Abstract
Objectives
Fractal analysis is a mathematical method used for the calculation of bone trabeculation and lacunarity. This study aims to evaluate the relationship between resonance frequency analysis (RFA) and fractal dimension (FD) of peri-implant bone to determine the preload stability of implants.
Materials and methods
In this study, the results of the fractal analysis calculated from the resonance frequency analysis results taken in the 3rd month of the patients who underwent 2-stage implant by the same doctor and the radiographs taken in the same session were evaluated. A hundred implants in 20 patients were applied in this study. The implant stability quotient (ISQ) values of the implants and fractal dimension values of the peri-implant bone were calculated.
Results
The findings showed that the ISQ1 (p = 0.008), ISQ2 (p = 0.038), ROI2 (p = 0.013), and ROI3 (p < 0.001) values were statistically significantly higher in men than women. The ISQ1 (p = 0.003), ISQ2 (p = 0.013), ROI1 (p = 0.011), and ROI3 (p < 0.001) of the mandible were statistically higher than the maxilla. The fractal dimension cut-off value to assess prosthetic loading was found 1.198.
Conclusion
Fractal analysis is a non-invasive method that can be used in conjunction with clinical examination in the prosthetic loading decision of implants. It is a valuable parameter that can be used without the need for an extra device when it is necessary to reduce the clinical study time.
Clinical relevance
Calculating the fractal dimension of the peri-implant bone is a practical, economical, and applicable method for clinicians. FD calculated from panoramic radiographs used for diagnosis in routine treatments in clinics where access to the necessary devices for ISQ measurement is not available will contribute to clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Objectives
Dental implants are commonly preferred treatment modalities for tooth loss as great alternative anchorage units for prosthetic crowns, bridges, and removable prostheses. Implants can be placed using a one-stage or two-stage surgery. Irrespective of the procedure used, before implant placement, a recovery time of 3–6 months is recommended [1, 2].
Osseointegration has a key role in the prosthetic loading of implants and histological analysis is the gold standard to confirm it. However, it cannot be used as it is an invasive method. Also, evaluation of the peri-implant bone is achieved using various radiographic techniques [3]. Resonance frequency analysis (RFA) is a clinically valuable diagnostic tool that demonstrates implant stability and is used to assess the osseointegration of implants in dental implantology. A small metal rod is placed into the implant and the device produces magnetic pulses transmitted through this metal bar to perform RFA on the inserted implant. This metal rod’s degree of vibration is reported as its resonance frequency and gives a quantitative outcome for the implant stability [4, 5]. RFA is easy to use and is reliable with which method to evaluate the osseointegration of dental implants before prosthetic loading [6].
Fractal analysis (FA) is a mathematical method that is used to calculate the complexity of irregular and complex structures. Mandelbrot was the first person to use the term “fractal” to describe complex geometric structures [7]. The complexity of irregular objects may be represented by fractal dimension (FD) as a quantitative outcome [8]. In the literature, it is stated that the trabecular bone microarchitecture can be evaluated using fractal analysis on digital radiographic images [9]. FA on digital radiographs is not affected by alterations of exposure parameters or patient positions [10, 11]. In standardized dental radiographs, fractal analysis can be used to detect pathological changes in the bone or to evaluate peri-implant bone[8].
The World Health Organization declared a pandemic in March 2020 due to SARS CoV-2, which causes COVID-19 disease and, is transmitted through person-to-person contact and direct contact with respiratory droplets. This situation has led to strict precautions in all countries around the world and has considerably affected the clinical practice of dentistry. In the White Paper published by Rutkowski et al., the points to be considered during surgical procedures to reduce aerosols are explained [12].
Alternative methods have been considered to reduce aerosol in the clinical setting and reduce cross-contamination during the COVID-19 pandemic. The authors aimed to use an alternative method to RFA, which uses extra parts to reduce the time that the patient stays in the chair after implant surgery and to reduce the risk of cross-contamination. Previous studies have shown the use of fractal analysis for the evaluation of peri-implant tissues. Some of these studies compared fractal dimensions with RFA values. However, no study has tested the reliability of the fractal dimension of the peri-implant bone as a diagnostic tool. This study aims to evaluate the usability of fractal dimension in the peri-implant bone as a diagnostic test before prosthetic loading.
