Abstract
Purpose
The aim of this study is to clarify the factors affecting physical function after allogeneic hematopoietic stem cell transplantation (HSCT).
Methods
We retrospectively analyzed 88 patients (median age, 44.5 years) who received allogeneic HSCT. Leg extension torque and peak oxygen consumption (VO2) were evaluated before and after HSCT. Patient factors (age, sex, underlying diseases, hemoglobin, serum albumin, and Karnofsky performance status score before transplant) and transplant factors (conditioning regimen, days to neutrophil engraftment, grades of acute graft-versus-host disease [GVHD], infections, and the interval between pre- and post-evaluation) were collected via chart review, and were used for correlational and comparison analyses in order to identify the variables associated with reduced post-HSCT leg extension torque and peak VO2. Stepwise multiple regression analyses for post-HSCT leg extension torque and post-HSCT peak VO2 were performed using age, sex, and the related variables with a p value < 0.2 in the correlational and comparison analyses.
Results
Leg extension torque and peak VO2 were significantly reduced after HSCT (p < 0.001). Pre-HSCT leg extension torque, grades of acute GVHD, age, and the interval between pre- and post-evaluation were identified as significant factors associated with reduced post-HSCT leg extension torque. However, none of these factors were significantly associated with reduced post-HSCT peak VO2, and only its pre-transplant value was identified as a significant factor.
Conclusions
These findings suggest that improvements in muscle strength and cardiopulmonary fitness before HSCT are crucial for maintaining post-treatment physical function, especially in elderly individuals with acute GVHD requiring a long-term stay in a protective environment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is a curative but intensive therapy for a variety of hematopoietic disorders, and the number of HSCTs has continued to increase over the last ten years, especially in the elderly population. The outcomes of HSCT have also improved and the number of recipients who achieve long-term survival after HSCT continues to increase. Therefore, the current goal of HSCT is not only curing disease but also maintaining a high quality of life while reducing physical and/or mental distress after HSCT [1,2,3].
Deconditioning and reduction of physical function are likely to occur after HSCT. Decreased physical activity due to isolation in a protective environment, and the impact of regimen-related toxicity and/or post-transplant complications have been reported as causes for this physical decline [4,5,6]. Decreases in endurance capacity may result in easy fatigability and loss of muscle strength may cause disabilities.
The purpose of exercise and rehabilitation for patients undergoing HSCT is to prevent deconditioning and recover from decreased physical function. Previous studies have shown the efficacy of rehabilitation in patients undergoing HSCT using a variety of exercise modalities, including aerobic, resistance, and mixed (aerobic and resistance) programs [7,8,9,10,11,12,13,14,15,16]. However, functional capacity declines after HSCT, even with exercise therapy [8, 10, 12, 17, 18]. Thus, identifying the factors related to physical function after HSCT is crucial to establish better preventive and rehabilitative strategies. Some studies have suggested that the decrease in fitness was associated with the fever period and total dose of corticosteroids [17], while the decrease in strength was associated with the total dose of corticosteroids [17, 18]. However, in these studies, the sample size was small [17], and a 6-min walk test was used for the evaluation of fitness [17, 18] instead of peak oxygen consumption (VO2) during cardiopulmonary exercise testing (CPX), which is the gold standard. In addition, certain important factors, such as baseline physical function before HSCT, were not included in these previous analyses [17, 18]. Thus, the aim of the present study was to explore the factors associated with post-HSCT leg extension muscle strength and cardiopulmonary fitness evaluated with peak VO2.
Methods
Study design
This was a retrospective cohort study performed at the Keio University Hospital in Tokyo, Japan. The study protocol was approved by the Ethics Committee of Keio University School of Medicine (No. 20120072).
