Abstract
Purpose
Bone metastases secondary to solid tumors increase the risk of skeletal-related events (SREs), including the occurrence of pathological fracture (PF), radiation to bone (RB), surgery to bone (SB), and spinal cord compression (SCC). The aim of this study was to evaluate the impact of SREs on patients’ pain, analgesic use, and pain interference with daily functioning.
Methods
Data were combined from patients with solid tumors and bone metastases who received denosumab or zoledronic acid across three identically designed phase 3 trials (N = 5543). Pain severity (worst pain) and pain interference were assessed using the Brief Pain Inventory at baseline and each monthly visit. Analgesic use was quantified using the Analgesic Quantification Algorithm.
Results
The proportion of patients with moderate/severe pain and strong opioid use generally increased in the 6 months preceding an SRE and remained elevated, while they remained relatively consistent over time in patients without an SRE. Regression analysis indicated that all SRE types were significantly associated with an increased risk of progression to moderate/severe pain and strong opioid use. PF, RB, and SCC were associated with significantly greater risk of pain interference overall. Results were similar for pain interference with emotional well-being. All SRE types were associated with significantly greater risk of pain interference with physical function.
Conclusions
SREs are associated with increased pain and analgesic use in patients with bone metastases. Treatments that prevent SREs may decrease pain and the need for opioid analgesics and reduce the impact of pain on daily functioning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone metastases are common in patients with advanced cancer, particularly those with breast and prostate cancers, with skeletal involvement in up to 75 % of patients [1, 2]. Other solid tumors that commonly affect bone are cancers of the lung, thyroid, kidney, and bladder [1, 2]. Advances in cancer treatments and earlier diagnosis have extended survival; patients with breast and prostate cancers live an average of 2 to 3 years after a diagnosis of bone metastasis [3]. However, extending survival also prolongs the course of the disease and its associated sequelae. Therefore, managing the symptoms of bone metastasis has become an important goal of therapy [4].
Bone metastases disturb the natural remodeling process between osteoblastic bone formation and osteoclastic bone resorption. Disrupting this balance causes an increase in bone osteolysis or in sclerotic bone depending on the lesion type [5–7]. Metastatic bone lesions ultimately weaken the structural integrity of bone, placing patients at an increased risk for developing skeletal complications such as pain, hypercalcemia, or the occurrence of skeletal-related events (SREs), which include pathological bone fractures, the need for radiation to bone to manage pain and control local tumor burden, compression of the spinal cord, and surgery to stabilize the bone or treat an existing fracture. A total of 64 % of patients with breast cancer and 49 % of those with prostate cancer develop skeletal complications within 2 years if bone metastases are not treated with a bone-targeted agent [8, 9], and 46 % of patients with lung cancer and other solid tumors develop bone complications during a 21-month observation period [10].
Pain is among the most common symptoms of bone metastasis in patients with advanced disease [11, 12]. Pain has a substantial psychological and physical impact on patients and is one of the most feared cancer symptoms [13, 14], with worsening pain often interpreted as disease progression [3]. The need for opioid analgesics increases as pain worsens, but some patients are reluctant to take opioids due to concerns about side effects (constipation, nausea, decreased alertness), tolerance, and addiction [3, 15]. In addition to the pain of bone metastases is the intensified pain associated with SREs [16]. Patients who experience pain and SREs are less able to perform daily tasks, leading to a loss of functional independence, and treating SREs requires travel time, work absenteeism, and possible in-patient hospital stays. Therefore, treatment goals for bone metastases include managing bone pain, delaying SREs, reducing the incidence of multiple SREs, and preserving patients’ function and well-being [10].
Pain associated with bone metastases has been well described [3, 12, 17], and the effects of bone-targeted agents on pain, analgesic use, and quality of life in patients with bone metastases have been reported previously [18, 19]. However, the precise impact of SREs exclusively, in addition to the pain of bone metastases and regardless of treatment received, has not yet been defined in a large patient population with a wide variety of tumor types. The objective of this study was to quantitate the impact of SREs by evaluating their association with pain and analgesic use and to determine the degree to which SREs interfere with daily functioning in a pooled analysis of patients with bone metastases who received bone-targeted agents across three large, phase 3 clinical trials [20–22].