Materials and methods
Patient selection
This study included 20 patients with 100 implants. All patients applied to Nuh Naci Yazgan University Faculty of Dentistry between January 2020 and November 2020 with the complaint of a missing tooth. This study was approved by the Ethics Boards and Commissions of Nuh Naci Yazgan University, Kayseri, Turkey (2020/18). The inclusion and exclusion criteria and the allocation process of patients are summarized in Fig. 1.
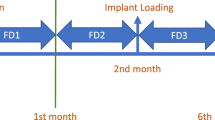
Surgical protocol and resonance frequency analysis
The two-stage implant surgery was used. At least 6 weeks after extraction of the tooth, bone-level implants (Implance, AGS Medical, Trabzon, Turkey) were installed. The implant lengths ranged from 8 to 12 mm and diameters ranged from 3.75 to 4.8 mm. The flap was closed primarily. A healing cap was inserted 3 months after implant surgery. The panoramic film was taken for control in the same session.
The RFA using the Osstell ISQ device (Osstell AB, Sampgatan, Goteborg, Sweden) technique was administered when the implant was uncovered. All RFA measurements were performed by the same surgeon who placed the implants. RFA measurements were recorded as the implant stability quotient (ISQ). RFA results will be given as ISQ in the continuation of the article. ISQ1 represents the average of the measurements taken in both the mesiodistal and distomesial directions of implants, while ISQ2 is the mean of the measurements performed in both the buccolingual and linguobuccal directions of implants. The measurements were registered numerically by the radiographs (Fig. 2) [13].
(A) Representative image showing the Osstell device operating with magnetic resonance and the measurement screen; (B) placement of measuring posts; (C) measuring the mesiodistal direction; (D) measuring the buccolingual direction [13]
Radiographic examination and evaluation
All digital panoramic images were obtained using the same machine (KaVO OP 3D Pro, PaloDEx Group Oy, Tuusula, Finland). Exposure parameters were standardized as 66–75 kVp, 10–14 mA, 16 s for all images. All radiographs were taken as the reference manual description. The Frankfort horizontal plane was parallel and the sagittal plane was perpendicular to the floor.
Fractal dimension calculation
For the fractal analysis, three regions of interest (ROIs) were determined. The average mesial and distal peri-implant bone measurements were calculated for the ROIs. Three ROIs were chosen from the peri-implant trabecular bone: adjacent to the neck (ROI1), the middle part (ROI2), and the apical third (ROI3) of the implant, a square of 33 × 33 pixels. All panoramic images were evaluated with the help of ImageJ version 1.3 software (National Institutes of Health, Bethesda, MD, USA, https://imagej.nih.gov/ij/download.html) in a Dell Precision T5400 workstation (Dell, TX, USA), with a 32-in. Dell liquid crystal display (LCD) screen with a resolution of 1280 × 1024 pixels in a darkroom. Fractal dimensions were evaluated by a dentomaxillofacial radiologist who did not know the patients’ history or ISQ values. ROI1 represents the average fractal dimension calculated from the mesial and distal from the coronal third of the peri-implant bone, ROI2 represents the average fractal dimension calculated from the mesial and distal from the middle third of the peri-implant bone and ROI3 represents the average fractal dimension calculated from the mesial and distal from the apical third of the peri-implant bone.
The box-counting method defined in 1999 by White and Rudolph [14] was used while calculating the fractal dimension. All digital panoramic images are saved as 8-bit. After the selection of ROI, the image was duplicated. Then, for the density correction, it was blurred with a Gaussian filter. The resulting image was subtracted from the original image and 128 grey value was added to each pixel location. Then, the image was made binary by thresholding on a brightness value of 128. Afterwards, the image was eroded, dilated, and skeletonized. The “box-counting” algorithm of the software was performed. The image was divided into squares of 2, 3, 4, 6, 8, 12, 16, 32, and 64 sized pixels. The squares, including the trabeculae and total number of squares, were calculated for each different sized pixel. A logarithmic scale graphic of the acquired values was plotted. The slope of the line, which was aligned to the plotted points on the graphic gave the fractal dimension value (Fig. 3).
Statistical analysis
The sample size was calculated with the G Power 3.1.9 program [15]. When the effect size was determined as 0.3, α = 0.05, and power as 0.90, the required minimum size of a sample was 88 implants.