Participants
Of 146 consecutive patients who underwent allogeneic HSCT from April 2008 to March 2013, 108 patients satisfied the inclusion and exclusion criteria. Inclusion criteria were aged 18 years or older on the day of HSCT, underwent allogeneic HSCT at Keio University Hospital, and were evaluated for leg extension muscle strength and/or cardiopulmonary fitness using CPX at both pre- and post-HSCT. Patients were excluded if they developed any severe physical dysfunctions that could affect muscular strength and fitness evaluation, such as joint contractures and/or severe joints pain of the lower extremities; avascular necrosis of the femur head; painful metastatic bone lesions; bone lesions requiring limited weight bearing; severe heart failure (New York Heart Association, III–IV); or required assistance for basic activities of daily living. Patients were also excluded from the study if they could not receive leg extension muscle strength and/or cardiopulmonary fitness evaluations due to acute somatic conditions (such as infection, fever, or acute bleeding) at the time of evaluation. After excluding these patients and those with missing data for the analyses, 88 patients were enrolled in the study.
Physical therapy
All patients participated in a rehabilitation program 5 days a week before, during, and after HSCT. At the rehabilitation gym, the patients received physical therapy including stretching of the neck, trunk, and extremities; resistance exercise for the muscles of the trunk and upper and lower extremities; aerobic exercise using a treadmill or cycle ergometer (up to 30 min) with an aim of approximately 60% of heart rate (HR) reserve calculated according to the Karvonen method [19]: (HRpeak during CPX − HRrest) × 60 % + HRrest; and walking and stair training. An infrared ear/finger clip heart rate sensor was used for monitoring the heart rates during exercise. The content and intensity of the exercise were adjusted according to the physical condition of each patient. From the start of conditioning to neutrophil engraftment and other periods of neutropenia, such as those caused by additional chemotherapy before HSCT, a similar exercise program was carried out in the protective environment or the ward. However, during this period, walking tended to be more frequent than exercise on the ergometer and treadmill due to the patients’ physical conditions and lack of equipment. As such, the location of exercise was changed from the ward to the rehabilitation gym after HSCT when permission from the attending hematologists was obtained after achieving sustained neutrophil engraftment.
Treatment of acute graft-versus-host disease
Primary treatment of acute graft-versus-host disease (GVHD) was provided according to its grades [20]. Patients with grade I acute GVHD were treated with topical steroids. Patients with grade II–IV acute GVHD were treated with 1.0–2.0 mg/kg/day of (methyl-)prednisolone, while grade II acute GVHD limited to the skin was treated with hydrocortisone infusion and/or 0.5–1.0 mg/kg/day of (methyl-)prednisolone. Once patients responded, the dose of steroid started being tapered 10% of initial dose every 5 days.
Multidisciplinary team approaches
For all the participants, team conferences with multidisciplinary members including registered dieticians, psychiatrists, dentists, transplant coordinators, pharmacists, physical therapists, and physiatrists were held every week or once every 2 weeks.
Evaluation of strength and cardiopulmonary fitness
Muscle strength and cardiopulmonary fitness evaluations were performed on each patient twice: before the HSCT conditioning regimen (pre) and at the initiation of gym-based training when hematopoietic recovery was obtained after HSCT (post).
-
a)
Leg extension muscle strength
To evaluate leg extension muscle strength, an isokinetic test of peak leg extension torque was performed with a recumbent cycle ergometer at 50 rpm (Strength Ergo 240™; Mitsubishi Electric Corporation, Tokyo, Japan). This test has excellent test-retest reliability and sufficient validity against a conventional isokinetic dynamometer [21, 22]. The backrest was adjusted to a reclining position (110°) and the seat position was adjusted so that the patient’s knee was flexed 20° when at maximal extension. The trunk of the body was fixed at the shoulders with seatbelts. The peak torque values for five revolutions were measured and averaged. Each patient performed the test twice and the higher value was adopted. The adopted peak leg extension torque was adjusted to a value per kg of body weight.