Methods
Study design
Data were pooled from three identically designed, international, randomized, double-blind, double-dummy, phase 3 trials comparing denosumab and zoledronic acid in patients with breast cancer, prostate cancer, and other solid tumors (the majority of patients in the other solid tumors trial had lung cancer (46 %) [23, 24]). Patients with multiple myeloma enrolled in the trial of patients with other solid tumors were excluded from this analysis to maintain consistency with the US-labeled indication of denosumab [25]. Eligibility criteria and study designs from each trial and for the prespecified combined analysis of these trials have been reported previously [20–22, 26]. Briefly, patients had a primary diagnosis of breast cancer (trial 1, N = 2046) [20], prostate cancer (trial 2, N = 1901) [21], or other solid tumors or multiple myeloma (trial 3, N = 1776; 180 with multiple myeloma) [22], with radiographic evidence of at least one bone metastasis or bone lesion and an Eastern Cooperative Oncology Group performance status of 0, 1, or 2. Patients were excluded if they had received prior intravenous (IV) bisphosphonate therapy and if they had a creatinine clearance <30 mL/min (per Zometa® prescribing information). Informed consent was obtained from all individual participants included in the study.
Assessments
The Brief Pain Inventory Short Form (BPI-SF) was administered to patients at baseline and each monthly visit. Pain severity was based on pain at its worst, with scores ranging from 0 (no pain) to 10 (pain as bad as can be imagined). A BPI score ≤4 indicates no/mild pain, and scores >4 indicate moderate/severe pain [12, 27, 28].
Pain interference with general activity, walking, work, mood, enjoyment of life, relationship with others, and sleep was also assessed using the BPI-SF. Pain interference scores ranged from 0 (does not interfere) to 10 (completely interferes). Pain interference subscales were divided according to interference with emotional well-being or affect (relationship with others, enjoyment of life, mood), interference with physical activity (walking, general activity, and work), and overall interference, which includes each subscale item and sleep [12, 27, 28]. A ≥2-point change from baseline in pain scores is considered clinically meaningful [27].
Analgesic use was quantified at each monthly visit using the Analgesic Quantification Algorithm (AQA). Analgesic use was recorded as concomitant medications and converted into AQA scores that ranged from 0 (no analgesic use) to 7 (>600 mg oral morphine equivalents per day). An AQA score ≥3 indicates strong opioid usage [29].
The functional assessment of cancer therapy-general (FACT-G) was completed at each monthly visit to measure cancer-specific quality of life (QoL) [30]. FACT-G scores are a summation of four subscale scores ranging from 0 (worst QoL) to 108 (best QoL). A ≥5-point change in the FACT-G total score is considered clinically meaningful [31].
Statistical analysis
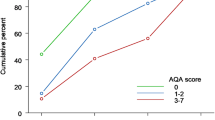
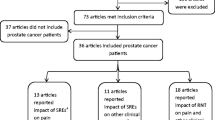
All randomized patients (except patients with multiple myeloma) were included in this posthoc analysis. In the descriptive analyses (Fig. 1), pain and analgesic use were analyzed from 6 months before to 6 months after the index date in both cohorts. For patients who had an on-study SRE, the index date was the time of the first on-study SRE. For patients who did not experience an on-study SRE, the index date was the median time to SRE in each SRE cohort to approximate natural disease progression. Regression analyses were performed to assess the risk of progressing to moderate/severe pain and strong opioid use and the risk of clinically meaningful worsening from baseline in pain interference associated with SREs (Fig. 2a, b, respectively). For pain and analgesic use outcomes, hazard ratios (HRs) and two-sided 95 % confidence intervals (CIs) were estimated using Cox proportional hazards models adjusting for the first on-study SRE (as time-dependent covariate), baseline bone metastases, analgesic score at baseline, worst pain score at baseline, region, ethnic group/race, and gender and stratified by study, treatment, and study randomization stratification factors. The median time to clinically meaningful increases (≥2 points) in pain interference from baseline was estimated using the Kaplan-Meier method; HRs were calculated using the Cox proportional hazards model. Correlations between clinically meaningful differences in overall pain interference (≥2-point increase) and FACT-G scores (≥5-point decrease) were calculated based on the Mantel-Haenszel method adjusting for study and treatment at each visit. The overall association between pain interference and FACT-G scores was measured based on the generalized estimating equations adjusting for study and treatment.
