Abstract
Study design
We reviewed the available literature systematically without meta-analysis following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Objective
To evaluate contemporary literature on use of spinal diffusion tensor imaging(sDTI) in spinal pathology.
Background
sDTI reveals the location and functional state of critical long tracts and is a potentially useful adjunct in disease management.
Methods
Studies were included if they presented or discussed data from investigative or therapeutic procedures involving sDTI on human subjects in the setting of surgically amenable spinal pathology. Studies were excluded if they were (1) restricted to computational models investigating parameters using data not obtained clinically, (2) about cranial DTI methods, (3) about spinal pathology data not related to surgical management, (4) discussions or overviews of methods/techniques with minimal inclusion of objective experimental or clinical data.
Results
Degenerative pathologies of interest were restricted to either cervical myelopathy (22/29,75.9%) or lumbar spondylosis 7/29,24.1%). Mass-occupying lesions included intradural pathology and discussed preoperative (7/9,77.8%) and intraoperative imaging(2/9,22.2%) as an adjunct to surgery 22.2%. Traumatic pathology focused on spinal cord injury prognosis and severity grading.
Conclusions
sDTI seems useful in surgical decision making and outcome measurements and in establishing clinical prognoses over a wide range of surgical pathologies. Further research is warranted with longer follow-up and larger population sizes in a prospective and controlled protocol.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Spinal surgery encompasses a wide range of pathologies requiring careful preoperative evaluation [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. The spinal cord, the caudal extension of the brain, comprises critical nuclei and tracts in a compact space [49]. Therefore, surgeries treating neural compression secondary to degenerative, traumatic, or mass-occupying lesions necessitate careful consideration of the validity and planning of approaches.
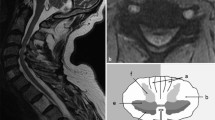
Imaging of the vertebral column, as with all surgical modalities, is a powerful tool in perioperative selection and planning, particularly for localizing critical long tracts [1,2,3,4,5,6,7,8,9,10]. High-resolution magnetic resonance imaging (MRI) of the spine is exceedingly difficult because of the compact anatomy, heterogeneous magnetic environments, and physiological motion of the spinal cord [1,2,3,4,5,6,7,8,9,10]. Advanced sequences have therefore been developed to allow improved resolution [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. Spinal diffusion tensor imaging (sDTI) enables tract characterization and has been applied to prognosis, planning, guidance, and outcomes in patients with surgically amenable degenerative disease [2, 4, 5, 7,8,9,10,11,12,13, 15,16,17,18, 21, 24,25,26,27,28, 30,31,32, 35,36,37,38,39,40, 42], intradural spinal lesions [1, 3, 6, 27, 41, 45,46,47], and traumatic spinal cord injury(SCI) [14, 19, 20, 26, 29, 33, 34, 43, 44]
Methods
We reviewed the available literature systematically without meta-analysis following PRISMA guidelines [48]. We queried the United States National Library of Medicine at the National Institutes of Health PubMed database and common Internet search engines for studies involving investigational or therapeutic applications of sDTI in human subjects. On September 24, 2022, 112 results were identified using the MeSH keywords ‘diffusion tensor imaging,’ ‘diffusion fiber tractography’ and ‘spinal pathology.’ Studies were included if they presented data involving the use of sDTI on human subjects in the setting of surgically amenable spinal pathology and were available in English language non-print formats. Studies were excluded if they were (1) restricted to computational models investigating parameters using data not obtained clinically, (2) about cranial DTI methods, (3) about spinal pathology data not related to surgical management, (4) discussions or overviews of methods/techniques with minimal inclusion of objective experimental or clinical data. Abstracts were analyzed qualitatively and independently by two authors for inclusion or exclusion. There was no funding for this study, and this study was exempt from IRB approval as it was a literature review. This review was not registered. Relevant data from individual studies were extracted and agreed upon for presentation and synthesis by two authors (TS, JK).