-
b)
Cardiopulmonary fitness
The CPX was performed to the symptom-limited maximum using an upright, servo motor type, cycle ergometer (Strength Ergo 8™; Mitsubishi Electric Corporation, Tokyo, Japan). For each patient, breath-by-breath VO2 was measured during the cycling exercise at 60 rpm through a face mask using an expired gas analyzer (AE-300S™; Minato Medical Science Company Limited, Tokyo, Japan or Vmax 29™; SensorMedics Corporation, Yorba Linda, CA, USA). Both systems consist of a dumbbell type paramagnetic oxygen analyzer and infrared carbon dioxide analyzer, and both systems’ reliability and validity have been confirmed [23,24,25,26]. After 2 min of rest and 2 min of unloaded pedaling, the exercise load was increased by 10–15 W per min using a ramp protocol. Exercise was continued up to the limits of tolerance indicated by reduced pedaling rotation (despite being encouraged), unbearable shortness of breath, and/or a plateau in VO2 or HR response. Peak VO2 (mL/kg/min) was measured as the average value obtained during the last 30 s of the incremental test as an index of endurance capacity. Peak VO2 was adjusted to a value per kilogram of body weight for the analyses.
Data collection
Demographic information and clinical data were collected via the medical charts. Demographic data included age, sex, underlying diseases (leukemia, lymphoma, multiple myeloma, or aplastic anemia), conditioning regimen (myeloablative conditioning or reduced-intensity conditioning, total body irradiation, or non-total body irradiation), serum albumin level, hemoglobin level, and Karnofsky performance status (KPS) score [27] before HSCT. The interval between pre- and post-evaluation, number of days from HSCT to neutrophil engraftment, grades of acute GVHD [20], and infections (cytomegalovirus disease, bacterial infection, and invasive pulmonary aspergillosis) were also collected as clinical data.
Analyses
Descriptive analyses were performed on the patients’ characteristics. Pre- and post-differences for leg extension torque and peak VO2 were examined using a paired t test.
To clarify the factors related to leg extension torque and peak VO2 post-HSCT, we analyzed their relationships with several variables at baseline and during the clinical course via correlational analyses or comparison analyses. For continuous variables such as age, serum albumin level, and hemoglobin level, correlations between these variables and post-HSCT leg extension torque or post-HSCT peak VO2 were analyzed using the Pearson’s product moment correlation coefficient or the Spearman’s correlation coefficient, depending on the type of variable. With regard to the categorical variables such as sex and infectious complications, post-HSCT leg extension torque and post-HSCT peak VO2 were divided into two groups according to the category and were then compared using an independent t test.
Stepwise multiple regression analyses for post-HSCT leg extension torque and post-HSCT peak VO2 were performed using age, sex, and the variables with a p value < 0.2 in the above correlational or comparison analyses.
All statistical analyses were performed using IBM SPSS version 23 (IBM Corporation, Armonk, NY, USA), and a p value < 0.05 was considered to be statistically significant.
Results
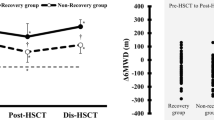
Patients’ characteristics are shown in Table 1. Both leg extension torque and peak VO2 significantly decreased after HSCT (p < 0.001 for both; Fig. 1). Of note, peak VO2 was evaluated in 67 of the 88 patients at both pre- and post-HSCT; 12 patients pre-HSCT and 16 patients post-HSCT could not be evaluated due to poor general condition and/or limited time for evaluation.
In the correlational or comparison analyses, variables with p < 0.2 were age, sex, serum albumin, pre-HSCT leg extension torque, pre-HSCT peak VO2, KPS score, pre- and post-evaluation interval, grades of acute GVHD, leukemia, aplastic anemia, cytomegalovirus disease, and invasive pulmonary aspergillosis for post-HSCT leg extension torque; and age, serum albumin, pre-HSCT leg extension torque, and pre-HSCT peak VO2 for post-HSCT peak VO2 (Tables 2 and 3). We included age, sex, and these variables with p < 0.2 in the multiple regression models. Multiple regression analysis for post-HSCT leg extension torque revealed that lower pre-HSCT leg extension torque, higher grades of acute GVHD, older age, and longer interval between pre- and post-evaluations were significant factors associated with reduced post-HSCT leg extension torque (Table 4(a)). Conversely, only lower pre-HSCT peak VO2 was significantly associated with reduced post-HSCT peak VO2 (Table 4(b)).