Proportion of patients with moderate/severe pain and strong opioid use. Moderate/severe pain is a BPI-SF worst pain score >4. Strong opioid use is an AQA score ≥3. Study visit −6 represents the visit 6 months before the occurrence of the first on-study SRE. The dashed vertical line represents the occurrence of the first SRE. Study visit 1 represents the first visit after the SRE. For patients with no SRE, data were not consistently available for months −6, −5, and −4. AQA Analgesic Quantification Algorithm, BPI-SF Brief Pain Inventory Short Form, SRE skeletal-related event
a Risk of progressing to moderate/severe pain and strong opioid use. Includes patients with baseline pain score ≤4 (pain progression; N = 2683 or AQA score ≤2) (opioid use; N = 4340); percentages indicate relative risk increase. *P < 005; **P < 0.01; ***P < 0.0001. b Risk of clinically meaningful worsening (≥2-point increase) from baseline in pain interference. Data include patients with baseline pain interference scores ≤8; percentages indicate relative risk increase. **P < 0.01; ***P ≤ 0.0001. AQA Analgesic Quantification Algorithm, CI confidence interval, SRE skeletal-related event
Results
Patients
This analysis included 5543 randomized patients from three clinical trials. The median time on study was 12 months overall (17 months in the breast cancer study, 12 months in the prostate cancer study, and 7 months in the other solid tumors study). Baseline characteristics are shown in Table 1. Most patients were Caucasian with a mean age of 62 years. The most common first on-study SRE was pathological fracture, followed by radiation to bone. A greater proportion of patients with an on-study SRE reported moderate/severe pain (BPI >4) at baseline compared to patients without an on-study SRE. The mean baseline AQA scores were similar between groups and represent nonopioid to weak opioid usage. A total of 8.4 % of patients with and 6.1 % of patients without an on-study SRE had an AQA score ≥5 at baseline, indicating opioid usage >300 mg oral morphine equivalent [29]. Pain interference was similar between groups. Among individual tumor types, patients with breast cancer and other solid tumors were younger than patients with prostate cancer (Table 2). Radiation to bone was the most common first on-study SRE in patients with prostate cancer and other solid tumors. Pathological fracture was most common in the breast cancer population.
Burden of SREs: worst pain and analgesic use
Among patients who had an on-study SRE, the proportion of patients with moderate/severe pain generally increased in the 6 months preceding the first on-study SRE (Fig. 1). Pain and analgesic use were most increased after spinal cord compression. Except for surgery to bone, the proportion of patients with moderate/severe pain remained elevated among those with an on-study SRE compared with those without an on-study SRE. A greater proportion of patients also progressed from no/low analgesic use to strong opioid use after SRE onset, with analgesic use remaining elevated for 6 months following the SRE. Similar to the pain severity outcomes, analgesic use remained consistent over time in those without an SRE.
Regression analysis showed that each SRE type was significantly associated with an increased risk of progressing from no/mild pain to moderate/severe pain (Table 3, Fig. 2a). Patients with spinal cord compression had the greatest increased risk followed by patients with surgery to bone, radiation to bone, and pathological fracture. Similarly, each SRE type was associated with a significant risk of progressing from no/low analgesic use to strong opioid use (Table 3, Fig. 2a). The greatest increased risk of progressing to strong opioid use was with spinal cord compression followed by radiation to bone, surgery to bone, and pathological fracture.
In the breast cancer population, those with spinal cord compression had the greatest increase in risk of progressing from no/mild pain to moderate/severe pain. However, only six patients had both spinal cord compression and a baseline pain score ≤4 (Table 3). The risk of progressing from no/low analgesic use to strong opioid use in this population was significant for all SREs, but the greatest increase was observed with spinal cord compression and surgery to bone. In the prostate cancer population, patients with radiation to bone, spinal cord compression, and pathological fracture were at a significantly greater risk of progressing to moderate/severe pain and strong opioid use (Table 3).