Results
A total of 47 studies met criteria and were selected for full review. These studies concentrated on one of three primary pathology categories: degenerative spinal disease (Table 1), neoplasia (Table 2), or spinal trauma (Table 3) using reported data from 2011 through 2021 in case series, case–control and cohort studies (Fig. 1). Reports reviewed ranged from level VI to level II scientific evidence according to the Centre of Evidence-Based Medicine(CEBM) [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]; 29.8% of the studies(14/47) were multivariate [4, 9,10,11,12, 18, 21,22,23, 26, 29,30,31, 36].
Degenerative pathologies included cervical spondylotic myelopathy (22/29,75.9%) and lumbar spondylosis(7/29,24.1) (Table 1), encompassing a total of 1389 individual patients. Degenerative studies concerned preoperative DTI for severity grading of myelopathy or radiculopathy(11/29,37.9%) and interval imaging during surgical procedures, including cervical (11/29,37.9%) and lumbar(2/29,6.9%) posterior column decompression, cervical laminoplasty (2/29,6.9%), lumbosacral percutaneous transforaminal endoscopic discectomy (PTED) (2/29,6.9%), or anterior cervical discectomy and fusion (ACDF) (1/29,3.4%) (Table 1).
Reviewed neoplastic and vascular pathologies included intramedullary tumors (IDIM), gliomas in 47.5% (28/59) and ependymal tumors in 44.1%(26/59), and case reports of diffuse large B cell lymphoma(DLBCL), neurofibroma, teratoma, primitive neuroectodermal tumor(PNET), and vascular malformations(5/59, 8.5%) (Table 2). The use of preoperative sDTI was assessed in 77.8% of reports (7/9) and coregistered neuronavigation using preoperative sDTI in 22.2% (2/9) (Table 2).
Traumatic pathology in the reports reviewed focused on general acute SCI(ASCI) in 67.3% of cases(187/278), ASCI secondary to blunt polytrauma in 21.9% (61/278), and ASCI secondary to tethered spinal cord in 10.8% (30/278) (Table 3). The spinal segments involved were the entire spine in 41.4% (115/278) of cases [20, 33, 34], the subaxial cervical spine in 51.4% (115/278) [14, 19, 26, 29, 43], and the thoracolumbar spine in 7.2% (20/278) [44]. All reports of sDTI studied either severity grading of injury or prognostic implications (Table 3).
Discussion
sDTI provides practical information in the perioperative surgical evaluation of spinal pathology. Nearby tract fibers can be located, and quantitative data allow clinical disease to be evaluated [50]. Fractional anisotropy (FA) provides a scalar value from 0 to 1 denoting the degree to which observed molecules preferentially diffuse across a single axis [50]. In healthy myelinated axons, FA values within a specific area of interest, or voxel, approach 1 as molecules move in a relatively linear fashion within an axon, but injured axons return FA values approaching 0 as molecules diffuse randomly in all directions in the absence of a functional cellular barrier [50]. Similarly, apparent diffusion coefficients (ADC) quantify the degree to which water diffusion across tissues is impeded, presumably because of intact cellular membranes [50]. Both values, along with additional parameters, have been heavily investigated to assess the extent of or changes in tissue injury.