Statistical analyses were performed using SPSS 21.0 (Chicago, IL, USA) and Turcosa software (Turcosa Analytics Ltf Co. Turkey, www.turcosa.com.tr). Descriptive statistics were performed. The normality of the data was assessed by the Shapiro–Wilk normality test and Q-Q graphs. The Mann–Whitney U test was used for the comparison of non-parametric variables between independent paired groups. To evaluate any possible correlations between ISQ1, ISQ2, ROI1, ROI2, and ROI3, Spearman’s correlation was used.
The receiver operating characteristic (ROC) graphs are curves formed by points at certain threshold values on the x-axis (1-selectivity) and the y-axis (sensitivity). The large area under the ROC curve also indicates that the diagnostic test makes good measurements [16]. The area under the curve (AUC) was calculated by ROC analysis. Fractal dimension diagnosis percentages were calculated by finding the cut-off values. A statistical significance level was considered as α < 0.05.
Results
In this study, the files of the 29 patients were analyzed retrospectively. The inclusion and exclusion criteria were applied and 100 implants from 20 patients were allocated. Of these 20 patients, 9 were male and 11 were female. The patients were at least 34 years old, with a maximum age 70 and a mean of 53 ± 10 years old.
There was no significant difference between the ISQ1, ISQ2, ROI1, ROI2, and ROI3 groups for age (p = 0.53). Fifty-seven implants were placed in the mandible and 43 were placed in the maxilla. ISQ1 (p = 0.008), ISQ2 (p = 0.038), ROI2 (p = 0.013), and ROI3 (p < 0.001) values were found to be significantly higher in males than females (Table 1). The ROI1 (p = 0.091) value did not show a significant difference between women and men.
In the comparison between the jaws, ISQ1 (p = 0.003), ISQ2 (p = 0.013), ROI1 (p = 0.011), and ROI3 (p < 0.001) values were found to be significantly higher in the mandible than in the maxilla (Table 2). The ROI2 (p = 0.209) value did not show a significant difference between maxilla and mandible.
There was a very strong, positive, and statistically significant correlation between ISQ1 and ROI1 (r: 0.6692, p < 0.001) and between ISQ1 and ROI2 (r: 0.6352, p < 0.001). There was a weak, positive, and statistically significant correlation between ISQ1 and ROI3 (r: 0.3696, p < 0.001) (Fig. 4).
Between ISQ2 and ROI1 (r: 0.6529, p < 0.001) and between ISQ2 and ROI2 (r: 0.6261, p < 0.001), there was a very strong, positive, and statistically significant correlation. There was a weak, positive, and statistically significant correlation between ISQ2 and ROI3 (r: 0.3614, p < 0.001) (Fig. 4).
ROC analysis results
As a result of the ROC analysis, a cut-off value of 1.198 was obtained, with a sensitivity of 0.93 and a specificity of 0.167 for the loading decision of the implant. When the area under the ROC curve was examined, it was seen that the 0.92 (z = 11.58; p < 0.001) area was statistically significant (Fig. 5; Table 3).
Discussion
The aim of this study is two-fold. The first aim of the study is the comparison of FD values of the peri-implant bone regions with the RFA values of the same implant and to evaluate its clinical usefulness, while the second aim is to determine a cut-off value for FD according to the stability of implants.
In this research, fractal analysis has been chosen as an alternative diagnostic method as it is a mathematical technique that assesses bone trabeculation, gives objective results, and can be studied outside the mouth. Hayek et al. compared the fractal dimension value of the pre-implant bone with the histological density of the extracted bone block during implant placement. They stated that as the fractal dimension increased, the bone density increased as well [17].
Abdulhameed et al. found that fractal analysis is a cost-effective, non-invasive diagnostic evaluation that has clinical significance in the examination of bone trabeculation in the study they assessed the effects of ultrasonic waves on the healing of peri-implant bone tissue [3]. Kato et al. propose that fractal analysis is a valuable evaluation tool for tracking dental implant stability [10].
In our clinic for following the case, in the case of multiple implants performed for a patient, panoramic radiography is used instead of periapical radiography to lower the radiation dose. Despite the numerical value of the fractal dimension changing in different radiography methods, the correlation in trabeculation will not change, so standardized panoramic films have been used in this study.