Burden of SREs: pain interference
Patients with on-study SREs had a shorter median time to worsening pain interference than those without on-study SREs (Table 4). Patients with spinal cord compression, radiation to bone, and pathological fracture as the first on-study SRE were at a significantly increased risk of clinically meaningful worsening in pain interference overall (Table 5, Fig. 2b). The impact of surgery to bone was also greater, though not significant. Results were similar for pain interference with emotional well-being (mood, relations with others, enjoyment of life; Table 5, Fig. 2b). All SRE types were significantly associated with an increased risk of pain interference with physical activity (walking, general activity, working; Table 5, Fig. 2b).
Comparable results were observed when the effect of a first on-study SRE on the risk of a clinically meaningful increase in pain interference was evaluated starting at the time of SRE diagnosis, rather than using a 28-day window.
For patients with breast cancer, spinal cord compression, radiation to bone, and pathological fracture were significantly associated with an increased risk of clinically meaningful worsening in pain interference overall (Table 5). Similar results were observed in patients with prostate cancer (Table 5); however, there were too few patients in the prostate cancer population with both surgery to bone and baseline pain interference scores ≤8 to provide meaningful results (n = 3).
Differences were observed in the pain interference subscales for each tumor type. In patients with breast cancer, surgery to bone, radiation to bone, and pathological fracture were significantly associated with an increased risk of a clinically meaningful increase in pain interference with physical function. For patients with prostate cancer, the greatest risk increase was with radiation to bone followed by spinal cord compression. Spinal cord compression and radiation to bone were significantly associated with an increased risk of pain interference with emotional well-being in the breast cancer population. For patients with prostate cancer, only radiation to bone had a significant impact on pain interference with emotional well-being (Table 5).
At any given study visit, up to 35 % of patients who experienced a clinically meaningful worsening in cancer-specific QoL (≥5-point decrease) had a clinically meaningful increase in pain interference. Significant correlations were noted between clinically meaningful increases in the overall pain interference score and clinically meaningful decreases in FACT-G total score at all visits (P < 0.0001 for all visits and overall).
Discussion
Improvements in cancer detection techniques and therapies have extended the lives of patients, and preserving patients’ function and well-being is an important part of optimally managing advanced cancer. In addition to treating bone metastases, reducing the complications of bone metastases by delaying or preventing skeletal complications is meaningful for patients and may lead to better overall clinical outcomes, such as maintenance/improvement in QoL and improved survival [32–37]. Here, we have shown in a large patient population that SREs are associated with an increase in pain and analgesic use. These results are expected to reflect real-world data because they are based on a large number of patients with a variety of tumor types. Except for surgery to bone, for which the statistical significance was limited by a small sample size, descriptive data show that the impact is greatest around the time of SRE occurrence, and pain and strong opioid use in patients with an SRE generally remain elevated at least 6 months after the event compared to patients without an SRE. These results suggest that patients who had pathological fracture, radiation to bone, or spinal cord compression did not fully recover following the SRE and that pain associated with these SREs was somewhat intractable despite strong opioid use. Managing pain associated with SREs may further expose patients to opioid-related side effects. Patients who had surgery to bone may have followed a different trend as the proportion of patients with strong opioid use remained high, but the proportion with moderate/severe pain decreased after surgery, suggesting that patients with a need for surgery to bone experience pain before surgery, but that the pain associated with surgery can be controlled with strong analgesic use. However, the small sample size limits our interpretation of these results. Patients with bone metastases who did not have an SRE did not experience an increase in pain and analgesic use in this study.
Among individual SREs, regression analysis showed that spinal cord compression and radiation to bone were generally associated with the greatest risk increase of an enduring progression in pain and analgesic use. These results were unexpected in patients who received radiation to bone, a palliative treatment, and may suggest that radiation is not providing the expected level of palliative symptom relief or that there may be certain aspects of bone metastasis pain that are not well controlled by radiotherapy and opioid analgesia. Indeed, patients may not respond to radiotherapy initially, or they may have recurring pain following an initial response requiring retreatment [38, 39]. The results could also be due to the way we measured pain (i.e., overall pain), which accounted for pain associated with multiple lesions that are not targeted simultaneously by radiation.