Discussion
This study identified the factors associated with post-treatment lower limb muscle strength and cardiopulmonary fitness in 88 patients who underwent allogenic HSCT. Both leg extension torque and peak VO2 significantly reduced after HSCT, and the pre-transplant values of peak VO2 and leg extension torque were significantly related to their respective post-transplant values. Post-HSCT leg extension torque was also significantly associated with grades of acute GVHD, age, and pre- and post-evaluation interval.
The effect of pre-HSCT physical status on post-HSCT status has not been well understood as previous studies did not include pre-transplant physical status into their analyses [17, 18]. Thus, to our knowledge, our study was the first to reveal that post-HSCT leg extension torque and peak VO2 were strongly associated with each of their pre-HSCT variables, respectively. These findings suggest that the higher the physical function before HSCT, the higher the physical function after HSCT. Previous studies showed that physical fitness was lower in patients before HSCT than in healthy subjects [28], and low functional capacity was associated with high mortality [29, 30] and longer hospital stay [30]. Considering these findings and those of the present study, maximizing physical capacity before HSCT could lead to better functional outcomes, as well as reduce the length of hospital stay and mortality risk.
Regarding leg extension torque, a significant negative correlation between the grades of acute GVHD and leg extension torque after HSCT was found. There are two possible reasons for this finding. First, acute GVHD is a significant factor that influences substantial deterioration in nutritional status during HSCT and in the early period after HSCT [31]. Second, it is known that the decrease in strength is associated with total dose of corticosteroids [17, 18]. In general, corticosteroids are administered to patients with grade II or higher GVHD and are often used at lower doses in grade II than in grade III or IV disease [32, 33]. Thus, steroidal muscle atrophy may have been involved in muscle weakness, in addition to exhaustion and malnutrition due to GVHD itself. Considering the relationship between the dose of corticosteroids and the severity of GVHD, our findings are consistent with previous studies that showed a relationship between muscle strength and corticosteroids dose [17, 18]. With regard to age, it has been reported that loss of muscle strength with aging [34,35,36,37] may be accelerated by the failure of muscle mass recovery after temporary disuse-induced muscle atrophy [35]. Therefore, the finding that the older the patients were, the poorer the muscle strength recovery was during HSCT is quite reasonable. The most logical answer to the question of why the interval between the evaluations was associated with reduced post-HSCT muscular strength is that the patients with longer evaluation intervals might have been in an unstable condition and stayed in the ward for a longer period to prevent infection; these conditions likely led to lower activity levels and might have weakened muscle strength.
Multiple regression analysis revealed that only pre-HSCT peak VO2 was associated with post-HSCT peak VO2. This indicates that the influence of exercise capacity before HSCT has the strongest effect compared with other factors. A relationship between hemoglobin values and exercise capacity was previously reported in healthy individuals [38, 39] and patients with various pathological conditions [40,41,42,43], including those requiring HSCT [18]. Although the findings from these previous studies suggested that hemoglobin level influences fitness level, we showed that the hemoglobin level before HSCT did not influence post-HSCT fitness.
The clinical implication drawn from the study is that maximizing the physical function before the HSCT is the key to preserve the function after the HSCT. Self-administered exercise before, during, and after HSCT was shown to be beneficial [12]. Furthermore, the supervised-individualized exercise before the HSCT was proven to be feasible [44]. The findings of these reports and ours suggest that it may be worth doing physical exercise before HSCT, although a well-designed randomized controlled trial is clearly warranted to ascertain the value of pre-HSCT physical exercise intervention.
