl 1):201–202
van der Heijde D et al (2019) Efficacy and safety of upadacitinib in patients with active ankylosing spondylitis (SELECT-AXIS 1): a multicentre, randomised, double-blind, placebo-controlled, phase 2/3 trial. Lancet 394(10214):2108–2117
Heijstek MW et al (2013) Effects of the live attenuated measles-mumps-rubella booster vaccination on disease activity in patients with juvenile idiopathic arthritis: a randomized trial. JAMA 309(23):2449–2456
De Felice KM, Kane S (2021) Safety of anti-TNF agents in pregnancy. J Allergy Clin Immunol 148(3):661–667
Acknowledgements
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
Sponsorship for this project and Rapid Service Fee were funded by the Ministry of Health, Riyadh, Kingdom of Saudi Arabia.
Author information
Authors and Affiliations
Contributions
HM, AJ, and ME contributed to conceptualization, and RB drafted the methodology. All authors contributed to the writing of the draft content related to their section, reviewed compiled drafts, and approved the final version for publication.
Corresponding author
Ethics declarations
Compliance with ethical standards
This article is based on previously published papers and on the results from consensus workshops and does not contain any new clinical studies with human participants or animals performed by any of the authors.
Medical writing, editorial, and other assistance
Medical writing and editorial assistance in the preparation of this article was provided by Sahar Shami, Lina Fakih, and Lynn Hajjar of Itkan Consulting Group. Support for this assistance was funded by Ministry of Health, Riyadh, Kingdom of Saudi Arabia.
Competing interests
All authors declare no competing or financial interests regarding the publications of these recommendations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al-Homood, I.A., Al Ghanim, N., Fatani, M.I.A. et al. The Saudi consensus recommendations for the management of psoriatic arthritis (2023). Clin Rheumatol 43, 879–894 (2024). https://doi.org/10.1007/s10067-024-06867-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-024-06867-x