Abstract
Purpose
To assess whether saphenous somatosensory-evoked potentials (saphSSEP) monitoring may provide predictive information of femoral nerve health during prone lateral interbody fusion (LIF) procedures.
Methods
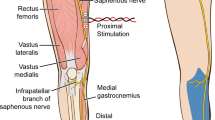
Intraoperative details were captured prospectively in consecutive prone LIF surgeries at a single institution. Triggered electromyography was used during the approach; saphSSEP was monitored throughout using a novel system that enables acquisition of difficult signals and real-time actionable feedback facilitating intraoperative intervention. Postoperative neural function was correlated with intraoperative findings.
Results
Fifty-nine patients (58% female, mean age 64, mean BMI 32) underwent LIF at 95 total levels, inclusive of L4-5 in 76%, fixated via percutaneous pedicle screws (81%) or lateral plate, with direct decompression in 39%. Total operative time averaged 149 min. Psoas retraction time averaged 16 min/level. Baseline SSEPs were unreliable in 3 due to comorbidities in 2 and anesthesia in 1; one of those resulted in transient quadriceps weakness, fully recovered at 6 weeks. In 25/56, no saphSSEP changes occurred, and none had postoperative femoral nerve deficits. In 24/31 with saphSSEP changes, responses recovered intraoperatively following intervention, with normal postoperative function in all but one with delayed quadriceps weakness, improved at 4 months and recovered at 9 months, and a second with transient isolated anterior thigh numbness. In the remaining 7/31, saphSSEP changes persisted to close, and resulted in 2 transient isolated anterior thigh numbness and 2 combined sensory and motor femoral nerve deficits, both resolved at between 4 and 8 months.
Conclusions
SaphSSEP was reliably monitored in most cases and provided actionable feedback that was highly predictive of neurological events during LIF.
Level of evidence
Diagnostic: individual cross-sectional studies with consistently applied reference standard and blinding.


Similar content being viewed by others
References
Lehmen JA, Gerber EJ (2015) MIS lateral spine surgery: a systematic literature review of complications, outcomes, and economics. Eur Spine J 24(Suppl 3):S287-313
Lykissas MG, Aichmair A, Hughes AP, Sama AA, Dr L, Taher F, Du JY, Cammisa FP, Girardi FP (2014) Nerve injury after lateral lumbar interbody fusion: a review of 919 treated levels with identification of risk factors. Spine J 2014:749–758
Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6:435–443
Tohmeh AG, Rodgers WB, Peterson MD (2011) Dynamically evoked, discrete-threshold electromyography in the extreme lateral interbody fusion approach. J Neurosurg Spine 14:31–37
Gonzalez AA, Jeyanandarajan D, Hansen C, Zada G, Hsieh PC (2009) Intraoperative neurophysiological monitoring during spine surgery: a review. Neurosurg Focus 27:E6
Gundanna M, Eskenazi M, Bendo J, Spivak J, Moskovich R (2003) Somatosensory evoked potential monitoring of lumbar pedicle screw placement for in situ posterior spinal fusion. Spine J 3:370–376
Lyon R, Gibson A, Burch S, Lieberman J (2010) Increases in voltage may produce false-negatives when using transcranial motor evoked potentials to detect an isolated nerve root injury. J Clin Monit Comput 24(6):441–448
Silverstein J, Mermelstein L, DeWal H, Basra S (2014) Saphenous nerve somatosensory evoked potentials: a novel technique to monitor the femoral nerve during transpsoas lumbar interbody fusion. Spine 39(15):1254–1260
Jain N, Alluri R, Phan K, Yanni D, Alvarez A, Guillen H, Mnatsakanyan L, Bederman SS (2021) Saphenous nerve somatosensory-evoked potentials monitoring during lateral interbody fusion. Global Spine J 11(5):722–726
Pimenta L, Taylor WR, Stone LE, Wali AR, Santiago-Dieppa DR (2020) Prone transpsoas technique for simultaneous single-position access to the anterior and posterior lumbar spine. Oper Neurosurg 20(1):E5–E12
Pimenta L, Amaral R, Taylor W, Tohmeh A, Pokorny G, Rodrigues R, Arnoni D, Guirelli T, Batista M (2020) The prone transpsoas technique: preliminary radiographic results of a multicenter experience. Eur Spine J 29(8):2104