Spinal DTI in degenerative disease
Degenerative spinal disease represents a broad grouping of related conditions and accounts for upwards of 30.1% of public health insurance claims in 2021 in the USA with increasing prevalence [51]. Given the complex multifactorial etiology and the challenge of managing a spectrum of interrelated pathologies, studies have attempted to elucidate disease prognosis and treatment efficacy in spinal spondylosis using objective grading schemes, radiographic evidence, and patient-reported outcome measures (PROMs) [52,53,54]. The literature reviewed showed a significant proportion of reports describing sDTI in prognosis prediction, severity grading, and surgical outcome evaluation in patients with spondylotic myelopathy or radiculopathy [2, 4, 5, 7,8,9,10,11,12,13, 15,16,17,18, 21,22,23,24, 28, 30,31,32, 35,36,37,38,39,40, 42]. A total of 12 cases evaluated sDTI correlations with the severity of cervical spondylytic myelopathy or spinal canal stenosis (Table 1). Among these, 58% (7/12) reported significant associations between FA and the measures investigated, 29%(2/7) of them including multivariate analysis [22, 23]. FA along with ADC correlated significantly with severity of myelopathy as illustrated by Nurick grade, suggesting that clinically significant injury to white matter tracts was detected accurately using sDTI [22, 23]. In the univariate analyses including 338 patients, FA was significantly associated with disease severity, discrimination between myelopathic and normal subjects, and modified or classic Japanese orthopedic association scales(mJOA/JOA) [2, 16, 35, 36, 38]. Additionally, FA, along with axial(AD), radial(RD), and mean diffusion(MD), was associated in all white matter columns at affected levels [5]. One univariate analysis across 129 patients reported no significant relationship between FA or ADC [35] and recovery rate [35], while another including 40 patients [16] reported no association of FA with mJOA. As both of those reports reported associations between said parameters in either JOA [35] or pathology versus normal [16], it is reasonable to conclude that FA and ADC are useful for identifying myelopathy and determining severity, but do not necessarily allow the slope of meaningful recovery to be predicted. Additionally, one univariate [35] and one multivariate [36], provided conflicting results about the usefulness of fiber tract density (FTD), the univariate study showing meaningful correlations of FTD with recovery rate and JOA and the multivariate study reporting no correlation between FTD and mJOA, though FTD was significantly associated with pathology versus normal (Table 1). The usefulness of FTD for identifying the severity or prognosis of myelopathy therefore remains uncertain and is a recommended focus for further investigation.
A total of 14 reports discussed the use of sDTI for assessing operative outcomes in cervical myelopathy [4, 7,8,9,10,11,12, 15, 18, 21, 24, 28, 30, 39, 42]; 11 of those 14 discussed results from posterior decompression with or without fusion (Table 1), seven (64%) including multivariate analyses [4, 9,10,11, 18, 28, 30]. Multivariate studies revealed significant associations between FA and mJOA in 42% of reports (5/12), FA with visual analog scales (VAS) and neck disability index (NDI) in one report and poor outcome as determined by a JOA recovery rate less than 50% in another (Table 1). An additional multivariate study found FTD to be negatively associated with mJOA at the most compressed level across 27 patients [10]. Also, two studies found FA to be correlated with differences in mJOA measured pre- and postoperatively [4, 24]. One univariate study across 15 patients found no associations of FA or MD with pre- versus postoperative mJOA values despite a noted significant improvement in mJOA status post-decompression [15]. In addition to FA and FTD, one univariate study investigated ADC, RD, AD, and MD before and after surgery, with significant findings for all parameters relating to changes in mJOA [42]. Another two multivariate reports queried FA or FA and FTD before and after cervical laminoplasty, with conflicting results [12, 21]. The first study, a prospective cohort across 75 patients, found FA to be an independent predictor of mJOA recovery rate at three and 6 months following surgery [12]. The second study, a case series across 20 patients, found significant associations between poor recovery and FA and reported a decreased FTD as an independent predictor [21]. The remaining study, focusing on DTI and surgically-treated cervical myelopathy, queried parameters relative to ACDF across 30 patients in a univariate fashion using multi-shot high-resolution DTI (msDTI) [39]. The authors reported a significant correlation between pre- and postoperative mJOA and FA values [39]. Considering the foregoing, it can be concluded that FA is likely at minimum to have significant clinical value for evaluating operative outcomes from laminectomy, laminoplasty, or ACDF, which is intuitively valid as those procedures are known to provide clinical benefit,[55, 56] and observed changes would be expected to correlate with radiographic parameters associated with white matter viability.