Bollen et al. compared FD values at the same ROIs on periapical and panoramic radiographs; they found that fractal dimensions obtained from periapical radiographs were higher than panoramic radiographs [18]. For this reason, the cut-off value, which was determined to be 1.198 in our study, is recommended to be used in panoramic radiographs. In periapical radiographs, this cut-off value will certainly vary.
Our study proceeded with following questions: (1) “Can many clinicians use the fractal dimension for the prosthetic analysis and the cut-off value in the loading decision?” Thus, we aimed to reduce cross-contamination by using less material by reducing the treatment time spent by the patient in the chair.
RFA is a non-invasive method for assessing implant stability and uses values expressed as the implant stability coefficient (ISQ) on a scale of 0 to 100 [19]. The implant stability quotient (ISQ) is a globally standardized method used to calculate implant stability. The clinical range of ISQ is from 55 to 80. Generally, higher values are observed in the mandible than in the maxilla. According to the literature, the ISQ value bigger than 70 is considered as high stability, between 60 and 69 as medium stability, and lower than 60 is considered as low stability. After the bone healing period and implant placement, the ISQ values are expected to be high. The opposite may be the sign of a possible failed implant [20,21,22,23,24,25,26,27,28]. Scarano et al. reported that as the RFA values increased, bone-implant contact also increased [29].
Our study results focused on the peri-implant bone before prosthetic loading. Suer et al. evaluated the FD values of the operating bone area before the implant placement and then examined the RFA after the placement of implants and found a positive correlation between the ISQ and FD values. They suggest that FA is a useful tool for calculating the biomechanical capability of the bone [19]. In a study that allocated 33 patients, Sansare et al. reported an increase in the fractal dimension values measured on panoramic radiographs 3 months after implant placement compared to before [30]. Willing et al. proposed that the peri-implant bone FD values increased for 2 years after placement; they also stated that the fractal dimension values in the peri-implant neck area of the implants could be useful in panoramic radiographs for the follow-up period [31]. Jing Mu et al. found a statistically significant increase in the fractal dimension of the peri-implant bone just before the prosthetic loading of the implants and 12 months after prosthetic loading. This study shows that the increase in bone trabeculation after loading is significant and the fractal analysis can be used as a follow-up tool for the peri-implant bone [32]. One of the limitations of this study is the absence of preoperative, postoperative, and long-follow-up radiographs. In more comprehensive studies, the usability of this analysis method as a diagnostic test in patients with follow-up can be evaluated.
In our study, ISQ1, ISQ2, ROI1, and ROI3 were found to be significantly higher in the mandible than in the maxilla. This result contradicts some studies in the literature. Lee et al. reported that the fractal size of the peri-implant bone obtained from the maxilla did not show a significant relationship with the ISQ values of the same implants. In the same study, they reported a significant correlation between the fractal size of the peri-implant bone in the mandible and the ISQ values [33]. Kulzky et al. reported that the fractal values obtained from the peri-implant bone in the maxilla were significantly higher than in the mandible [4]. We think that the sample size of the studies should be expanded.
In this study, we used ROC curves to evaluate the usability of fractal analysis as a diagnostic test. As a result, we found a cut-off value of 1.198 with a sensitivity of 0.93 and a specificity of 0.167. In these results, the AUC was found to be 0.92. ROC curves show the overall discriminatory power of a diagnostic test. The perfect test has an AUC of 1.0 [34]. As a result of the study, AUC’s value close to 1 shows that fractal analysis can be used as a reliable diagnostic test. Of note, the cut-off value of 1.198 is a value obtained from panoramic radiographs and the fractal size obtained in the periapical film and the panoramic film of the same implant will differ.
The limitation of this study was that the fractal size of the implants in different regions was not examined. Further studies with larger sample sizes are needed to compare regions with different bone densities such as maxilla anterior, maxilla posterior, mandible anterior, and mandible posterior.
Conclusions
Fractal analysis is a non-invasive method that can be used to evaluate osseointegration before prosthetic loading. It is a valuable parameter that can guide the treatment process together with clinical examination when the required device for resonance frequency analysis cannot be reached or when it is necessary to reduce the working time in the mouth. However, there is a need for multicenter studies using different radiography devices and more implants.