There were limitations in this study. The study was conducted at a single facility. Only patients who could be evaluated for leg extension muscle strength and cardiopulmonary fitness using CPX were analyzed; therefore, those in poor general condition were not included. In addition, precise information about the dose of steroids and exercise adherence could not be obtained and were not included in the analyses because of the retrospective nature of the study. A prospective study including patients with various characteristics is necessary to increase the generalizability of our findings.
In conclusion, our findings suggest that improving muscular strength and cardiopulmonary fitness before receiving HSCT is important for maintaining physical function after HSCT treatment. Additionally, we emphasize the importance of commencing rehabilitation earlier before HSCT. Our study also suggests that careful consideration should be paid to lower limb muscle strength, especially in elderly individuals who are developing acute GVHD and those who are staying in a protective environment long-term.
References
Gruber U, Fegg M, Buchmann M, Kolb HJ, Hiddemann W (2003) The long-term psychosocial effects of haematopoetic stem cell transplantation. Eur J Cancer Care (Engl) 12:249–256. https://doi.org/10.1046/j.1365-2354.2003.00411_2.x
Gratwohl A, Baldomero H, Passweg J, Frassoni F, Niederwieser D, Schmitz N, Urbano-Ispizua A; Accreditation Committee of the European Group for Blood and Marrow Transplantation (EBMT); Working Parties Acute (ALWP) Chronic Leukemias (CLWP); Lymphoma Working Party (2003) Hematopoietic stem cell transplantation for hematological malignancies in Europe. Leukemia 17:941–959. https://doi.org/10.1038/sj.leu.2402896
Kopp M, Holzner B, Meraner V, Sperner-Unterweger B, Kemmler G, Nguyen-Van-Tam DP, Nachbaur D (2005) Quality of life in adult hematopoietic cell transplant patients at least 5 yr after treatment: a comparison with healthy controls. Eur J Haematol 74:304–308. https://doi.org/10.1111/j.1600-0609.2004.00402.x
Hacker ED, Larson J, Kujath A, Peace D, Rondelli D, Gaston L (2011) Strength training following hematopoietic stem cell transplantation. Cancer Nurs 34:238–249. https://doi.org/10.1097/NCC.0b013e3181fb3686
Steinberg A, Asher A, Bailey C, Fu JB (2015) The role of physical rehabilitation in stem cell transplantation patients. Support Care Cancer 23:2447–2460. https://doi.org/10.1007/s00520-015-2744-3
Larsen J, Nordström G, Ljungman P, Gardulf A (2007) Factors associated with poor general health after stem-cell transplantation. Support Care Cancer 15:849–857. https://doi.org/10.1007/s00520-006-0200-0
Cunningham BA, Morris G, Cheney CL, Buergel N, Aker SN, Lenssen P (1986) Effects of resistive exercise on skeletal muscle in marrow transplant recipients receiving total parenteral nutrition. JPEN J Parenter Enteral Nutr 10:558–563. https://doi.org/10.1177/0148607186010006558
Mello M, Tanaka C, Dulley FL (2003) Effects of an exercise program on muscle performance in patients undergoing allogeneic bone marrow transplantation. Bone Marrow Transplant 32:723–728. https://doi.org/10.1038/sj.bmt.1704227
Jarden M, Baadsgaard MT, Hovgaard DJ, Boesen E, Adamsen L (2009) A randomized trial on the effect of a multimodal intervention on physical capacity, functional performance and quality of life in adult patients undergoing allogeneic SCT. Bone Marrow Transplant 43:725–737. https://doi.org/10.1038/bmt.2009.27