Of the seven reports that focused on degenerative lumbosacral pathology, three queried the severity grading of radiculopathy [8, 32, 40], two surgical posterior column decompression [13, 37], and two PTED [17, 31], one of which was the only lumbosacral report to include multivariate analysis [31]. All three reports that commented on severity grading described positive associations between FA and ADC and the extent of disease according to PROMs or observed severity of spinal canal or foraminal stenosis (Table 1). Two of the reports [31, 37] discussed significant associations of FA or FA and ADC with improvement in surgical outcome measures and found FA to be an independent predictor of mJOA [31]. The third, a univariate analysis, found FA to correlate significantly with severity of compression at three and 30 days post-intervention, but significance was lost at 90 days [17]. The final study was a case report describing increases of multiple outcome measures along with improvement in FA values following posterior column decompression at one, two and three months post-surgery [13]. Although they were less numerous, studies investigating degenerative lumbosacral disease therefore paralleled those focusing on cervical pathology. One question arising is whether sDTI is clinically necessary in pre- and postoperative assessment, given that all associations are relative to PROM scales as a surrogate for operative efficacy. It is likely that the added costs of performing interval MRI in such patients provides only academic value, which could pave the way for further developments.
Spinal DTI and neoplastic disease and vascular malformations
Of the seven reports discussing the use of sDTI in treating spinal cord neoplasia or vascular malformations (limited to cavernous malformations), three studies were case series [7, 41, 47] with univariate analyses while the remainder comprised reports of 1–4 cases [1, 3, 4, 6, 25, 46]. The level of evidence for such pathologies in these reports was therefore no greater than IV (Table 2). The studies overwhelmingly discussed the use of sDTI for preoperative assessment of lesion resectability (77%,7/9), all such lesions being intramedullary and including all spinal cord segments (Table 2). The three case series with statistical analyses found the method useful for identifying discrete operative plans, one finding a significant association between FA and tensor trace (TRACE) [45]. The remaining two reports described sDTI and pre-defined resection types, grouping the lesions based on the proportion of fibers identified on diffuse tensor tractography (DTT) as piercing or circumventing them [7, 41]. One such study found an association between DTT category and FA and ADC values, suggesting a more objective bridge to operators or radiologists, individually identifying the locations of tracts by image appearance [41]. The other study found sDTI category to be significantly positively and negatively associated, respectively, with distinct intraoperative planes in type 1 (no fibers passing through lesion) and type III (large volume of fibers passing through lesion). Accordingly, most type 1 lesions were amenable to gross total resection while type III lesions were more often managed by subtotal resection or biopsy, although these findings were not statistically significant [27]. Likewise, no significant differences were found between sDTI type and postoperative McCormick grade, neurological improvement, or good functional outcome [27].
Two case reports described preoperative sDTI for intraoperative neuronavigation in the resection of IDIM and IDEM tumors [3, 25]. One reported the successful use of sDTI integrated into an intraoperative virtual reality display for various degrees of resection for an IDIM cervical ependymoma and glioblastoma [3], while the other reported the use of preoperative sDTI combined with intraoperative computed tomography in resecting an IDIM recurrent cervicomedullary subependymoma and an IDEM thoracic spinal neurofibroma [25]. Both reports anecdotally reported good surgical results [3, 25]. The literature about sDTI in spinal neoplasia remains relatively sparse; it could have considerable value in intraoperative navigation and preoperative surgical evaluation, but further investigation is warranted.