References
Miranda Burgos P (2007) On the influence of micro-and macroscopic surface modifications on bone integration of titanium implants. Dissertation, Göteborg University.
Kola MZ, Shah AH, Khalil HS, Rabah AM, Harby NMH, Sabra SA, Raghav D (2015) Surgical templates for dental implant positioning; current knowledge and clinical perspectives. Niger J Surg 21:1–5
Abdulhameed EA, Al-Rawi NH, Uthman AT, Samsudin AR (2018) Bone texture fractal dimension analysis of ultrasound-treated bone around implant site: a double-blind clinical trial. Int J Dent 2018:1–10. https://doi.org/10.1155/2018/2672659
Kulczyk T, Czajka-Jakubowska A, Przystańska A (2018) A comparison between the implant stability quotient and the fractal dimension of alveolar bone at the implant site. Biomed Res Int. https://doi.org/10.1155/2018/4357627
Yoon H-G, Heo S-J, Koak J-Y, Kim S-K, Lee S-YJTjoap, (2011) Effect of bone quality and implant surgical technique on implant stability quotient (ISQ) value. J Adv Prosthodont 3:10–15
Aparicio C, Lang NP, Rangert B (2006) Validity and clinical significance of biomechanical testing of implant/bone interface. Clin Oral Implants Res 17(2):2–7. https://doi.org/10.1111/j.1600-0501.2006.01365.x
Mandelbrot B (1967) How long is the coast of Britain? Statistical self-similarity and fractional dimension. Science 156:636–638. https://doi.org/10.1126/science.156.3775.636
Kış HC, Güleryüz Gürbulak A (2020) Evaluation of the peri-implant bone trabecular microstructure changes in short implants with fractal analysis. Int J Implant Dent 6:1–8
Soylu E, Coşgunarslan A, Çelebi S, Soydan D, Demirbaş AE, Demir O (2021) Fractal analysis as a useful predictor for determining osseointegration of dental implant? A retrospective study. Int J Implant Dent 7:1–8
Kato CN, Barra SG, Tavares NP, Amaral TM, Brasileiro CB, Mesquita RA, Abreu LG (2019) Use of fractal analysis in dental images: a systematic review. Dentomaxillofac Radiol. https://doi.org/10.1259/dmfr.20180457
Zeytinoğlu M, İlhan B, Dündar N, Boyacioğlu HJ (2015) Fractal analysis for the assessment of trabecular peri-implant alveolar bone using panoramic radiographs. Clin Oral Investig 19:519–524
Rutkowski JL, Camm DP, El Chaar E (2020) AAID white paper: Management of the dental implant patient during the COVID-19 pandemic and beyond. J Oral Implantol 46:454–466
Tulyaganov JShAA, Safarov MT, Arslanov OU, Ziyadullaeva NS, Kudratov Sh (2020) Tissue engineering by guided bone regeneration with application of bioglass “bioactive glass” in patients with diabetes for dental implantation. Am J Med Med Sci 10:646–651. https://doi.org/10.5923/j.ajmms.20201009.04
White SC, Rudolph DJ (1999) Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Med, Oral Pathol, Oral Radiol, Endodontol 88:628–635
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191. https://doi.org/10.3758/bf03193146
Bahadır E and Kalender B (2018) [ROC Analizi ile Zung Depresyon Ölçeği Kesme Noktalarının Belirlenmesi.] Adnan Menderes Üniversitesi Sosyal Bilimler Enstitüsü Dergisi 5:137–147. https://doi.org/10.30803/adusobed.407400
Hayek E, Aoun G, Bassit R, Nasseh I (2020) Correlating radiographic fractal analysis at implant recipient sites with primary implant stability: An in vivo preliminary study. Cureus. https://doi.org/10.7759/cureus.6539
Bollen A, Taguchi A, Hujoel P, Hollender L (2001) Fractal dimension on dental radiographs. Dentomaxillofac Radiol 30:270–275
Tolga Suer B, Yaman Z, Buyuksarac B (2016) Correlation of fractal dimension values with implant insertion torque and resonance frequency values at implant recipient sites. Int J Oral Maxillofac Implants 31:55–62
Sennerby L (2013) [Jahre Erfahrung mit der Resonanzfrequenzanalyse.] Implantologie. 21:21–33.