For pathological fractures, the magnitude of the effect may have been underestimated, because pathological fractures were identified according to regularly scheduled skeletal surveys (every 12 weeks), and may not have become symptomatic until later. With regard to the clinical trial design, we chose to use regularly scheduled skeletal surveys to detect pathological fractures objectively rather than based on investigator/patient reports, to mitigate potential assessment and reporting bias. While the overall burden of symptomatic skeletal events has not been established, the treatment effect (denosumab vs zoledronic acid) has been evaluated in patients with prostate cancer in these trials, and the SSE and SRE results were shown to be comparable [21, 40].
Among patients who experienced at least one SRE, 63 % of those with prostate cancer [41] and 69 % of those with breast cancer [42] developed subsequent SREs. In our population, a greater proportion of patients experienced an on-study SRE if they had experienced a previous SRE, compared with patients who did not have a previous SRE (40.3 vs 31.2 %). Preventing or delaying a first SRE would thus likely decrease the risk of subsequent SREs.
Measuring pain severity alone is insufficient to fully capture the impact of pain on patients. Evaluating the degree to which pain interferes with daily functioning overall as well as with individual aspects of daily functioning (emotional well-being and physical functioning) provides a more complete picture of patients’ experience. In this study, all SRE types except for surgery to bone were associated with a greater risk of pain interference overall, which is consistent with the pain severity results. Also, similar to the pain severity results, patients who had spinal cord compression and radiation to bone had the greatest risk increase in pain interference. For the subdimensions, all SRE types except for surgery to bone had an impact on pain interference with emotional well-being, and all SREs, including surgery to bone, had an impact on interference with physical activity. Therefore, SREs impact not only the sensory aspects of pain but also patients’ reaction to pain [28]. At each study visit, there was a significant correlation between increases in pain interference and decreases in cancer-specific QoL, suggesting that preventing SREs with bone-targeted agents may help maintain QoL in patients with bone metastases irrespective of antitumor therapies and disease burden.
The limitations of these analyses include that they were not prespecified. As individual SREs occur at different rates, and as we could not control the number of events for each SRE type, we may not have had an adequate sample size to detect significance in some instances (e.g., surgery to bone). Additionally, in some cases, we may have underestimated the impact of SREs, given that pain and analgesic use were assessed at monthly visits rather than through diaries at the time the SRE occurred. As such, we may not have captured the immediate and likely more substantial impact of the event. The descriptive analyses were meant to provide a visual representation of the change in pain and analgesic use over time in patients with and without an SRE, but do not take into account baseline differences in pain and analgesic use. We adjusted for those baseline differences in the regression model, and patients’ onset of SRE was also factored into the time-dependent analysis. However, considering the exploratory nature of the analysis, we cannot draw conclusions about causality. Another limitation is that all patients in these studies were receiving active treatment to delay SREs; untreated patients may have even greater increases in pain and analgesic use as well as decreases in QoL with SRE development. A previous report suggested that ~50 % of patients with breast cancer and bone metastases and ~80 % of those with prostate or lung cancer and bone metastases were not receiving treatment to prevent SREs [43]. Finally, selection bias may have caused an underestimation of the impact, because patients with a poor performance status were excluded from the trials and these patients may be at the highest risk for SREs and sustained decreases in QoL related to bone complications.
Conclusion
Patients who experienced SREs were at a greater risk of increased pain and opioid analgesic usage. Pain was severe enough to interfere with daily functioning. By preventing SREs, bone-targeted agents such as denosumab or bisphosphonates may delay pain worsening, help patients avoid the need for increased analgesic use, and thus reduce the burden of SREs on daily functioning.