Obrien J, Haines C, Dooley ZA, Turner AW, Jackson D (2014) Femoral nerve strain at L4–L5 is minimized by hip flexion and increased by table break when performing lateral interbody fusion. Spine 39(1):33–38
Buckland AJ, Beaubrun BM, Isaacs E, Moon J, Zhou P, Horn S, Poorman G, Tishelman JC, Day LM, Errico TJ, Passias PG, Protopsaltis T (2018) Psoas morphology differs between supine and sitting magnetic resonance imaging lumbar spine: Implications for lateral lumbar interbody fusion. Asian Spine J 12(1):29–36
American Clinical Neurophysiology Society. Guideline 11B: Recommended Standards for Intraoperative Monitoring of Somatosensory Evoked Potentials. 2009. Retrieved from ACNS.org
Duncan JW, Bailey RA, Baena R (2012) Intraoperative decrease in amplitude of somatosensory-evoked potentials of the lower extremities with interbody fusion cage placement during lumbar fusion surgery. Spine 37(20):E1290–E1295
Cheng I, Briseno MR, Arrigo RT, Bains N, Ravi S, Tran A (2015) Outcomes of two different techniques using the lateral approach for lumbar interbody arthrodesis. Global Spine J 5:305–314
Cheng I, Acosta F, Chang K, Pham M (2016) Point-counterpoint: the use of neuromonitoring in lateral transpsoas surgery. Spine 41(8S):S145–S151
Gunnarsson T, Krassioukov AV, Sarjeant R, Fehlings MG (2004) Real-time continuous intraoperative electromyographic and somatosensory evoked potential recordings in spinal surgery: correlation of clinical and electrophysiologic findings in a prospective, consecutive series of 213 cases. Spine 29:677–684
Houten JK, Alexandre LC, Nasser R, Wollowick AL (2011) Nerve injury during the transpsoas approach for lumbar fusion. J Neurosurg Spine 15:280–284
Chaudhary K, Speights K, McGuire K, White AP (2015) Trans-cranial motor evoked potential detection of femoral injury in trans-psoas lateral lumbar interbody fusion. J Clin Monit Comput 29:549–554
Berends HI, Journée HL, Rácz I, van Loon J, Härtl R, Spruit M (2016) Multimodality intraoperative neuromonitoring in extreme lateral interbody fusion. transcranial electrical stimulation as indispensable rearview. Eur Spine J 25:1581–1586
Uribe JS, Isaacs RE, Youssef JA, Khajavi K, Balzer JR, Kanter AS, Kuelling FA, Peterson MD (2015) Solas degenerative study group can triggered electromyography monitoring throughout retraction predict postoperative symptomatic neuropraxia after XLIF? results from a prospective multicenter trial. Eur Spine J 24(Suppl 3):S378–S385
Block J, Silverstein JW, Ball HT, Mermelstein LE, DeWal HS, Madhok R, Basra SK, Goldstein MJ (2015) Motor evoked potentials for femoral nerve protection in transpsoas lateral access surgery of the spine. Neurodiagnostic J 55:36–45
Riley MR, Doan AT, Vogel RW, Aguirre AO, Pieri KS, Scheid EH (2018) Use of motor evoked potentials during lateral lumbar interbody fusion reduces postoperative deficits. Spine J 18:1763–1778
Chui J, Murkin JM, Turkstra T, McKenzie N, Guo L, Quantz M (2017) A novel automated somatosensory evoked potential (SSEP) monitoring device for detection of intraoperative peripheral nerve injury in cardiac surgery: a clinical feasibility study. J Cardiothorac Vasx Anesth 31(4):1174–1182
Chui J, Murkin JM, Drosdowech D (2019) A pilot study of a novel automated somatosensory evoked potential (SSEP) monitoring device for detection and prevention of intraoperative peripheral nerve injury in total shoulder arthroplasty surgery. J Neurosurg Anesthesiol 31(3):291–298
Funding
No funding was provided for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Tohmeh is a consultant for Alphatec Spine, the manufacturer of the device used in this study, but received no financial support or remuneration related to the publication of this article. C. Somers has no conflicts. K. Howell is an employee of Alphatec Spine. All authors have full control of the primary data and allow the journal to review the data if requested.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tohmeh, A., Somers, C. & Howell, K. Saphenous somatosensory-evoked potentials monitoring of femoral nerve health during prone transpsoas lateral lumbar interbody fusion. Eur Spine J 31, 1658–1666 (2022). https://doi.org/10.1007/s00586-022-07224-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07224-9