Kokovic V, Jung R, Feloutzis A, Todorovic VS, Jurisic M, Hämmerle CH (2014) Immediate vs. early loading of SLA implants in the posterior mandible: 5-year results of randomized controlled clinical trial. Clin Oral Implants Res 25:114–119
Bornstein MM, Hart CN, Halbritter SA, Morton D, Buser D (2009) Early loading of nonsubmerged titanium implants with a chemically modified sand-blasted and acid-etched surface: 6-month results of a prospective case series study in the posterior mandible focusing on peri-implant crestal bone changes and implant stability quotient (ISQ) values. Clin Implant Dent Relat Res 11:338–347
Baltayan S, Pi-Anfruns J, Aghaloo T, Moy PK (2016) The predictive value of resonance frequency analysis measurements in the surgical placement and loading of endosseous implants. Oral Maxillofac Surg 74:1145–1152
Östman PO, Hellman M, Albrektsson T, Sennerby L (2007) Direct loading of Nobel Direct® and Nobel Perfect® one-piece implants: a 1-year prospective clinical and radiographic study. Clin Oral Implants Res 18:409–418
Rodrigo D, Aracil L, Martin C, Sanz M (2010) Diagnosis of implant stability and its impact on implant survival: a prospective case series study. Clin Oral Implants Res 21:255–261
Pagliani L, Sennerby L, Petersson A, Verrocchi D, Volpe S, Andersson PJ (2013) The relationship between resonance frequency analysis (RFA) and lateral displacement of dental implants: an in vitro study. J Oral Rehabil 40:221–227
Trisi P, Carlesi T, Colagiovanni M, Perfetti G (2010) Implant stability quotient (ISQ) vs direct in vitro measurement of primary stability (micromotion): effect of bone density and insertion torque. J Osteol Biomat 1:141–149
Hicklin SP, Schneebeli E, Chappuis V, Janner SFM, Buser D, Brägger U (2016) Early loading of titanium dental implants with an intra-operatively conditioned hydrophilic implant surface after 21 days of healing. Clin Oral Implants Res 27:875–883
Scarano A, Degidi M, Iezzi G, Petrone G, Piattelli A (2006) Correlation between implant stability quotient and bone-implant contact: a retrospective histological and histomorphometrical study of seven titanium implants retrieved from humans. Clin Implant Dent Relat Res 8:218–222
Sansare K, Singh D, Karjodkar F (2012) Changes in the fractal dimension on pre-and post-implant panoramic radiographs. Oral Radiol 28:15–23
Wilding R, Slabbert J, Kathree H, Owen C, Crombie K, Delport PJ (1995) The use of fractal analysis to reveal remodeling in human alveolar bone following the placement of dental implants. Arch Oral Biol 40:61–72
Mu TJ, Lee DW, Park KH, Moon IS (2013) Changes in the fractal dimension of peri-implant trabecular bone after loading: a retrospective study. J Periodontal Implant Sci 43:209–214
Lee DH, Ku Y, Rhyu IC, Hong JU, Lee CW, Heo MS, Huh KH (2010) A clinical study of alveolar bone quality using the fractal dimension and the implant stability quotient. J Periodontal Implant Sci 40:19–24
Mazıcıoğlu MM, Hatipoğlu N, Öztürk A, Çiçek B, Üstünbaş HB, Kurtoğlu S (2010) Waist circumference and mid− upper arm circumference in evaluation of obesity in children aged between 6 and 17 years. J Clin Res Pediatr Endocrinol 2(4):144–150. https://doi.org/10.4274/jcrpe.v2i4.144
Acknowledgements
We would like to thank the radiology technician and staff of the Nuh Naci Yazgan, University Department of Oral and Maxillofacial Radiology. Also, special thanks to the company Implance (Adel Dental).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in this study were by the ethical standards of the Research Ethical Commission and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required. Nevertheless, consent is obtained from each patient who is treated in the clinic, by informing that the treatment information can be used in scientific research.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Öztürk, K., Kış, H.C. Peri-implant bone microstructural analysis and comparison of resonance frequency analysis before prosthetic placement: a retrospective study. Clin Oral Invest 26, 4967–4975 (2022). https://doi.org/10.1007/s00784-022-04464-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04464-3