References
Coleman RE (2001) Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev 27(3):165–176
Coleman RE (2006) Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 12(20 Pt 2):6243s–6249s
von Moos R, Sternberg C, Body JJ, Bokemeyer C (2013) Reducing the burden of bone metastases: current concepts and treatment options. Support Care Cancer 21(6):1773–1783
Vadhan-Raj S, von Moos R, Fallowfield LJ, Patrick DL, Goldwasser F, Cleeland CS, Henry DH, Novello S, Hungria V, Qian Y, Feng A, Yeh H, Chung K (2012) Clinical benefit in patients with metastatic bone disease: results of a phase 3 study of denosumab versus zoledronic acid. Ann Oncol 23(12):3045–3051
Mundy GR (2002) Metastasis to bone: causes, consequences and therapeutic opportunities. Nat Rev Cancer 2(8):584–593
Roodman GD (2004) Mechanisms of bone metastasis. N Engl J Med 350(16):1655–1664
Ford JA, Mowatt G, Jones R (2012) Assessing pharmacological interventions for bone metastases: the need for more patient-centered outcomes. Expert Rev Clin Pharmacol 5(3):271–279
Lipton A, Theriault RL, Hortobagyi GN, Simeone J, Knight RD, Mellars K, Reitsma DJ, Heffernan M, Seaman JJ (2000) Pamidronate prevents skeletal complications and is effective palliative treatment in women with breast carcinoma and osteolytic bone metastases: long term follow-up of two randomized, placebo-controlled trials. Cancer 88(5):1082–1090
Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L, Chin JL, Vinholes JJ, Goas JA, Zheng M, Zoledronic Acid Prostate Cancer Study Group (2004) Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone-refractory prostate cancer. J Natl Cancer Inst 96(11):879–882
Rosen LS, Gordon D, Tchekmedyian NS, Yanagihara R, Hirsh V, Krzakowski M, Pawlicki M, De Souza P, Zheng M, Urbanowitz G, Reitsma D, Seaman J (2004) Long-term efficacy and safety of zoledronic acid in the treatment of skeletal metastases in patients with nonsmall cell lung carcinoma and other solid tumors: a randomized, phase III, double-blind, placebo-controlled trial. Cancer 100(12):2613–2621
Costa L, Lipton A, Hadji P, Chen YM, Kosmidis P (2013) Treatment of bone metastases before the onset of pain. Int J Clin Oncol 18(3):531–538
Cleeland CS (2006) The measurement of pain from metastatic bone disease: capturing the patient’s experience. Clin Cancer Res 12(20 Pt 2):6236s–6242s
Lemay K, Wilson KG, Buenger U, Jarvis V, Fitzgibbon E, Bhimji K, Dobkin PL (2011) Fear of pain in patients with advanced cancer or in patients with chronic noncancer pain. Clin J Pain 27(2):116–124
Cleeland CS, Body JJ, Stopeck A, von Moos R, Fallowfield L, Mathias SD, Patrick DL, Clemons M, Tonkin K, Masuda N, Lipton A, de Boer R, Salvagni S, Oliveira CT, Qian Y, Jiang Q, Dansey R, Braun A, Chung K (2013) Pain outcomes in patients with advanced breast cancer and bone metastases: results from a randomized, double-blind study of denosumab and zoledronic acid. Cancer 119(4):832–838
Maltoni M (2008) Opioids, pain, and fear. Ann Oncol 19(1):5–7
Costa L, Major PP (2009) Effect of bisphosphonates on pain and quality of life in patients with bone metastases. Nat Clin Pract Oncol 6(3):163–174
Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA, Pandya KJ (1994) Pain and its treatment in outpatients with metastatic cancer. N Engl J Med 330(9):592–596
von Moos R, Body JJ, Egerdie B, Stopeck A, Brown JE, Damyanov D, Fallowfield LJ, Marx G, Cleeland CS, Patrick DL, Palazzo FG, Qian Y, Braun A, Chung K (2013) Pain and health-related quality of life in patients with advanced solid tumours and bone metastases: integrated results from three randomized, double-blind studies of denosumab and zoledronic acid. Support Care Cancer 21(12):3497–3507
Costa L, Badia X, Chow E, Lipton A, Wardley A (2008) Impact of skeletal complications on patients’ quality of life, mobility, and functional independence. Support Care Cancer 16(8):879–889
Stopeck AT, Lipton A, Body JJ, Steger GG, Tonkin K, de Boer RH, Lichinitser M, Fujiwara Y, Yardley DA, Viniegra M, Fan M, Jiang Q, Dansey R, Jun S, Braun A (2010) Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol 28(35):5132–5139