Spinal DTI and spinal cord injury
SCI remains a devastating injury resulting in either focal or complete long tract disruption at affected levels with varying severity [57]. Management unfortunately remains largely supportive, medical options being largely academic; surgical options are aimed at decompressing and stabilizing the surrounding mesenchymal columns as indicated to prevent recurring or progressive injury [57]. Accordingly, the reviewed literature concerning sDTI and applications to SCI focused on severity grading of disease and prognosis (Table 3). Studies ranged across all segments of the spinal cord and queried either ASCI of any mechanism [14, 19, 33, 35, 43, 44], ASCI secondary to blunt spinal trauma [26, 39], pediatric SCI [20], or SCI secondary to tethered cord syndrome [33]. All studies were either case series or case–control studies with a single multivariate study querying blunt ASCI (Table 3). The majority(55%,5/9), limited to univariate case series, found significant associations of FA or FA and FTD with severity of injury, as determined by the Acute Spinal Cord Injury Assessment score (ASIA) on admission and the Subaxial Cervical Spine Injury Classification score (SLICS); there was complete SCI across 168 cases [14, 19, 20, 26, 43]. An additional two studies found correlations between FA at the distal quarter of the spinal cord and urinary incontinence [34] and between FTD and interval improvement in long tract function as determined by the American Spinal Injury Association Impairment Scale (AIS) [44]. However, the remaining case series across 25 patients found no correlation between FA or FTD and ASIA [33], and the sole case–control study across 35 patients reported that sDTI parameters were not predictors for ambulation at six and twelve months as measured on multiple PROM scales [29]. Nevertheless, most studies appear to suggest a potential role of sDTI for clarifying prognosis in SCI.
As current predictors of the natural history of disease rely imperfectly on admission categorization schema such as ASIA, improved methods via noninvasive imaging provide an exciting option, particularly regarding ambulation. Patients presenting with SCI resulting in severe distal paresis invariably ask the same question, ‘what are the odds I will walk again?’, which remains difficult to answer; we are limited to historical methods supplemented by physical examination [57]. Further prospective studies of sDTI applicability with larger sample sizes are highly warranted and clinically relevant.
Current state of spinal DTI in the clinical setting
sDTI is a promising advance in neurosurgical pathology and its clinical applicability continues to evolve. As it stands, DTI parameters, particularly FA and ADC, appear to offer accurate prognoses in the context of degenerative disease and traumatic SCI, with possible uses in determining surgical outcomes. However, as mentioned, many studies reporting such results do so relative to currently-used PROMs, suggesting a possible need to change current methods. Severity characterization and outcome analysis would likely benefit if objective data offered by noninvasive imaging were used rather than subjective PROM values, which have inherent bias. Patients can embellish or underplay symptoms, or their effect on daily function, because of sociocultural variables and individual perceptions. Additionally, such parameters would be particularly useful for patients who cannot communicate for medical or cultural reasons. The application of sDTI in surgical resection of spinal cord neoplasms and malformations is truly a nascent field, most of the works reviewed being restricted to operative feasibility in the form of case reports or series. A few case reports describe the potential applicability of preoperative tractography merged with intraoperative imaging in neuronavigation for challenging lesions. Cumulatively, the results of these reports appear promising, but continued investigation and validation are required, and future developments will be influenced by ongoing technological advances.
Conclusions
sDTI seems useful for surgical decision making and outcome measurements and establishing clinical prognoses in a wide range of neurosurgical pathologies. Results were promising in evaluating degenerative disease, intradural operative neuronavigation/planning, and SCI severity grading. Further controlled prospective research with longer follow-up and population sizes is warranted.