Baumann FT, Kraut L, Schüle K, Bloch W, Fauser AA (2010) A controlled randomized study examining the effects of exercise therapy on patients undergoing haematopoietic stem cell transplantation. Bone Marrow Transplant 45:355–362. https://doi.org/10.1038/bmt.2009.163
Baumann FT, Zopf EM, Nykamp E, Kraut L, Schüle K, Elter T, Fauser AA, Bloch W (2011) Physical activity for patients undergoing an allogeneic hematopoietic stem cell transplantation: benefits of a moderate exercise intervention. Eur J Haematol 87:148–156. https://doi.org/10.1111/j.1600-0609.2011.01640.x
Wiskemann J, Dreger P, Schwerdtfeger R, Bondong A, Huber G, Kleindienst N, Ulrich CM, Bohus M (2011) Effects of a partly self-administered exercise program before, during, and after allogeneic stem cell transplantation. Blood 117:2604–2613. https://doi.org/10.1182/blood-2010-09-306308
DeFor TE, Burns LJ, Gold EM, Weisdorf DJ (2007) A randomized trial of the effect of a walking regimen on the functional status of 100 adult allogeneic donor hematopoietic cell transplant patients. Biol Blood Marrow Transplant 13:948–955. https://doi.org/10.1016/j.bbmt.2007.04.008
Persoon S, Kersten MJ, van der Weiden K, Buffart LM, Nollet F, Brug J, Chinapaw MJ (2013) Effects of exercise in patients treated with stem cell transplantation for a hematologic malignancy: a systematic review and meta-analysis. Cancer Treat Rev 39:682–690. https://doi.org/10.1016/j.ctrv.2013.01.001
van Haren IE, Timmerman H, Potting CM, Blijlevens NM, Staal JB, Nijhuis-van der Sanden MW (2013) Physical exercise for patients undergoing hematopoietic stem cell transplantation: systematic review and meta-analyses of randomized controlled trials. Phys Ther 93:514–528. https://doi.org/10.2522/ptj.20120181
Bergenthal N, Will A, Streckmann F, Wolkewitz KD, Monsef I, Engert A, Elter T, Skoetz N (2014) Aerobic physical exercise for adult patients with haematological malignancies. Cochrane Database Syst Rev 11:CD009075. https://doi.org/10.1002/14651858.CD009075.pub2
Takekiyo T, Dozono K, Mitsuishi T, Murayama Y, Maeda A, Nakano N, Kubota A, Tokunaga M, Takeuchi S, Takatsuka Y, Utsunomiya A (2015) Effect of exercise therapy on muscle mass and physical functioning in patients undergoing allogeneic hematopoietic stem cell transplantation. Support Care Cancer 23:985–992. https://doi.org/10.1007/s00520-014-2425-7
Morishita S, Kaida K, Yamauchi S, Sota K, Ishii S, Ikegame K, Kodama N, Ogawa H, Domen K (2013) Relationship between corticosteroid dose and declines in physical function among allogeneic hematopoietic stem cell transplantation patients. Support Care Cancer 21:2161–2169. https://doi.org/10.1007/s00520-013-1778-7
Karvonen MJ, Kentala E, Mustala O (1957) The effects of training on heart rate; a longitudinal study. Ann Med Exp Biol Fenn 35:307–315
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, Thomas ED (1995) 1994 consensus conference on acute GVHD grading. Bone Marrow Transplant 15:825–828
Tateishi K, Yamada S, Omori Y, Kobayashi T, Aoki H, Morio Y (2001) Reliability of StrengthErgo240 for leg extension strength. Phys Ther Jpn 28:329–331 (in Japanese)
Kobayashi T, Yamada S, Omori Y, Tateishi K, Aoki H, Morio Y (2001) The relationships between muscle strength torque measured by pedaling type isokinetic machine and that by conventional isokinetic dynamometer. Phys Ther Jpn 28:338–342 (in Japanese)