Fizazi K, Carducci M, Smith M, Damiäo R, Brown J, Karsh L, Milecki P, Shore N, Rader M, Wang H, Jiang Q, Tadros S, Dansey R, Goessl C (2011) Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet 377(9768):813–822
Henry DH, Costa L, Goldwasser F, Hirsh V, Hungria V, Prausova J, Scagliotti GV, Sleeboom H, Spencer A, Vadhan-Raj S, von Moos R, Willenbacher W, Woll PJ, Wang J, Jiang Q, Jun S, Dansey R, Yeh H (2011) Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol 29(9):1125–1132
Henry D, Vadhan-Raj S, Hirsh V, von Moos R, Hungria V, Costa L, Woll PJ, Scagliotti G, Smith G, Feng A, Jun S, Dansey R, Yeh H (2014) Delaying skeletal-related events in a randomized phase 3 study of denosumab versus zoledronic acid in patients with advanced cancer: an analysis of data from patients with solid tumors. Support Care Cancer 22(3):679–687
Scagliotti GV, Hirsh V, Siena S, Henry DH, Woll PJ, Manegold C, Solal-Celigny P, Rodriguez G, Krzakowski M, Mehta ND, Lipton L, Garcia-Saenz JA, Pereira JR, Prabhash K, Ciuleanu TE, Kanarev V, Wang H, Balakumaran A, Jacobs I (2012) Overall survival improvement in patients with lung cancer and bone metastases treated with denosumab versus zoledronic acid: subgroup analysis from a randomized phase 3 study. J Thorac Oncol 7(12):1823–1829
XGEVA® [package insert]. Thousand Oaks, CA: Amgen Inc. http://pi.amgen.com/united_states/xgeva/xgeva_pi.pdf. Accessed 31 March 2014
Lipton A, Fizazi K, Stopeck AT, Henry DH, Brown JE, Yardley DA, Richardson GE, Siena S, Maroto P, Clemens M, Bilynskyy B, Charu V, Beuzeboc P, Rader M, Viniegra M, Saad F, Ke C, Braun A, Jun S (2012) Superiority of denosumab to zoledronic acid for prevention of skeletal-related events: a combined analysis of 3 pivotal, randomised, phase 3 trials. Eur J Cancer 48(16):3082–3092
Cleeland CS, Ryan KM (1994) Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap 23(2):129–138
Cleeland CS (2009) The brief pain inventory user guide. The University of Texas MD. Anderson Cancer Center, Houston. http://www.mdanderson.org/education-and-research/departments-programs-and-labs/departments-and-divisions/symptom-research/symptom-assessment-tools/BPI_UserGuide.pdf. Accessed 31 March 2014.
Chung KC, Barlev A, Braun AH, Qian Y, Zagari M (2014) Assessing analgesic use in patients with advanced cancer: development of a new scale—the Analgesic Quantification Algorithm. Pain Med 15(2):225–232
Cella DF, Tulsky DS, Gray G, et al (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 11(3):570–579
Webster K, Cella D, Yost K (2003) The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes 1:79
Sathiakumar N, Delzell E, Morrisey MA, Falkson C, Yong M, Chia V, Blackburn J, Arora T, Kilgore ML (2011) Mortality following bone metastasis and skeletal-related events among men with prostate cancer: a population-based analysis of US Medicare beneficiaries, 1999–2006. Prostate Cancer Prostatic Dis 14(2):177–183
Sathiakumar N, Delzell E, Morrisey MA, Falkson C, Yong M, Chia V, Blackburn J, Arora T, Brill I, Kilgore ML (2012) Mortality following bone metastasis and skeletal-related events among women with breast cancer: a population-based analysis of U.S. Medicare beneficiaries, 1999-2006. Breast Cancer Res Treat 131(1):231–238
Fizazi K, Massard C, Smith M, Rader M, Brown J, Milecki P, Shore N, Oudard S, Karsh L, Carducci M, Damiao R, Wang H, Ying W, Goessl C (2015) Bone-related parameters are the main prognostic factors for overall survival in men with bone metastases from castration-resistant prostate cancer. Eur Urol 68(1):42–50
Yong M, Jensen AO, Jacobsen JB, Norgaard M, Fryzek JP, Sorensen HT (2011) Survival in breast cancer patients with bone metastases and skeletal-related events: a population-based cohort study in Denmark (1999-2007). Breast Cancer Res Treat 129(2):495–503
Norgaard M, Jensen AO, Jacobsen JB, Cetin K, Fryzek JP, Sorensen HT (2010) Skeletal related events, bone metastasis and survival of prostate cancer: a population based cohort study in Denmark (1999 to 2007). J Urol 184(1):162–167