References
F Alkherayf AF Arab E Tsai 2015 Conus medullaris teratoma with utilization of fiber tractography: case report J Neurol Surg Rep 76 1 e183 187
A Banaszek J Bladowska P Szewczyk P Podgorski M Sasiadek 2014 Usefulness of diffusion tensor MR imaging in the assessment of intramedullary changes of the cervical spinal cord in different stages of degenerative spine disease Eur Spine J 23 7 1523 1530
CG Benjamin A Frempong-Boadu M Hoch M Bruno T Shepherd D Pacione 2019 Combined use of diffusion tractography and advanced intraoperative imaging for resection of cervical intramedullary spinal cord neoplasms: a case series and technical note OperNeurosurg (Hagerstown) 17 5 525 530
S Bhosale P Ingale S Srivastava N Marathe P Bhide 2019 Diffusion tensor imaging as an additional postoperative prognostic predictor factor in cervical myelopathy patients: an observational study J Craniovertebr Junction Spine 10 1 10 13
JL Cui X Li TY Chan KC Mak KD Luk Y Hu 2015 Quantitative assessment of column-specific degeneration in cervical spondylotic myelopathy based on diffusion tensor tractography Eur Spine J 24 1 41 47
C Dauleac C Frindel F Cotton I Pelissou-Guyotat 2019 Tractography-based surgical strategy for cavernoma of the conus medullaris: case illustration J Neurosurg Spine 32 4 611 612
F Dong Y Wu P Song 2018 A preliminary study of 3.0-T magnetic resonance diffusion tensor imaging in cervical spondylotic myelopathy Eur Spine J 27 8 1839 1845
Y Eguchi S Ohtori M Suzuki 2016 Discrimination between lumbar intraspinal stenosis and foraminal stenosis using diffusion tensor imaging parameters: preliminary results Asian Spine J 10 2 327 334
BM Ellingson N Salamon JW Grinstead LT Holly 2014 Diffusion tensor imaging predicts functional impairment in mild-to-moderate cervical spondylotic myelopathy Spine J 14 11 2589 2597
BM Ellingson N Salamon DC Woodworth LT Holly 2015 Correlation between degree of subvoxel spinal cord compression measured with super-resolution tract density imaging and neurological impairment in cervical spondylotic myelopathy J Neurosurg Spine 22 6 631 638
S Liu S Buch Y Chen HS Choi Y Dai C Habib J Hu JY Jung Y Luo D Utriainen M Wang 2017 Susceptibility-weighted imaging: current status and future directions NMR Biomed 30 4 e3552
X Han X Ma D Li 2020 The evaluation and prediction of laminoplasty surgery outcome in patients with degenerative cervical myelopathy using diffusion tensor MRI AJNR Am J Neuroradiol 41 9 1745 1753
SW Hughes PJ Hellyer DJ Sharp RD Newbould MC Patel PH Strutton 2020 Diffusion tensor imaging of lumbar spinal nerves reveals changes in microstructural integrity following decompression surgery associated with improvements in clinical symptoms: a case report MagnReson Imaging 69 65 70
BF Iliescu P Gutu MG Dabija 2021 Traumatic subaxial cervical spine injury - improving initial evaluation through correlation of diffusion tensor imaging and subaxial cervical spine injury classification SLIC score Surg Neurol Int 12 10
M Kitamura S Maki M Koda 2020 Longitudinal diffusion tensor imaging of patients with degenerative cervical myelopathy following decompression surgery J Clin Neurosci 74 194 198
JW Lee JH Kim JB Park 2011 Diffusion tensor imaging and fiber tractography in cervical compressive myelopathy: preliminary results Skeletal Radiol 40 12 1543 1551
J Li H Cui Z Liu 2019 Utility of diffusion tensor imaging for guiding the treatment of lumbar disc herniation by percutaneous transforaminal endoscopic discectomy Sci Rep 9 1 18753
S Maki M Koda M Kitamura 2017 Diffusion tensor imaging can predict surgical outcomes of patients with cervical compression myelopathy Eur Spine J 26 9 2459 2466
M Mossa-Basha DJ Peterson DS Hippe 2021 Segmented quantitative diffusion tensor imaging evaluation of acute traumatic cervical spinal cord injury Br J Radiol 94 1118 20201000
MJ Mulcahey AF Samdani JP Gaughan 2013 Diagnostic accuracy of diffusion tensor imaging for pediatric cervical spinal cord injury Spinal Cord 51 7 532 537