Koike A, Hiroe M, Adachi H, Yajima T, Yamauchi Y, Nogami A, Ito H, Miyahara Y, Korenaga M, Marumo F (1994) Oxygen uptake kinetics are determined by cardiac function at onset of exercise rather than peak exercise in patients with prior myocardial infarction. Circulation 90:2324–2332. https://doi.org/10.1161/01.CIR.90.5.2324
Shimada Y, Yoshiya I, Hirata T, Takezawa J, Taenaka N (1984) Evaluation of a system for on-line analysis of VO2 and VCO2 for clinical applicability. Anesthesiology 61:311–314
Macfarlane DJ (2001) Automated metabolic gas analysis systems: a review. Sports Med 31:841–861
Vehrs PR, George JD, Fellingham GW, Plowman SA, Dustman-Allen K (2007) Submaximal treadmill exercise test to predict VO2max in fit adults. Meas Phys Educ Exerc Sci 11:61–72. https://doi.org/10.1080/10913670701294047
Karnofsky DA, Abelmann WH, Craver LF, Burchenal JH (1948) The use of the nitrogen mustards in the palliative treatment of carcinoma. With particular reference to bronchogenic carcinoma. Cancer 1:634–656. https://doi.org/10.1002/1097-0142(194811)1:4<634::AID-CNCR2820010410>3.0.CO;2-L
Morishita S, Kaida K, Ikegame K, Yoshihara S, Taniguchi K, Okada M, Kodama N, Ogawa H, Domen K (2012) Impaired physiological function and health-related QOL in patients before hematopoietic stem-cell transplantation. Support Care Cancer 20:821–829. https://doi.org/10.1007/s00520-011-1156-2
Jones LW, Devlin SM, Maloy MA, Wood WA, Tuohy S, Espiritu N, Aquino J, Kendig T, Michalski MG, Gyurkocza B, Schaffer WL, Ali B, Giralt S, Jakubowski AA (2015) Prognostic importance of pretransplant functional capacity after allogeneic hematopoietic cell transplantation. Oncologist 20:1290–1297. https://doi.org/10.1634/theoncologist.2015-0200
Wood WA, Deal AM, Reeve BB, Abernethy AP, Basch E, Mitchell SA, Shatten C, Hie Kim Y, Whitley J, Serody JS, Shea T, Battaglini C (2013) Cardiopulmonary fitness in patients undergoing hematopoietic SCT: a pilot study. Bone Marrow Transplant 48:1342–1349. https://doi.org/10.1038/bmt.2013.58
Urbain P, Birlinger J, Lambert C, Finke J, Bertz H, Biesalski HK (2013) Longitudinal follow-up of nutritional status and its influencing factors in adults undergoing allogeneic hematopoietic cell transplantation. Bone Marrow Transplant 48:446–451. https://doi.org/10.1038/bmt.2012.158
Martin PJ, Rizzo JD, Wingard JR, Ballen K, Curtin PT, Cutler C, Litzow MR, Nieto Y, Savani BN, Schriber JR, Shaughnessy PJ, Wall DA, Carpenter PA (2012) First- and second-line systemic treatment of acute graft-versus-host disease: recommendations of the American Society of Blood and Marrow Transplantation. Biol Blood Marrow Transplant 18:1150–1163. https://doi.org/10.1016/j.bbmt.2012.04.005
Murata M (2016) Treatment of acute graft-versus-host disease. Rinsho Ketsueki 57:2176–2182 (in Japanese). https://doi.org/10.11406/rinketsu.57.2176
Ditroilo M, Forte R, Benelli P, Gambarara D, De Vito G (2010) Effects of age and limb dominance on upper and lower limb muscle function in healthy males and females aged 40-80 years. J Sports Sci 28:667–677. https://doi.org/10.1080/02640411003642098
Hvid L, Aagaard P, Justesen L, Bayer ML, Andersen JL, Ørtenblad N, Kjaer M, Suetta C (2010) Effects of aging on muscle mechanical function and muscle fiber morphology during short-term immobilization and subsequent retraining. J Appl Physiol 109:1628–1634. https://doi.org/10.1152/japplphysiol.00637.2010