Cetin K, Christiansen CF, Jacobsen JB, Norgaard M, Sorensen HT (2014) Bone metastasis, skeletal-related events, and mortality in lung cancer patients: a Danish population-based cohort study. Lung Cancer 86(2):247–254
Nieder C (2014) Repeat palliative radiotherapy for painful bone metastases. Lancet Oncol 15(2):126–128
Chow E, van der Linden YM, Roos D, Hartsell WF, Hoskin P, Wu JS, Brundage MD, Nabid A, Tissing-Tan CJ, Oei B, Babington S, Demas WF, Wilson CF, Meyer RM, Chen BE, Wong RK (2014) Single versus multiple fractions of repeat radiation for painful bone metastases: a randomised, controlled, non-inferiority trial. Lancet Oncol 15(2):164–171
Smith MR, Coleman RE, Klotz L, Pittman KB, Milecki P, Wei R, Balakumaran A, Fizazi K (2014) Denosumab for the prevention of symptomatic skeletal events in patients with castration-resistant advanced prostate cancer: a comparison with skeletal-related events. J Clin Oncol 32(4 suppl):35
Hussain A, Yong C, Tkaczuk K, Qian Y, Arellano J, Balakumaran A, Liede A, Mullins CD, Onukwugha E (2014) Prevalence of and factors associated with skeletal-related events in older United States women diagnosed with metastatic breast cancer. Poster presented at: MASCC/ISOO International Symposium on Supportive Care in Cancer; June 26–28, 2014, Miami, FL, USA
Abdulhalim AM, Hussain A, Mullins CD, Qian Y, Arellano J, Balakumaran A, Onukwugha E (2014) Burden and timing of first and subsequent skeletal related events (SREs) in US elderly men with metastatic prostate cancer. Presented at: International Society for Pharmacoeconomics and Outcomes Research; May 31-June 4, 2014, Montreal, QC, Canada
Oster G, Lamerato L, Glass AG, Richert-Boe KE, Lopez A, Chung K, Richhariya A, Dodge T, Wolff GG, Balakumaran A, Edelsberg J (2013) Natural history of skeletal-related events in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systems. Support Care Cancer 21(12):3279–3286
Acknowledgments
This study was supported by Amgen. Medical writing support was provided by Lori (Gorton) Smette, PhD, of Amgen. The study sponsor was involved in the study design, analyses, interpretation of the findings, and decision to submit the article for publication. Study investigators collected data and interpreted the findings. The authors had access to all data, reviewed each draft, and provided approval to submit the article for publication.
Conflict of interest
Roger von Moos received speaker honoraria, consultant fee, and unrestricted research grant from Amgen; speaker honoraria and consultant fee from GSK and Novartis; speaker honoraria, consultant fee, and research grant from Roche; and speaker honoraria from Bayer.
Jean-Jacques Body received lecture and consulting fees from Amgen and has a consultant/advisory role with Bayer.
Janet Brown is a member of the advisory boards for Amgen and Novartis.
Charles Cleeland is a previous consultant for Amgen.
Danail Damyanov and Felipe Salvador Palazzo have nothing to disclose.
Blair Egerdie received research funding from and is an advisory board member and a lecturer for Amgen.
Gavin Marx received funding from Amgen, Sanofi, and AstraZeneca.
Donald Patrick received past consultancy fees from Amgen.
Lesley Fallowfield received consultancy and advisory board fees in the past from Amgen.
Alison Stopeck received consultancy and honorarium from Amgen and clinical trial support to her institution from Amgen.
Ada Braun is a former employee of Amgen and owns stock in the company.
Arun Balakumaran is a former employee of Amgen and owns stock in Amgen and Merck.
Ying Zhou and Yi Qian are employees of Amgen and hold stock in the company.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Patients provided written informed consent before any study-specific procedures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
von Moos, R., Body, JJ., Egerdie, B. et al. Pain and analgesic use associated with skeletal-related events in patients with advanced cancer and bone metastases. Support Care Cancer 24, 1327–1337 (2016). https://doi.org/10.1007/s00520-015-2908-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2908-1