M Nakamura K Fujiyoshi O Tsuji 2012 Clinical significance of diffusion tensor tractography as a predictor of functional recovery after laminoplasty in patients with cervical compressive myelopathy J Neurosurg Spine 17 2 147 152
M Nukala J Abraham G Khandige BK Shetty APA Rao 2019 Efficacy of diffusion tensor imaging in identification of degenerative cervical spondylotic myelopathy Eur J Radiol Open 6 16 23
S Rajasekaran JS Yerramshetty VS Chittode RM Kanna G Balamurali AP Shetty 2014 The assessment of neuronal status in normal and cervical spondylotic myelopathy using diffusion tensor imaging Spine (Phila Pa 1976) 39 15 1183 1189
A Rao H Soliman M Kaushal 2018 Diffusion tensor imaging in a large longitudinal series of patients with cervical spondylotic myelopathy correlated with long-term functional outcome Neurosurgery 83 4 753 760
T Scullen J Riffle S Koga J Kalyvas 2019 Novel technique of coregistered intraoperative computed tomography and preoperative magnetic resonance imaging and diffusion tensor imaging navigation in spinal cord tumor resection Ochsner J 19 1 43 48
O Seboco F Gebremariam G Joubert 2021 Correlation of blunt cervical spinal cord injury magnetic resonance imaging tractography with the American Spinal Injury Association impairment scale motor scores SA J Radiol 25 1 2038
M Setzer RD Murtagh FR Murtagh 2010 Diffusion tensor imaging tractography in patients with intramedullary tumors: comparison with intraoperative findings and value for prediction of tumor resectability J Neurosurg Spine 13 3 371 380
S Shabani M Kaushal M Budde B Schmit MC Wang S Kurpad 2019 Comparison between quantitative measurements of diffusion tensor imaging and T2 signal intensity in a large series of cervical spondylotic myelopathy patients for assessment of disease severity and prognostication of recovery J Neurosurg: Spine 31 4 473 479
K Shanmuganathan J Zhuo UK Bodanapally 2020 Comparison of acute diffusion tensor imaging and conventional magnetic resonance parameters in predicting long-term outcome after blunt cervical spinal cord injury J Neurotrauma 37 3 458 465
C Shen H Xu B Xu 2018 Value of conventional MRI and diffusion tensor imaging parameters in predicting surgical outcome in patients with degenerative cervical myelopathy J Back MusculoskeletRehabil 31 3 525 532
Y Shi F Zhao W Dou 2021 Quantitative evaluation of intraspinal lumbar disc herniation-related lumbosacral radiculopathy before and after percutaneous transforaminal endoscopic discectomy using diffusion tensor imaging Spine (Phila Pa 1976) 46 13 E734 E742
Y Shi Y Zou Y Feng 2020 A quantitative and clinical evaluation of nerve roots in lumbosacral radiculopathy using diffusion tensor imaging Jpn J Radiol 38 3 222 230
R Singh S Magu A Baskar RK Rohilla K Kaur S Kaur 2020 Correlation of clinical findings in acute spinal injury patients with magnetic resonance including diffusion tensor imaging and fiber tractography Spine Surg Relat Res 4 4 305 313
H Wang X Li Y Wang 2019 Assessing spinal cord injury area in patients with tethered cord syndrome by diffusion tensor imaging World Neurosurg 127 e542 e547
K Wang Z Chen F Zhang 2017 Evaluation of DTI parameter ratios and diffusion tensor tractography grading in the diagnosis and prognosis prediction of cervical spondylotic myelopathy Spine (Phila Pa 1976) 42 4 E202 E210
CY Wen JL Cui MP Lee KC Mak KD Luk Y Hu 2013 Quantitative analysis of fiber tractography in cervical spondylotic myelopathy Spine J 13 6 697 705
W Wu J Liang Y Chen A Chen Y Wu Z Yang 2017 Microstructural changes are coincident with the improvement of clinical symptoms in surgically treated compressed nerve roots Sci Rep 7 44678
W Wu Z Yang T Zhang 2020 Microstructural changes in compressed cervical spinal cord are consistent with clinical symptoms and symptom duration Spine (Phila Pa 1976) 45 16 E999 E1005
H Zhang L Guan Y Hai Y Liu H Ding X Chen 2020 Multi-shot echo-planar diffusion tensor imaging in cervical spondylotic myelopathy: a longitudinal study The Bone & Joint J 102 9 1210 1218