Kubo K, Ishida Y, Komuro T, Tsunoda N, Kanehisa H, Fukunaga T (2007) Age-related differences in the force generation capabilities and tendon extensibilities of knee extensors and plantar flexors in men. J Gerontol A Biol Sci Med Sci 62:1252–1258
Macaluso A, Nimmo MA, Foster JE, Cockburn M, McMillan NC, De Vito G (2002) Contractile muscle volume and agonist-antagonist coactivation account for differences in torque between young and older women. Muscle Nerve 25:858–863. https://doi.org/10.1002/mus.10113
Gledhill N (1982) Blood doping and related issues: a brief review. Med Sci Sports Exerc 14:183–189
Gledhill N, Warburton D, Jamnik V (1999) Haemoglobin, blood volume, cardiac function, and aerobic power. Can J Appl Physiol 24:54–65
Benedetto D, Rao CM, Cefalù C, Aguglia DO, Cattadori G, D'Ascola DG, Benedetto FA, Agostoni P, Sciomer S (2015) Effects of blood transfusion on exercise capacity in thalassemia major patients. PLoS One 10:e0127553. https://doi.org/10.1371/journal.pone.0127553
Cattadori G, Agostoni P, Corrà U, Sinagra G, Veglia F, Salvioni E, Bonomi A, La Gioia R, Scardovi AB, Ferraironi A, Emdin M, Metra M, Di Lenarda A, Limongelli G, Raimondo R, Re F, Guazzi M, Belardinelli R, Parati G, Caravita S, Magrì D, Lombardi C, Frigerio M, Oliva F, Girola D, Mezzani A, Farina S, Mapelli M, Scrutinio D, Pacileo G, Apostolo A, Iorio A, Paolillo S, Filardi PP, Gargiulo P, Bussotti M, Marchese G, Correale M, Badagliacca R, Sciomer S, Palermo P, Contini M, Giannuzzi P, Battaia E, Cicoira M, Clemenza F, Minà C, Binno S, Passino C, Piepoli M, MECKI score Research Group (appendix) (2017) Heart failure and anemia: effects on prognostic variables. Eur J Intern Med 37:56–63. https://doi.org/10.1016/j.ejim.2016.09.011
Odden M, Whooley M, Shlipak M (2004) Association of chronic kidney disease and anemia with physical capacity: the heart and soul study. J Am Soc Nephrol 15:2908–2915. https://doi.org/10.1097/01.ASN.0000143743.78092.E3
Ferrari M, Manea L, Anton K, Bruzzone P, Meneghello M, Zamboni F, Purgato L, Cazzoletti L, Ferrari P, Testi R (2015) Anemia and hemoglobin serum levels are associated with exercise capacity and quality of life in chronic obstructive pulmonary disease. BMC Pulm Med 15:58. https://doi.org/10.1186/s12890-015-0050-y
van Haren I, Staal JB, Potting CM, Atsma F, Hoogeboom TJ, Blijlevens NMA, Nijhuis-van der Sanden MWG (2018) Physical exercise prior to hematopoietic stem cell transplantation: a feasibility study. Physiother Theory Pract 34(10):747–756. https://doi.org/10.1080/09593985.2018.1423655
Acknowledgements
We would like to thank Toru Satoh, Yuichi Tamura, Yoshinori Katsumata, and Koichiro Azuma for supporting the cardiopulmonary exercise evaluations.
Funding
This work was supported in part by Japan Agency for Medical Research and Development (AMED) Practical Research for Innovative Cancer Control Grant Number 16ck0106215.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ishikawa, A., Otaka, Y., Kamisako, M. et al. Factors affecting lower limb muscle strength and cardiopulmonary fitness after allogeneic hematopoietic stem cell transplantation. Support Care Cancer 27, 1793–1800 (2019). https://doi.org/10.1007/s00520-018-4433-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4433-5