J Zhang F Zhang F Xiao 2018 Quantitative Evaluation of the compressed L5 and S1 nerve roots in unilateral lumbar disc herniation by using diffusion tensor imaging Clin Neuroradiol 28 4 529 537
M Zhao B Shi T Chen 2017 Axial MR diffusion tensor imaging and tractography in clinical diagnosed and pathology confirmed cervical spinal cord astrocytoma J Neurol Sci 375 43 51
W Zheng H Chen N Wang 2018 Application of diffusion tensor imaging cutoff value to evaluate the severity and postoperative neurologic recovery of cervical spondylotic myelopathy World Neurosurg 118 e849 e855
F Zhu Y Liu L Zeng 2021 Evaluating the severity and prognosis of acute traumatic cervical spinal cord injury: a novel classification using diffusion tensor imaging and diffusion tensor tractography Spine (Phila Pa 1976) 46 10 687 694
F Zhu L Zeng S Gui 2021 The role of diffusion tensor imaging and diffusion tensor tractography in the assessment of acute traumatic thoracolumbar spinal cord injury World Neurosurg 150 e23 e30
E Maj B Szemplinska W Szeszkowski 2020 Role of diffusion tensor imaging parameters in the characterization and differentiation of infiltrating and non-infiltrating spinal cord tumors : preliminary study Clin Neuroradiol 30 4 739 747
F Granata S Racchiusa E Mormina 2017 Presurgical role of MRI tractography in a case of extensive cervicothoracic spinal ependymoma Surg Neurol Int 8 56
AF Choudhri MT Whitehead P Klimo Jr BK Montgomery FA Boop 2014 Diffusion tensor imaging to guide surgical planning in intramedullary spinal cord tumors in children Neuroradiology 56 2 169 174
D Moher A Liberati J Tetzlaff DG Altman 2009 The PRISMA group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement PLoS Med 6 7 e1000097
L Cathenaut B Leonardon R Kuster P Inquimbert R Schlichter S Hugel 2022 Inhibitory interneurons with differential plasticities at their connections tune excitatory–inhibitory balance in the spinal nociceptive system Pain 163 5 e675 e688
MM D'Souza A Choudhary M Poonia P Kumar S Khushu 2017 Diffusion tensor MR imaging in spinal cord injury Injury 48 4 880 884
CS Parenteau EC Lau IC Campbell 2021 Prevalence of spine degeneration diagnosis by type, age, gender, and obesity using Medicare data Sci Rep 11 5389
TO Wichmann MM Rasmussen HB Einarsson 2021 Predictors of patient satisfaction following anterior cervical discectomy and fusion for cervical radiculopathy Clin Neurol Neurosurg 205 106648
AM Zeitlberger M Sosnova M Ziga 2021 Assessment of the minimum clinically important difference in the smartphone-based 6-minute walking test after surgery for lumbar degenerative disc disease Spine (Phila Pa 1976) 46 18 E959 E965
M Scott-Young SM Lee D Nielsen E Rathbone M Rackham W Hing 2022 Comparison of mid-to long-term follow-up of patient-reported outcomes measures after single-level lumbar total disc arthroplasty, multi-level lumbar total disc arthroplasty, and the lumbar hybrid procedure for the treatment of degenerative disc disease Spine 47 5 377 386
H Wadhwa J Sharma K Varshneya 2021 Anterior cervical discectomy and fusion versus laminoplasty for multilevel cervical spondylotic myelopathy: a national administrative database analysis World Neurosurg 152 e738 e744
SD Lockey SM Trent SB Kalantar 2022 Cervical myelopathy: an update on posterior decompression Clin Spine Surg 35 1 E87 93
JA Flack KD Sharma JY Xie 2022 Delving into the recent advancements of spinal cord injury treatment: a review of recent progress Neural Regen Res 17 2 283 291
Funding
This work did not utilize grants or technical or corporate support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or proprietary interest in the subject matter of this article.
Ethical approval
This paper was exempt from IRB approval as it is a literature review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Scullen, T., Milburn, J., Aria, K. et al. The use of diffusion tensor imaging in spinal pathology: a comprehensive literature review. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08231-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08231-8